-
 Towards Cervical Cancer Elimination: Insights from an In-Depth Regional Review of Patients with Cervical Cancer
Towards Cervical Cancer Elimination: Insights from an In-Depth Regional Review of Patients with Cervical Cancer -
 Advances in Screening, Immunotherapy, Targeted Agents, and Precision Surgery in Cervical Cancer: A Comprehensive Clinical Review (2018–2025)
Advances in Screening, Immunotherapy, Targeted Agents, and Precision Surgery in Cervical Cancer: A Comprehensive Clinical Review (2018–2025) -
 Reawakening Differentiation Therapy in Acute Myeloid Leukemia: A Comprehensive Review of ATRA-Based Combination Strategies
Reawakening Differentiation Therapy in Acute Myeloid Leukemia: A Comprehensive Review of ATRA-Based Combination Strategies -
 Metastasis-Free Survival in Patients with Biochemical Recurrence After Robot-Assisted Radical Prostatectomy: A Multicenter, Retrospective Cohort Study in Japan (MSUG94 Group)
Metastasis-Free Survival in Patients with Biochemical Recurrence After Robot-Assisted Radical Prostatectomy: A Multicenter, Retrospective Cohort Study in Japan (MSUG94 Group)
Journal Description
Current Oncology
Current Oncology
is an international, peer-reviewed, open access journal that since 1994 represents a multidisciplinary medium for clinical oncologists to report and review progress in the management of this disease, and published monthly online by MDPI (from Volume 28, Issue 1 - 2021). The Canadian Association of Medical Oncologists (CAMO), Canadian Association of Psychosocial Oncology (CAPO), Canadian Association of General Practitioners in Oncology (CAGPO), Cell Therapy Transplant Canada (CTTC) and others are affiliated with Current Oncology and their members receive discounts on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Oncology)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 22.8 days after submission; acceptance to publication is undertaken in 2.6 days (median values for papers published in this journal in the second half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Clusters of Oncology: Cancers, Current Oncology, Onco and Targets.
Impact Factor:
3.4 (2024);
5-Year Impact Factor:
3.3 (2024)
Latest Articles
Urachal Signet Ring Cell Carcinoma: A Clinicopathological Analysis of 28 Cases
Curr. Oncol. 2026, 33(3), 153; https://doi.org/10.3390/curroncol33030153 (registering DOI) - 7 Mar 2026
Abstract
Background: Urachal carcinoma is a rare malignancy comprising less than 1% of all bladder cancers. The signet-ring cell subtype is particularly aggressive and poses significant diagnostic and therapeutic challenges. Methods: A retrospective review of urachal carcinoma cases from 1989 to 2023 was
[...] Read more.
Background: Urachal carcinoma is a rare malignancy comprising less than 1% of all bladder cancers. The signet-ring cell subtype is particularly aggressive and poses significant diagnostic and therapeutic challenges. Methods: A retrospective review of urachal carcinoma cases from 1989 to 2023 was conducted using data from BC Cancer and MD Anderson Cancer Center. The study analyzed 75 patients, including 28 signet-ring cell carcinoma (SRCC) cases and a control group of 47 non-SRCC cases, to compare survival patterns, treatment outcomes, and histopathological features. Results: Clinically, the SRCC subtype was associated with advanced stage at presentation (pT3/pT4) and a higher recurrence rate (82% vs. 53%; p = 0.01). Survival analysis demonstrated worse outcomes for the SRCC cohort, with a five-year cancer-specific survival (CSS) of 39% compared to 64% in the non-signet group (p = 0.053). Partial cystectomy remained the primary surgical approach for both cohorts. Adjuvant chemotherapy was administered more often in SRCC cases (86% vs. 47%). Conclusions: By providing a comprehensive multi-institutional analysis, this study establishes urachal SRCC as a distinct clinical entity with a strong independent prognostic significance. Despite aggressive multimodal management, it carries a poorer prognosis compared to urachal non-SRCC, emphasizing the need for subtype-specific therapeutic guidelines.
Full article
(This article belongs to the Section Genitourinary Oncology)
►
Show Figures
Open AccessArticle
Real-World Treatment Patterns and Survival in Patients with ROS1-Positive Advanced Non-Small Cell Lung Cancer in Canada and Europe
by
Winson Y. Cheung, Adam Lee, Helena Bote de Cabo, Kathrin Burdenski, Petros Christopoulos, Bárbara Pinto-Correia, Simon Deshayes, Nicolas Girard, Pooja Hindocha, Áine Madden, Marta Mella, Joana Moreira, Silvia Rizzi, Delvys Rodríguez Abreu, Marta Soares, Joseph Thomas, Maria Han, Christophe Y. Calvet, Gabrielle Emanuel, Mrudula B. Glassberg, Hazel Jacobs, Caroline Rault, Yong Yuan and Christos Chouaidadd
Show full author list
remove
Hide full author list
Curr. Oncol. 2026, 33(3), 152; https://doi.org/10.3390/curroncol33030152 - 6 Mar 2026
Abstract
Real-world data on patients with ROS1-positive advanced non-small cell lung cancer (NSCLC) remain scarce. In this descriptive observational retrospective cohort study, we describe characteristics, treatments, and real-world progression-free survival (rwPFS) and overall survival (OS) among patients with ROS1-positive advanced NSCLC (de
[...] Read more.
Real-world data on patients with ROS1-positive advanced non-small cell lung cancer (NSCLC) remain scarce. In this descriptive observational retrospective cohort study, we describe characteristics, treatments, and real-world progression-free survival (rwPFS) and overall survival (OS) among patients with ROS1-positive advanced NSCLC (de novo or recurrent) using secondary data pooled from clinical sites in Canada, France, Germany, Portugal, and Spain as part of the Oncology Evidence Network. Site-specific patient inclusion periods occurred between 2009 and 2023, with follow-up to 2024, allowing ≥1 year of potential follow-up at each site. In total, 108 patients were included, with most (n = 105; 97.2%) having a de novo diagnosis of advanced NSCLC. 103 patients (95.4%) received ≥1 line of systemic anticancer therapy (SACT), of which 65 (63.1%) received first-line targeted therapy, mostly crizotinib monotherapy (n = 45) or crizotinib-based regimens (n = 10), with a median (95% CI) rwPFS and OS of 14.0 (8.3–19.8) and 47.9 (27.3–not estimable) months, respectively. Thirty-eight of the 103 SACT-treated patients (36.9%) received first-line non-targeted therapy, mostly platinum-based chemotherapy (n = 26); median (95% CI) rwPFS and OS were 9.0 (7.5–11.0) and 29.3 (17.7–65.7) months, respectively. Results from this study indicated a tendency for longer survival using currently available ROS1-targeted versus non-targeted therapy for patients with ROS1-positive advanced NSCLC. Nevertheless, survival outcomes were limited, highlighting the importance of more effective emerging treatments for ROS1-positive disease.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Artificial Intelligence in Prostate MRI: Comparison of an AI-Based Software and an Experienced Radiologist for Detecting Clinically Significant Prostate Cancer
by
Roberto Castellana, Simona Marzi, Andrea Russo, Maria Consiglia Ferriero, Irene Terrenato, Eugenia Papaleo, Giuseppe Navanteri, Davide Vitale, Giuseppe Pizzi, Antonello Vidiri and Luca Bertini
Curr. Oncol. 2026, 33(3), 151; https://doi.org/10.3390/curroncol33030151 - 6 Mar 2026
Abstract
Background: Multiparametric MRI is central to detecting clinically significant prostate cancer (csPCa), but diagnostic accuracy depends on reader experience. Artificial intelligence (AI) tools may support prostate MRI interpretation and reduce inter-reader variability. This study compared the detection rate of a trial, non-commercial version
[...] Read more.
