-
 Parents’ Experiences and Clinicians’ Perceptions of Managing Cancer Pain in Young Children at Home
Parents’ Experiences and Clinicians’ Perceptions of Managing Cancer Pain in Young Children at Home -
 Dosimetric Comparison of VMAT Alone and VMAT with HDR Brachytherapy Boost Using Clinical and Biological Dose Models in Localized Prostate Cancer
Dosimetric Comparison of VMAT Alone and VMAT with HDR Brachytherapy Boost Using Clinical and Biological Dose Models in Localized Prostate Cancer -
 Methylation Status of the Telomerase Reverse Transcriptase Promoter in Parotid Tumours and Adjacent Parotid Gland Tissue: A Pilot Study on the Implications for Recurrence and Development of Malignancy
Methylation Status of the Telomerase Reverse Transcriptase Promoter in Parotid Tumours and Adjacent Parotid Gland Tissue: A Pilot Study on the Implications for Recurrence and Development of Malignancy -
 Renal Cell Carcinoma: Prognosis in the Era of Targeted Therapy
Renal Cell Carcinoma: Prognosis in the Era of Targeted Therapy -
 Cervical Cancer Screening Cascade: A Framework for Monitoring Uptake and Retention Along the Screening and Treatment Pathway
Cervical Cancer Screening Cascade: A Framework for Monitoring Uptake and Retention Along the Screening and Treatment Pathway
Journal Description
Current Oncology
Current Oncology
is an international, peer-reviewed, open access journal published online by MDPI (from Volume 28 Issue 1-2021). Established in 1994, the journal represents a multidisciplinary medium for clinical oncologists to report and review progress in the management of this disease. The Canadian Association of Medical Oncologists (CAMO), the Canadian Association of Psychosocial Oncology (CAPO), the Canadian Association of General Practitioners in Oncology (CAGPO), the Cell Therapy Transplant Canada (CTTC), the Canadian Leukemia Study Group (CLSG) and others are affiliated with the journal and their members receive a discount on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Oncology)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.5 days after submission; acceptance to publication is undertaken in 2.5 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Clusters of Oncology: Cancers, Current Oncology, Onco and Targets.
Impact Factor:
3.4 (2024);
5-Year Impact Factor:
3.3 (2024)
Latest Articles
History and Development of Clinical Use of Functional Stereotaxy for Radiation Oncologists: From Its Origins to Its Current State
Curr. Oncol. 2025, 32(12), 656; https://doi.org/10.3390/curroncol32120656 (registering DOI) - 22 Nov 2025
Abstract
►
Show Figures
Background: Stereotactic radiosurgery (SRS) was originally conceived as a noninvasive alternative to functional neurosurgery by the Swedish neurosurgeon Lars Leksell. This review traces the historical development of stereotactic methods from early mechanical frames to advanced image-guided systems and examines the pivotal innovations that
[...] Read more.
Background: Stereotactic radiosurgery (SRS) was originally conceived as a noninvasive alternative to functional neurosurgery by the Swedish neurosurgeon Lars Leksell. This review traces the historical development of stereotactic methods from early mechanical frames to advanced image-guided systems and examines the pivotal innovations that enable precise intracranial targeting for SRS. Methods: Using PubMed and Google Scholar, we reviewed the literature on the general history of functional stereotactic neurosurgery and radiosurgery, its indications, and how their treatment methods evolved, focusing mainly on the early period from the end of the 18th century to the 1990s. Results: The origins of stereotaxy as a principle and technique were traced back to the early 20th century with animal studies by Horsley and Clarke, later adapted for human use by Spiegel and Wycis, and then Talairach in the 1940s. This enabled the precise targeting of deep brain structures for lesion-based interventions in movement, pain, and psychiatric disorders. Deep Brain Stimulation (DBS) emerged in the 1980s as a reversible treatment for tremor. Stereotactic radiosurgery was conceived in 1951 as a noninvasive alternative functional approach and saw limited use until the 1990s due to imaging constraints. With MRI-guided planning, its application has expanded mostly to the management of benign and malignant tumors and vascular disorders, as well as for functional approaches, particularly for trigeminal neuralgia, tremor, epilepsy, and OCD. Conclusions: This review underscores how technological progress and shifting clinical priorities have transformed SRS from a niche neurosurgical technique into a cornerstone of modern clinical practice, with functional SRS representing its latest clinical field of expansion.
Full article
Open AccessArticle
Mode of Minimally Invasive Surgery Associated with Venous Thromboembolism Incidence in Gynecologic Cancer Patients
by
Terry Kara, Selphee Tang, Alon D. Altman, Gregg Nelson and Christa Aubrey
Curr. Oncol. 2025, 32(12), 655; https://doi.org/10.3390/curroncol32120655 (registering DOI) - 22 Nov 2025
Abstract
Postoperative venous thromboembolism (VTE) after minimally invasive surgery (MIS) for gynecologic malignancy is uncommon. Our objective was to characterize the rates and identify risk factors of postoperative VTE. A retrospective cohort study of patients undergoing MIS for gynecologic malignancy at three Canadian institutions
[...] Read more.
Postoperative venous thromboembolism (VTE) after minimally invasive surgery (MIS) for gynecologic malignancy is uncommon. Our objective was to characterize the rates and identify risk factors of postoperative VTE. A retrospective cohort study of patients undergoing MIS for gynecologic malignancy at three Canadian institutions from 2014 to 2020 was performed. The primary outcome was incidence of VTE within 90 days post-operatively. Descriptive statistics were used for clinicopathologic factors, and univariate analysis compared differences between groups. Rate and 95% confidence interval for VTE per 1000 surgeries were calculated. A total of 1786 patients met inclusion criteria, 85.3% uterine, 11.5% cervical, and 2.3% had ovarian cancer. Modes of surgery included robotic (49.4%), laparoscopic (20.7%), or combined laparoscopic/vaginal (29.9%). There were 15 VTE events at 90 days post-operatively (0.84%). Rates of VTE were lowest in patients who underwent robotic surgery, followed by combined laparoscopic/vaginal, and highest in a laparoscopic approach (p = 0.047). Pelvic lymphadenectomy (p = 0.038) and adjuvant chemotherapy (p = 0.022) were the only significant factors associated with risk of VTE. The incidence of VTE after MIS for gynecologic malignancy is low. Robotic surgery was associated with a lower incidence, although event rates are low, and further research is warranted.
Full article
(This article belongs to the Special Issue Optimizing Surgical Management for Gynecologic Cancers)
Open AccessArticle
Prognostic Significance of Complete Blood Count-Derived Inflammatory Biomarkers in Patients with Small Cell Neuroendocrine Carcinoma of the Cervix
by
Mingxuan Zhu, Jing Liu, Yuqin Wang, Huaiwu Lu and Qin Xu
Curr. Oncol. 2025, 32(12), 654; https://doi.org/10.3390/curroncol32120654 - 21 Nov 2025
Abstract
Background: Small cell neuroendocrine carcinoma of the cervix (SCNEC) is a rare and highly aggressive malignancy with limited prognostic biomarkers available for clinical use. Inflammatory markers derived from complete blood count (CBC) have been shown to reflect the systemic immune response and tumor
[...] Read more.
