Electronic Health Literacy, Psychological Distress, and Quality of Life in Urological Cancer Patients: A Longitudinal Study During Transition from Inpatient to Outpatient Care
Simple Summary
Abstract
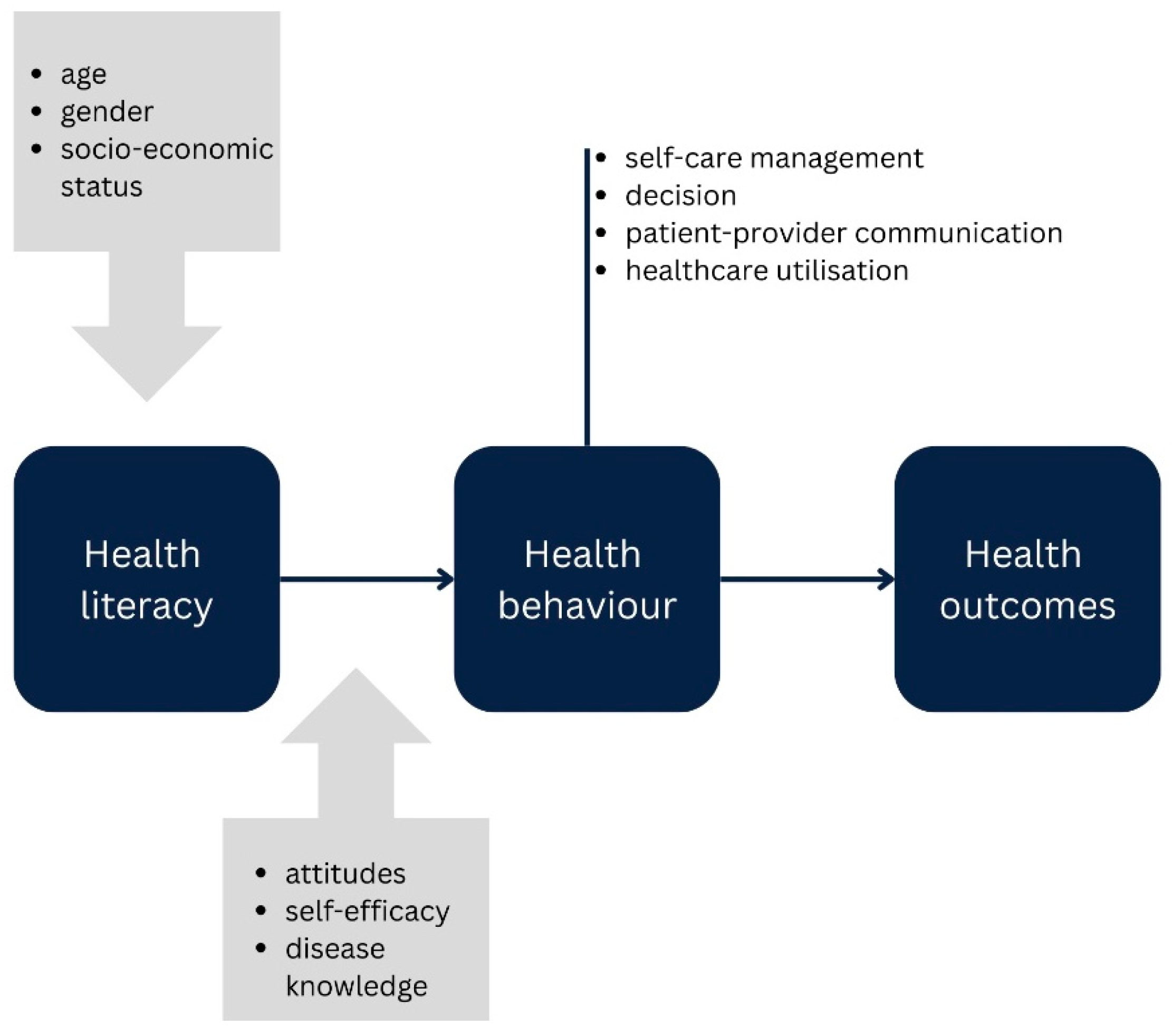
1. Introduction
2. Materials and Methods
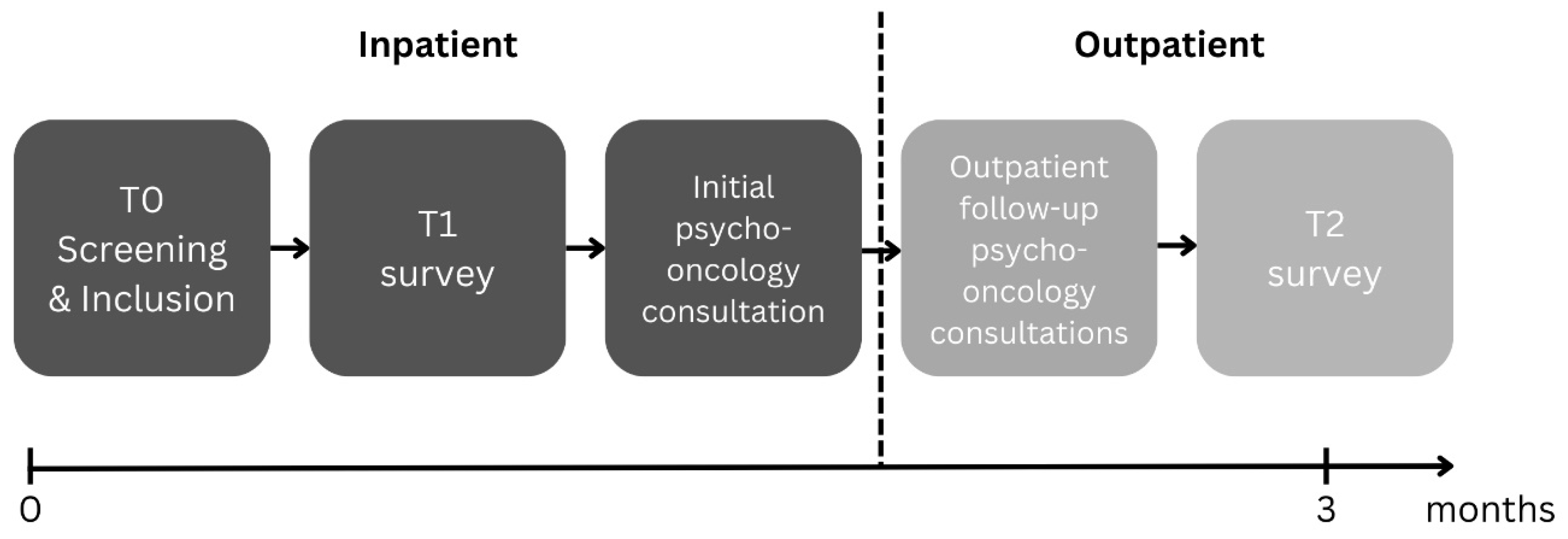
2.1. Study Design and Participants
2.2. Instruments
2.3. Statistical Analysis
3. Results
3.1. Sample and Dataset Generation
3.2. Sample Characteristics
3.3. Group Differences by Electronic Health Literacy
3.4. Age as Moderator
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DT | Distress Thermometer |
| ECOG | Eastern Cooperative Oncology Group Performance Status |
| eHEALS | Electronic health literacy survey |
| eHL | Electronic health literacy |
| EORTC | European Organisation for Research and Treatment of Cancer |
| GAD | Generalised anxiety disorder |
| HL | Patient group with high electronic health literacy |
| LL | Patient group with low electronic health literacy |
| PHQ | Patient health questionnaire |
| PO-BADO | Basic Documentation for Psycho-Oncology |
References