Background: Multiparametric MRI is central to detecting clinically significant prostate cancer (csPCa), but diagnostic accuracy depends on reader experience. Artificial intelligence (AI) tools may support prostate MRI interpretation and reduce inter-reader variability. This study compared the detection rate of a trial, non-commercial version an AI-based software (PAROS) with that of an experienced radiologist. Methods: This retrospective single-center study included 150 patients who underwent prostate MRI followed by combined systematic and MRI-targeted transperineal biopsy. MRI examinations were interpreted by an experienced radiologist according to PI-RADS v2.1 and independently analyzed using a precommercial trial version of PAROS operating on biparametric MRI. Histopathology served as the reference standard. Detection rate was evaluated using sensitivity, specificity, and positive and negative likelihood ratios (PLR and NLR) at PI-RADS thresholds ≥3 and ≥4. Results: CsPCa was present in 63.3% of patients. At both PI-RADS thresholds, PAROS and the radiologist showed comparable sensitivity and specificity, wuth extremely low NLRs, indicating excellent rule-out capability. PLRs were modest and similar at PI-RADS ≥ 3 (1.26 vs. 1.42) and 1.88 for both at PI-RADS ≥ 4. PAROS detected more lesions, particularly in the transition zone. Conclusions: PAROS achieved csPCa detection comparable to an experienced radiologist, supporting its role as a decision-support tool in prostate MRI interpretation.
Full article
(This article belongs to the Special Issue New and Emerging Trends in Prostate Cancer)
►▼
Show Figures

Figure 1
Open AccessArticle
Scientific Meetings in Medical Oncology: Are We Facing a Time- and Resource-Consuming Plethora?
by
Vittorio Gebbia, Dario Piazza, Fabrizio Scrima, Alessia Passanisi, Daniela Sambataro, Giuseppa Scandurra and Maria Rosaria Valerio
Curr. Oncol. 2026, 33(3), 150; https://doi.org/10.3390/curroncol33030150 - 5 Mar 2026
Abstract
►▼
Show Figures
Background: In recent years, the rapid advances in molecular biology and cancer pathophysiology, and the rapid availability of new therapeutic agents, have led to an exponential increase in the number of medical oncology conferences. This plethora may partly result from excessive duplication,
[...] Read more.
Background: In recent years, the rapid advances in molecular biology and cancer pathophysiology, and the rapid availability of new therapeutic agents, have led to an exponential increase in the number of medical oncology conferences. This plethora may partly result from excessive duplication, undertaken without scientific or updating aims, under pressure from sponsors or other motivations unrelated to scientific advancement. The quality of meetings is therefore to be analyzed. Methods: A panel of medical oncologists, psychologists, and health-related data managers reviewed the characteristics of 99 out of 125 medical oncology conferences. The meetings were assessed for quality using a 0–5 score based on five parameters: attendees-to-speaker ratio, speaker quality, adequate time allocated for discussion, availability of feedback, and fairness of speeches. Results: The panelists identified 25 of 99 scientific events (25%; 95% CI 17–35%) at the 75th percentile and classified them as high-tier meetings, with a total score of 4–5. There were 5 national conferences, 6 regional conferences, and 14 local conferences. Forty-five meetings (56%; 95%Cl 35–56%) reached a score of 0–2 and twenty-nine (29%; 95%Cl 21–39%) a score of 3, and all were considered low tiers. This difference was statistically significant (p = 0.002709) in favor of high-titer national conferences. Conclusions: Although this paper has several limitations, the results indicate that many conferences were of moderate to poor quality, with a significant prevalence of low-tier events at regional and local levels and a higher concentration of low-tier events within this group. Scientific societies should implement adequate countermeasures.
Full article

Graphical abstract
Open AccessArticle
Higher Dose Irradiation for Malignant Spinal Cord Compression: Long-Term Results of the RAMSES-01 Trial
by
Dirk Rades, Darejan Lomidze, Natalia Jankarashvili, Fernando Lopez Campos, Arturo Navarro-Martin, Barbara Segedin, Blaz Groselj, Charlotte Kristiansen, Kristopher Dennis and Jon Cacicedo
Curr. Oncol. 2026, 33(3), 149; https://doi.org/10.3390/curroncol33030149 - 4 Mar 2026
Abstract
Despite the increasing popularity of upfront decompressive surgery, there are still patients with malignant spinal cord compression (MSCC) and expected longer-term survival receiving irradiation alone. In these patients, local progression-free survival (LPFS) may be improved with doses beyond the commonly applied regimen of
[...] Read more.
Despite the increasing popularity of upfront decompressive surgery, there are still patients with malignant spinal cord compression (MSCC) and expected longer-term survival receiving irradiation alone. In these patients, local progression-free survival (LPFS) may be improved with doses beyond the commonly applied regimen of 10 × 3.0 Gy. A prospective phase 2 trial (RAMSES-01) investigated the benefit of two regimens, 15 × 2.633 and 18 × 2.333 Gy, compared with a 10 × 3.0 Gy (historical control). Patients in the phase 2 cohort had significantly better local progression-free survival (LPFS) after 1 year. Since recurrent MSCC-related motor weakness is a serious situation, it must be avoided as long as possible. In this respect, it is important to know whether the superiority of 15 × 2.633 and 18 × 2.333 Gy found in the RAMSES-01 trial still exists after 2 or 3 years. This led to the current study. In the phase 2 group, 2- and 3-year LPFS rates were 93.1% and 93.1%, respectively, and survival rates were 54.2% and 36.1%, respectively. According to propensity-adjusted Cox regression analyses, radiotherapy regimens in the phase 2 cohort resulted in significantly better LPFS at 2 (p = 0.017) and 3 (p = 0.013) years. In contrast, survival was not significantly different (p = 0.251 and p = 0.288, respectively). Radiation myelopathy and pathologic vertebral fractures were not observed in any group. Given the limitations of this study, irradiation 15 × 2.633 or 18 × 2.333 Gy may be an alternative option for patients with MSCC and longer expected survival treated with irradiation alone.
