Journal Description
Journal of Clinical Medicine
Journal of Clinical Medicine
is an international, peer-reviewed, open access journal of clinical medicine, published semimonthly online by MDPI. The International Bone Research Association (IBRA), Spanish Society of Hematology and Hemotherapy (SEHH), Japan Association for Clinical Engineers (JACE), European Independent Foundation in Angiology/ Vascular Medicine (VAS) and others are all affiliated with JCM, and their members receive a discount on article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, PMC, Embase, CAPlus / SciFinder, and other databases.
- Journal Rank: JCR - Q1 (Medicine, General and Internal) / CiteScore - Q1 (General Medicine)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 17.7 days after submission; acceptance to publication is undertaken in 2.7 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
- Companion journals for JCM include: Epidemiologia, Transplantology, Uro, Sinusitis, Rheumato, Journal of Clinical & Translational Ophthalmology, Journal of Vascular Diseases, Osteology, Complications, Therapeutics, Sclerosis, Pharmacoepidemiology and Journal of CardioRenal Medicine.
- Journal Clusters of Hematology: Hemato, Hematology Reports, Thalassemia Reports and Journal of Clinical Medicine.
Impact Factor:
2.9 (2024);
5-Year Impact Factor:
3.3 (2024)
Latest Articles
Cognitive Impairment in Patients with Severe COPD: A Cross-Sectional Study
J. Clin. Med. 2025, 14(19), 7122; https://doi.org/10.3390/jcm14197122 (registering DOI) - 9 Oct 2025
Abstract
Background/Objectives: Cognitive impairment (CI) in patients with chronic obstructive pulmonary disease (COPD) has been associated with reduced physical activity and decreased adherence to inhalation therapy. The primary aim of this study is to examine the prevalence of CI in patients with severe
[...] Read more.
Background/Objectives: Cognitive impairment (CI) in patients with chronic obstructive pulmonary disease (COPD) has been associated with reduced physical activity and decreased adherence to inhalation therapy. The primary aim of this study is to examine the prevalence of CI in patients with severe COPD and secondly compare outcomes with non-COPD comparators. Methods: Patients with severe COPD defined as forced expiratory volume in first second (FEV1) <50% were recruited between January 2021 to January 2023 along with non-COPD comparators. CI was defined as a MoCA score <26, adding one point for participants with ≤12 years of education. Additionally, two functional cognitive tests were included: the Continuous Reaction Time test (CRT) and a driving simulator. Results: Eighty patients with COPD (mean age 64 years) and 22 non-COPD comparators (mean age 61 years) participated. CI was identified in 32 patients with COPD (40%) and six non-COPD comparators (27%) with a 0.87 non-significant difference (95% CI: −0.15–1.88). The functional tests showed a 0.267 difference in CRT index (95% CI: 0.023–0.511) and a 0.056 difference in standard deviation from center of the road (95% CI: 0.002–0.11) revealing a significantly poorer performance in functional tests among patients compared to non-COPD comparators. Nineteen patients with COPD and one non-COPD comparator failed the driving test (p = 0.04). Conclusions: CI was found in 40% of patients with severe COPD based on MoCA score. While MoCA score did not differ between the two groups, functional tests demonstrated significantly reduced abilities in patients compared with non-COPD comparators.
Full article
(This article belongs to the Section Respiratory Medicine)
Open AccessArticle
Sleep Quality and Sex-Specific Physical Activity Benefits Predict Mental Health in Romanian Medical Students: A Cross-Sectional Analysis
by
Catalin Plesea-Condratovici, Alina Plesea-Condratovici, Silvius Ioan Negoita, Valerian-Ionut Stoian, Lavinia-Alexandra Moroianu and Liliana Baroiu
J. Clin. Med. 2025, 14(19), 7121; https://doi.org/10.3390/jcm14197121 (registering DOI) - 9 Oct 2025
Abstract
Background: Evidence on how everyday walking and sleep relate to mood in health profession students from Central–Eastern Europe remains limited. Methods: We conducted a cross-sectional study among 277 Romanian medical students. Data were collected using validated instruments for physical activity (IPAQ-SF),
[...] Read more.
Background: Evidence on how everyday walking and sleep relate to mood in health profession students from Central–Eastern Europe remains limited. Methods: We conducted a cross-sectional study among 277 Romanian medical students. Data were collected using validated instruments for physical activity (IPAQ-SF), sleep quality (PSQI), and depressive/anxiety symptoms (HADS). Associations were examined using bivariate and multivariable regression models, including sex-stratified analyses. Results: In bivariate analysis, total physical activity was inversely correlated with depressive symptoms (ρ = −0.19, p < 0.001). However, in the multivariable model, this effect was not statistically significant after controlling for other factors. Poor sleep quality emerged as the dominant independent predictor of both depression (β = 0.37, p < 0.001) and anxiety (β = 0.40, p < 0.001). Walking time and frequency were specifically protective against depressive symptoms. Sex-stratified analyses revealed distinct patterns: female students benefited more from walking, whereas male students showed stronger associations between overall physical activity and lower depressive symptoms. Conclusions: Within the constraints of a cross-sectional design, this study provides novel evidence from Eastern Europe that sleep quality and physical activity are central to student mental health. Psychological benefits of walking appear sex-specific, and the null mediation finding suggests benefits operate via direct or unmodelled pathways. Sleep is a critical independent target for tailored, lifestyle-based strategies.
Full article
(This article belongs to the Special Issue Clinical Perspectives on Physical Activity and Health Across the Lifespan)
►▼
Show Figures
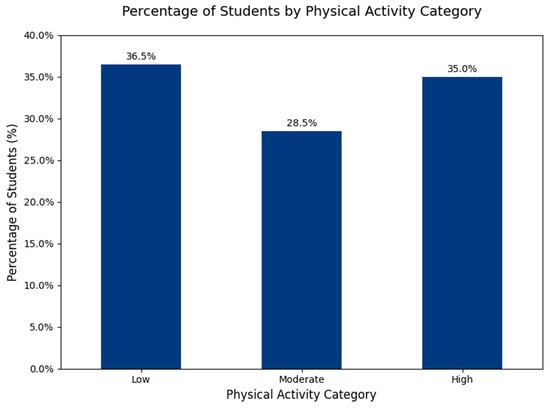
Figure 1
Open AccessArticle
The Association Between Cardiorespiratory Fitness Directly Assessed by the Cardiopulmonary Stress Test and the Perception of Stress
by
Gianluigi Oggionni, Marcello Rizzi, Giuseppina Bernardelli, Mara Malacarne, Massimo Pagani and Daniela Lucini
J. Clin. Med. 2025, 14(19), 7120; https://doi.org/10.3390/jcm14197120 (registering DOI) - 9 Oct 2025
Abstract
Background/Objectives: Cardiorespiratory fitness (CRF) represents a strong and consistent predictor of mortality among adults. It is ideally expressed as the maximum or peak rate of oxygen consumption per kilogram of body mass (VO2max) determined by the cardiopulmonary exercise test (CPX). Variance
[...] Read more.