Background: Small cell neuroendocrine carcinoma of the cervix (SCNEC) is a rare and highly aggressive malignancy with limited prognostic biomarkers available for clinical use. Inflammatory markers derived from complete blood count (CBC) have been shown to reflect the systemic immune response and tumor progression in various cancers, but their prognostic value in SCNEC remains unclear. Methods: We retrospectively analyzed clinical data from patients diagnosed with SCNEC between 2004 and 2024 across two centers. Internal validation was performed by dividing patients into training and test cohorts. Cox regression analyses and Kaplan–Meier survival analyses were used to evaluate prognostic factors and treatment outcomes. Inverse probability of treatment weighting (IPTW) was applied to reduce baseline imbalances. Patients were randomly divided into training and test cohorts. A nomogram was constructed to predict 3-year and 5-year progression-free survival (PFS) with performance evaluated using receiver operating characteristic (ROC) curves, calibration plots, and decision curve analysis (DCA). Results: 196 participants were included in the study. Age, FIGO 2018 stage, surgery, neutrophil-to-lymphocyte ratio (NLR), and monocyte-to-lymphocyte ratio (MLR) were independently associated with PFS. High MLR (>0.19) was significantly linked to shorter PFS. After IPTW adjustment, the protective effect of low MLR on PFS remained significant (p = 0.029). The constructed nomogram demonstrated excellent predictive performance, with area under the curve (AUC) values of 0.799 and 0.787 for 3-year and 5-year PFS in the training cohort, and 0.802 for endpoints in the test cohort. Conclusions: MLR was identified as an independent prognostic biomarker for PFS in SCNEC, with potential value in risk stratification and personalized treatment strategies. Additionally, we developed a reliable nomogram that accurately predicts 3-year and 5-year PFS, serving as a practical tool for individualized prognosis and clinical decision-making.
Full article
(This article belongs to the Section Gynecologic Oncology)
►▼
Show Figures

Figure 1
Open AccessReview
High-Throughput 3D Bioprinted Organoids of Skin Cancer Utilized for Diagnosis and Personalized Therapy
by
Arvind Kumar Shukla, Sandhya Shukla, Sonali Pradeep Suryawanshi, Adarsha Mahendra Upadhyay, Navin Ray, Govindhan Thiruppathi, Sayan Deb Dutta and Raj Kumar Mongre
Curr. Oncol. 2025, 32(12), 653; https://doi.org/10.3390/curroncol32120653 - 21 Nov 2025
Abstract
Recent advancements in three-dimensional (3D) bioprinting have revolutionized the modeling of skin cancer, enabling the fabrication of high-throughput, patient-specific organoids that recapitulate the structural, functional, and microenvironmental complexity of native tumors. This review focuses on the integration of cutting-edge bioprinting technologies with bioengineered
[...] Read more.
Recent advancements in three-dimensional (3D) bioprinting have revolutionized the modeling of skin cancer, enabling the fabrication of high-throughput, patient-specific organoids that recapitulate the structural, functional, and microenvironmental complexity of native tumors. This review focuses on the integration of cutting-edge bioprinting technologies with bioengineered extracellular matrices and patient-derived cells to generate physiologically relevant skin cancer models for diagnostic and personalized medicine applications. Key technological innovations, including novel bioinks, multi-material printing strategies, and biomimetic approaches, are discussed for their ability to replicate tumor-stroma interactions, vascularization, and immune microenvironments. The utility of bioprinted organoids in high-throughput drug screening, mutation-targeted therapy design, and biomarker discovery is critically evaluated. Additionally, we address current challenges in standardization, reproducibility, and clinical translation, highlighting regulatory and quality-control considerations. Collectively, this review emphasizes the transformative potential of 3D bioprinted skin cancer organoids as platforms for precision oncology, bridging bioengineering advances with translational research to accelerate therapeutic development and personalized treatment strategies.
Full article
(This article belongs to the Section Dermato-Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Outcomes Following Colorectal Cancer Resection in Elderly Patients
by
Richard Grainger, Tatiana S. Temperley, Hugo C. Temperley, Ben Creavin, Emily Harrold, Cillian Clancy, James O’Riordan, David Gallagher, Brian J. Mehigan, John Larkin, Charles Gillham, Dara Kavanagh, Paul H. McCormick and Michael E. Kelly
Curr. Oncol. 2025, 32(12), 652; https://doi.org/10.3390/curroncol32120652 - 21 Nov 2025
Abstract
Background: Colorectal cancer (CRC) mainly affects older adults, yet elderly patients are underrepresented in outcomes research. Accurate risk stratification tools, such as the Charlson Comorbidity Index (CCI), are essential for guiding surgical decisions in this group. Methods: We conducted a retrospective review of
[...] Read more.
Background: Colorectal cancer (CRC) mainly affects older adults, yet elderly patients are underrepresented in outcomes research. Accurate risk stratification tools, such as the Charlson Comorbidity Index (CCI), are essential for guiding surgical decisions in this group. Methods: We conducted a retrospective review of patients aged 75 years or older who underwent colorectal cancer resection at a tertiary centre between January 2019 and September 2024. Clinical, pathological, and molecular data were analyzed. The primary outcome was a composite of major postoperative complications (Clavien–Dindo grade 3 or higher) or 30-day mortality, stratified by CCI (5 or higher vs. less than 5). Statistical tests included chi-square, Fisher’s exact, and Mann–Whitney U as appropriate. Results: The median age was 81 years (range 75–97), with 59.7% male. CCI ≥ 5 was observed in 24.6% (51/211). The primary composite outcome of major postoperative complications or 30-day mortality occurred in 15/51 (29.4%) patients with a CCI ≥ 5 compared to 19/160 (11.9%) with a CCI < 5 (p = 0.04). Major complications occurred in 18.5% (39/211) of cases, and the 30-day mortality rate was 3.3% (7/211). Laparoscopic resection was independently protective in multivariate analysis (adjusted OR 0.37, p = 0.048), while age ≥85 and emergency presentation were not statistically significant predictors. Conclusions: Colorectal resection in patients aged ≥75 is linked with acceptable morbidity and low short-term death rates. A CCI ≥ 5 significantly predicts adverse outcomes and should be included in preoperative assessments. Minimally invasive surgery seems advantageous and should be considered, when possible, to enhance results in this high-risk group.
Full article
(This article belongs to the Special Issue Advances in Geriatric Oncology: Toward Optimized Cancer Care)
Open AccessArticle
Effects of Resistance Exercise on Quality of Life, Anxiety, Depression, Sleep Quality and Inflammatory Parameters in Patients with Colorectal Cancer Undergoing Active Treatment: A Pilot Randomized Clinical Trial
by
Juan Luis Sánchez-González, Jesus Perez, Eduardo José Fernández-Rodríguez, Emilio Fonseca-Sánchez, Yolanda López-Mateos, Claudia María Sanz-Blanco, Francisco Javier Martín-Vallejo, Alberto García-Martín and Carlos Martín-Sánchez
Curr. Oncol. 2025, 32(12), 651; https://doi.org/10.3390/curroncol32120651 - 21 Nov 2025
Abstract
►▼
Show Figures
Objective: The primary objective of this pilot randomized clinical trial was to determine the effect of adding a supervised resistance exercise programme to a home-based physical activity plan on health-related quality of life in patients with colorectal cancer undergoing active treatment. The secondary
[...] Read more.