Full article
(This article belongs to the Special Issue Innovations in Patient-Centred Palliative Radiotherapy in Oncology: From Clinical Trials to Real-World Practice)
►▼
Show Figures

Figure 1
Open AccessReview
Unlocking KRAS: Navigating Its Molecular Biology and Treatment Landscape Among Gastrointestinal Malignancies
by
Austin Frisch, Eric Martin, Timothy Cannon, Raymond Wadlow, Srivatsan Raghavan, Triparna Sen and Nagla Abdel Karim
Curr. Oncol. 2026, 33(3), 148; https://doi.org/10.3390/curroncol33030148 - 3 Mar 2026
Abstract
KRAS-targeted therapy has opened new doors in the world of oncology, and many trials are underway for KRAS specific treatments for gastrointestinal (GI) malignancies. Outlining the current state of KRAS therapy and the remaining research gaps pertaining to these deadly cancers is
[...] Read more.
KRAS-targeted therapy has opened new doors in the world of oncology, and many trials are underway for KRAS specific treatments for gastrointestinal (GI) malignancies. Outlining the current state of KRAS therapy and the remaining research gaps pertaining to these deadly cancers is crucial for the development of future therapeutics. In this review, we focus on the relationship between KRAS and GI malignancies. Current therapies are discussed with an in-depth exploration of the KRAS gene and how it connects to pancreatic, colorectal and other GI malignancies. Promising clinical trials and future therapies are highlighted while discussing the molecular biology behind them. Specifically, trials focusing on upcoming KRAS on and off inhibitors in development as well as variant focused inhibitors targeting the more common mutations G12D and G12V. We discuss exciting new pan/multi KRAS inhibitors that have been successful in pre-clinical trials. More unique therapeutic options include KRAS T cell therapies, vaccines, and combination strategies with immunotherapy. Furthermore, we address the difficulties with KRAS therapy, and the potential future directions needed to overcome them. An in-depth current literature review was done along with a review of the active clinical trials for KRAS-targeted therapeutics involving GI malignancies.
Full article
(This article belongs to the Special Issue Therapeutic Studies from Pre-Clinical to Clinical (Phase I–IV) for Gastrointestinal Cancers)
►▼
Show Figures

Figure 1
Open AccessReview
Molecular Mechanisms of Juvenile Nasopharyngeal Angiofibroma: A Narrative Review
by
Xingchen Liu, Junying Hu, Weigang Gan, Feng Liu and Bing Zhong
Curr. Oncol. 2026, 33(3), 147; https://doi.org/10.3390/curroncol33030147 - 3 Mar 2026
Abstract
►▼
Show Figures
Juvenile nasopharyngeal angiofibroma (JNA), a rare vascular tumor in adolescent males, involves dysregulated angiogenesis and hormonal interplay. Key molecular drivers include HIF-1α, VEGF, bFGF, and β-catenin, promoting tumor growth via pathways like Wnt/β-catenin and Ras signaling. Androgens and estrogen modulate progression, though mechanisms
[...] Read more.
Juvenile nasopharyngeal angiofibroma (JNA), a rare vascular tumor in adolescent males, involves dysregulated angiogenesis and hormonal interplay. Key molecular drivers include HIF-1α, VEGF, bFGF, and β-catenin, promoting tumor growth via pathways like Wnt/β-catenin and Ras signaling. Androgens and estrogen modulate progression, though mechanisms remain debated. Targeted therapies reduce tumor proliferation and vascularity in preclinical studies, yet clinical translation is hindered by drug resistance and inconsistent biomarker expression. Hormonal and MMP-targeted approaches also show potential but require validation. This review consolidates JNA’s molecular landscape, emphasizing the need for personalized strategies, biomarker refinement, and combination therapies to improve therapeutic outcomes for this challenging tumor.
Full article

Graphical abstract
Open AccessArticle
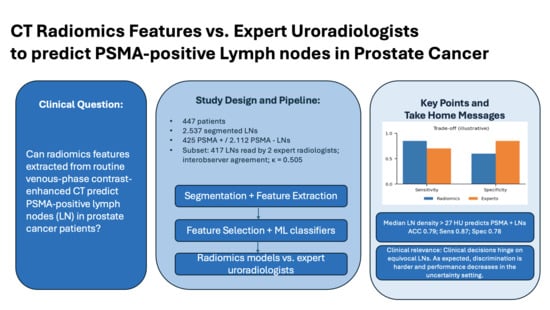
CT Radiomics Models Did Not Outperform Experts in Predicting [68Ga]Ga-PSMA-PET Positivity in Prostate Cancer Lymph Node Staging
by
Thula Cannon Walter-Rittel, Boris Gorodetski, Alexander Hartenstein, Julian Rogasch, Imke Schatka, Holger Amthauer, Marcus Makowski, Charlie Alexander Hamm and Tobias Penzkofer
Curr. Oncol. 2026, 33(3), 146; https://doi.org/10.3390/curroncol33030146 - 2 Mar 2026
Abstract
Background: The use of [68Ga]Ga-PSMA-PET/CT for prostate cancer (PCa) staging is limited by cost and availability. This study evaluates whether radiomic features from contrast-enhanced (CE) CT can predict PSMA-positive lymph nodes (LNs) as a surrogate for metastasis. Methods: A
[...] Read more.