Background/Objectives: Cardiorespiratory fitness (CRF) represents a strong and consistent predictor of mortality among adults. It is ideally expressed as the maximum or peak rate of oxygen consumption per kilogram of body mass (VO2max) determined by the cardiopulmonary exercise test (CPX). Variance in CRF is mainly attributable to genetics and physical training; nevertheless, strong behavioral and socioeconomic confounders need to be considered. Among those, psychosocial stress may play an important role. Some papers show an association between low CRF and chronic stress conditions; nevertheless, CRF is generally estimated by indirect assessment and not directly measured by CPX. Methods: CRF was directly assessed by performing a CPX in 145 consecutive subjects (56 male, 89 female) (age 19–65 years) who attended our Exercise Medicine unit for health check-ups. Weekly total volume of physical activity (PA) was evaluated using a validated questionnaire (IPAQ); perceptions of stress, fatigue, and somatic symptoms were assessed using a self-administered questionnaire. Results: VO2max was negatively correlated with perception of stress (p = 0.03), fatigue (p < 0.001), and somatic symptoms (p < 0.001); as expected, it was positively correlated with the weekly volume of PA (p < 0.001). This link was further evidenced by the observation that subjects who did not meet the PA goals as indicated by WHO guidelines presented a higher perception of stress, fatigue, and symptoms, as compared to physically active subjects. Conclusions: This direct link might, on the one hand, corroborate the role of exercise as a tool to manage stress and, on the other hand, focus on the role of stress as a possible determinant of CRF.
Full article
(This article belongs to the Special Issue Advancements in Diagnostic Innovations in Sports Cardiology)
Open AccessReview
Sleep Disorders in Neurodegenerative Diseases with Dementia: A Comprehensive Review
by
Natalia Siwecka, Michał Golberg, Dominika Świerczewska, Beata Filipek, Karolina Pendrasik, Adrianna Bączek-Grzegorzewska, Mariusz Stasiołek and Mariola Świderek-Matysiak
J. Clin. Med. 2025, 14(19), 7119; https://doi.org/10.3390/jcm14197119 (registering DOI) - 9 Oct 2025
Abstract
Dementia is a growing problem of global relevance, currently affecting over 55 million people worldwide. The number of new dementia cases is still increasing, primarily due to the aging of society. Dementia is defined as a substantial decline in cognitive function, and it
[...] Read more.
Dementia is a growing problem of global relevance, currently affecting over 55 million people worldwide. The number of new dementia cases is still increasing, primarily due to the aging of society. Dementia is defined as a substantial decline in cognitive function, and it is inherently associated with neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, dementia with Lewy bodies, frontotemporal dementia, and vascular dementia. Of note, most patients suffering from neurodegenerative conditions, in addition to cognitive impairment, often experience various types of sleep disorders, including insomnia, rapid eye movement sleep behavior disorder, sleep-disordered breathing, and circadian rhythm disturbances. There is increasing evidence of a bidirectional interaction between sleep disturbances and mental health. Disrupted sleep may directly aggravate neuropsychiatric symptoms, like depression, anxiety, agitation, and hallucinations, and conversely, such symptoms can make sleeping more difficult. This creates a feedback loop that inevitably leads to disease progression and deterioration in quality of life. In this review, we provide an up-to-date overview of the nature and mechanisms behind sleep disorders in major neurodegenerative diseases, summarize treatment strategies for handling sleep disturbances, and discuss the clinical relevance of sleep–mental health interactions in the context of neurodegeneration-associated dementia. Neurodegeneration is a complex problem on the border between neurology and psychiatry, and it poses a challenge to the healthcare system, as it requires multidisciplinary approaches for optimal management. Understanding the connection between sleep and neuropsychiatric symptoms offers further opportunities for better symptom control, improved quality of life, and slower cognitive decline.
Full article
(This article belongs to the Special Issue The Association Between Sleep Disorders and Metabolic and Mental Health)
Open AccessArticle
Transpancreatic Sphincterotomy Is a Safe and Effective Pancreatic Guidewire-Assisted Cannulation Method: Real-World Data Analysis of the Hungarian ERCP Registry
by
Dániel Pécsi, Nelli Farkas, Szilárd Gódi, Péter Hegyi, Andrea Szentesi, István Altorjay, Tamás Bakucz, Ákos Orbán-Szilágyi, Zoltán Szepes, László Czakó, Árpád Patai, Tibor Gyökeres, Roland Fejes, Zsolt Dubravcsik and Áron Vincze
J. Clin. Med. 2025, 14(19), 7118; https://doi.org/10.3390/jcm14197118 (registering DOI) - 9 Oct 2025
Abstract
Background/Objectives: Difficult biliary cannulation during endoscopic retrograde cholangiopancreatography (ERCP) poses significant challenges and increases the risk of adverse events. Pancreatic guidewire (PGW)-assisted techniques offer potential solutions, but real-world comparative data are limited. Methods: This cohort study of prospectively collected data analyzed 234 ERCP
[...] Read more.
Background/Objectives: Difficult biliary cannulation during endoscopic retrograde cholangiopancreatography (ERCP) poses significant challenges and increases the risk of adverse events. Pancreatic guidewire (PGW)-assisted techniques offer potential solutions, but real-world comparative data are limited. Methods: This cohort study of prospectively collected data analyzed 234 ERCP cases from the Hungarian ERCP Registry, focusing on three PGW-assisted methods: transpancreatic sphincterotomy (TPS), double-guidewire technique (DGW), and prophylactic pancreatic stent-assisted cannulation (PPS-C). Results: TPS demonstrated the highest primary cannulation success rate (83.1%), significantly outperforming DGW (67.7%) and PPS-C (67.6%) (p < 0.001). With salvage methods, cannulation success was high across all groups. Post-ERCP pancreatitis rates were low (5.0% TPS, 5.6% DGW, 3.9% PPS-C), but prophylactic measures (pancreatic stents, indomethacin) were underutilized. Conclusions: Our findings suggest that TPS is a safe and effective alternative for difficult biliary cannulation in ERCP. Routine considerations of post-ERCP pancreatitis prophylaxis (prophylactic pancreatic stents and non-steroidal suppositories) are recommended in all PGW-assisted cannulations to minimize complications.
Full article
(This article belongs to the Section Gastroenterology & Hepatopancreatobiliary Medicine)
Open AccessArticle
Evaluation of Ganglion Cell–Inner Plexiform Layer Thickness in the Diagnosis of Preperimetric and Early Perimetric Glaucoma
by
Ilona Anita Kaczmarek, Marek Edmund Prost and Radosław Różycki
J. Clin. Med. 2025, 14(19), 7117; https://doi.org/10.3390/jcm14197117 (registering DOI) - 9 Oct 2025
Abstract
Background: Optical coherence tomography (OCT) is the main diagnostic technology used to detect damage to the retinal ganglion cells (RGCs) in glaucoma. However, it remains unclear which OCT parameter demonstrates the best diagnostic performance for eyes with early, especially preperimetric glaucoma (PPG). We
[...] Read more.
