Journal Description
Current Oncology
Current Oncology
is an international, peer-reviewed, open access journal published online by MDPI (from Volume 28 Issue 1-2021). Established in 1994, the journal represents a multidisciplinary medium for clinical oncologists to report and review progress in the management of this disease. The Canadian Association of Medical Oncologists (CAMO), the Canadian Association of Psychosocial Oncology (CAPO), the Canadian Association of General Practitioners in Oncology (CAGPO), the Cell Therapy Transplant Canada (CTTC), the Canadian Leukemia Study Group (CLSG) and others are affiliated with the journal and their members receive a discount on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Oncology)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.5 days after submission; acceptance to publication is undertaken in 2.5 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Clusters of Oncology: Cancers, Current Oncology, Onco and Targets.
Impact Factor:
3.4 (2024);
5-Year Impact Factor:
3.3 (2024)
Latest Articles
Machine Learning-Based Prognostic Modelling Using MRI Radiomic Data in Cervical Cancer Treated with Definitive Chemoradiotherapy and Brachytherapy
Curr. Oncol. 2025, 32(11), 602; https://doi.org/10.3390/curroncol32110602 (registering DOI) - 27 Oct 2025
Abstract
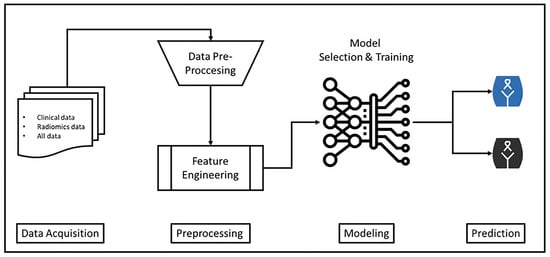
Background: This study aims to evaluate the contribution of clinical and radiomic features to machine learning-based models for survival prediction in patients with locally advanced cervical cancer. Methods: Clinical and radiomic data from 161 patients were retrospectively collected from a single center. Radiomic
[...] Read more.
Background: This study aims to evaluate the contribution of clinical and radiomic features to machine learning-based models for survival prediction in patients with locally advanced cervical cancer. Methods: Clinical and radiomic data from 161 patients were retrospectively collected from a single center. Radiomic features were obtained from contrast-enhanced magnetic resonance imaging (MRI) T1-weighted (T1W), T2-weighted (T2W), and diffusion-weighted (DWI) sequences. After data cleaning, feature engineering, and scaling, survival prediction models were created using the CatBoost algorithm with different data combinations (clinical, clinical + T1W, clinical + T2W, clinical + DWI). The performance of the models was evaluated using test accuracy, precision, recall, F1-score, ROC curve, and Bland–Altman analysis. Results: Models using both clinical and radiomic features showed significant improvements in accuracy and F1-score compared to models based solely on clinical data. In particular, the CatBoost_CLI + T2W_DMFS model achieved the best performance, with a test accuracy of 92.31% and an F1-score of 88.62 for distant metastasis-free survival prediction. ROC and Bland–Altman analyses further demonstrated that this model has high discriminative power and prediction consistency. Conclusions: The CatBoost algorithm shows high accuracy and reliability for survival prediction in locally advanced cervical cancer when clinical and radiomic features are combined. The addition of radiomics data significantly improves model performance.
Full article
(This article belongs to the Special Issue Clinical Management of Cervical Cancer)
►
Show Figures
Open AccessArticle
A Retrospective Analysis of Endovascular Stent Insertion for Malignant Superior Vena Cava Obstruction, Focusing on Anticoagulation Practices
by
Joshua Walker, Amsajini Ravinthiranathan, Athanasios Diamantopoulos, Spyridon Gennatas and Alexandros Georgiou
Curr. Oncol. 2025, 32(11), 601; https://doi.org/10.3390/curroncol32110601 (registering DOI) - 27 Oct 2025
Abstract
Background/Objectives: A knowledge gap persists regarding anticoagulation therapy after endovascular stent insertion for malignant superior vena cava obstruction (mSVCO). Guidelines are supported by retrospective studies with a radiological focus and lack specific drug recommendations. No studies to date have captured the multi-disciplinary nature
[...] Read more.
Background/Objectives: A knowledge gap persists regarding anticoagulation therapy after endovascular stent insertion for malignant superior vena cava obstruction (mSVCO). Guidelines are supported by retrospective studies with a radiological focus and lack specific drug recommendations. No studies to date have captured the multi-disciplinary nature of decision-making over time. Methods: This single-center retrospective service evaluation includes patients with solid organ malignancy who received a stent for mSVCO between July 2016 and May 2022. Patient and treatment characteristics, clinical outcomes and prescribing decisions were collected from medical records and analyzed. Results: Of 49 patients (55% female, mean age 59), 73% had metastatic extra-thoracic disease at stent insertion. Technical success was achieved in 98% of cases and 92% survived to discharge. Forty-eight patients were followed until death. Median survival was 2.4 months. Post-procedure imaging (performed in 55% of patients) revealed 10 (21%) cases of systemic venous thromboembolism and 7 cases of stent thrombosis. Forty-four (91%) patients received anticoagulation therapy (62% therapeutic dose low molecular weight heparin). Those with thrombotic complications were fitter pre-procedurally than the rest of the cohort. There was one case of major bleeding. Twenty-two instances of therapy modification occurred following the initial plan, including nine changes due to a patient preference for oral therapy. Conclusion: Patients undergoing stenting for mSVCO demonstrate high thrombotic risk and a poor prognosis. Anticoagulation plans are frequently modified post discharge due to changing risk profiles and patient preferences. Multi-disciplinary collaboration is essential to support patient-centered and individualized management. Future research should investigate direct oral anticoagulants and anti-platelet therapy and develop risk assessment tools for this population.