Background: The use of [68Ga]Ga-PSMA-PET/CT for prostate cancer (PCa) staging is limited by cost and availability. This study evaluates whether radiomic features from contrast-enhanced (CE) CT can predict PSMA-positive lymph nodes (LNs) as a surrogate for metastasis. Methods: A retrospective study of 447 patients included 2537 segmented LNs (425 PET-positive, 2112 PET-negative). Two uroradiologists assessed 417 LNs on CE-CT using a four-point Likert scale. Radiomic features were extracted, selected using four algorithms, and analyzed with six model-building methods. Model performance was compared to radiologist ratings. Results: Radiomic models achieved an accuracy of 0.77–0.85, sensitivity of 0.85–0.91, and specificity of 0.74–0.85. Compared to radiologists, models had higher NPV (0.97–0.98 vs. 0.96) and sensitivity (0.85–0.91 vs. 0.76), but radiologists had superior accuracy (0.95 vs. 0.77–0.85) and specificity (0.97–0.98 vs. 0.74–0.85). In a subanalysis of LNs rated as probably benign or malignant, expert radiologists outperformed the algorithm with greater specificity and PPV (p < 0.005). A density threshold of >27 HU predicted PSMA-positive LNs with 0.79 accuracy, 0.87 sensitivity, and 0.78 specificity. Conclusions: While radiomics did not outperform expert radiologists, the single first-order parameter CT density >27 HU was predictive of PSMA-positive LNs. Clinical Relevance Statement: Radiomic models did not outperform expert uroradiologists. However, in high-volume or resource-limited settings lacking access to [68Ga]Ga-PSMA-PET/CT, they may help improve LN assessment in PCa patients with CT alone.
Full article
(This article belongs to the Special Issue AI-Powered Oncologic Nuclear Medicine in Clinical Translation: Advanced Assessment of Tumor Load and Microenvironment)
►▼
Show Figures
Graphical abstract
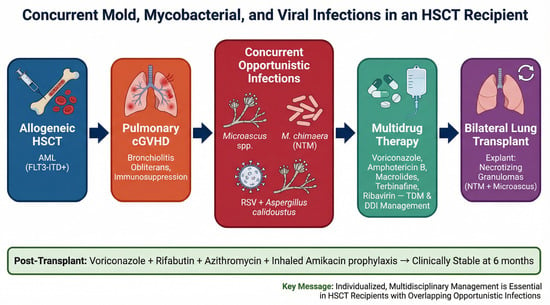
Open AccessCase Report
Concurrent Mold, Mycobacterial, and Viral Infections in a Hematopoietic Stem Cell Transplant Recipient Undergoing Lung Transplantation for Graft-Versus-Host Disease
by
Layan Akkielah, Wayne Leung, Serena Wang, Lili Ataie, Anargyros Xenocostas, Asma Syed, Ying-Han R. Hsu, Michael Silverman, Fatimah AlMutawa and MohammadReza Rahimi Shahmirzadi
Curr. Oncol. 2026, 33(3), 145; https://doi.org/10.3390/curroncol33030145 - 2 Mar 2026
Abstract
Hematopoietic stem cell transplant (HSCT) recipients are at high risk for opportunistic infections due to profound immunosuppression and graft-versus-host disease (GvHD). Molds and nontuberculous mycobacteria (NTM) pose diagnostic and therapeutic challenges, especially when infections overlap. A 42-year-old woman with prior allogeneic HSCT for
[...] Read more.
Hematopoietic stem cell transplant (HSCT) recipients are at high risk for opportunistic infections due to profound immunosuppression and graft-versus-host disease (GvHD). Molds and nontuberculous mycobacteria (NTM) pose diagnostic and therapeutic challenges, especially when infections overlap. A 42-year-old woman with prior allogeneic HSCT for acute myeloid leukemia (AML) developed pulmonary infections with Microascus spp. and Mycobacterium chimaera, later complicated by Aspergillus calidoustus and RSV infection. Initial therapy included voriconazole, amphotericin B, and a macrolide-based multidrug regimen for NTM. Modifications were required for drug resistance and hepatotoxicity. Despite partial response, recurrent fungal infection necessitated prolonged antifungal therapy, including adjunctive inhaled amphotericin B and terbinafine. Ultimately, progressive bronchiolitis obliterans prompted bilateral lung transplantation. Explant pathology revealed necrotizing granulomas positive for NTM and Microascus spp. Post-transplant prophylaxis with voriconazole, rifabutin, azithromycin, and inhaled amikacin prevented recurrence, and the patient remained clinically stable at 6-month follow-up. This case illustrates the complexity of managing overlapping mold and NTM infections in HSCT recipients, highlighting the need for individualized, multidisciplinary care. Therapeutic drug monitoring, careful adjustment for drug–drug interactions, and the use of adjunctive inhaled antifungals were critical to achieving a favorable outcome.
Full article
(This article belongs to the Section Hematology)
►▼
Show Figures
Graphical abstract
Open AccessArticle
PD-L1 Negative Advanced Non-Small Cell Lung Cancer: Practice Patterns and Real-World Outcomes
by
Audrey-Ann Bégin, Maude Dubé-Pelletier, Catherine Labbé, Vicky Mai, Michaël Maranda-Robitaille and Marie-Hélène Denault
Curr. Oncol. 2026, 33(3), 144; https://doi.org/10.3390/curroncol33030144 - 28 Feb 2026
Abstract
The standard first-line treatment for metastatic non-small cell lung cancer (NSCLC) without oncogenic alterations and programmed death-ligand 1 (PD-L1) expression < 1% is a combination of chemotherapy (CT) and immunotherapy (IO). However, real-world overall survival (OS) appears more modest than in clinical trials,
[...] Read more.
The standard first-line treatment for metastatic non-small cell lung cancer (NSCLC) without oncogenic alterations and programmed death-ligand 1 (PD-L1) expression < 1% is a combination of chemotherapy (CT) and immunotherapy (IO). However, real-world overall survival (OS) appears more modest than in clinical trials, averaging 10–13 months. This retrospective study aimed to assess treatment patterns and real-world outcomes at the Institut universitaire de cardiologie et de pneumologie de Québec (IUCPQ). Patients diagnosed between January 2019 and December 2023 with advanced PD-L1 <1% NSCLC and treated with palliative intent at IUCPQ were included and categorized by first-line treatment. Progression-free survival (PFS) and OS of the CT + IO and CT groups were compared using Kaplan–Meier curves and Cox regression analyses. Data regarding regimen selection, adverse events and subsequent treatment lines were collected. Among 217 eligible patients, 82 (37.8%) received CT + IO, 32 (14.7%) CT alone, 16 (7.4%) targeted therapy, and 87 (40.1%) supportive care. Median PFS was 5.3 vs. 4.7 months (p = 0.5) and OS 14.4 vs. 13.5 months (p = 0.2) for CT + IO and CT alone, respectively. In the CT + IO group, treatment discontinuation was mainly due to disease progression (59.4%) or adverse events (36.2%). Immune-related adverse events occurred in 29.3%, most frequently pneumonitis (8.5%). Therefore, in this cohort, no statistically significant survival difference was observed between CT + IO and CT alone. However, these findings should be interpreted cautiously given the non-randomized design, baseline imbalances between groups, and the limited sample size of the CT alone cohort. Tolerability of CT + IO was consistent with that observed in clinical trials.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures

Figure 1
Open AccessReview
The Rising Power of Electrochemotherapy in Musculoskeletal Oncology
by
Nicolas Papalexis, Giuliano Peta, Simone Quarchioni, Laura Campanacci, Alessandro Gasbarrini, Giuseppe Tedesco, Michela Carta, Maddalena Di Carlo, Marco Miceli and Giancarlo Facchini
Curr. Oncol. 2026, 33(3), 143; https://doi.org/10.3390/curroncol33030143 - 28 Feb 2026
Abstract
Electrochemotherapy is a minimally invasive treatment based on the principle of reversible electroporation of target cells in pathologic tissues in order to increase the local effect of chemotherapeutic agents. The mechanism of action relies on temporarily increasing cell permeability to increase the uptake
[...] Read more.