Background: Optical coherence tomography (OCT) is the main diagnostic technology used to detect damage to the retinal ganglion cells (RGCs) in glaucoma. However, it remains unclear which OCT parameter demonstrates the best diagnostic performance for eyes with early, especially preperimetric glaucoma (PPG). We determined the diagnostic performance of ganglion cell–inner plexiform layer (GCIPL) parameters using spectral-domain OCT (SD-OCT) in primary open-angle preperimetric and early perimetric glaucoma and compared them with optic nerve head (ONH) and peripapillary retinal nerve fiber layer (pRNFL) parameters. Methods: We analyzed 101 eyes: 36 normal eyes, 33 with PPG, and 32 with early perimetric glaucoma. All patients underwent Topcon SD–OCT imaging using the Optic Disc and Macular Vertical protocols. The diagnostic abilities of the GCIPL, rim area, vertical cup-to-disc ratio (CDR), and pRNFL were assessed using the area under the receiver operating characteristic curve (AUC). Results: For PPG, the AUCs ranged from 0.60 to 0.63 (GCIPL), 0.82 to 0.86 (ONH), and 0.49 to 0.75 (pRNFL). For early perimetric glaucoma, the AUCs for GCIPL and pRNFL ranged from 0.81 to 0.88 and 0.57 to 0.91, respectively, whereas both ONH parameters demonstrated an AUC of 0.89. The GCIPL parameters were significantly lower than both ONH parameters in detecting preperimetric glaucoma (p < 0.05). For early perimetric glaucoma, comparisons between the AUCs of the best-performing mGCIPL parameters and those of the best-performing pRNFL and ONH parameters revealed no significant differences in their diagnostic abilities (p > 0.05). Conclusions: GCIPL parameters exhibited a diagnostic performance comparable to that of ONH and pRNFL parameters for early perimetric glaucoma. However, their ability to detect preperimetric glaucoma was significantly lower than the ONH parameters.
Full article
(This article belongs to the Section Ophthalmology)
Open AccessReview
Multiple Myeloma Laboratory Diagnostics Made Simple: Practical Insights and Key Recommendations
by
Ana Marta Pires, João Pedro Barreto, Joana Caetano, Maria José Soares, Catarina Geraldes, Bruno Fernandes, Margarida Coucelo, Sérgio Chacim, Henrique Coelho, Cecília Correia, Ana Paula Cruz, Manuel Cunha, Maria Rosário Cunha, Nuno Cunha, Patrícia Ferraz, José Guilherme Freitas, Rui Henrique, Susana Lisboa, Paulo Lúcio, Artur Paiva, Cláudia Pedrosa, Inês Ramos, Ana Bela Sarmento-Ribeiro, Patrícia Seabra, Joana Sevilha, Maria José Rego de Sousa, Sara Sousa, Teresa Sousa, Márcio Tavares, Fernanda Trigo, Adriana Roque, Rui Bergantim, Cristina João and on behalf of the Portuguese Multiple Myeloma Groupadd
Show full author list
remove
Hide full author list
J. Clin. Med. 2025, 14(19), 7115; https://doi.org/10.3390/jcm14197115 (registering DOI) - 9 Oct 2025
Abstract
Multiple myeloma is a clonal plasma cell malignancy with a highly variable range of clinical manifestations. Over recent decades, substantial progress has been made in laboratory diagnostics, which has deepened our understanding of disease biology, improved risk stratification, and informed treatment strategies. In
[...] Read more.
Multiple myeloma is a clonal plasma cell malignancy with a highly variable range of clinical manifestations. Over recent decades, substantial progress has been made in laboratory diagnostics, which has deepened our understanding of disease biology, improved risk stratification, and informed treatment strategies. In an era of transformation and innovation, conventional laboratory methods remain essential, as cutting-edge technologies might not be immediately accessible to all laboratories. Nonetheless, even widely used laboratory methodologies present many challenges, such as variability in assay performance, interpretative criteria, and standardization. This review by the Portuguese Multiple Myeloma Group of the Portuguese Society of Hematology provides a comprehensive overview and practical appraisal of current conventional laboratory methods employed for multiple myeloma diagnosis.
Full article
(This article belongs to the Section Clinical Laboratory Medicine)
►▼
Show Figures
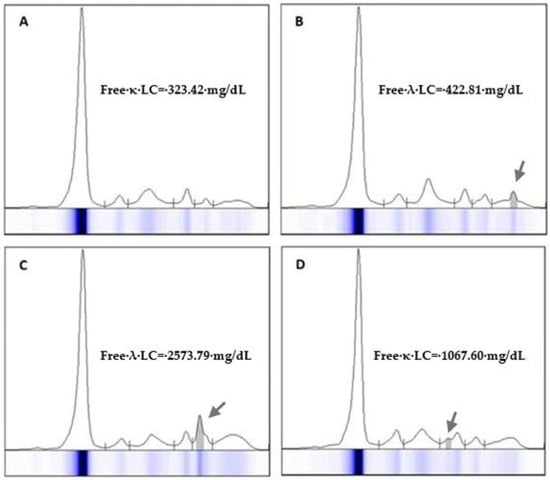
Figure 1
Open AccessArticle
Surgery in Staphylococcus aureus Infective Endocarditis: Clinical Outcomes, Neurological Sequelae, and Prognostic Implications
by
Ahmed Elderia, Julian Hinzmann, Patricia Soehne, Walid Bennour, Thorsten Wahlers and Carolyn Weber
J. Clin. Med. 2025, 14(19), 7114; https://doi.org/10.3390/jcm14197114 - 9 Oct 2025
Abstract
Background:Staphylococcus aureus infective endocarditis (SA-IE) is believed to provoke higher rates of complications compared to other organisms that commonly cause IE (non-SA-IE). We believe that Staphylococcus aureus (S. aureus) has a high propensity to cause embolic events and cerebrovascular neurological
[...] Read more.
Background:Staphylococcus aureus infective endocarditis (SA-IE) is believed to provoke higher rates of complications compared to other organisms that commonly cause IE (non-SA-IE). We believe that Staphylococcus aureus (S. aureus) has a high propensity to cause embolic events and cerebrovascular neurological complications. Methods: We conducted a single-center retrospective analysis, encompassing 529 patients who had undergone valve surgery for IE. Patients were divided according to causative microorganism into SA-IE and non-SA-IE groups. Subsequently, analyses of outcome differences between the two groups were performed, with a focus on neurological complications. Results: In the examined population, 128 (24.2%) had IE mediated by S. aureus. Patients with SA-IE were mostly male (69.3%) but had a higher proportion of females compared to non-SA-IE patients (30.7% vs. 21.8%; p = 0.039) and were significantly younger (61.1 [45.8–69.9] vs. 66.1 [54.3–74.4]; p = 0.002). Patients with SA-IE had comparable comorbidities to patients with non-SA-IE. Neurological complications were much more common in SA-IE (42.2%) compared to non-SA-IE (22.9%); (p < 0.001). Postoperative neurological complications were nearly equal in both groups—SA-IE 5.5% vs 6.2% in non-SA-IE (p = 0.752); 30-day mortality was significantly higher in patients with SA-IE vs. non-SA-IE (20.3% vs 12.5%; p = 0.028). However, the 1-year mortality rate did not differ between groups (29.4% vs. 22.2%; p = 0.121). Conclusions: Patients with SA-IE are subject to a higher incidence of neurological events prior to surgery and almost twice the short-term mortality rate compared to IE caused by other microorganisms. However, no observable discrepancy in the incidence of neurological events was found between SA- and non-SA-IE cases post-surgery.