Objective: The primary objective of this pilot randomized clinical trial was to determine the effect of adding a supervised resistance exercise programme to a home-based physical activity plan on health-related quality of life in patients with colorectal cancer undergoing active treatment. The secondary objectives were to evaluate its effects on anxiety, depression, sleep quality, and inflammatory parameters. Methods: This is a pilot randomized clinical trial with parallel groups. Patients with CRC were recruited through the Oncology Department at the Salamanca University Health Care Complex in Spain. They were randomly allocated to receive either a home-based physical activity plus a supervised resistance training programme, or the home-based physical activity plan only. The primary outcome was health-related quality of life measures and the secondary outcomes included anxiety, depression and sleep quality evaluations. The supervised training lasted 8 weeks for each patient. Results: A total of 40 patients were recruited, 20 for each group. Adding a supervised resistance exercise programme to the home-based activity plan improved symptoms related to quality of life, such as fatigue (p = 0.040) and constipation (p = 0.015). However, no significant effect was found with regard to other health-related quality of life, anxiety, depression or sleep variables. Conclusions: Fatigue and constipation in patients with CRC receiving chemo- and/or immunotherapy may benefit from the introduction of supervised resistance exercise training programmes.
Full article

Figure 1
Open AccessArticle
Serum p-Cresol and 7-HOCA Levels and Fatty Acid and Purine Metabolism Are Associated with Survival, Progression, and Molecular Classification in GB—Serum Proteome and Metabolome Analysis Pre vs. Post Up-Front Chemoirradiation
by
Andra V. Krauze, M. Li, Y. Zhao, E. Tasci, S. Chappidi, T. Cooley Zgela, M. Sproull, M. Mackey and K. Camphausen
Curr. Oncol. 2025, 32(11), 650; https://doi.org/10.3390/curroncol32110650 - 20 Nov 2025
Abstract
Background: Glioblastoma (GB) is the most common primary brain tumor, with poor prognosis, significant neurological symptoms, and near-universal recurrence. Biomarker development is often limited by the scarcity of tumor tissue available for study. Noninvasive serum-based profiling offers potential to improve outcomes. Purpose: This
[...] Read more.
Background: Glioblastoma (GB) is the most common primary brain tumor, with poor prognosis, significant neurological symptoms, and near-universal recurrence. Biomarker development is often limited by the scarcity of tumor tissue available for study. Noninvasive serum-based profiling offers potential to improve outcomes. Purpose: This study examined serum proteomic and metabolomic profiles pre- and post-concurrent chemoirradiation (CRT) to identify associations with patient outcomes and molecular classification, and to explore relevant signaling and metabolic pathways. Methods: Serum samples from 109 GB patients, obtained prior to and following completion of CRT, were analyzed with each patient serving as their own control, using a SOMAScan® proteomic assay (7289 proteins) and metabolomics (SECIM, 6015 compounds). Clinical data were obtained through chart review. Proteomic and metabolomic changes were examined at baseline (prior to CRT) and in alteration (pre- vs. post-CRT) for their association with overall survival (OS), progression-free survival (PFS), MGMT, and IDH status. Cox models, gene set enrichment analysis (Hallmark, GSEA), and Kaplan–Meier survival analysis were used. Results: Several hundred proteins and metabolites were associated with OS and PFS. MGMT status was known in 60% and IDH in 38% of patients. Pre-CRT DLST (HR 11.7, p < 0.001, adj p = 0.01) was the only protein significantly associated with OS. Pre-CRT, and higher 7-HOCA was linked to worse OS (HR 1.3) and PFS (HR 1.5), while increased p-cresol was associated with improved OS (HR 0.8) and PFS (HR 0.9). Kaplan–Meier analysis based on signal alteration post-CRT vs. pre-CRT, revealed superior OS with lower DLST and MSR1 and superior PFS with higher PGAM2 and ATG5, and lower 7-HOCA. Pathway analysis linked improved PFS to fatty acid metabolism, citric acid cycle, and purine biosynthesis. MGMT and IDH class comparisons revealed associations primarily with amino acid and fatty acid metabolism. Both MGMT methylation and IDH mutation correlated with increased PLAG12B expression, with significance only for MGMT (p < 0.001). IDH mutation was associated with decreased MSR1 (p = 0.047) and p-cresol (p < 0.001). Conclusions: Serum-based fatty acid and purine metabolism pathways are associated with OS and PFS in GB. 7-HOCA and p-cresol emerged as potential biomarkers linked to treatment response and molecular subtype. These findings support further investigation of noninvasive biospecimens for clinically actionable biomarkers in GB.
Full article
(This article belongs to the Special Issue Advances in Radiation Treatment for Brain Tumors)
►▼
Show Figures

Figure 1
Open AccessReview
Neurofibromatosis Type 1 and the Search for Effective Tumor Therapies Using High-Throughput Drug Screening
by
Stephanie J. Bouley, Benjamin E. Housden and James A. Walker
Curr. Oncol. 2025, 32(11), 649; https://doi.org/10.3390/curroncol32110649 - 20 Nov 2025
Abstract
Neurofibromatosis type 1 (NF1) is a complex, multisystem, genetic disorder caused by germline NF1 variants that predispose affected individuals to tumors of the nervous system. With the identification of the NF1 gene in the late 1980s and the elucidation of the role of
[...] Read more.
Neurofibromatosis type 1 (NF1) is a complex, multisystem, genetic disorder caused by germline NF1 variants that predispose affected individuals to tumors of the nervous system. With the identification of the NF1 gene in the late 1980s and the elucidation of the role of the encoded protein, neurofibromin, in regulating RAS signaling, considerable research effort has been invested to identify therapeutic treatments for NF1 tumors. Over the past two decades, high-throughput drug screening approaches have been a significant component of these endeavors. However, considerable variability exists among studies in terms of disease models, symptom targets, screening libraries, methods, and outcomes. In this review, we present an overall summary of efforts toward discovering new therapeutic strategies for NF1-related tumors using high-throughput screening and how such findings can be employed for prospective research in the NF1 field.
Full article
(This article belongs to the Special Issue Neurofibromatosis Type 1 (NF1) Tumor Spectrum)
►▼
Show Figures

Graphical abstract
Open AccessOpinion
Zolbetuximab or Immunotherapy as the Initial Targeted Therapy in CLDN18.2-Positive, HER2-Negative Advanced Gastric Cancer: Weighing the Options
by
Jacob C. Easaw, Howard J. Lim, Hatim Karachiwala, Sharlene Gill, Xiaofu Zhu and Justin Bateman
Curr. Oncol. 2025, 32(11), 648; https://doi.org/10.3390/curroncol32110648 - 20 Nov 2025
Abstract
Advanced gastric/gastroesophageal junction (G/GEJ) adenocarcinoma remains a common and deadly form of cancer. Advances in G/GEJ cancer treatment have improved survival outcomes with the claudin-18.2 (CLDN18.2)-targeted agent, zolbetuximab, and immune checkpoint inhibitors (ICIs) targeting the PD-1 receptor. This article offers an evidence-informed opinion
[...] Read more.