Full article
(This article belongs to the Special Issue The Role of Real-World Evidence (RWE) in Thoracic Malignancies)
►▼
Show Figures
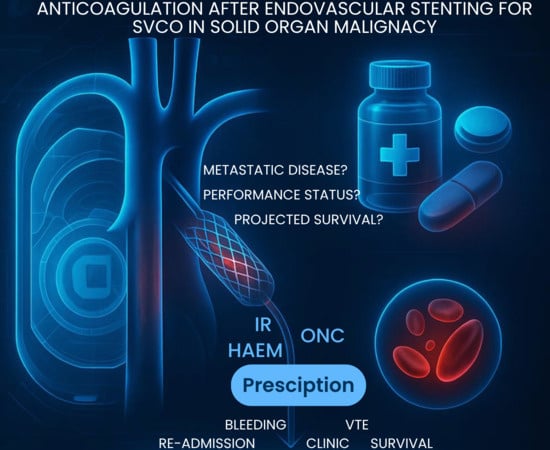
Graphical abstract
Open AccessReview
Advances in Therapeutic Vaccines Against HPV: A Review of Human Clinical Trials
by
Elena Martín, Gabriel Reina and Silvia Carlos
Curr. Oncol. 2025, 32(11), 600; https://doi.org/10.3390/curroncol32110600 (registering DOI) - 25 Oct 2025
Abstract
Cervical cancer remains a major public health concern, particularly in low- and middle-income countries (LMICs) where access to preventive measures is limited. Persistent infection with high-risk human papillomavirus (HPV) types, mainly HPV16 and HPV18, is the key cause of cervical cancer. While prophylactic
[...] Read more.
Cervical cancer remains a major public health concern, particularly in low- and middle-income countries (LMICs) where access to preventive measures is limited. Persistent infection with high-risk human papillomavirus (HPV) types, mainly HPV16 and HPV18, is the key cause of cervical cancer. While prophylactic HPV vaccines effectively prevent new infections, they offer no therapeutic benefit for individuals with established lesions. This review evaluates the clinical evidence on therapeutic HPV vaccines, focusing on their ability to promote viral clearance. A bibliographic search was conducted in PubMed, selecting human studies reporting outcomes on HPV clearance. Seventeen clinical trials were identified, including DNA-based (VGX-3100, GX-188E), viral-vector (MVA E2, TG4001), peptide-based (Pepcan), and bacterial-vector (GLT 001) vaccines. Among them, DNA-based vaccines, particularly VGX-3100, showed the most consistent results, whereas several protein- or vector-based approaches demonstrated variable outcomes. Early therapeutic HPV vaccine trials faced setbacks due to limited efficacy, delivery approaches, and study design challenges, preventing progression to late-phase development. Recent DNA-based candidates, however, are advancing through phase II/III trials. While none have yet to be approved for commercial use, these vaccines elicit virus-specific T-cell responses and can induce regression of precancerous lesions, offering a promising addition to prophylactic vaccination and screening. Variability in study designs and endpoints underlines the need for standardized protocols and further phase III trials. Overall, therapeutic HPV vaccines represent a rapidly advancing field with the potential to complement prophylactic vaccination and screening, thereby strengthening global cervical cancer control efforts, particularly in LMICs.
Full article
(This article belongs to the Section Gynecologic Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Symptom Reporting Behaviors, Symptom Burden, and Quality of Life in Patients with Hormone Receptor–Positive Breast Cancer Undergoing Adjuvant Endocrine Therapy
by
Ece Ulukal Karanci, Halil Göksel Güzel and Banu Öztürk
Curr. Oncol. 2025, 32(11), 599; https://doi.org/10.3390/curroncol32110599 (registering DOI) - 24 Oct 2025
Abstract
Background: Adjuvant endocrine therapy (AET) enhances survival outcomes in hormone receptor–positive (HR+) breast cancer. However, this treatment is associated with toxicities that may adversely affect the quality of life (QoL) and impact patient–physician communication. A thorough understanding of symptom-reporting behaviors is essential
[...] Read more.
Background: Adjuvant endocrine therapy (AET) enhances survival outcomes in hormone receptor–positive (HR+) breast cancer. However, this treatment is associated with toxicities that may adversely affect the quality of life (QoL) and impact patient–physician communication. A thorough understanding of symptom-reporting behaviors is essential for optimizing survivorship care. Methods: This cross-sectional study surveyed 191 female patients with HR+ breast cancer undergoing adjuvant AET (tamoxifen or aromatase inhibitors ± ovarian function suppression [OFS]) at Antalya Training and Research Hospital between July and August 2025. QoL, symptom burden, and adverse event (AE) reporting behaviors were assessed using validated instruments (European Organization for Research and Treatment of Cancer Quality of Life Questionnaire C30 [EORTC QLQ-C30], adapted Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events [PRO-CTCAE]). Categorical variables were compared using chi-square tests, and multivariate analyses were performed using logistic regression. Results: The median age was 54 years (interquartile range [IQR]: 46–61 years). The following independent variables were identified as predictors of a higher symptom burden: prior chemotherapy (odds ratio [OR]: 3.75; 95% confidence interval [CI]: 1.46–9.69; p = 0.006), OFS use (OR: 3.29; 95% CI: 1.51–7.15; p = 0.003), AE reporting to physicians (OR: 3.52; 95% CI: 1.80–6.88; p < 0.001), and complementary and alternative medicine (CAM) use (OR: 7.27; 95% CI: 1.57–33.63; p = 0.011). Independent predictors of poor QoL included receiving psychological support (OR: 0.36; 95% CI: 0.19–0.67; p = 0.002) and AE reporting (OR: 0.28; 95% CI: 0.13–0.64; p = 0.001). Conclusions: Symptom burden and QoL in patients with HR+ breast cancer receiving AET are influenced by clinical history, including chemotherapy and OFS; behavioral factors, such as reporting behaviors; and supportive care, including CAM and psychological support. The routine integration of patient-reported outcomes and proactive symptom monitoring is crucial for delivering personalized and effective survivorship care.
Full article
(This article belongs to the Section Breast Cancer)
►▼
Show Figures

Figure 1
Open AccessArticle
Using the Edmonton Symptom Assessment System (ESAS) to Describe Symptom Burden Associated with Breast Cancer and Related Treatments: A Cross-Sectional Study
by
Sofia Torres, Maureen Trudeau, Geoffrey Liu, Nicholas Mitsakakis and Ahmed M. Bayoumi
Curr. Oncol. 2025, 32(11), 598; https://doi.org/10.3390/curroncol32110598 (registering DOI) - 24 Oct 2025
Abstract
Background: Symptom burden and functional impairment are common in women with breast cancer, yet their prevalence and clinical significance across the disease spectrum remain underexplored. We sought to describe symptom burden and performance status using patient-reported outcome measures and to identify patient characteristics
[...] Read more.