Full article
(This article belongs to the Special Issue Clinical Advances in Cardiovascular Interventions)
►▼
Show Figures
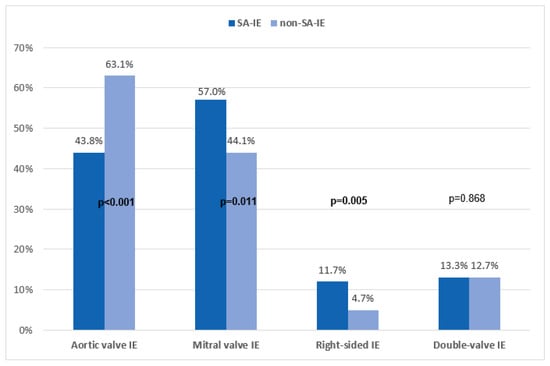
Figure 1
Open AccessArticle
Femoral Closure with Single ProGlide® in Transcatheter Aortic Valve Implantation: A Registry-Based Study
by
Kévin Roulot, Marion Kibler, Antonin Trimaille, Adrien Carmona, Amandine Granier, Philoktimon Plastaras, Jérome Rischner, Stéphane Greciano, Pierre Leddet, Fabien De Poli, Mohamad Kanso, Ulun Crimizade, Karen Boyer, Minh Hoang, Michel Kindo, Laurence Jesel, Olivier Morel and Patrick Ohlmann
J. Clin. Med. 2025, 14(19), 7113; https://doi.org/10.3390/jcm14197113 - 9 Oct 2025
Abstract
Background: Vascular closure of the femoral artery during transcatheter aortic valve implantation (TAVI) remains a critical step prone to complications, despite advancements in introducer technology. The traditional technique involves using two ProGlide® suture closure devices (2P), but alternative approaches, such as employing
[...] Read more.
Background: Vascular closure of the femoral artery during transcatheter aortic valve implantation (TAVI) remains a critical step prone to complications, despite advancements in introducer technology. The traditional technique involves using two ProGlide® suture closure devices (2P), but alternative approaches, such as employing a single ProGlide® device (1P), have emerged. Aims: We sought to evaluate the efficacy and safety of the 1P strategy compared to the standard 2P closure technique during transfemoral TAVI procedures. Methods: A registry-based study was conducted at the University Hospitals of Strasbourg, France, from January 2020 to December 2023. Consecutive patients who underwent TAVI via the transfemoral approach were deemed eligible. Results: The study cohort consisted of 1303 patients, with a mean age of 81.7 years and 47% female. The 1P strategy was used in 733 cases (56.3%), while the 2P technique was employed in 570 patients (43.7%). Hemostasis was achieved in the catheterization laboratory without additional devices in 30.4% of the single-ProGlide® pre-closing cases. Vascular complication rates were similar in both groups, at 11.3% for the 1P technique and 11.4% for the 2P technique (p = 0.964). However, vascular closure device failure was significantly less frequent in the 1P group (1.6%) compared to the 2P group (5.3%). Conclusions: The 1P strategy for pre-closing during TAVI is as effective and safe as the conventional 2P approach. The 1P method offers potential advantages in terms of simplicity and cost-effectiveness.
Full article
(This article belongs to the Section Cardiovascular Medicine)
►▼
Show Figures
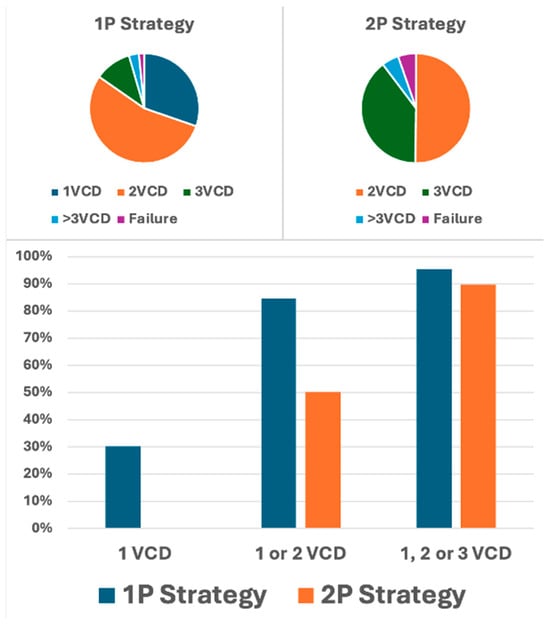
Figure 1
Open AccessArticle
Clinical Value of Transcutaneous PCO2 in Free Flap Blood Supply
by
Fangfang Liu, Nannan Han, Lei Wang, Jinxiu Dong, Min Ruan and Youguo Ying
J. Clin. Med. 2025, 14(19), 7112; https://doi.org/10.3390/jcm14197112 - 9 Oct 2025
Abstract
Background: Transcutaneous PCO2 (TcPCO2) effectively represents the partial pressure of carbon dioxide in deep tissues, providing us with more accurate information regarding deep tissue perfusion and oxygen metabolism. Based on this, we aimed to explore the clinical value of TcPCO
[...] Read more.
Background: Transcutaneous PCO2 (TcPCO2) effectively represents the partial pressure of carbon dioxide in deep tissues, providing us with more accurate information regarding deep tissue perfusion and oxygen metabolism. Based on this, we aimed to explore the clinical value of TcPCO2 in assessing free flap blood supply during oral cancer surgery. Methods: A total of 27 patients undergoing oral cancer reconstruction with free flap reconstruction were enrolled. For enrolled patients, continuous monitoring was conducted before, during, and after free flap transplantation surgery. Results: A total of 121 measurements were taken, comprising 93 instances in the normal flap group and 28 instances in the insufficient flap group. The TcPCO2 levels were significantly higher and transcutaneous PO2 (TcPO2) levels were lower in the insufficient group (p < 0.001). The cutoff values for TcPCO2 and TcPO2, calculated using the Youden index, were 66 mmHg and 16 mmHg, respectively. TcPCO2 exhibits high specificity in monitoring the blood supply of free flaps. The area under the ROC curve (AUC) for TcPCO2 in predicting insufficient flap perfusion was calculated to be 0.912. Conclusions: TcPCO2 demonstrates high specificity in assessing blood supply in free flaps for patients undergoing oral cancer surgery and has diagnostic significance for early identification of insufficient flap.
Full article
(This article belongs to the Section Dentistry, Oral Surgery and Oral Medicine)
►▼
Show Figures
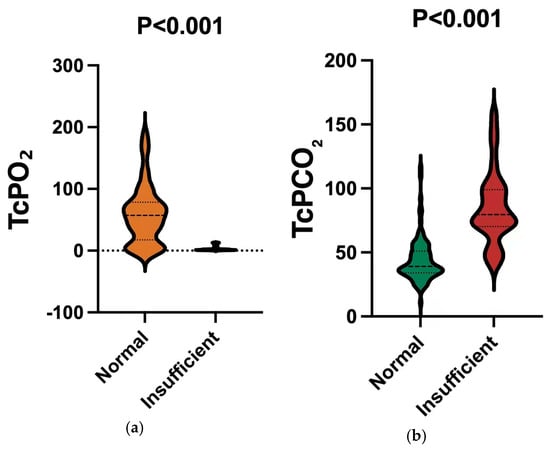
Figure 1
Open AccessReview
Functional Capacity Evaluation and Rehabilitation Strategies in Cardiac Amyloidosis: A Comprehensive Review
by
Anthoula Plevritaki, Konstantinos Volaklis, Eleni Nakou, Constantinos Davos, Ioannis Kopidakis, Eleftherios Kallergis, Eirini Savva, Emmanouil Simantirakis, Aneta Aleksova and Maria Marketou
J. Clin. Med. 2025, 14(19), 7111; https://doi.org/10.3390/jcm14197111 - 9 Oct 2025
Abstract
Cardiac amyloidosis (CA) is an increasingly recognized cause of restrictive cardiomyopathy characterized by amyloid fibril deposition in the heart, leading to severe functional impairments and poor prognosis. This review aims to provide a comprehensive overview of the pathophysiology of CA, emphasizing the mechanisms
[...] Read more.