Advanced gastric/gastroesophageal junction (G/GEJ) adenocarcinoma remains a common and deadly form of cancer. Advances in G/GEJ cancer treatment have improved survival outcomes with the claudin-18.2 (CLDN18.2)-targeted agent, zolbetuximab, and immune checkpoint inhibitors (ICIs) targeting the PD-1 receptor. This article offers an evidence-informed opinion on considerations when selecting between these first-line treatments for G/GEJ adenocarcinoma in patients with HER2-negative disease that expresses CLDN18.2 and/or PD-L1, including the reliability of biomarker scoring and interpretation, overall survival (OS) rates, toxicity profiles, and logistical practicalities. Evidence from Phase III trials for zolbetuximab and ICIs suggest similar OS benefits of 14–18 months compared to chemotherapy alone, but there appears to be a gradient of benefit for ICIs with increasing PD-L1 combined positive score (CPS). There is high inter-observer variability in CPS scoring, particularly at lower thresholds. Zolbetuximab is associated with high rates of nausea and vomiting during the initial infusion, whereas ICIs are associated with risk of later-onset immune-related toxicities that can be fatal in rare cases. In considering the available evidence, our opinion is that zolbetuximab is a reasonable option for initial targeted treatment in HER2-/CLDN18.2-positive advanced G/GEJ when PD-L1 CPS score is <10 based on the reliability of biomarker testing, comparable OS, and avoidance of potentially irreversible ICI-induced immune toxicity.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Predicting the Consistency of Vestibular Schwannoma and Its Implication in the Retrosigmoid Approach: A Single-Center Analysis
by
Raffaele De Marco, Giovanni Morana, Silvia Sgambetterra, Federica Penner, Antonio Melcarne, Diego Garbossa, Michele Lanotte, Roberto Albera and Francesco Zenga
Curr. Oncol. 2025, 32(11), 647; https://doi.org/10.3390/curroncol32110647 - 19 Nov 2025
Abstract
To explore the relationship between magnetic resonance imaging (MRI) parameters, including T2-weighted intensity and apparent diffusion coefficient (ADC), and intraoperative tumor characteristics, particularly consistency, in vestibular schwannomas (VSs). The association between tumor consistency, facial nerve (FN) function, and postoperative outcomes was analyzed. A
[...] Read more.
To explore the relationship between magnetic resonance imaging (MRI) parameters, including T2-weighted intensity and apparent diffusion coefficient (ADC), and intraoperative tumor characteristics, particularly consistency, in vestibular schwannomas (VSs). The association between tumor consistency, facial nerve (FN) function, and postoperative outcomes was analyzed. A single-center retrospective analysis included newly diagnosed VS cases (2020–2023) with cisternal involvement (Samii T3a; volume ≥ 0.7 cm3). T2 and ADC maps from the perimetral region of interest were normalized, and tumors were categorized into 3 classes by combining qualitative consistency (soft, fibrous, or fibrous/hard), ultrasonic aspirator power, and adherence to neurovascular structures. FN function was assessed using the House–Brackmann scale at the immediate postoperative period and 12-month follow-up. MRIs of 33 VSs (18 solid and 15 cystic) were analyzed. Normalized values of both T2 (N-T2mean) and ADC (N-ADCmin) maps predicted the classical radiological differentiation. N-ADCmin may have some role in predicting consistency (value 1.361, p = 0.017, accuracy 0.48) and demonstrated a significant association (p = 0.04) with the FN outcome in the immediate postoperative period. An augmented consistency could impair FN function by increasing the intrameatal pressure related to greater transmission of shocks derived from the dissection maneuvers of the cisternal component of the tumor. The possibility of non-invasively exploring VS consistency with a parameter easily calculable on MRI might be beneficial in surgical planning, modifying the timing of the opening of the meatus with respect to what could be the surgical routine in some centers.
Full article
(This article belongs to the Topic Innovations in Brain Tumor Surgery: Techniques and Outcomes)
►▼
Show Figures

Figure 1
Open AccessCase Report
Serial Functional and Genomic Analyses Illuminate Clonal Evolution in Metastatic NSCLC with 12-Year Survival
by
Vikrant S. Bakaya, Sabina A. Schneider, Tracy Nguyen, Derrick C. Phu, Lucas A. Alvarez, Steven S. Evans, Paula J. Bernard, Federico R. Francisco, Adam J. Nagourney, Luisa Torres, John Henry, Jr., Paulo D’Amora and Robert A. Nagourney
Curr. Oncol. 2025, 32(11), 646; https://doi.org/10.3390/curroncol32110646 - 19 Nov 2025
Abstract
Background: Non-small cell lung cancer (NSCLC) is the most common form of lung cancer and a leading cause of cancer-related death. Despite therapeutic advances, long-term survival in stage IV disease is uncommon. Tumor analyses that combine genomic and functional platforms may provide the
[...] Read more.
Background: Non-small cell lung cancer (NSCLC) is the most common form of lung cancer and a leading cause of cancer-related death. Despite therapeutic advances, long-term survival in stage IV disease is uncommon. Tumor analyses that combine genomic and functional platforms may provide the opportunity to monitor clonal dynamics and guide therapy selection. Case Presentation: We report a 67-year-old woman with metastatic poorly differentiated lung adenocarcinoma, who achieved four durable remissions and survived nearly 12 years. Serial studies using ex vivo analysis of programmed cell death (EVA/PCD) functional-profiling-guided therapeutic choices were correlated with next-generation sequencing (NGS). Molecular events included the emergence of a BRAF V600E mutation responsive to dabrafenib plus trametinib and the acquisition of an EGFR exon 19 deletion responsive to Osimertinib. EVA/PCD identified activity for targeted agents and revealed synergy for vinorelbine plus Osimertinib not predicted by genomic profiling, which provided additional response. Discussion: This case highlights clonal evolution in NSCLC and illustrates how serial tissue analyses correlating phenotypic and genomic events can offer therapeutic interventions to provide long-term survival. Conclusions: The integration of functional and genomic profiling may improve personalized treatment in NSCLC by interrogating tumor heterogeneity and clonal evolution to inform rational therapeutic selection.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures
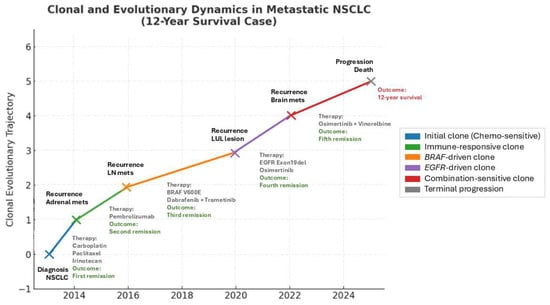
Figure 1
Open AccessArticle
Examining the Association Between Equity-Related Factors and EQ-5D-3L Health Utilities of Patients with Cancer
by
Teresa C. O. Tsui, Rebecca E. Mercer, Eleanor M. Pullenayegum and Kelvin K. W. Chan
Curr. Oncol. 2025, 32(11), 645; https://doi.org/10.3390/curroncol32110645 - 19 Nov 2025
Abstract
Background: EQ-5D-3L health utilities inform health technology assessments in oncology, often derived from clinical trials enrolling highly selected populations, which may over-estimate real-world health utilities. Little is known about the association between socioeconomic status (SES) and EQ-5D-3L health utilities. Our objective was to
[...] Read more.
