- Review
Transitional Care in Cardiorenal Patients: A Proposal for an Integrated Model
- Caterina Carollo,
- Alessandra Sorce and
- Giuseppe Mulè
- + 4 authors
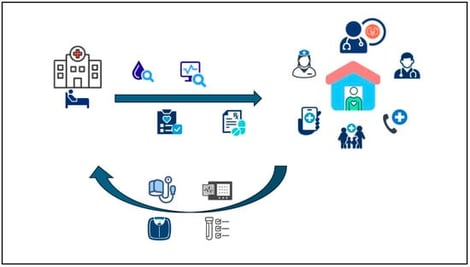
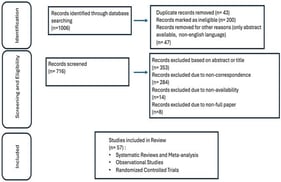
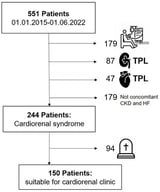
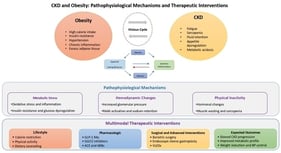
Heart failure (HF) and chronic kidney disease (CKD) are prevalent conditions in older adults, often coexisting and significantly increasing the risk of hospitalization, cardiovascular events, and mortality. Traditional hospital-based care, while essential for acute management, is often insufficient to ensure continuity of care and optimal long-term outcomes. Home-based care, although promising for improving quality of life and reducing hospital-acquired complications, faces challenges related to treatment adherence, monitoring, and caregiver support. Recent evidence highlights the potential of multidisciplinary, patient-centered care models integrating physicians, nurses, pharmacists, and family caregivers. Technological innovations, including telemedicine, remote monitoring, mobile health applications, and artificial intelligence, have shown efficacy in early detection of clinical deterioration, improving adherence, and reducing cardiovascular events in HF and CKD patients. Structured patient education, caregiver training, and proactive follow-up are key elements to optimize transitions from hospital to home and to improve long-term outcomes, including reduced rehospitalizations and better quality of life. Future care strategies should focus on personalized, integrated approaches that combine technology, education, and multidisciplinary collaboration to address the complex needs of HF and CKD patients, while mitigating healthcare costs and enhancing overall patient well-being.
1 January 2026