Cardiac amyloidosis (CA) is an increasingly recognized cause of restrictive cardiomyopathy characterized by amyloid fibril deposition in the heart, leading to severe functional impairments and poor prognosis. This review aims to provide a comprehensive overview of the pathophysiology of CA, emphasizing the mechanisms underlying functional capacity limitations and highlighting the importance of precise physiological assessment tools. We focus on objective measures such as cardiopulmonary exercise testing, field-based functional tests, and frailty evaluations that are vital for prognosis and tailoring patient care. With recent advances in disease-modifying therapies extending survival, maintaining and improving functional status through multidisciplinary rehabilitation emerges as a crucial therapeutic target. Evidence suggests that structured aerobic and resistance training can enhance exercise tolerance, strength, and quality of life in CA patients, although further research is needed to optimize rehabilitation protocols. By integrating clinical, physiological, and rehabilitative insights, this review underscores the value of a patient-centered approach aimed at preserving functional capacity and improving outcomes in this complex and systemic disease.
Full article
(This article belongs to the Special Issue The Role of Cardiac Rehabilitation After Myocardial Infarction, Coronary Artery Bypass Surgery, and in Other Cardiac Diseases)
►▼
Show Figures
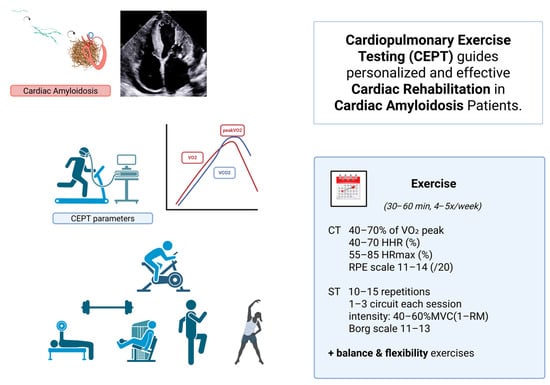
Figure 1
Open AccessArticle
Prevalence of Sleep Disturbance and Associated Risk Factors in Degenerative Cervical Myelopathy
by
Salim Yakdan, Karan Joseph, Jingyi Zhang, Miguel A. Ruiz-Cardozo, Aryan Pradhan, Alisha Dhallan, Faraz Arkam, Willliam Mualem, Garrison Bentz, Diogo P. Moniz Garcia, Benjamin Plog, Alexander T. Yahanda, Daniel Hafez, Wilson Z. Ray, Camilo A. Molina and Jacob K. Greenberg
J. Clin. Med. 2025, 14(19), 7110; https://doi.org/10.3390/jcm14197110 - 9 Oct 2025
Abstract
Study Design: Retrospective Case–Control. Objectives: Sleep disturbances negatively impact quality of life and increase illness susceptibility. Chronic pain is a risk factor for sleep disruption, particularly in patients with degenerative spinal conditions. Existing studies suggest that degenerative cervical myelopathy (DCM) patients often experience
[...] Read more.
Study Design: Retrospective Case–Control. Objectives: Sleep disturbances negatively impact quality of life and increase illness susceptibility. Chronic pain is a risk factor for sleep disruption, particularly in patients with degenerative spinal conditions. Existing studies suggest that degenerative cervical myelopathy (DCM) patients often experience sleep disturbances, possibly due to spinal cord compression and pain. However, most research is limited to small, single-center studies, creating a need for broader analyses. Methods: We utilized the Merative Explorys Dataset, focusing on electronic health record data of patients diagnosed with DCM and sleep disorders identified via ICD codes. Comorbidities analyzed included depression/bipolar disorder, chronic pulmonary disease, migraine, osteoarthritis, hypertension, malignancy, diabetes, and cerebrovascular disease. Patient demographic information (age, race, sex, and body mass index (BMI)) was included as covariates. Logistic regression analyses were performed to evaluate the association between each comorbidity and the risk of sleep disturbance. Results: Among 40,551 DCM patients, significant predictors of sleep disturbance included higher BMI (OR: 1.05, 95% CI: 1.05–1.06), depression/bipolar disorder (OR: 1.65, 95% CI: 1.56–1.74), chronic pulmonary disease (OR: 1.26, 95% CI: 1.20–1.33), migraine (OR: 1.32, 95% CI: 1.22–1.43), and hypertension (OR: 1.16, 95% CI: 1.10–1.23). Conclusions: This large-scale analysis demonstrates the multifactorial nature of sleep disturbances in DCM, highlighting strong associations with BMI and respiratory conditions, suggesting a contributory role of sleep-disordered breathing. The identification of migraines as a risk factor highlights the need for multidisciplinary management. Addressing modifiable risk factors such as BMI and mental health may improve sleep quality in DCM patients.
Full article
(This article belongs to the Special Issue Emerging Trends in Cervical Spine Surgery)
►▼
Show Figures

Figure 1
Open AccessArticle
Multidimensional Impulsivity Profile in Young Adults Aged 16 to 25 with Borderline Personality Disorder: A Study Based on the UPPS-P Model
by
Anaïs Mungo, Marie Delhaye and Matthieu Hein
J. Clin. Med. 2025, 14(19), 7109; https://doi.org/10.3390/jcm14197109 - 9 Oct 2025
Abstract
Background: Borderline Personality Disorder (BPD) often emerges during adolescence and young adulthood, a period marked by heightened vulnerability to impulsivity and affective dysregulation. While impulsivity is a core feature of BPD, its multidimensional expression in this age group remains insufficiently documented. This
[...] Read more.
Background: Borderline Personality Disorder (BPD) often emerges during adolescence and young adulthood, a period marked by heightened vulnerability to impulsivity and affective dysregulation. While impulsivity is a core feature of BPD, its multidimensional expression in this age group remains insufficiently documented. This study examined impulsivity traits in young adults with BPD, their associations with depressive and anxiety symptoms, and their links to risk behaviors. Methods: A total of 160 participants aged 16–25 were recruited in Belgium between 2021 and 2023: 44 with BPD from inpatient and outpatient psychiatric services and 116 healthy controls from schools and universities. Assessments included the short UPPS-P, Beck Depression Inventory-II (BDI-II), State-Trait Anxiety Inventory (STAI-T), and the Diagnostic Interview for Borderlines–Revised (DIB-R). Logistic regressions with robust errors and Kendall’s tau-b correlations were used. Results: Compared with controls, individuals with BPD scored higher on all UPPS-p subscales except Sensation Seeking (e.g., Negative Urgency: 14 vs. 10, p < 0.001). Logistic regression identified Negative Urgency (OR = 5.31, 95% CI: 2.07–13.62, p = 0.001) and Positive Urgency (OR = 3.26, 95% CI: 1.37–7.75, p = 0.007) as independent predictors of BPD. Within the BPD group, depressive and anxiety symptoms correlated with several UPPS-P dimensions, notably Negative Urgency and Lack of Perseverance. Suicide attempts were associated with the DIB-R total score, BDI-II, and STAI-T, while substance use was linked to the DIB-R impulsivity subscale and STAI-T. Conclusions: Emotional impulsivity—particularly Negative Urgency—emerges as a central feature of BPD in emerging adulthood. Its interplay with depressive and anxiety symptoms, and its associations with suicidal and addictive behaviors, support a dual-level conceptualization of impulsivity as both a dispositional trait and a state-dependent clinical risk factor.