Background: Symptom burden and functional impairment are common in women with breast cancer, yet their prevalence and clinical significance across the disease spectrum remain underexplored. We sought to describe symptom burden and performance status using patient-reported outcome measures and to identify patient characteristics associated with symptoms requiring clinical intervention. Methods: In this cross-sectional study, women with stage I–IV breast cancer completed the Edmonton Symptom Assessment System (ESAS) and the Patient-Reported Functional Status tool. We assessed the prevalence and severity of symptoms and calculated summary distress scores. Multivariable logistic regression was used to identify patient characteristics associated with clinically significant symptoms (ESAS ≥ 4). Results: Among 381 women (mean age 56.8 years; 27% metastatic; 72% with no comorbidities), 70% reported at least one moderate to severe symptom. The most common were tiredness (31%), lack of well-being (30%), and anxiety (21%). Mean summary distress scores were low overall. Most patients reported functional status scores of 0 or 1, and 43% of those with scores ≥2 had metastatic disease. Compared with metastatic patients, women within the first year after diagnosis were less likely to report a symptom requiring intervention (OR 0.49, 95% CI 0.24–0.90). Conclusions: Clinically significant symptoms are common among women with breast cancer, including those with potentially curable disease. Threshold-based use of ESAS, rather than reliance on mean scores, provides a more accurate assessment of patient needs. These findings support the routine integration of patient-reported outcomes into oncology care and underscore the importance of targeted multidisciplinary interventions.
Full article
(This article belongs to the Section Breast Cancer)
►▼
Show Figures

Figure 1
Open AccessSystematic Review
Metabolic Imaging as Future Technology and Innovation in Brain-Tumour Surgery: A Systematic Review
by
Thomas Kapapa, Ralph König, Jan Coburger, Benjamin Mayer, Kornelia Kreiser and Volker Rasche
Curr. Oncol. 2025, 32(11), 597; https://doi.org/10.3390/curroncol32110597 (registering DOI) - 24 Oct 2025
Abstract
Background: Standard imaging in neurosurgery often fails to visualize infiltrative tumor regions that extend beyond contrast enhancement. Metabolic imaging using hyperpolarized 13C-MRI may offer new intraoperative insights into tumor biology. Objective: To systematically assess the clinical and technical evidence on hyperpolarized MRI for
[...] Read more.
Background: Standard imaging in neurosurgery often fails to visualize infiltrative tumor regions that extend beyond contrast enhancement. Metabolic imaging using hyperpolarized 13C-MRI may offer new intraoperative insights into tumor biology. Objective: To systematically assess the clinical and technical evidence on hyperpolarized MRI for metabolic tumour characterization in patients with malignant brain tumors. Eligibility criteria: We included original human studies reporting on hyperpolarized 13C-MRI for perioperative and diagnostic use in brain tumor patients. Reviews, animal studies, and technical-only reports were excluded. Information sources: Searches were conducted in PubMed, Embase, and Web of Science on 26 December 2024. Risk of bias: Methodological quality was assessed using the QUADAS-2 tool. Synthesis of results: A qualitative synthesis was performed, and where feasible, random-effects meta-analysis was used to calculate standardized mean differences (SMDs) and heterogeneity statistics. Results: Three studies (n = 15 patients) met inclusion criteria. The bicarbonate-to-pyruvate ratio showed a significant difference between tumor and non-tumour brain (SMD = 1.34, p = 0.002), whereas pyruvate-to-lactate ratio (kPL) values showed minimal difference (SMD = 0.06, p = 0.730). Asmall effect was observed for kPL between tumor and normal-appearing white matter (SMD = –0.33). One study provided qualitative data only. Overall heterogeneity was high (I2 = 69.4%). Limitations: Limitations include small sample sizes, heterogeneous methodologies, and limited availability of patient-level data. Interpretation: Hyperpolarized 13C-MRI shows metabolic differentiation between tumor and healthy tissue in certain parameters, especially bicarbonate metabolism. While promising, the technology requires further clinical validation before routine intraoperative application.
Full article
(This article belongs to the Topic Innovations in Brain Tumor Surgery: Techniques and Outcomes)
►▼
Show Figures

Figure 1
Open AccessCase Report
Exceptional Response to Trastuzumab Deruxtecan (T-DXd) in HER2-Positive Metastatic Endometrial Cancer
by
Riccardo Vida, Michele Bartoletti, Lucia Lerda, Serena Corsetti, Simona Scalone, Anna Calabrò, Angela Caroli, Monica Rizzetto, Giulia Zapelloni, Elisabetta Caccin, Stefano Fucina, Giorgia Bortolin, Sara Cecco, Paolo Baldo, Sandro Pignata, Daniela Califano, Vincenzo Canzonieri, Antonino Ditto and Fabio Puglisi
Curr. Oncol. 2025, 32(11), 596; https://doi.org/10.3390/curroncol32110596 - 24 Oct 2025
Abstract
Objectives: Endometrial cancer is the most common gynaecologic malignancy, and its mortality rate is rising. Advanced or recurrent disease remains challenging because historically there have been limited therapeutic options. We aim to describe a complete and durable response to the HER2-directed antibody–drug conjugate
[...] Read more.
Objectives: Endometrial cancer is the most common gynaecologic malignancy, and its mortality rate is rising. Advanced or recurrent disease remains challenging because historically there have been limited therapeutic options. We aim to describe a complete and durable response to the HER2-directed antibody–drug conjugate trastuzumab deruxtecan (T-DXd) in a heavily pretreated patient with HER2-positive, mismatch-repair-deficient metastatic serous endometrial cancer. Methods: A 72-year-old woman underwent hysterectomy, bilateral salpingo-oophorectomy, and staging procedures for FIGO stage IIIA, high-grade serous papillary endometrial carcinoma. Tumour profiling revealed dMMR, a p53 abnormal pattern, and HER2 overexpression (IHC 3+). She received carboplatin/paclitaxel plus avelumab, followed by pegylated liposomal doxorubicin and weekly paclitaxel. After progression on paclitaxel, off-label T-DXd was initiated. Molecular data (FoundationOne CDx) were collected, along with and serial imaging and CA125 assessments. Results: The patient developed cough after two cycles of T-DXd; interstitial lung disease was excluded, and treatment resumed with steroid cover. By December 2024, PET/CT demonstrated complete metabolic response, with resolution of vaginal-vault and para-aortic lesions and normalisation of CA125. Real-world progression-free survival exceeded eight months, with ongoing symptom improvement. Treatment was generally well tolerated; the principal adverse event was grade 3 neutropenia requiring dose reduction. No cardiotoxicity or interstitial lung disease occurred. Conclusions: This case illustrates that T-DXd can induce deep and durable remission in HER2-positive, dMMR metastatic serous endometrial cancer after multiple lines of therapy. It adds real-world evidence supporting further investigation of HER2-directed antibody–drug conjugates in gynaecologic malignancies, and underscores the need for confirmatory trials and refined biomarker-driven patient selection.
