- Review
The Effects of Microplastics and Nanoplastics in the Nasal Airway and Upper Respiratory Tract
- Maayan S. Kahan,
- Benjamin S. Bleier and
- Mansoor M. Amiji
- + 1 author
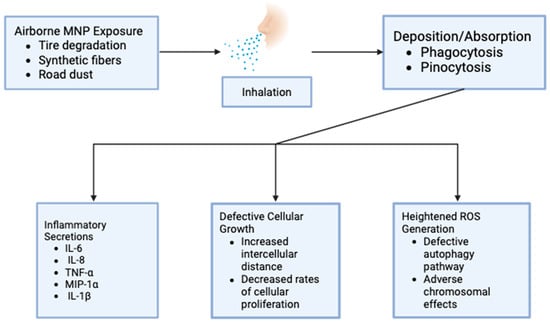
Environmental microplastic pollution is rising, and the recent literature reflects these conditions primarily by focusing on the effects of microplastics in the human lung and gut region. Despite the specific prevalence of airborne microplastics, the bulk of the existing literature neglects the point of initial contact of microplastics with the human body, namely the upper airway, specifically the nasal region. This review aims to highlight recent findings surrounding the effects of microplastics in the nose in both in vitro and clinical models. Areas of particular interest include changes in cell morphology, microplastic permeation, cytotoxicity, and inflammatory effects. Although permeation and toxicity findings vary across studies, the literature collectively indicates hazards to cellular health and potential impacts on patient quality of life.
22 December 2025