Full article
(This article belongs to the Special Issue (Recent Advances) Treating Psychiatry Disorders in Children and Adolescents: From Theory to Practice: 2nd Edition)
►▼
Show Figures

Figure 1
Open AccessArticle
Physician Empathy as Perceived by Parents of Children with Psychiatric Disorders: A Quantitative Analysis of Pediatric Consultations
by
Elisabeta-Oana Avram, Lavinia-Alexandra Moroianu, Cecilia Curis, Oana-Maria Isaila, Elena-Alexandra Bratu, Iulian Bounegru, Alexandru Paul Baciu and Eduard Drima
J. Clin. Med. 2025, 14(19), 7108; https://doi.org/10.3390/jcm14197108 - 9 Oct 2025
Abstract
Background: Clinician empathy is associated with family satisfaction and reduced anxiety, but quantitative data from the parents’ perspective in pediatric psychiatry are limited. Objective: To assess parent-perceived physician empathy in pediatric psychiatry consultations and explore its associations with clinical and demographic
[...] Read more.
Background: Clinician empathy is associated with family satisfaction and reduced anxiety, but quantitative data from the parents’ perspective in pediatric psychiatry are limited. Objective: To assess parent-perceived physician empathy in pediatric psychiatry consultations and explore its associations with clinical and demographic factors. Methods: Cross-sectional, consecutive sample of parents attending an outpatient pediatric psychiatry clinic (n = 163 parents). A 10-item behavioral empathy scale (range 10–40) was used. Analyses included reliability testing, group comparisons, correlations, OLS regression, and exploratory PCA. Results: The mean total empathy score was 34.5 (SD 4.2); most parents rated physicians as highly empathic (65%). Parents of children with ASD reported lower empathy compared to those with anxiety/depression. Empathy increased modestly with child age and was associated with a calmer state at the end of the visit. PCA suggested exploratory evidence of potential subdimensions, including child-centered communication and listening/facilitation. Conclusions: Parent-perceived empathy in this sample was generally high; however, behaviors that directly involve and facilitate the child (listening, encouraging questions) may need strengthening, particularly for children with ASD. Results should be interpreted in light of the single-center design, the absence of a recorded participation rate, parent-proxy reporting, and the exploratory nature of the PCA.
Full article
(This article belongs to the Special Issue Advances in Stigma and Discrimination in Pediatric Mental Health)
►▼
Show Figures

Figure 1
Open AccessSystematic Review
Beyond Racial Categorization in Sports Cardiology: A Systematic Review of Cardiac Adaptations in Athletes
by
Douglas Corsi, Rafael Hernandez, Jasmine Yimeng Bao, Stephen Garrova and David Shipon
J. Clin. Med. 2025, 14(19), 7107; https://doi.org/10.3390/jcm14197107 - 9 Oct 2025
Abstract
Background/Objectives: Race-based cardiac screening criteria in sports cardiology, including the “Black athlete’s heart” concept, assume biological distinctions that may not reflect physiological reality. This systematic review evaluates whether geographic ancestry provides more clinically relevant predictors of cardiac adaptation than racial categorization. Methods: PubMed
[...] Read more.
Background/Objectives: Race-based cardiac screening criteria in sports cardiology, including the “Black athlete’s heart” concept, assume biological distinctions that may not reflect physiological reality. This systematic review evaluates whether geographic ancestry provides more clinically relevant predictors of cardiac adaptation than racial categorization. Methods: PubMed was searched (January 2005–July 2025) for studies examining cardiac adaptations in athletes by ethnicity. Data extraction captured demographics, geographic origin, cardiac assessments, and outcomes. Narrative synthesis was employed due to methodological heterogeneity. Results: Forty-seven studies (n = 66,130) revealed substantial within-race heterogeneity. The “Black athlete repolarization variant” prevalence ranged from 1.8% (Brazilian) to 30% (Ghanaian) Black athletes. Left ventricular wall thickness >12 mm (normal <11 mm) occurred in 7.1% of Black versus 0.4% of White athletes, yet varied significantly within Black populations—10.8 ± 1.2 mm in Sub-Saharan versus 9.4 ± 1.1 mm in African-American athletes (p < 0.001). Relative wall thickness ≥0.44 (normal ≤0.42) was presented in 43% of West/Middle African, 23% of East African, and 7% of White athletes. T-wave inversion showed four-fold variation within Black populations (3.6–8.5% West African versus 0.5–2.0% African-American/Caribbean). Current International Criteria demonstrated inequitable specificity: 3.3% false-positive rate in Black versus 1.4% in White athletes. Conclusions: Geographic ancestry explains more cardiac variation than racial categories, supporting contemporary understanding of race as a sociopolitical construct. The persistent diagnostic disparities in ECG screening specificity highlight the need for reform. Transitioning toward protocols incorporating continental origin, anthropometric factors, and social determinants of health—while eliminating terminology like “Black athlete’s heart”—represents an important step toward achieving equity in cardiovascular care for diverse athletic populations.
Full article
(This article belongs to the Section Sports Medicine)
►▼
Show Figures

Figure 1
Open AccessReview
Optimizing Aesthetic Results in Implant-Based Breast Reconstruction: Patient Factors, Surgical Techniques, and Adjunctive Strategies
by
Elisa Bertulla and Edoardo Raposio
J. Clin. Med. 2025, 14(19), 7106; https://doi.org/10.3390/jcm14197106 - 9 Oct 2025
Abstract
Background: Breast reconstruction following mastectomy plays a crucial role in breast cancer management, restoring physical form and significantly impacting psychological well-being and quality of life. Implant-based breast reconstruction (IBBR) is the most performed technique worldwide due to its relative simplicity, shorter operative
[...] Read more.
Background: Breast reconstruction following mastectomy plays a crucial role in breast cancer management, restoring physical form and significantly impacting psychological well-being and quality of life. Implant-based breast reconstruction (IBBR) is the most performed technique worldwide due to its relative simplicity, shorter operative times, and avoidance of donor site morbidity. Achieving satisfactory aesthetic outcomes, however, remains challenging, as multiple factors—including patient characteristics, surgical technique, implant selection, timing of reconstruction, and adjuvant therapies—can influence the final appearance. Methods: Literature research was performed via PubMed, Scopus and Cochrane Library Database, focusing on studies examining aesthetic outcomes in implant-based breast reconstruction published between 2015 and 2025. Data on type of study, sample size, aesthetic evaluation methods, and duration of follow-up were collected and summarized. Results: Among 747 articles identified, only 25 articles fulfilled inclusion criteria, including mostly retrospective studies, but also prospective studies, randomized clinical trials, and reviews. Factors such as BMI, inframammary fold management, and implant selection were consistently reported to influence aesthetic outcomes. Surgical techniques including ADM use, axillary advancement sutures, hybrid reconstruction with fat grafting, and prepectoral implant placement were associated with improved patient satisfaction. Patient satisfaction often differs from surgeon-assessed outcomes, emphasizing the importance of subjective evaluation. Conclusions: Despite the heterogeneity and retrospective nature of many studies, evidence indicates that optimizing aesthetic outcomes in IBBR relies on careful patient selection, tailored surgical planning, and meticulous use of evidence-based techniques, including implant selection, flap-based support, and adjunctive strategies. Patient-reported outcomes are essential for evaluating success, and future research should focus on standardized outcome measures and prospective studies to further refine reconstructive approaches and maximize both cosmetic satisfaction and quality of life.