Electrochemotherapy is a minimally invasive treatment based on the principle of reversible electroporation of target cells in pathologic tissues in order to increase the local effect of chemotherapeutic agents. The mechanism of action relies on temporarily increasing cell permeability to increase the uptake of cytotoxic drugs in the intracellular space. Originally developed for the treatment of cutaneous malignancies, electrochemotherapy has significantly evolved over the past few decades, thanks to advancements in electrode design and image guidance, finding fertile ground in musculoskeletal oncological pathologies, such as bone and soft tissue tumors and different kinds of vascular malformations. Moreover, initial experiences have reported on the treatment of other soft tissue tumors such as desmoid fibromatosis. The aim of this review is to summarize the literature on the role of electrochemotherapy across a variety of musculoskeletal conditions, starting from established oncologic indications, such as metastatic bone or soft tissue tumors, to emerging evidence on primary musculoskeletal pathology, with particular attention paid to the results of the leading studies relating to the efficacy, complications, and recurrence rate.
Full article
(This article belongs to the Section Bone and Soft Tissue Oncology)
►▼
Show Figures
Figure 1
Open AccessArticle
Exploring the Impact of Gender and Income on Concerns Reported by Cancer Survivors Aged ≥85 Years in Canada: A Secondary Analysis of the Canadian Transitions Survey
by
Lorelei Newton, Irene Nicoll, Fay J. Strohschein and Margaret I. Fitch
Curr. Oncol. 2026, 33(3), 142; https://doi.org/10.3390/curroncol33030142 - 28 Feb 2026
Abstract
This study describes concerns, positive experiences and suggestions for improvement in survivorship care from the perspectives of cancer survivors aged ≥85 years based on gender and income levels. A national Canadian survey was conducted in 2016 focusing on cancer survivors’ needs and experiences
[...] Read more.
This study describes concerns, positive experiences and suggestions for improvement in survivorship care from the perspectives of cancer survivors aged ≥85 years based on gender and income levels. A national Canadian survey was conducted in 2016 focusing on cancer survivors’ needs and experiences with follow-up care after treatment. This paper reports a secondary analysis drawn from the survey data reported qualitatively. In total, 581 respondents aged ≥85 years responded, of which 399 confirmed gender and annual household income. Within this group, 201 were male, and 198 were female. Two-thirds of the males (n = 134 males, 66.7%) and 80.8% of the females (n = 160) reported annual household income under $50K (CAD). Limited differences were noted between survivors’ responses according to sex and/or income levels. Concerns focused on physical challenges and body changes. Positive comments reflected appreciation of the care provided by attentive healthcare professionals. Suggestions for improvement addressed the need for improved person-centred care and availability of services for older adults. The survivors faced a range of physical, emotional and practical challenges following cancer treatment. The study highlights the importance of considering how living alone or with others, community connection, and the burden of co-morbidities compounding physical challenges after cancer intersect to create unique situations for this age group.
Full article
(This article belongs to the Section Oncology Nursing)
Open AccessReview
Systemic Treatment for Hepatocellular Carcinoma Recurrence After Liver Transplantation
by
Chiara Mazzarelli, Francesco Berardi, Alessandra Bonfichi, Marina Clemente, Michele Orlando, Marina Strollo and Luca Saverio Belli
Curr. Oncol. 2026, 33(3), 141; https://doi.org/10.3390/curroncol33030141 - 28 Feb 2026
Abstract
Hepatocellular carcinoma (HCC) is a leading cause of cancer-related mortality worldwide, and liver transplantation (LT) remains the only curative treatment addressing both tumor burden and underlying liver disease. Despite an adequate candidate selection, HCC recurrence after LT occurs in 8–20% of cases and
[...] Read more.
Hepatocellular carcinoma (HCC) is a leading cause of cancer-related mortality worldwide, and liver transplantation (LT) remains the only curative treatment addressing both tumor burden and underlying liver disease. Despite an adequate candidate selection, HCC recurrence after LT occurs in 8–20% of cases and is associated with a poor prognosis, particularly in patients who experience an early relapse. The management of HCC recurrence remains particularly challenging due to the lifelong immunosuppression required after LT, which may promote tumor progression and restrict therapeutic options. This review synthesizes the current evidence on systemic therapies for recurrent HCC after LT, focusing on tyrosine kinase inhibitors (TKIs), immunotherapy, and the current available immunosuppression strategies. Unfortunately, in this setting, robust prospective studies are lacking, and clinical decision-making remains based on retrospective data and expert consensus. Future research should prioritize the prospective evaluation of systemic regimens, integration of immunosuppression modulation, and careful exploration of immunotherapy or new target therapies in this special population.
Full article
(This article belongs to the Special Issue Systemic Therapy in Hepatocellular Carcinoma: Current Challenges and Future Directions)
►▼
Show Figures
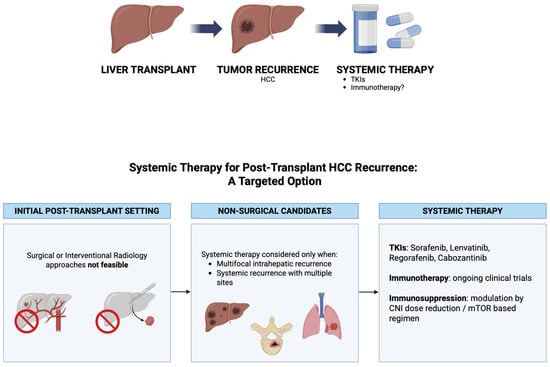
Figure 1
Open AccessReview
Salvage or Second Autologous SCT in Relapsed Multiple Myeloma (2016–2026): A Decade in Review
by
Marwa Nassar, Nourah Alzaidy, Abdulrahman Nasiri, Amr Hanbali, Mahmoud A. Aljurf and Mostafa F. Mohammed Saleh
Curr. Oncol. 2026, 33(3), 140; https://doi.org/10.3390/curroncol33030140 - 28 Feb 2026
Abstract
Background: The role of second or salvage autologous stem cell transplantation (ASCT2) in relapsed multiple myeloma (MM) has evolved substantially over the past decade with the introduction of novel agents, maintenance strategies, and cellular immunotherapies. The clinical value of ASCT2 in the contemporary
[...] Read more.