Background: EQ-5D-3L health utilities inform health technology assessments in oncology, often derived from clinical trials enrolling highly selected populations, which may over-estimate real-world health utilities. Little is known about the association between socioeconomic status (SES) and EQ-5D-3L health utilities. Our objective was to examine EQ-5D-3L health utilities across SES in a real-world sample of patients with cancer. Methods: We conducted a cross-sectional analysis of EQ-5D-3L responses from 170 adult patients with cancer accrued from an Ontario oncology centre. We fitted multivariable linear regression models to estimate associations between covariates and EQ-5D-3L health utilities. Results: Lower EQ-5D-3L health utilities were significantly associated with the lowest and undisclosed family income categories in models with and without birth sex (p < 0.05). In the model including birth sex, disutility estimates for lowest family income (<CAD 29K) and undisclosed income was −0.202, 95% CI (−0.371 to −0.033), and −0.123 (−0.235 to −0.012), respectively. For the model excluding birth sex, disutility estimates for lowest income and undisclosed income was −0.163 (−0.280 to −0.046) and −0.106 (−0.184 to −0.028). Conclusions: Lower EQ-5D-3L health utilities were significantly associated with low income and nondisclosure, highlighting the need to incorporate SES in analyzing health utilities in cancer care.
Full article
(This article belongs to the Section Health Economics)
►▼
Show Figures
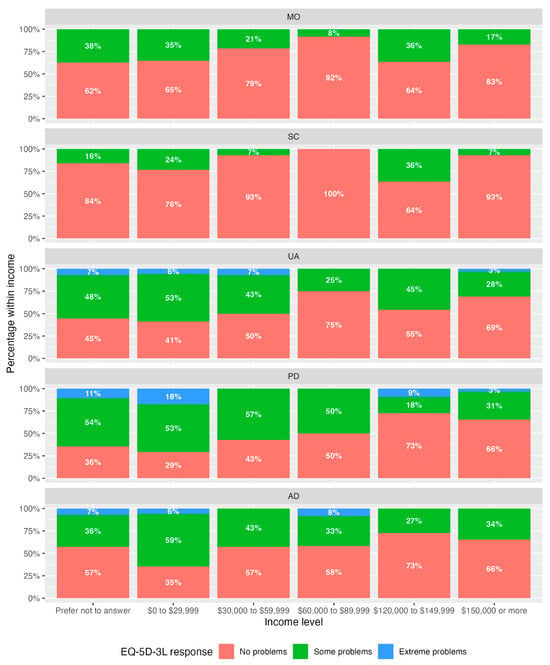
Figure 1
Open AccessArticle
Parenteral Nutrition in Patients with Incurable Cancer: Exploring the Heterogenous and Non-Randomised Clinical Landscape
by
Marianne Erichsen, Tora S. Solheim, Inger Ottestad, Ingvild Paur, Rikka F. Sande, Astrid Nygaard, Emilie H. Markhus, Lene Thoresen, Morten Thronæs, Randi J. Tangvik, Kari Sygnestveit, Patrik Hansson, Cathrine Vestnor, Gunnhild Jakobsen, Ørnulf Paulsen, Erik Torbjørn Løhre and Trude R. Balstad
Curr. Oncol. 2025, 32(11), 644; https://doi.org/10.3390/curroncol32110644 - 18 Nov 2025
Abstract
Background: There is an insufficient knowledge base for optimal parenteral nutrition (PN) use for patients with incurable cancer, leading to vague guidelines and varied practices. The aim of the study is to describe the practices and actual outcomes of PN in patients
[...] Read more.
Background: There is an insufficient knowledge base for optimal parenteral nutrition (PN) use for patients with incurable cancer, leading to vague guidelines and varied practices. The aim of the study is to describe the practices and actual outcomes of PN in patients with incurable cancer at Norwegian hospitals. Methods: This multicentre study retrospectively reviewed 507 deceased patients (>18 years) receiving PN between 2011 and 2017. Data were collected from PN initiation until death, and analyses were descriptive. Results: Fifty-one percent had upper and lower gastrointestinal cancers, and the main PN indications were insufficient intake (75%) and gastrointestinal malfunction (47%). Sixty-seven percent received no anticancer treatment. Forty-three (8%) received PN as temporary bridging to anticancer treatment, of whom fifteen (35%) resumed or initiated treatment. The median PN dose corresponded to 53% of estimated energy requirements, and 94% of the patients had complementary energy intake. The most common reason for discontinuation was expected imminent death (47%). While common symptoms during PN were nausea (52%), vomiting (46%), and oedema (37%), 15% reported improved wellbeing. Conclusions: In this real-world cohort, up to 80% of the patients would not meet the eligibility criteria of previous trials due to cancer diagnosis and treatment, gastrointestinal tract function, weight loss criteria or complications such as ascites. This study highlights the heterogeneity in how patients with incurable cancer receive PN, and emphasises the importance of individualised PN treatment, carefully and safely managed to meet the patients’ palliative care situation. Future real-world pragmatic patient-centred protocols bridging the gap between clinical trials and patients in clinical practice are warranted.
Full article
(This article belongs to the Section Palliative and Supportive Care)
►▼
Show Figures

Figure 1
Open AccessArticle
Diversity and Experiences of Radiation Oncologists in Canada: A Survey of Gender Identity, Sexual Orientation, Disability, Race, Ethnicity, Religion, and Workplace Discrimination—A National Cross-Sectional Electronic Survey
by
Amanda F. Khan, Stefan Allen, Ian J. Gerard, Rhys Beaudry, Glen Bandiera, David Bowes, Jolie Ringash, Reshma Jagsi, Jennifer Croke and Shaun K. Loewen
Curr. Oncol. 2025, 32(11), 643; https://doi.org/10.3390/curroncol32110643 - 17 Nov 2025
Abstract
►▼
Show Figures
Background: This study’s objective was to be the first to explore the ethnicity/cultural origins, gender identity, ability/disability, sexual orientation, socioeconomic background, and harassment/discrimination experiences of Canadian radiation oncologists (ROs). Methods: Following a literature review and input from content experts, an ethics-approved national cross-sectional
[...] Read more.