Full article
(This article belongs to the Section Gynecologic Oncology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Primary Intracranial Meningeal Melanocytoma with Malignant Transformation: A Case Report and Comparison of Early Versus Late Immunotherapy Interventions
by
Yi-Qi Zhang, Kun-Ming Rau, Cheng-Loong Liang, Yu-Duan Tsai, He-Tai Jheng and Kuo-Wei Wang
Curr. Oncol. 2025, 32(11), 595; https://doi.org/10.3390/curroncol32110595 - 24 Oct 2025
Abstract
Primary meningeal melanocytoma is an uncommon, pigmented neoplasm that rarely undergoes malignant transformation, and therapeutic guidelines remain undefined. We report a 43-year-old woman who initially presented with a sudden headache and a right temporal intraparenchymal mass. Subtotal resection revealed a melanocytoma (WHO grade
[...] Read more.
Primary meningeal melanocytoma is an uncommon, pigmented neoplasm that rarely undergoes malignant transformation, and therapeutic guidelines remain undefined. We report a 43-year-old woman who initially presented with a sudden headache and a right temporal intraparenchymal mass. Subtotal resection revealed a melanocytoma (WHO grade I); residual tumor was treated with Gamma Knife. About 15 months later, she deteriorated rapidly due to malignant transformation with cerebral hemorrhage and spinal leptomeningeal metastasis. Pembrolizumab was initiated within four weeks of the malignant diagnosis and produced transient neurological improvement. Due to symptomatic progression, ipilimumab plus nivolumab was commenced and achieved temporary radiographic stabilization, but the patient succumbed to diffuse progression later. Including this case, only five intracranial melanocytomas with malignant transformation treated with immune checkpoint inhibitors have been reported. Our experience supports initiating immunotherapy promptly after malignant transformation and suggests that sequential dual-agent blockade may modestly extend disease control.
Full article
(This article belongs to the Section Neuro-Oncology)
►▼
Show Figures

Figure 1
Open AccessReview
HPV Testing, Self-Collection, and Vaccination: A Comprehensive Approach to Cervical Cancer Prevention
by
Shannon Salvador
Curr. Oncol. 2025, 32(11), 594; https://doi.org/10.3390/curroncol32110594 - 23 Oct 2025
Abstract
This white paper, prepared by a consortium of Canadian national and provincial organizations and experts, outlines urgent strategies to curb the rising incidence of HPV-related cancers, of which, cervical cancer is currently the fastest-growing cancer in Canada. Despite school-based vaccination programs, the national
[...] Read more.
This white paper, prepared by a consortium of Canadian national and provincial organizations and experts, outlines urgent strategies to curb the rising incidence of HPV-related cancers, of which, cervical cancer is currently the fastest-growing cancer in Canada. Despite school-based vaccination programs, the national HPV vaccine uptake remains suboptimal at about 64%, far below the 90% coverage target by 2025 necessary to eliminate cervical cancer by 2040. The report emphasizes a multi-pronged approach: support access to HPV vaccination with expanded funding policies and education around school-based programs while addressing inequities in underserved populations. HPV testing is highlighted as the preferred method for cervical cancer screening, offering higher sensitivity than Pap smears. Self-collection is presented as an innovative strategy to reduce barriers, particularly for marginalized groups, with promising evidence from Canadian pilots and international models. Crucially, we call for investment in comprehensive, population-based databases to track vaccination, screening participation, and follow-up care. Robust registries would allow targeted outreach to under- or never-screened individuals, ensure timely follow-up of abnormal results, and measure the impact of prevention programs across Canada. With vaccination, equitable access to HPV testing, integration of self-collection, and strong data systems, Canada can achieve its goal of eliminating cervical cancer within two decades.
Full article
(This article belongs to the Special Issue Action and Impact: Prevention and Screening Strategies Contributing to the Elimination of Cervical Cancer)
Open AccessArticle
Effects of Hydrocodone Rescheduling on Pain Management Practices Among Older Breast Cancer Patients
by
Chan Shen, Mohammad Ikram, Shouhao Zhou, Roger Klein, Douglas Leslie and James Douglas Thornton
Curr. Oncol. 2025, 32(11), 593; https://doi.org/10.3390/curroncol32110593 - 23 Oct 2025
Abstract
Hydrocodone, a commonly prescribed opioid, was rescheduled from Schedule III to Schedule II in October 2014, imposing stricter prescribing regulations. While prior studies have examined its effects in general populations, its impact on breast cancer patients remains unclear. We evaluated changes in pain
[...] Read more.
Hydrocodone, a commonly prescribed opioid, was rescheduled from Schedule III to Schedule II in October 2014, imposing stricter prescribing regulations. While prior studies have examined its effects in general populations, its impact on breast cancer patients remains unclear. We evaluated changes in pain management among older women with early-stage breast cancer following this policy change. Using SEER-Medicare data from 2011–2019, we identified a retrospective cohort of 52,792 women aged ≥66 years. We assessed trends in the use of hydrocodone, non-hydrocodone opioids, NSAIDs, and antidepressants before and after rescheduling. Hydrocodone use declined from 55% to 40%, while non-hydrocodone opioid use increased from 43% to 50%. Multivariable logistic regression adjusted for demographic and clinical factors confirmed a significant decrease in hydrocodone use (AOR: 0.81, 95% CI: 0.75–0.86) and an increase in non-hydrocodone opioid use (AOR: 1.25, 95% CI: 1.21–1.30). Hydrocodone dosage also declined, while non-hydrocodone opioid dosages remained stable. No significant changes were observed in NSAID or antidepressant use. These findings suggest that hydrocodone rescheduling significantly altered opioid prescribing patterns, reducing hydrocodone use and prompting a shift toward alternative opioids. Further research is warranted to evaluate the appropriateness and outcomes of such shifts in cancer pain management.
Full article
(This article belongs to the Section Breast Cancer)
►▼
Show Figures

Figure 1
Open AccessArticle
Assessment of Fear of Cancer Recurrence in Patients with Colorectal Cancer and Its Association with Pet Ownership: A Cross-Sectional Study
by
Enes Erul, Aslı Nur Avcı, Erman Akkus, Ömer Faruk Ayas, Furkan Berk Danısman and Güngör Utkan
Curr. Oncol. 2025, 32(11), 592; https://doi.org/10.3390/curroncol32110592 - 23 Oct 2025
Abstract
Fear of cancer recurrence (FCR) is a frequent and distressing concern among colorectal cancer (CRC) survivors, often exerting a profound impact on psychological well-being, daily functioning, and treatment adherence. While several clinical and sociodemographic factors have been linked to FCR, the potential role
[...] Read more.