Background: The role of second or salvage autologous stem cell transplantation (ASCT2) in relapsed multiple myeloma (MM) has evolved substantially over the past decade with the introduction of novel agents, maintenance strategies, and cellular immunotherapies. The clinical value of ASCT2 in the contemporary era requires reappraisal based on modern real-world and prospective data. Methods: We conducted a targeted literature review of PubMed-indexed studies published between January 2016 and January 2026 evaluating second or salvage autologous transplantation in adult patients with relapsed or refractory multiple myeloma. Retrospective registry analyses, real-world cohorts, and prospective randomized trials were included, focusing on feasibility, toxicity, progression-free survival (PFS), overall survival (OS), and prognostic determinants. Fourteen key studies formed the core evidence base, supplemented by guideline statements and comparative immunotherapy data. Results: Across large registry and institutional series, ASCT2 was consistently feasible with low non-relapse mortality (≤5% at day 100–1 year). The median PFS ranged from 9.8 to 30.2 months and the median OS from approximately 30 to >80 months, with outcomes strongly influenced by duration of remission after first ASCT. Patients relapsing ≥24 months after ASCT1 derived the greatest benefit, achieving a median PFS of 17–45 months and OS exceeding 60 months in favorable-risk subgroups. Post-ASCT2 maintenance, particularly with lenalidomide or carfilzomib-based regimens, significantly prolonged disease control in randomized and real-world studies. Conversely, the phase III GMMG ReLApsE trial did not demonstrate a survival advantage for routine salvage ASCT over continuous lenalidomide-based therapy, highlighting the importance of patient selection. In heavily refractory or cytopenic populations, ASCT2 provided modest disease control but enabled hematopoietic recovery and access to subsequent therapies. Conclusions: In the modern treatment landscape, second or salvage autologous transplantation remains a valid, safe, and effective strategy for carefully selected patients with relapsed multiple myeloma, particularly those with chemosensitive disease and prolonged initial remissions. ASCT2 should be integrated in a risk-adapted manner alongside maintenance therapy and emerging immunotherapies, serving as a durable consolidation or bridging approach rather than routine therapy for all relapsed patients.
Full article
(This article belongs to the Section Hematology)
►▼
Show Figures
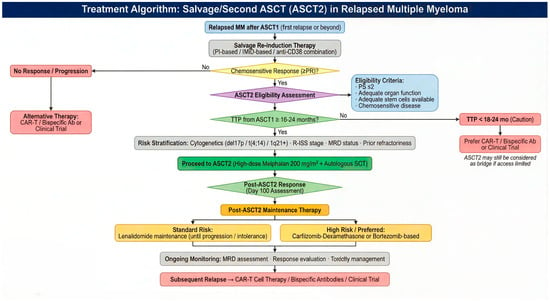
Figure 1
Open AccessArticle
Associations Between Early Neurosurgical Workflow and Survival in Primary Central Nervous System Lymphoma: A Single-Center Retrospective Study
by
Emre Ozkara, Eray Horoz, Zuhtu Ozbek, Deniz Arik, Funda Canaz, Suzan Saylisoy, Hava Uskudar Teke and Murat Vural
Curr. Oncol. 2026, 33(3), 139; https://doi.org/10.3390/curroncol33030139 - 27 Feb 2026
Abstract
Primary central nervous system lymphoma (PCNSL) is an aggressive malignancy for which early management decisions frequently occur within neurosurgical workflows prior to oncologic treatment. In this retrospective single-center study, we aimed to explore whether early neurosurgical workflow characteristics are associated with survival outcomes
[...] Read more.
Primary central nervous system lymphoma (PCNSL) is an aggressive malignancy for which early management decisions frequently occur within neurosurgical workflows prior to oncologic treatment. In this retrospective single-center study, we aimed to explore whether early neurosurgical workflow characteristics are associated with survival outcomes in patients with PCNSL. Consecutive adult patients diagnosed with PCNSL between 2012 and 2022 were included, and the variables of interest comprised pre-biopsy corticosteroid exposure, the interval between diagnostic magnetic resonance imaging (MRI) and stereotactic biopsy, and the time from biopsy to initiation of high-dose methotrexate–based induction therapy. All patients were treated under a standardized hematology protocol to limit systemic treatment heterogeneity. Overall survival (OS) and progression-free survival (PFS) were calculated from the date of diagnostic biopsy, and survival analyses were performed using Kaplan–Meier methods and log-rank testing. Twenty-nine patients met the inclusion criteria. Median OS and PFS were not reached in steroid-naïve patients, whereas pre-biopsy corticosteroid exposure was associated with consistently shorter survival trajectories, with a clear separation of the survival curves, despite conventional statistical significance not being reached. Similarly, median OS and PFS were not reached in patients undergoing biopsy within 7 days of MRI, and an MRI-to-biopsy interval exceeding 7 days demonstrated an unfavorable survival trajectory compared with earlier biopsy; biopsy-to-induction timing did not show a measurable association with early survival outcomes. Established prognostic stratification using Memorial Sloan–Kettering Cancer Center classes showed expected survival discrimination within the cohort, supporting internal validity. Given the limited sample size and retrospective design, all findings should be interpreted as exploratory associations rather than evidence of causality. These results suggest that early neurosurgical workflow characteristics, particularly empiric pre-biopsy corticosteroids avoidance and diagnostic delay minimization, may be associated with early survival trajectories in PCNSL and warrant further evaluation in larger prospective studies.
Full article
(This article belongs to the Section Neuro-Oncology)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Outcomes with Avelumab Maintenance Treatment for Advanced Urothelial Cancer in a US Patient Cohort
by
Kenneth Carson, Seyed Hamidreza Mahmoudpour, Chiemeka Ike, Sebastian Monzon, Stamatina Fragkogianni and Mairead Kearney
Curr. Oncol. 2026, 33(3), 138; https://doi.org/10.3390/curroncol33030138 - 27 Feb 2026
Abstract
Background: This study describes treatment patterns and clinical outcomes in patients with advanced urothelial carcinoma (aUC) in the US following the approval of avelumab for first-line maintenance treatment. Methods: This retrospective cohort study used deidentified patient data from the Tempus database. Eligible patients
[...] Read more.