Background: This study’s objective was to be the first to explore the ethnicity/cultural origins, gender identity, ability/disability, sexual orientation, socioeconomic background, and harassment/discrimination experiences of Canadian radiation oncologists (ROs). Methods: Following a literature review and input from content experts, an ethics-approved national cross-sectional electronic survey was developed in English and French and electronically distributed to all ROs in Canada (n = 598). Descriptive statistics summarized responses. Comparisons between groups were performed using Chi-square tests, and content analysis was performed on open-ended responses. Results: The survey was completed in full by 42.5% of ROs (254/598). Most respondents were male (62.9%), 35–44 years old (39.2%), and heterosexual (94.3%). 41.2% identified as belonging to a racialized group, which is higher than the overall Canadian population (27%), but Black, Indigenous, and Southeast Asian ROs were underrepresented (1.9% vs. 4%, <1% vs. 5% and 1.6% compared to 4%, respectively). A significant subset analysis showed that only 20% (21/105) of racialized ROs were women, whereas Caucasian women comprised 49.3% (74/150) of Caucasian respondents (p < 0.001). While 75.4% of respondents reported job satisfaction, 42.1% reported experiencing workplace discrimination/harassment within the past 5 years; most commonly, this was perpetrated by fellow faculty (31.7%; 58/183) or patients or their family members (31.7%; 58/183). Respondents felt that gender, race/ethnicity, and age were the three top reasons for discrimination/harassment, with double the amount of racialized ROs reporting harassment compared to White ROs (p < 0.001). Nearly half (45.2%; 114/252) did not understand how to report, or felt uncomfortable reporting, workplace discrimination/harassment. Conclusions: This study highlights high harassment and discrimination rates amongst Canadian ROs, especially amongst racialized women, which may affect career satisfaction and attrition rates. Compared to census data, Black, Indigenous, and Southeast Asian ROs were underrepresented, and amongst racialized ROs, racialized women were significantly underrepresented. These findings underscore the need for targeted diversity initiatives, improved mentorship programs, and stronger institutional policies to address harassment and foster an inclusive work environment.
Full article

Figure 1
Open AccessArticle
Complications of Robotic Pelvic Lymph Node Dissection for Prostate Cancer: An Analysis of the National Surgical Quality Improvement Program Targeted Prostatectomy Database
by
Vatsala Mundra, Renil S. Titus, Eusebio Luna-Velasquez, Jiaqiong Xu, Carlos Riveros, Sanjana Ranganathan, Aamuktha Porika, Brian J. Miles, Dharam Kaushik, Christopher J. D. Wallis and Raj Satkunasivam
Curr. Oncol. 2025, 32(11), 642; https://doi.org/10.3390/curroncol32110642 - 16 Nov 2025
Abstract
Introduction/Background: Treatment of localized prostate cancer includes radical prostatectomy (RP) with or without pelvic lymph node dissection (PLND). While multiple guidelines recommend PLND for staging purposes, recent data has shown questionable therapeutic benefit. Thus, understanding the morbidity associated with PLND is important for
[...] Read more.
Introduction/Background: Treatment of localized prostate cancer includes radical prostatectomy (RP) with or without pelvic lymph node dissection (PLND). While multiple guidelines recommend PLND for staging purposes, recent data has shown questionable therapeutic benefit. Thus, understanding the morbidity associated with PLND is important for counseling patients. We used the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) targeted prostatectomy database to quantify real-world 30-day postoperative outcomes of patients undergoing contemporary robot-assisted PLND at the time of RP for prostate cancer to quantify the incremental morbidity. Methods: We conducted a retrospective cohort study using the NSQIP database of adult patients undergoing radical prostatectomy from 2019 to 2022. The primary outcomes were procedure-specific outcomes such as lymphocele and rectal injury. Secondary outcomes included a composite of any of the following 30-day major postoperative outcomes: mortality, reoperation, cardiac or neurologic event, as well as the individual components of this outcome, as well as infectious and other complications. We also analyzed yearly trends associated with PLND. Groups were balanced using propensity score matching (PSM) with a 1:1 ratio using demographic characteristics, prior medical history, and cancer staging data. Likelihood of complications was assessed by conditional logistic regression. Results: We identified 13,413 patients between 2019 and 2022 who underwent robotic prostatectomy: 11,341 (85%) had PLND while 2072 (15%) did not. After PSM, our cohort included 2071 matched pairs of patients with and without PLND. Patients who underwent PLND were more likely to be diagnosed with lymphocele (2.14% vs. 0.68%, OR 4.17; 95% CI 2.00, 8.68), have unplanned readmission (4.22% vs. 3.27%, OR 1.31; 95% CI 1.03, 1.65), and develop organ-site/space SSI (1.18% vs. 0.60%) (OR 1.97, 95% CI 1.20, 3.23). There was no significant association between the receipt of PLND and the likelihood of urinary leak or fistula, or ureteral obstruction. There were no significant differences between the two groups with respect to secondary outcomes of interest. Conclusion: Contemporary robotic PLND is associated with a 3-fold increased likelihood of lymphocele, as well as increased likelihood of unplanned readmission and organ-site SSI, though no significant differences in major postoperative complications were identified. We found that the odds of lymphoceles, readmission, and SSI in our study are lower than previously reported. These data provide real-world data to guide patient counseling and optimize patient selection for PLND at the time of RALP.
Full article
(This article belongs to the Section Surgical Oncology)
Open AccessArticle
Cancer Treatment Patterns Among Yukon Residents Referred to British Columbia for Care: A 13-Year Retrospective Study
by
Kaylie Willemsma, Jonathan Simkin, Debon Lee, Emma Quinn, Kira Makuk, Emily B. Jackson, Andrew Bang, Manik Chahal, Ying Wang and Jessica Chan
Curr. Oncol. 2025, 32(11), 641; https://doi.org/10.3390/curroncol32110641 - 16 Nov 2025
Abstract
►▼
Show Figures
Yukon residents often must travel long distances to access specialized cancer care, which may impact cancer treatment patterns. We conducted a retrospective study to characterize all adult breast, prostate, colorectal, and lung cancer cases from the Yukon, diagnosed from 2009 to 2021 and
[...] Read more.
Yukon residents often must travel long distances to access specialized cancer care, which may impact cancer treatment patterns. We conducted a retrospective study to characterize all adult breast, prostate, colorectal, and lung cancer cases from the Yukon, diagnosed from 2009 to 2021 and seen in consultation at BC Cancer. We collected data on demographics, tumour characteristics and treatment, including timepoints for cancer care. A secondary analysis of non-referred cases was conducted. There were a total of 336 breast, 270 prostate, 279 colorectal and 266 lung cancer cases diagnosed in the Yukon from 2009 to 2021, of which 298 (88.7%), 120 (44.4%), 206 (73.8%) and 204 (76.7%) cases were referred to BC Cancer, and 266 (79.2%), 118 (43.7%), 204 (73.1%) and 183 (68.8%) were included in this study, respectively. Most cases were diagnosed at an early stage (breast: 92.9%, prostate: 82.2%, colorectal: 72.1%, lung: 45.9%). Nearly 70% of cases resided in Whitehorse (Yukon’s capital), where most Yukon residents live. Compared to available published Canadian timepoints, Yukon patients had similar or shorter wait times in 13 of 22 timepoints along the pathway to diagnosis and treatment. However, time from biopsy to surgery had the longest relative wait times across all tumour groups (range: 26–60% longer). Our study provides baseline data that can help inform cancer care provision for Yukon residents.