Fear of cancer recurrence (FCR) is a frequent and distressing concern among colorectal cancer (CRC) survivors, often exerting a profound impact on psychological well-being, daily functioning, and treatment adherence. While several clinical and sociodemographic factors have been linked to FCR, the potential role of pet companionship has not been systematically investigated in this population. This cross-sectional study included 167 patients with CRC, assessing FCR with the Fear of Cancer Recurrence Inventory–Short Form (FCRI-SF), psychological distress with the DASS-21, and quality of life with the FACT-G. More than half of the participants (62.3%) met the threshold for high FCR. Multivariable logistic regression revealed that female sex, higher educational attainment, and increased depressive and anxiety symptoms were independently associated with greater odds of high FCR. Conversely, better overall quality of life was linked to lower FCR, with each additional FACT-G point reducing the likelihood of high fear by 5%. Notably, pet ownership emerged as a robust protective factor: pet owners demonstrated approximately one-quarter the odds of high FCR compared with non-owners. Subgroup analyses suggested that this protective effect was particularly evident among women and patients with fewer children, groups potentially more vulnerable to social isolation. These findings highlight pet ownership as a novel factor associated with reduced FCR in CRC patients and suggest potential directions for supportive interventions integrating companion animals into survivorship care.
Full article
(This article belongs to the Special Issue Routine Screening for Distress, Depression and Anxiety in Oncology: Where Are We Now?)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Barriers and Facilitators to Cervical Cancer Screening in Northern Uganda: Qualitative Insights from Healthcare Workers and Administrators
by
Noemi Maria Felisi, David Oyet, Kayeny Miriam Melody Yung, Emmanuel Ochola, Riccardo Vecchio and Anna Odone
Curr. Oncol. 2025, 32(11), 591; https://doi.org/10.3390/curroncol32110591 - 23 Oct 2025
Abstract
Background: Cervical cancer (CC) is the most common cancer among Ugandan women and the leading cause of cancer mortality. Screening has proven to be a cost-effective method in reducing its burden, yet uptake among women of reproductive age remains alarmingly low, with national
[...] Read more.
Background: Cervical cancer (CC) is the most common cancer among Ugandan women and the leading cause of cancer mortality. Screening has proven to be a cost-effective method in reducing its burden, yet uptake among women of reproductive age remains alarmingly low, with national adherence rates under 10%. Objective: This study explored healthcare workers’ (HWs) perspectives on barriers and facilitators to screening and attitudes toward implementing human papillomavirus (HPV) DNA testing with self-collection. Methods: A qualitative research design was employed. Twenty semi-structured interviews were conducted with purposively sampled healthcare providers and administrators across different cadres at a referral hospital and three peripheral health centres in Northern Uganda. Interviews were analysed thematically using the Social Ecological Model. Data collection and analysis proceeded iteratively until thematic saturation. Reporting follows the Consolidated Criteria for Reporting Qualitative Research (COREQ). Results: Participants described individual and interpersonal barriers such as limited awareness, poor preventive health-seeking, fear of results, stigma, and limited male involvement. Organisational barriers included staff shortages, weak referral practices, and stock-outs of supplies, while policy constraints included limited governmental support and competing priorities. Facilitators included targeted health education, routine referrals from all service entry points, outreach screening, and donor support. Most respondents favoured scaling up of self-collected HPV testing, citing higher acceptability and feasibility for outreach, contingent on sustained supplies, laboratory capacity, and training. Conclusions: Multi-level interventions are needed to strengthen facility workflows, staff capability, community engagement, and reliable supply chains. Expanding access to self-collected HPV testing may overcome major barriers and represents a promising strategy to increase screening uptake in Uganda and similar low resource settings.
Full article
(This article belongs to the Section Gynecologic Oncology)
Open AccessArticle
Comparative Efficacy of Photodynamic Therapy and Cold Knife Conization for Cervical High-Grade Squamous Intraepithelial Lesions
by
Xiaoyun Wang, Yiquan Chen, Jianxia Huang, Qiong He and Jianwei Zhou
Curr. Oncol. 2025, 32(11), 590; https://doi.org/10.3390/curroncol32110590 - 22 Oct 2025
Abstract
(1) Background: Photodynamic therapy (PDT) using 5-aminolevulinic acid (5-ALA) offers a non-invasive alternative for managing cervical intraepithelial neoplasia. This comparative study assessed the efficacy and safety of 5-ALA PDT versus cervical conization in treating HSIL. (2) Methods: A total of 137 patients with
[...] Read more.
(1) Background: Photodynamic therapy (PDT) using 5-aminolevulinic acid (5-ALA) offers a non-invasive alternative for managing cervical intraepithelial neoplasia. This comparative study assessed the efficacy and safety of 5-ALA PDT versus cervical conization in treating HSIL. (2) Methods: A total of 137 patients with HSIL and HPV infection, confirmed by pathological biopsy, were included. Based on patient preference and gynecological evaluation, participants were allocated into the PDT group and the CKC group. Follow-up assessments were conducted at 6 months post-treatment, involving HPV testing, cytology, and colposcopy. Additionally, any discomfort or side effects experienced during treatment were documented, along with a preliminary analysis of treatment costs and duration. (3) Results: The overall lesion remission rates were 88.0% for the PDT group and 89.6% for the CKC group, while HPV clearance rates were 80.0% and 82.7%, respectively. Although no statistically significant difference in efficacy was observed between the two groups, the PDT group exhibited a notably lower incidence of side effects. Nevertheless, the PDT group was associated with higher costs and longer treatment duration. (4) Conclusions: These findings indicate that 5-ALA PDT achieves comparable efficacy to CKC in the treatment of HSIL. Therefore, PDT may serve as a valuable therapeutic option for patients seeking fertility preservation or less invasive management strategies.
Full article
(This article belongs to the Section Gynecologic Oncology)
►▼
Show Figures

Figure 1
Open AccessReview
ctDNA in Pancreatic Adenocarcinoma: A Critical Appraisal
by
Sujata Ojha, William Sessions, Yuhang Zhou and Kyaw L. Aung
Curr. Oncol. 2025, 32(11), 589; https://doi.org/10.3390/curroncol32110589 - 22 Oct 2025
Abstract
Pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest malignancies due to late diagnosis and limited treatment options. Circulating tumor DNA (ctDNA) is a promising, minimally invasive biomarker that could improve the clinical outcomes of patients with PDAC by enabling early disease detection,
[...] Read more.
Pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest malignancies due to late diagnosis and limited treatment options. Circulating tumor DNA (ctDNA) is a promising, minimally invasive biomarker that could improve the clinical outcomes of patients with PDAC by enabling early disease detection, minimal residual disease (MRD) assessment, precise prognostication, and accurate treatment monitoring. CtDNA has prognostic as well as predictive value in both resectable and metastatic settings, with serial measurements enhancing risk stratification and recurrence prediction beyond CA19-9. However, despite the promise, the true potential of ctDNA has not yet been fulfilled in patients with PDAC. The current limitations include a low sensitivity of ctDNA assays in early stage PDAC, challenges in the assay interpretation due to the specific nature of ctDNA shedding in PDAC, inter-patient heterogeneity, and technical variability. As precision oncology advances, ctDNA will be a powerful tool for personalized care in PDAC, but rigorous validation of its use within specific clinical contexts is still needed before the true potential of ctDNA is realized for patients with PDAC.
Full article
(This article belongs to the Section Oncology Biomarkers)
►▼
Show Figures

Figure 1
Open AccessReview
Artificial Intelligence in Clinical Oncology: From Productivity Enhancement to Creative Discovery
by
Masahiro Kuno, Hiroki Osumi, Shohei Udagawa, Kaoru Yoshikawa, Akira Ooki, Eiji Shinozaki, Tetsuo Ishikawa, Junna Oba, Kensei Yamaguchi and Kazuhiro Sakurada
Curr. Oncol. 2025, 32(11), 588; https://doi.org/10.3390/curroncol32110588 - 22 Oct 2025
Abstract
►▼
Show Figures
Modern clinical oncology faces an unprecedented data complexity that exceeds human analytical capacity, making artificial intelligence (AI) integration essential rather than optional. This review examines the dual impact of AI on productivity enhancement and creative discovery in cancer care. We trace the evolution
[...] Read more.
Modern clinical oncology faces an unprecedented data complexity that exceeds human analytical capacity, making artificial intelligence (AI) integration essential rather than optional. This review examines the dual impact of AI on productivity enhancement and creative discovery in cancer care. We trace the evolution from traditional machine learning to deep learning and transformer-based foundation models, analyzing their clinical applications. AI enhances productivity by automating diagnostic tasks, streamlining documentation, and accelerating research workflows across imaging modalities and clinical data processing. More importantly, AI enables creative discovery by integrating multimodal data to identify computational biomarkers, performing unsupervised phenotyping to reveal hidden patient subgroups, and accelerating drug development. Finally, we introduce the FUTURE-AI framework, outlining the essential requirements for translating AI models into clinical practice. This ensures the responsible deployment of AI, which augments rather than replaces clinical judgment, while maintaining patient-centered care.
Full article

Figure 1
Open AccessArticle
Skeletal Muscle Radiation Attenuation at C3 Predicts Survival in Head and Neck Cancer
by
Felix Barajas Ordonez, Kunpeng Xie, André Ferreira, Robert Siepmann, Najiba Chargi, Sven Nebelung, Daniel Truhn, Stefaan Bergé, Philipp Bruners, Jan Egger, Frank Hölzle, Markus Wirth, Christiane Kuhl and Behrus Hinrichs-Puladi
Curr. Oncol. 2025, 32(10), 587; https://doi.org/10.3390/curroncol32100587 - 21 Oct 2025
Abstract
Background: Sarcopenia assessed by skeletal muscle area (SMA) at the third lumbar vertebra (L3) is an established prognostic marker in many malignancies, including head and neck cancer (HNC). However, in HNC, L3 is rarely assessed. The prognostic value of myosteatosis, measured by
[...] Read more.
Background: Sarcopenia assessed by skeletal muscle area (SMA) at the third lumbar vertebra (L3) is an established prognostic marker in many malignancies, including head and neck cancer (HNC). However, in HNC, L3 is rarely assessed. The prognostic value of myosteatosis, measured by skeletal muscle radiation attenuation (SMRA) remains largely unexplored. This study evaluated both muscle metrics at the third cervical vertebra (C3) for locoregional control (LRC) and overall survival (OS) in HNC. Methods: SMA and SMRA at C3 were quantified in CT scans of 904 HNC cases by a deep learning-based segmentation pipeline with manual verification. Cox proportional hazards models assessed associations with LRC and OS. Results: Median SMA was 36.64 cm2 (IQR: 30.12–42.44). Median SMRA was 50.77 HU (IQR: 43.04–57.39). In multivariable analysis, lower SMA (HR 1.85, 95% CI: 1.19–2.88, p ≤ 0.001) and lower SMRA (HR 1.76, 95% CI: 1.22–2.54, p < 0.001) were associated with lower LRC. For OS, lower SMA (HR 1.53, 95% CI:1.06–2.20, p = 0.02) and lower SMRA (HR 2.13, 95% CI: 1.58–2.88, p < 0.001) were associated with a worse outcome in multivariable analysis. Conclusions: Both SMRA and SMA assessed at C3 correlate with worse LRC and OS in HNC.
Full article
(This article belongs to the Section Head and Neck Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Integrating Structured Peer Support Pathways for Patients Undergoing Cellular Therapies: Insights from a Participatory Study
by
Karine Bilodeau, Pegah Torabi, Ludovic Tamaro, Sandie Oberoi, Deborah Pascale, Kelley Kilpatrick, David Ogez, Marie-Pascale Pomey, Katia Dumont, Catherine Paquette-Gascon, Israel Fortin, Isabelle Fleury and Imran Ahmad
Curr. Oncol. 2025, 32(10), 586; https://doi.org/10.3390/curroncol32100586 - 21 Oct 2025
Abstract
Individuals diagnosed with hematological cancer often face an emotionally demanding journey, frequently reporting high levels of distress and unmet needs, including a lack of personalized and emotional support. Our research team co-developed structured support provided by trained Accompanying patients (APs) during key stages
[...] Read more.
Individuals diagnosed with hematological cancer often face an emotionally demanding journey, frequently reporting high levels of distress and unmet needs, including a lack of personalized and emotional support. Our research team co-developed structured support provided by trained Accompanying patients (APs) during key stages of the care pathway for individuals with hematological cancers treated with cellular therapies. This paper presents findings on the anticipated needs that APs can address, their role within the care team, and the key facilitators, challenges, and strategies needed to implement structured peer support. Using a participatory action research approach, three working sessions were conducted with 16 key stakeholders to co-develop the structured support pathways. Data from group discussions (n = 3) underwent thematic analysis to identify essential components for adapting the support offered by APs, as well as the barriers and facilitators to its implementation. Findings show that APs can help address a wide range of practical, emotional, social, and psychological needs while enhancing patient understanding and continuity of care. Participants emphasized the importance of clear role definitions, adequate training, and supportive tools to ensure the safe and effective involvement of APs. Organizational and communication challenges were also identified, along with strategies to promote long-term sustainability. This initiative represents the first structured peer support program tailored to cellular therapies in Canada and offers a promising model to improve patient experience, foster relational continuity, and support cancer survivors across the care continuum.