Background: This study describes treatment patterns and clinical outcomes in patients with advanced urothelial carcinoma (aUC) in the US following the approval of avelumab for first-line maintenance treatment. Methods: This retrospective cohort study used deidentified patient data from the Tempus database. Eligible patients had completed first-line systemic anticancer treatment for aUC between July 2020 and March 2023. Results: In total, 974 eligible patients were identified; most (72%) were male. Median age at diagnosis was 70 years. Among patients who completed first-line platinum-based chemotherapy (644 [66%]), 574 (89%) had no evidence of disease progression. Of 219 patients who received first-line maintenance, 135 (62%) received avelumab. Median (95% CI) overall survival (OS) and progression-free survival (PFS) from avelumab maintenance start were 14.9 months (13.1—not estimable [NE) and 6.4 months (4.6—NE), respectively. Enfortumab vedotin (EV) was the most common second-line treatment after avelumab (70%). Median (95% CI) OS and PFS from second-line EV start were 11.6 months (6.1—NE) and 6.6 months (4.1—NE), respectively. Conclusions: Results provide insights into the impact of avelumab first-line maintenance treatment in patients with aUC in the US. Effectiveness data are consistent with previous findings, supporting the use of avelumab maintenance in patients without disease progression following first-line platinum-based chemotherapy. Second-line EV after progression on avelumab maintenance had similar effectiveness to results from other real-world studies.
Full article
(This article belongs to the Section Genitourinary Oncology)
►▼
Show Figures
Figure 1
Open AccessReview
Health-Related Quality of Life in Long-Term Prostate Cancer Survivors Who Received Hormone Therapy: A Scoping Review
by
Maya Basbous, Keyi Yang, Volker Arndt and Melissa S. Y. Thong
Curr. Oncol. 2026, 33(3), 137; https://doi.org/10.3390/curroncol33030137 - 26 Feb 2026
Abstract
Prostate cancer accounts for the largest group of cancer survivors in men. Hormone therapy is essential, especially in advanced disease. While its short-term effects are well studied, research into the long-term effects on health-related quality of life (HRQOL) remains limited. Therefore, this review
[...] Read more.
Prostate cancer accounts for the largest group of cancer survivors in men. Hormone therapy is essential, especially in advanced disease. While its short-term effects are well studied, research into the long-term effects on health-related quality of life (HRQOL) remains limited. Therefore, this review aims to synthesize and identify key gaps in the literature on HRQOL and symptom burden in long-term prostate cancer survivors who underwent hormone therapy. After searching four databases until 15 April 2025, we identified 14 observational studies that reported on general and prostate cancer-specific HRQOL in prostate cancer survivors ≥ 5 years post-diagnosis. Survivors who underwent hormone therapy reported worse global health status and physical, emotional, and social functioning compared to those treated with local therapies like prostatectomy or radiation. These survivors also experienced greater symptom burdens, alongside worse vitality and mental health. Prostate cancer-specific issues, such as bowel and urinary bother and sexual dysfunction, were also more pronounced in hormone therapy recipients. Nevertheless, outcomes beyond 15 years remain under-researched. The findings of this review highlight the importance of discussing long-term HRQOL compromises with patients who consider hormone therapy. However, they warrant cautious interpretation, particularly due to limited details on hormone therapy regimens and inadequate control for stage.
Full article
(This article belongs to the Section Oncology Nursing)
►▼
Show Figures

Figure 1
Open AccessArticle
Deep Learning-Derived Pathomic Features Predict NCIT Efficacy in Resectable Locally Advanced ESCC: Clinical Utility and Mechanistic Insights
by
Kunrui Zhu, Jie Tong, Yaqi Duan, Yiming Li, Yanqi Feng, Yuelin Han, Xiangtian Xiao, Zhuoyan Han and Shu Xia
Curr. Oncol. 2026, 33(3), 136; https://doi.org/10.3390/curroncol33030136 - 26 Feb 2026
Abstract
Background: Esophageal squamous cell carcinoma (ESCC) is the predominant subtype of esophageal cancer, with poor outcomes following neoadjuvant chemoradiotherapy (NCRT). Neoadjuvant chemoimmunotherapy (NCIT) has emerged as a promising strategy, but reliable predictive biomarkers remain lacking. This study aimed to develop an AI-driven
[...] Read more.
Background: Esophageal squamous cell carcinoma (ESCC) is the predominant subtype of esophageal cancer, with poor outcomes following neoadjuvant chemoradiotherapy (NCRT). Neoadjuvant chemoimmunotherapy (NCIT) has emerged as a promising strategy, but reliable predictive biomarkers remain lacking. This study aimed to develop an AI-driven pathomic model for NCIT response prediction and explore its biological mechanisms. Methods: We analyzed 269 H&E-stained whole-slide images (WSIs) from 198 ESCC patients (104 from Tongji Hospital, 94 from TCGA). Using ResNet152, we segmented WSIs into four tissue categories (tumor cells, stroma, lymphocytes, and necrosis), extracted spatially weighted pathomic features, and constructed the ECiT score via logistic regression. An integrated model combining the ECiT score with clinical variables (T stage, P53 status) was developed. Mechanistic analyses were performed using TCGA-ESCA and GSE160269 datasets. Results: The integrated model achieved AUCs of 0.897 (training) and 0.809 (temporal validation), outperforming clinical (AUC = 0.624) and pathomic-only (AUC = 0.751) models. Mechanistically, a high ECiT score correlated with enhanced immune activation (elevated CD4+ memory T cell infiltration), while low scores were linked to endoplasmic reticulum (ER) stress-unfolded protein response (UPR) activation. EIF2S3 was identified as a key molecular mediator, correlating with three pathomic features, UPR activation, and poor prognosis. Conclusions: This study may offer a preliminary indicator that could assist in personalized clinical decision-making. Correlative evidence suggests that the EIF2S3-mediated ER stress–UPR axis represents a potential candidate therapeutic target to overcome NCIT resistance, generating testable hypotheses to advance precision oncology for resectable locally advanced ESCC.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Concurrent Chemoradiotherapy with Daily Low-Dose Carboplatin in Older Patients with Unresectable Locally Advanced Non-Small-Cell Lung Cancer: Clinical Outcomes and Prognostic Significance of Systemic Inflammation Markers
by
Yu Miura, Hisao Imai, Satoshi Endo, Kosuke Hashimoto, Ou Yamaguchi, Atsuto Mouri, Ken Masubuchi, Takeshi Masubuchi, Yuka Fujita, Shingo Kato, Hiroshi Kagamu and Kyoichi Kaira
Curr. Oncol. 2026, 33(3), 135; https://doi.org/10.3390/curroncol33030135 - 25 Feb 2026
Abstract
Older patients with unresectable locally advanced non-small-cell lung cancer (NSCLC) frequently receive concurrent chemoradiotherapy (CCRT) with daily low-dose carboplatin; however, real-world data on its efficacy, safety, and prognostic factors remain limited. We aimed to retrospectively evaluate the clinical outcomes of this regimen and
[...] Read more.