Full article
(This article belongs to the Special Issue Advances in Breast Reconstruction: New Technologies Improving Clinical Outcomes)
►▼
Show Figures

Figure 1
Open AccessArticle
Unraveling the Easix Score: Its Association with Vasopressor Need in Critically Ill Septic Pediatric Hematology–Oncology Patients
by
Lama Elbahlawan, Majd Khiami, Chad Blackshear, Saad Ghafoor, Alexandra Schaller, Sherry Johnson, Gabriela Maron, Raktima Datta, Amr Qudeimat and Jennifer McArthur
J. Clin. Med. 2025, 14(19), 7105; https://doi.org/10.3390/jcm14197105 - 9 Oct 2025
Abstract
Background: Sepsis is a common and serious complication in pediatric hematology oncology (PHO) patients. The Endothelial Activation and Stress Index (EASIX) score offers a potentially accessible tool for risk stratification in septic patients. Our objective was to evaluate the association of the
[...] Read more.
Background: Sepsis is a common and serious complication in pediatric hematology oncology (PHO) patients. The Endothelial Activation and Stress Index (EASIX) score offers a potentially accessible tool for risk stratification in septic patients. Our objective was to evaluate the association of the EASIX score with adverse clinical outcomes among septic PHO patients. Methods: A retrospective review was conducted for all PHO patients admitted to the intensive care unit (ICU) with sepsis from July 2022 to December 2024. Results: A total of 53 patients with 65 sepsis events were included in this analysis. The median age was 14.9 [IQR 9.9] y and the most common disease was hematologic malignancy. In our cohort, 60% needed vasopressors, 36% required invasive mechanical ventilation, and 22% underwent renal replacement therapy (RRT). Log2-EASIX > 2.5 was associated with higher vasopressor requirements (87% versus 45% in the low log2-EASIX group, p = 0.001) and an increased need for RRT (39% versus 12%, p = 0.024). Septic PHO patients with log2-EASIX > 2.5 were 6.9 times more likely to require vasopressor support [(95% CI 1.7–27.8) p = 0.007]. In addition, PHO patients with log2-EASIX > 2.5 had a longer ICU stay (7 d versus 2 d in the low log2-EASIX group, p = 0.024) and an extended overall hospitalization (33 d versus 25 d, p = 0.029). Conclusions: A higher EASIX score was associated with adverse outcomes in critically ill septic PHO patients. Our findings suggest that the EASIX score can be used as a tool for identifying septic patients at an increased risk of clinical deterioration and poor outcomes. Prospective studies in larger cohorts are warranted to validate and expand upon these findings.
Full article
(This article belongs to the Special Issue Clinical Advances in Pediatric Critical Care Medicine)
►▼
Show Figures
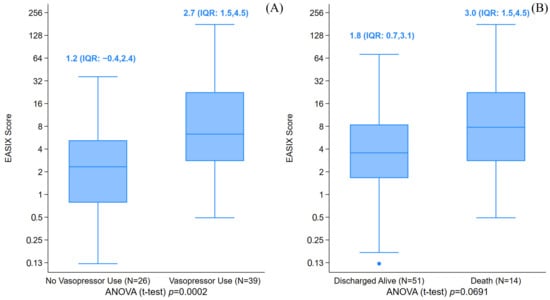
Figure 1
Open AccessReview
Hungry Bone Syndrome After Parathyroidectomy for Secondary Hyperparathyroidism: Pathogenesis and Contemporary Clinical Considerations
by
Adina Coman, Cristi Tarta, Marco Marian, Daian Ionel Popa, Sorin Olariu, Mihai Rosu, Diana Utu, Florina Buleu, Anca-Monica Macovei-Oprescu, Dorin Novacescu, Flavia Zara and Marius Murariu
J. Clin. Med. 2025, 14(19), 7104; https://doi.org/10.3390/jcm14197104 - 9 Oct 2025
Abstract
Secondary hyperparathyroidism (SHPT) in chronic kidney disease often necessitates parathyroidectomy (PTX), but this definitive treatment can precipitate hungry bone syndrome (HBS)—a profound, prolonged hypocalcemia caused by the rapid skeletal uptake of minerals after surgery. HBS results from the abrupt cessation of parathyroid hormone
[...] Read more.
Secondary hyperparathyroidism (SHPT) in chronic kidney disease often necessitates parathyroidectomy (PTX), but this definitive treatment can precipitate hungry bone syndrome (HBS)—a profound, prolonged hypocalcemia caused by the rapid skeletal uptake of minerals after surgery. HBS results from the abrupt cessation of parathyroid hormone (PTH)-driven bone resorption while bone formation continues, leading to intensive mineral deposition (mainly calcium) into chronically demineralized bone. Clinically, HBS ranges from asymptomatic biochemical disturbances to life-threatening hypocalcemia with tetany, seizures, and/or cardiac arrhythmias. This illustrative review synthesizes current knowledge of HBS pathogenesis and management in the context of SHPT. We detail how the high-turnover bone remodeling state of SHPT (osteitis fibrosa cystica) creates an expansive unmineralized osteoid pool that avidly mineralizes post-PTX. We also explore molecular mechanisms (e.g., RANKL/OPG dysregulation, Wnt/β-catenin activation, osteocyte-driven signals, and calcium-sensing receptor effects) that underpin this process. Key preoperative risk factors for HBS include very elevated PTH and alkaline phosphatase levels, large skeletal calcium deficits, younger patient age, and total PTX. We outline the typical postoperative course of HBS, phased from immediate acute hypocalcemia to a nadir and gradual recovery. Prevention and management strategies are emphasized, centered on vigilant monitoring and aggressive calcium and calcitriol supplementation, with preoperative optimization (e.g., vitamin D loading, calcimimetics) to mitigate severity. By enhancing risk stratification and perioperative care, clinicians can improve outcomes and safely navigate patients through this challenging complication of endocrine surgery.
Full article
(This article belongs to the Special Issue Endocrine Surgery: Current Developments and Trends)
►▼
Show Figures
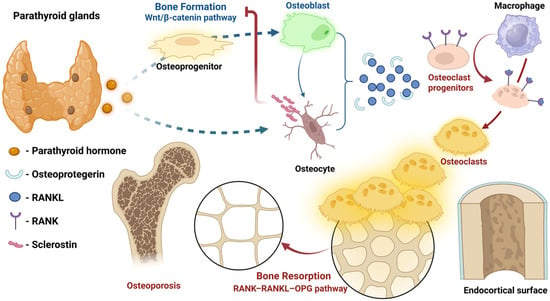
Figure 1
Open AccessArticle
Triple-Negative Apocrine Carcinoma: Largest Cohort Highlights Unique Biology and Survival Advantage
by
Tugba Basoglu, Ugur Ozkerim, Sila Oksuz, Oguzcan Kinikoglu, Sedat Yildirim, Sermin Kokten, Heves Surmeli, Deniz Isik, Ozlem Nuray Sever, Seval Ay Ersoy, Hatice Odabas and Nedim Turan
J. Clin. Med. 2025, 14(19), 7103; https://doi.org/10.3390/jcm14197103 - 9 Oct 2025
Abstract
Background/Objectives: Triple-negative breast cancer (TNBC) is a heterogeneous entity lacking ER, PR, and HER2, with aggressive biology and high recurrence risk. Neoadjuvant chemotherapy (NACT) is the standard of care, and a pathological complete response (pCR) is a surrogate marker for survival. Within
[...] Read more.