Full article
(This article belongs to the Section Cell Therapy)
►▼
Show Figures
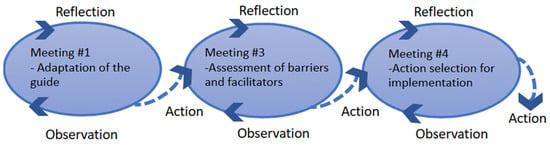
Figure 1
Open AccessArticle
Dynamic Monitoring of Recurrent Ovarian Cancer Using Serial ctDNA: A Real-World Case Series
by
Eric Rios-Doria, Jonathan B. Reichel, Marc R. Radke, Enna Manhardt, Mayumi Rubin-Saika, Christina Lockwood, Elizabeth M. Swisher and Kalyan Banda
Curr. Oncol. 2025, 32(10), 585; https://doi.org/10.3390/curroncol32100585 - 21 Oct 2025
Abstract
Recurrent ovarian cancer (OC) is challenging to detect early using current methods like CA-125 and imaging. Circulating tumor DNA (ctDNA) may improve disease monitoring. Here, we assess the real-world clinical utility of serial ctDNA analyses in patients with recurrent OC. We analyzed serial
[...] Read more.
Recurrent ovarian cancer (OC) is challenging to detect early using current methods like CA-125 and imaging. Circulating tumor DNA (ctDNA) may improve disease monitoring. Here, we assess the real-world clinical utility of serial ctDNA analyses in patients with recurrent OC. We analyzed serial plasma samples (N = 23) from six patients with recurrent OC using a tumor-informed next-generation sequencing assay targeting 68 cancer-related genes developed at the University of Washington. ctDNA variant allele frequencies (VAFs) were correlated with CA-125 levels, radiographic findings, and clinical outcomes. ctDNA levels generally reflected clinical status, accurately mirroring disease progression and therapeutic response. In one patient, rising ctDNA preceded clinical recurrence by four months, despite normal CA-125 and imaging, highlighting its potential advantage. Conversely, some patients exhibited clinical progression with undetectable ctDNA, indicating limitations in assay sensitivity, biological factors, or metastatic sites (e.g., brain metastases). ctDNA and CA-125 showed complementary value in most cases, suggesting potential combined use in clinical monitoring. Our findings demonstrate that ctDNA is a promising biomarker to complement existing monitoring approaches for recurrent OC. In some cases, capable of predicting relapse and treatment response ahead of current clinical indicators. However, identified discordances underscore technical and biological challenges that warrant further investigation. Larger prospective studies are necessary to refine ctDNA’s clinical utility and integration into personalized OC care.
Full article
(This article belongs to the Special Issue Exploring Rare Gynecologic Tumors: A Cutting-Edge Perspective on Modern Diagnostic and Therapeutic Strategies)
►▼
Show Figures
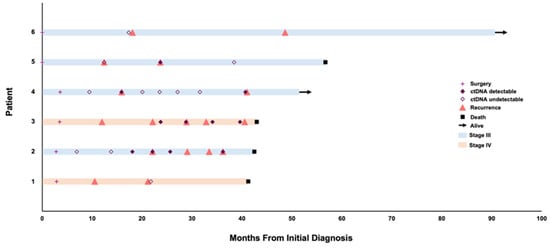
Figure 1
Open AccessReview
Neoadjuvant Strategies for Patients with Resectable Biliary Tract Cancers: A Review
by
Chelsea R. Olson, Gabriela L. Aitken, Michael W. Spinrad and Evan S. Glazer
Curr. Oncol. 2025, 32(10), 584; https://doi.org/10.3390/curroncol32100584 - 20 Oct 2025
Abstract
Cholangiocarcinoma (CC) is a rare and aggressive malignancy that arises from the epithelial cells (cholangiocytes) of the biliary tree. Biliary tract cancers (BTC) include both CC and gall bladder cancer. Surgical resection is considered the only curative treatment. Recently, however, a fundamental shift
[...] Read more.
Cholangiocarcinoma (CC) is a rare and aggressive malignancy that arises from the epithelial cells (cholangiocytes) of the biliary tree. Biliary tract cancers (BTC) include both CC and gall bladder cancer. Surgical resection is considered the only curative treatment. Recently, however, a fundamental shift in the understanding of the molecular profiles of these tumors has led to a molecular-targeted approach with improved survival rates in some patients with these tumors. In patients with local or limited regional disease, neoadjuvant therapies offer a way to downstage tumors, assess tumor biology, potentially achieve R0 resection, and potentially prevent both locoregional and distant recurrence by treating occult micrometastatic disease. Because BTC are rare and surgery is the standard of care for patients with non-metastatic disease, there is very little data evaluating neoadjuvant strategies in resectable disease. Immunotherapies and molecularly targeted agents originally developed for advanced disease in the adjuvant or palliative settings are now being considered for neoadjuvant use. This review aims to summarize the data and provide a rationale for the role of neoadjuvant treatment in patients with resectable BTC. While there is no high-level evidence, studies show that neoadjuvant therapy that incorporates targeted treatments and immunotherapies under multidisciplinary oversight benefits select patients and is a valuable tool in the treatment of BTC. We favor molecular testing to guide neoadjuvant therapy for patients with BTC, when feasible, to prevent unnecessary operations and minimize the risk of recurrence or metastasis.