Full article

Figure 1
Open AccessArticle
Acupuncture Improves Functional Limitations for Cancer Patients with Chronic Pain: A Secondary Analysis of PEACE Randomized Clinical Trial
by
Lingyun Sun, Mothi Babu Ramalingam, Raymond Baser, Marco Santos Teles, Christina Seluzicki, Qing Susan Li and Jun J. Mao
Curr. Oncol. 2025, 32(11), 640; https://doi.org/10.3390/curroncol32110640 - 16 Nov 2025
Abstract
Chronic pain significantly impairs functional performance in patients with cancer. Although acupuncture is effective for cancer-related pain, its impact on pain-related functional interference remains unclear. This secondary analysis of the PEACE randomized clinical trial included patients with prior cancer diagnoses and musculoskeletal pain
[...] Read more.
Chronic pain significantly impairs functional performance in patients with cancer. Although acupuncture is effective for cancer-related pain, its impact on pain-related functional interference remains unclear. This secondary analysis of the PEACE randomized clinical trial included patients with prior cancer diagnoses and musculoskeletal pain for ≥3 months. Participants were randomized to groups undergoing 10 weeks of electro-acupuncture, auricular acupuncture, or a waitlist control. Functional performance was assessed using the Quick-Disability Arm/Shoulder/Hand (Q-DASH) for upper limbs and the Western Ontario and McMaster Universities Osteoarthritis (WOMAC) subscale for lower limbs (higher scores = worse function). Linear mixed models compared changes over time between groups, with week 12 as the primary endpoint. Functional changes were also compared between pain responders and non-responders in the acupuncture arms. Among 360 patients (mean [SD] age, 62.1 [12.7] years; 69.7% women), mean baseline Q-DASH and WOMAC scores were 33.2 (19.8) and 33.3 (20.3). At week 12, both electro-acupuncture and auricular acupuncture significantly improved function versus waitlist: Q-DASH by −7.18 and −9.64 points, respectively, and WOMAC by −6.89 and −7.61 points (all p < 0.001). No differences were found between the two acupuncture groups. Treatment effects on Q-DASH diminished during follow-up, while improvements on WOMAC persisted. Within the acupuncture groups, pain responders achieved greater functional gains than non-responders (Q-DASH, −6.74; WOMAC, −6.16; both p < 0.001). Electro-acupuncture and auricular acupuncture improved upper and lower extremity function in cancer patients with chronic pain. These findings support acupuncture as a potential adjunct in functional rehabilitation for cancer survivors.
Full article
(This article belongs to the Special Issue Cancer Rehabilitation: Innovations in Practice & Enhancing Survivorship Care)
►▼
Show Figures

Figure 1
Open AccessArticle
Efficacy of Anti-VEGF and Anti-EGFRs in Microsatellite Instable (MSI-H) Metastatic Colorectal Cancer in a Turkish Oncology Group (TOG) Cohort Study
by
İlknur Deliktaş Onur, Mutlu Doğan, Mehmet Akif Öztürk, Taha Koray Sahin, Murat Kiracı, Ahmet Melih Arslan, Eda Karapelit, Bahar Beliz Karaoğlan, Nargiz Majidova, Elif Şahin, Sabin Göktaş, Abdullah Sakin, Ali Oğul, Emine Türkmen, Kadriye Başkurt, Zeynep Yüksel Yaşar, Yakup Ergün, Esma Türkmen Bekmez, Şafak Yıldırım Dişli, Sinem Akbaş, Sema Türker, Ömer Dizdar, Öznur Bal, Tuğba Yavuzşen, Melek Karakurt, Arzu Hatime Yaşar, Tuğba Başoğlu, Faysal Dane, Şuayip Yalçın and Öztürk Ateşadd
Show full author list
remove
Hide full author list
Curr. Oncol. 2025, 32(11), 639; https://doi.org/10.3390/curroncol32110639 - 14 Nov 2025
Abstract
Background: Mismatch repair-deficient (dMMR)/microsatellite instability-high (MSI-H) colorectal tumors constitute 5% of metastatic colorectal cancer(mCRC). Immunotherapy is a new standard, but it is difficult to provide for all patients. 5-Flurouracil-based treatment with anti-EGFRs (cetuximab and panitumumab) in RAS/BRAF-wild or anti-VEGF (bevacizumab) is used in
[...] Read more.
Background: Mismatch repair-deficient (dMMR)/microsatellite instability-high (MSI-H) colorectal tumors constitute 5% of metastatic colorectal cancer(mCRC). Immunotherapy is a new standard, but it is difficult to provide for all patients. 5-Flurouracil-based treatment with anti-EGFRs (cetuximab and panitumumab) in RAS/BRAF-wild or anti-VEGF (bevacizumab) is used in mCRC. Data is limited for the efficacy of anti-VEGF or anti-EGFRs in dMMR/MSI-H mCRC due to the small number of cases in the colorectal cancer population in trials. Aims: To evaluate prognostic factors in dMMR/MSI-H mCRC and compare progression-free survival time of patients receiving anti-VEGF and anti-EGFR combined with first-line 5FU-based therapy. Methods: Patients with metastatic dMMR/MSI-H colorectal cancer diagnosed between January 2015 and January 2023 were included in this cohort study. Progression-free survival times of patients treated with first-line therapy were compared. Prognostic factors associated with overall survival were investigated. Results: A total of 132 patients were included. Mutation rates were 35.6% (n:47) for RAS and 12.1% (n: 16) for BRAF (. Median progression-free survival (PFS) was 10.9 (95% CI: 9.2–12.6) months. Median overall survival (OS) was 44 months (95% CI: 26.23–63.03). 82 (62.1%) patients had primary tumor resection (PTR), 26 (19.7%) had PTR and metastasectomy. A total of 17 (12.8%) de novo mCRC patients had maximal cytoreductive surgery (MCS). A total of 14 (10.6%) patients had subsequent immunotherapy (IO). In multivariate analysis, RAS/BRAF mutation status, MCS, and subsequent IO are defined as prognostic factors for OS (p < 0.01, p: 0.022, and p: 0.005, respectively). No statistically significant difference (PFS, OS) was found in patients receiving first-line anti-VEGF or anti-EGFR therapy. Conclusions: dMMR/MSI-H mCRC is an entity with different tumor biology. We consider that dMMR/MSI-H mCRC patients with BRAF wild, MCS and subsequent IO have better outcomes with 1st line 5FU-based treatment with anti-VEGF/anti-EGFRs.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures
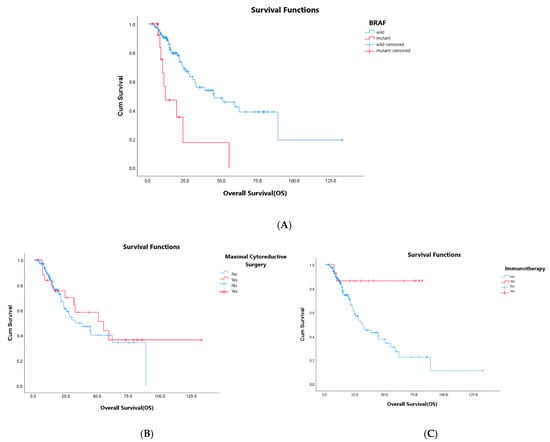
Figure 1
Open AccessArticle
Confirmatory Clinical Validation of a Serum-Based Biomarker Signature for Detection of Early-Stage Pancreatic Ductal Adenocarcinoma
by
Patricio M. Polanco, Tamas Gonda, Erkut Borazanci, Evan S. Glazer, Jose G. Trevino, George DeMuth, Lisa Ford, Thomas King, Norma A. Palma and Randall E. Brand
Curr. Oncol. 2025, 32(11), 638; https://doi.org/10.3390/curroncol32110638 - 13 Nov 2025
Abstract
Early detection of pancreatic ductal adenocarcinoma (PDAC) could extend patient survival, and biomarkers to facilitate this are urgently needed. Here, we performed a second independent validation of PancreaSure, a 5-plex serum biomarker signature to detect early-stage PDAC in high-risk individuals. In contrast to
[...] Read more.