Older patients with unresectable locally advanced non-small-cell lung cancer (NSCLC) frequently receive concurrent chemoradiotherapy (CCRT) with daily low-dose carboplatin; however, real-world data on its efficacy, safety, and prognostic factors remain limited. We aimed to retrospectively evaluate the clinical outcomes of this regimen and examined whether systemic inflammation-based indices predict prognosis in this setting. We reviewed 52 consecutive patients with locally advanced NSCLC treated with first-line CCRT using daily low-dose carboplatin at three Japanese institutions between April 2007 and December 2019. The median progression-free survival (PFS) and overall survival (OS) were 11.5 and 40.1 months, respectively. Twenty patients received durvalumab as consolidation therapy. In the overall cohort, multivariate analysis identified the Glasgow Prognostic Score (GPS) as an independent predictor of PFS. A GPS of 0–1 was also associated with a significantly longer OS in univariate analysis. CCRT with daily low-dose carboplatin provided durable disease control with acceptable toxicity in older patients with unresectable stage II/III NSCLC. The GPS appears to be a simple marker for PFS in this population and may aid in pretreatment risk stratification alongside histology and consolidation strategies.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Expression of Serum Adenosine Deaminase in Pediatric Non-Hodgkin Lymphoma and Its Association with Clinical Outcomes and Survival
by
Xiuli Zhu, Yuqiao Diao and Yan Chen
Curr. Oncol. 2026, 33(3), 134; https://doi.org/10.3390/curroncol33030134 - 25 Feb 2026
Abstract
Background: Pediatric non-Hodgkin lymphoma (NHL) is a heterogeneous malignancy with variable outcomes. Adenosine deaminase (ADA), a key enzyme in purine metabolism, has been implicated in tumor progression and immune evasion, yet its role in pediatric NHL remains underexplored. Methods: This retrospective study included
[...] Read more.
Background: Pediatric non-Hodgkin lymphoma (NHL) is a heterogeneous malignancy with variable outcomes. Adenosine deaminase (ADA), a key enzyme in purine metabolism, has been implicated in tumor progression and immune evasion, yet its role in pediatric NHL remains underexplored. Methods: This retrospective study included 215 pediatric NHL patients categorized into precursor cell lymphoma (n = 88) and mature cell lymphoma (n = 127) groups based on pathology. Patients were further defined into good (n = 143) and poor prognosis (n = 72) groups according to international response criteria. Serum ADA and other laboratory parameters were measured at diagnosis. Results: Precursor cell lymphomas showed higher rates of bone marrow involvement, peripheral blood involvement, and clinical stage IV disease compared to mature cell lymphomas. ADA levels were significantly elevated in precursor cell lymphomas and in the poor prognosis group. Elevated ADA was strongly correlated with a poor prognosis. Multivariable analysis identified precursor cell lymphoma, fever, bone marrow involvement, elevated LDH, and elevated ADA as independent predictors of poor prognosis (all p < 0.05). Conclusions: Serum ADA is significantly elevated in pediatric NHL, particularly in precursor cell subtypes and poor prognosis cases, and serves as a potential prognostic marker. ADA may help improve risk stratification and guide personalized treatment strategies.
Full article
(This article belongs to the Section Hematology)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- Current Oncology Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal Browser-
arrow_forward_ios
Forthcoming issue
arrow_forward_ios Current issue - Volumes not published by MDPI
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomolecules, Cancers, Cells, Organoids, Current Oncology
Advances in Glioblastoma: From Biology to Therapeutics
Topic Editors: Javier S. Castresana, Miguel IdoateDeadline: 31 March 2026
Topic in
Cancers, IJMS, Pharmaceuticals, Pharmaceutics, Sci. Pharm., Current Oncology, Molecules
Recent Advances in Anticancer Strategies, 2nd Edition
Topic Editors: Hassan Bousbaa, Zhiwei HuDeadline: 31 May 2026
Topic in
Brain Sciences, Cancers, JCM, Neurology International, Diagnostics, Therapeutics, Current Oncology
Innovations in Brain Tumor Surgery: Techniques and Outcomes
Topic Editors: Maria Caffo, Teresa SommaDeadline: 30 June 2026
Topic in
Cancers, Current Oncology, JCM, Medicina, Onco
Cancer Biology and Radiation Therapy: 2nd Edition
Topic Editors: Chang Ming Charlie Ma, Ka Yu Tse, Ming-Yii Huang, Mukund SeshadriDeadline: 25 July 2026

Conferences
Special Issues
Special Issue in
Current Oncology
Biliary Tract Cancer Updates: Advancements and Insights
Guest Editor: Kristen R. SpencerDeadline: 15 March 2026
Special Issue in
Current Oncology
An In-Depth Review of Desmoid Tumours
Guest Editor: Lloyd MackDeadline: 15 March 2026
Special Issue in
Current Oncology
Cost Effectiveness vs. Affordability in the Age of Targeted Drug Therapies
Guest Editor: Ramy SalehDeadline: 15 March 2026
Special Issue in
Current Oncology
Surgical Management of Patients with Hepatobiliary and Pancreatic Malignancies
Guest Editors: Cameron E Gaskill, Jessica E. MaxwellDeadline: 31 March 2026
Topical Collections
Topical Collection in
Current Oncology
New Insights into Prostate Cancer Diagnosis and Treatment
Collection Editor: Sazan Rasul
Topical Collection in
Current Oncology
New Insights into Breast Cancer Diagnosis and Treatment
Collection Editors: Filippo Pesapane, Matteo Suter
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series in "Exercise and Cancer Management"
Collection Editors: Linda Denehy, Ravi Mehrotra, Nicole Culos-Reed
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series: Contemporary Perioperative Concepts in Cancer Surgery
Collection Editors: Vijaya Gottumukkala, Jörg Kleeff