Full article
(This article belongs to the Special Issue Biliary Tract Cancer Updates: Advancements and Insights)
►▼
Show Figures
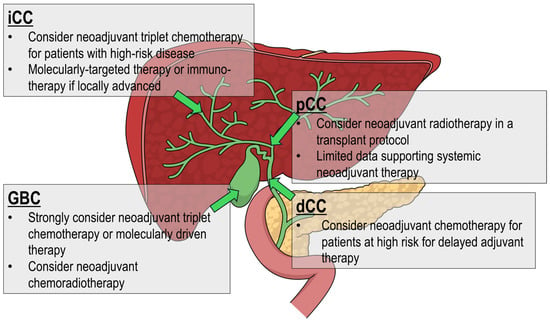
Figure 1
Open AccessReview
Chemokine Receptors in Peripheral Blood Mononuclear Cells as Predictive Biomarkers for Immunotherapy Efficacy in Non-Small Cell Lung Cancer
by
Paloma Galera, Antía Iglesias-Beiroa, Berta Hernández-Marín, Dulce Bañón, Teresa Arangoa, Lucía Castillo, María Álvarez-Maldonado, Cristina Gil-Olarte, Rafael Borregón, María Iribarren, Ramon Colomer and Jacobo Rogado
Curr. Oncol. 2025, 32(10), 583; https://doi.org/10.3390/curroncol32100583 - 20 Oct 2025
Abstract
Non-small cell lung cancer (NSCLC) remains a leading cause of cancer-related mortality globally. The advent of immune checkpoint inhibitors (ICIs) has significantly improved outcomes for a subset of patients; however, predictive biomarkers to identify responders are still lacking. Peripheral blood mononuclear cells (PBMCs)
[...] Read more.
Non-small cell lung cancer (NSCLC) remains a leading cause of cancer-related mortality globally. The advent of immune checkpoint inhibitors (ICIs) has significantly improved outcomes for a subset of patients; however, predictive biomarkers to identify responders are still lacking. Peripheral blood mononuclear cells (PBMCs) offer a minimally invasive means to assess systemic immune status and have emerged as a potential source of predictive biomarkers. Recent studies have highlighted the role of chemokines and their receptors in modulating immune responses against tumors. In particular, the expression levels of chemokine receptors such as CXCR4 on PBMCs have been associated with patient responses to ICIs. The differences in expression of these receptors correlates with enhanced T cell trafficking and infiltration into the tumor microenvironment, leading to improved antitumor activity. This review consolidates current evidence on the prognostic and predictive value of chemokine receptor expression in PBMCs, like T cells, for NSCLC patients treated with ICIs. Understanding these associations can aid in the development of non-invasive biomarkers to guide treatment decisions and improve patient stratification in immunotherapy.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures
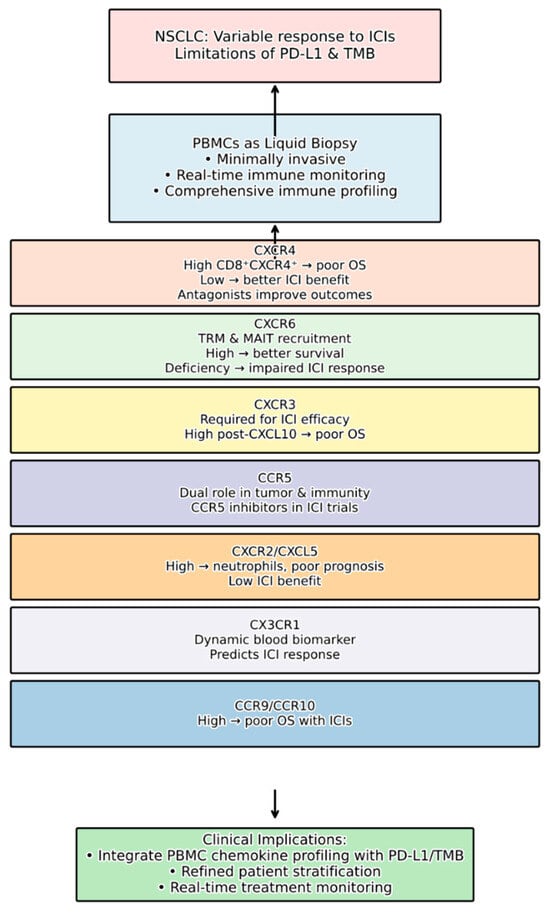
Figure 1

Journal Menu
► ▼ Journal Menu-
- Current Oncology Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal Browser-
arrow_forward_ios
Forthcoming issue
arrow_forward_ios Current issue - Volumes not published by MDPI
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomedicines, Cancers, Current Oncology, Diagnostics, JCM
Advances in Magnetic Resonance Imaging (MRI) and Its Role in Radiation Therapy
Topic Editors: Indra J. Das, Minsong CaoDeadline: 31 October 2025
Topic in
Cancers, IJMS, Pharmaceuticals, Pharmaceutics, Sci. Pharm., Current Oncology, Molecules
Recent Advances in Anticancer Strategies, 2nd Edition
Topic Editors: Hassan Bousbaa, Zhiwei HuDeadline: 31 March 2026
Topic in
Brain Sciences, Cancers, JCM, Neurology International, Diagnostics, Therapeutics, Current Oncology
Innovations in Brain Tumor Surgery: Techniques and Outcomes
Topic Editors: Maria Caffo, Teresa SommaDeadline: 30 June 2026
Topic in
Cancers, Current Oncology, JCM, Medicina, Onco
Cancer Biology and Radiation Therapy: 2nd Edition
Topic Editors: Chang Ming Charlie Ma, Ka Yu Tse, Ming-Yii Huang, Mukund SeshadriDeadline: 25 July 2026

Conferences
Special Issues
Special Issue in
Current Oncology
Evolution of Treatments of Prostate Cancer: From Biology to Current Advanced Technologies
Guest Editor: Fernando MunozDeadline: 31 October 2025
Special Issue in
Current Oncology
The Evolving Role of Surgery in Multidisciplinary Care for Sarcoma Patients
Guest Editors: Russell G. Witt, Elizabeth Lilley, Heather LyuDeadline: 31 October 2025
Special Issue in
Current Oncology
Sarcoma Surgeries: Oncological Outcomes and Prognostic Factors
Guest Editor: Mai-Kim GervaisDeadline: 31 October 2025
Special Issue in
Current Oncology
Exploring Rare Gynecologic Tumors: A Cutting-Edge Perspective on Modern Diagnostic and Therapeutic Strategies
Guest Editors: Brigida Anna Maiorano, Vera LoizziDeadline: 31 October 2025
Topical Collections
Topical Collection in
Current Oncology
New Insights into Prostate Cancer Diagnosis and Treatment
Collection Editor: Sazan Rasul
Topical Collection in
Current Oncology
New Insights into Breast Cancer Diagnosis and Treatment
Collection Editors: Filippo Pesapane, Matteo Suter
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series in "Exercise and Cancer Management"
Collection Editors: Linda Denehy, Ravi Mehrotra, Nicole Culos-Reed
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series: Contemporary Perioperative Concepts in Cancer Surgery
Collection Editors: Vijaya Gottumukkala, Jörg Kleeff