Advances in Anti-Cancer Drugs
Topic Information
Dear Colleagues,
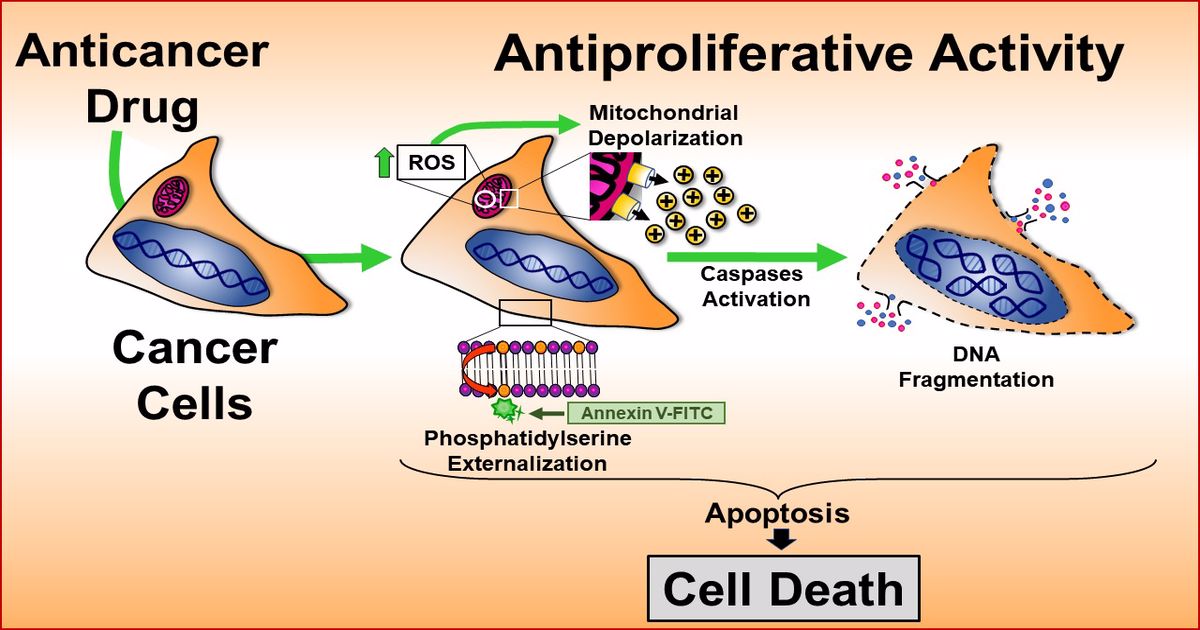
We hope this message finds you well. As large quantities of novel synthetic and natural molecules continue to be generated or discovered, there is challenging to identify and characterize therapeutic agents with effective anti-cancer activity. The aim of this particular Topic, "Advances in Anti-Cancer Drugs”, pretends aims to collect a group of publications focused on novel chemical compounds with cytotoxic activity on cancer cells in vitro, in vivo, or both, and particularly those articles including novel biomarkers and target proteins with potential therapeutic properties. In addition, studies on drug repurposing, including approved, discontinued, and shelved drugs, with anti-cancer activity, are encouraged for submission. Moreover, immunotherapy, electrochemotherapy, gene therapy, and phytomedicine studies are highly welcome. The submitted manuscripts should include the partial mechanism used for the novel compounds or strategies to induce cell death. This Topic provides a suitable platform to disseminate anti-cancer discoveries at the bench and the bedside. Thus, we are delighted to invite you for an excellent opportunity to publish your manuscript in our journal.
Dr. Armando Varela-Ramirez
Dr. Elisa Robles-Escajeda
Dr. Blanca E. Ruiz-Medina
Dr. Patricia Talamás-Rohana
Dr. Rachid Skouta
Topic Editors
Keywords
- anticancer
- antiproliferation
- apoptosis
- biomarkers
- cell cycle
- cell signaling
- drug discovery
- immunotherapy, gene therapy
- phytomedicine