Early detection of pancreatic ductal adenocarcinoma (PDAC) could extend patient survival, and biomarkers to facilitate this are urgently needed. Here, we performed a second independent validation of PancreaSure, a 5-plex serum biomarker signature to detect early-stage PDAC in high-risk individuals. In contrast to the first validation, this study’s cohort was preemptively balanced for age and sex and only included samples stored for fewer than 5 years. The primary endpoint was to measure test sensitivity against the performance target of 65%. Measuring specificity against the performance target of 90% and comparing test performance to that of carbohydrate antigen 19-9 (CA 19-9) alone were secondary endpoints. Signature analytes were retrospectively measured in serum from a blinded independent cohort of Stage I and II PDAC cases and high-risk controls. A predictive signal for PDAC was generated from a predefined cutoff established in a previous model development study. PancreaSure distinguished early-stage PDAC from controls with 76.5% sensitivity (95% CI, 67.7–83.9), significantly higher than the performance target (p = 0.005). PancreaSure achieved 87.8% specificity (95% CI, 83.9–91.4), similar to the performance goal, and significantly outperformed sensitivity of CA 19-9 alone (p = 0.02). These results confirm that PancreaSure performs well at detecting early-stage PDAC in high-risk individuals.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
Open AccessArticle
Electronic Health Literacy, Psychological Distress, and Quality of Life in Urological Cancer Patients: A Longitudinal Study During Transition from Inpatient to Outpatient Care
by
Dominik Fugmann, Steffen Holsteg, Ralf Schäfer, Günter Niegisch, Ulrike Dinger and André Karger
Curr. Oncol. 2025, 32(11), 637; https://doi.org/10.3390/curroncol32110637 - 13 Nov 2025
Abstract
Urological cancers are associated with reduced quality of life and high psychological burden, yet affected patients receive less psychosocial support than other cancer groups. Electronic health literacy (eHL) may facilitate independent access to resources, but its role for psychological outcomes and quality of
[...] Read more.
Urological cancers are associated with reduced quality of life and high psychological burden, yet affected patients receive less psychosocial support than other cancer groups. Electronic health literacy (eHL) may facilitate independent access to resources, but its role for psychological outcomes and quality of life in this group is unclear. This study examined associations between eHL, psychological symptoms, and quality of life during transition from inpatient to outpatient care. A prospective, single-centre observational study was conducted. Eligible inpatients (urological cancer, Distress Thermometer ≥5 and/or request for psycho-oncological support) received an initial psycho-oncology consultation and completed surveys during inpatient treatment (T1) and three months later (T2). Measures included socio-demographics, PO-BADO, eHL (eHEALS), distress, depression (PHQ-2), anxiety (GAD-2), and quality of life (EORTC QLQ-C30). Of 108 patients completing T1, 71 completed T2. After controlling for age, eHL was not significantly associated with distress, depression, anxiety, or quality of life. Age did not moderate these relationships. In this sample, eHL showed no significant associations with psychological outcomes or quality of life. However, higher age was linked to lower eHL, suggesting that older patients may face barriers to digital health engagement. Age-related differences in eHL should be considered when designing digital support services for urological cancer patients.
Full article
(This article belongs to the Special Issue Psychological Interventions for Cancer Survivors)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- Current Oncology Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal Browser-
arrow_forward_ios
Forthcoming issue
arrow_forward_ios Current issue - Volumes not published by MDPI
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Cancers, IJMS, Pharmaceuticals, Pharmaceutics, Sci. Pharm., Current Oncology, Molecules
Recent Advances in Anticancer Strategies, 2nd Edition
Topic Editors: Hassan Bousbaa, Zhiwei HuDeadline: 31 March 2026
Topic in
Brain Sciences, Cancers, JCM, Neurology International, Diagnostics, Therapeutics, Current Oncology
Innovations in Brain Tumor Surgery: Techniques and Outcomes
Topic Editors: Maria Caffo, Teresa SommaDeadline: 30 June 2026
Topic in
Cancers, Current Oncology, JCM, Medicina, Onco
Cancer Biology and Radiation Therapy: 2nd Edition
Topic Editors: Chang Ming Charlie Ma, Ka Yu Tse, Ming-Yii Huang, Mukund SeshadriDeadline: 25 July 2026
Topic in
Cancers, Diagnostics, Gastrointestinal Disorders, JCM, Current Oncology
Metastatic Colorectal Cancer: From Laboratory to Clinical Studies, 2nd Edition
Topic Editors: Ioannis Ntanasis-Stathopoulos, Diamantis I. TsilimigrasDeadline: 20 August 2026

Conferences
Special Issues
Special Issue in
Current Oncology
Therapeutic Advances in Cystectomy for Bladder Cancer
Guest Editor: Saum B. GhodoussipourDeadline: 30 November 2025
Special Issue in
Current Oncology
Resistance to Chemotherapy and Targeted Therapy in Cancer: Understanding the Pathogenesis and Identifying the Best Approaches to Overcome This Challenge
Guest Editor: Oudai HassanDeadline: 30 November 2025
Special Issue in
Current Oncology
Hype or Hope—Combination Therapies for Lung Cancer
Guest Editor: Daniel BreadnerDeadline: 30 November 2025
Special Issue in
Current Oncology
Advancements in Thyroid Cancer Management
Guest Editor: Leonardo RossiDeadline: 30 November 2025
Topical Collections
Topical Collection in
Current Oncology
New Insights into Prostate Cancer Diagnosis and Treatment
Collection Editor: Sazan Rasul
Topical Collection in
Current Oncology
New Insights into Breast Cancer Diagnosis and Treatment
Collection Editors: Filippo Pesapane, Matteo Suter
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series in "Exercise and Cancer Management"
Collection Editors: Linda Denehy, Ravi Mehrotra, Nicole Culos-Reed
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series: Contemporary Perioperative Concepts in Cancer Surgery
Collection Editors: Vijaya Gottumukkala, Jörg Kleeff