Background/Objectives: Triple-negative breast cancer (TNBC) is a heterogeneous entity lacking ER, PR, and HER2, with aggressive biology and high recurrence risk. Neoadjuvant chemotherapy (NACT) is the standard of care, and a pathological complete response (pCR) is a surrogate marker for survival. Within TNBC, apocrine differentiation (TNAC) is a distinct subtype, often androgen receptor (AR)-positive, with lower chemosensitivity but a favorable prognosis. Comparative studies of TNAC versus classical TNBC remain limited. This study aimed to define clinical and biological differences between TNAC and non-apocrine TNBC (NA-TNBC), representing the largest TNAC cohort to date. Methods: This retrospective study included 129 non-metastatic TNBC patients treated with NACT and surgery (2010–2020). Patients were classified as TNAC or NA-TNBC. Demographic, clinicopathological, and immunohistochemical data (including Ki-67 and AR) were collected. Tumor-infiltrating lymphocytes (TILs), delta Ki-67, pathological complete response (pCR), and survival outcomes were evaluated. Results: Of 129 TNBC patients, 45 (34.9%) were TNAC. AR positivity occurred in 64.4% of TNACs. TNAC patients were predominantly postmenopausal. pCR rates were significantly lower in TNAC (6.6% vs. 30.9%, p = 0.002). TNACs exhibited lower baseline Ki-67, delta Ki-67, and TIL positivity (13.3% vs. 30%). Despite this, 5-year overall survival was higher in TNAC (86% vs. 78%). Delta Ki-67 > 20% strongly predicted pCR across the cohort (p < 0.001). Carboplatin was rarely used in TNAC (8.3%), but was associated with a higher pCR rate (50% vs. 2.4%, p = 0.018). Conclusions: TNAC represents a biologically distinct TNBC subtype, characterized by low pCR but favorable survival. Recognition of its unique features may guide treatment de-escalation and exploration of AR-targeted therapies. Prospective studies focusing on TNAC are warranted.
Full article
(This article belongs to the Topic Triple-Negative Breast Cancer: Genetic Vulnerabilities and Emerging Targets for Precision Oncology)
►▼
Show Figures
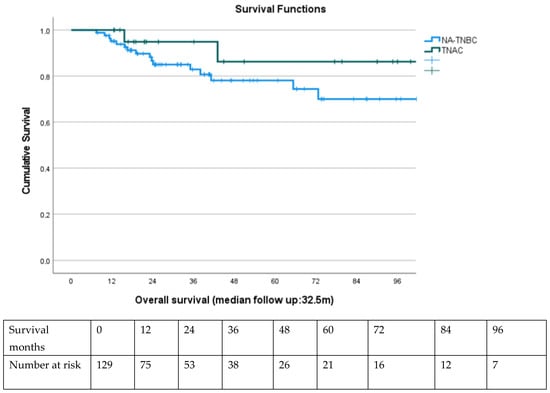
Figure 1
Open AccessReview
The Role of Inflammasomes in LPS and Gram-Negative Bacterial Sepsis
by
Eduardo Hernández-Cuellar, Kohsuke Tsuchiya, Oscar Medina-Contreras and Ricardo Valle-Ríos
J. Clin. Med. 2025, 14(19), 7102; https://doi.org/10.3390/jcm14197102 - 9 Oct 2025
Abstract
Background/Objectives: Sepsis is a life-threatening condition characterized by an uncontrolled immune response due to systemic infections. It is responsible for millions of deaths worldwide. Although inflammasomes play an important role in host defense, they have a detrimental role in sepsis induced by
[...] Read more.
Background/Objectives: Sepsis is a life-threatening condition characterized by an uncontrolled immune response due to systemic infections. It is responsible for millions of deaths worldwide. Although inflammasomes play an important role in host defense, they have a detrimental role in sepsis induced by LPS or Gram-negative bacteria. We aimed to revise the molecular mechanisms of inflammasome activation in sepsis by LPS and Gram-negative bacteria other than cytokine release as treatments blocking TNF-α and IL-1 cytokines have been ineffective even though cytokine storm is associated with lethality. Results: Studies with knockout mice deficient in inflammasome-derived cytokines have shown contrasting results on the role of these proinflammatory cytokines in the lethality of LPS- and Gram-negative-induced sepsis. However, DAMPs released after non-canonical inflammasome activation such as extracellular DNA, histones, HMGB1, and tissue factor result in disseminated-intravascular coagulation (DIC) and mortality in mice. Blocking these products in preclinical studies with animal models showed improved clinical scores and survival after LPS-induced sepsis or polymicrobial sepsis induced by Cecal Ligation and Puncture. Conclusions: Even though immunomodulatory drugs have shown inconclusive results as therapies for sepsis, blocking DAMPs associated with DIC may be considered for clinical trials in the future, especially in patients presenting biomarkers of coagulopathies.
Full article
(This article belongs to the Special Issue Sepsis: New Insights into Diagnosis and Treatment)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- JCM Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomedicines, Cancers, Current Oncology, Diagnostics, JCM
Advances in Magnetic Resonance Imaging (MRI) and Its Role in Radiation Therapy
Topic Editors: Indra J. Das, Minsong CaoDeadline: 31 October 2025
Topic in
Clinics and Practice, Cosmetics, JCM, Medicina, Dermato, LabMed, Psychology International
Advances in Psychodermatology
Topic Editors: Jacek C. Szepietowski, Andrzej JaworekDeadline: 30 November 2025
Topic in
Dentistry Journal, JCM, Materials, Biomedicines, Life
Medical and Dental Care, Photobiomodulation and Photomedicine
Topic Editors: Samir Nammour, Chukuka Samuel Enwemeka, Aldo Brugnera JuniorDeadline: 31 December 2025
Topic in
Applied Sciences, IJERPH, JCM, JPM, Technologies, Healthcare
Smart Healthcare: Technologies and Applications, 2nd Edition
Topic Editors: Gang Kou, Shuai Ding, Li Luo, Tian Lu, Yogesan KanagasingamDeadline: 20 January 2026

Conferences
Special Issues
Special Issue in
JCM
Endovascular Surgery: State of the Art and Clinical Perspectives
Guest Editors: Andrea Xodo, Francesco SquizzatoDeadline: 9 October 2025
Special Issue in
JCM
Oral and Maxillofacial Surgery: Recent Clinical Advances and Future Directions
Guest Editors: Funda Göker, Gianluca M. Tartaglia, Massimo Del FabbroDeadline: 10 October 2025
Special Issue in
JCM
New Insights into Physical Therapy
Guest Editors: Patsaki Irini, George KoumantakisDeadline: 10 October 2025
Special Issue in
JCM
New Insights into Diabetes and Cardiovascular Diseases
Guest Editor: Simona GiubilatoDeadline: 10 October 2025
Topical Collections
Topical Collection in
JCM
Coronavirus Disease 2019: Clinical Presentation, Pathogenesis and Treatment
Collection Editor: Vito Racanelli
Topical Collection in
JCM
Practice and Research in Clinical Pharmacology
Collection Editors: Antonio J. Carcas-Sansuán, Alberto M. Borobia Pérez
Topical Collection in
JCM
Pediatric and Adolescent Gynecology
Collection Editor: Panagiotis Christopoulos