- Cancer Today, Globocan 2022 (Version 1.1). World Health Organization. 2024. Available online: https://gco.iarc.who.int/media/globocan/factsheets/populations/900-world-fact-sheet.pdf (accessed on 24 March 2025).
- Alam, R.; Patel, S.H.; Kates, M.R.; Singla, N.; Pavlovich, C.P.; Allaf, M.E.; Bivalacqua, T.J.; Pierorazio, P.M. Differential changes in self-reported quality of life in elderly populations after diagnosis of a genitourinary malignancy. Urol. Oncol. Semin. Orig. Investig. 2022, 40, 455.e1–455.e10. [Google Scholar] [CrossRef]
- Anderson, D.; Razzak, A.N.; McDonald, M.; Cao, D.; Hasoon, J.; Viswanath, O.; Kaye, A.D.; Urits, I. Mental Health in Urologic Oncology. Health Psychol. Res. 2022, 10, 37518. [Google Scholar] [CrossRef]
- Weis, J.; Hönig, K.; Bergelt, C.; Faller, H.; Brechtel, A.; Hornemann, B.; Stein, B.; Teufel, M.; Goerling, U.; Erim, Y.; et al. Psychosocial distress and utilization of professional psychological care in cancer patients: An observational study in National Comprehensive Cancer Centers (CCCs) in Germany. Psycho-Oncology 2018, 27, 2847–2854. [Google Scholar] [CrossRef] [PubMed]
- Stengel, A.; Dinkel, A.; Karger, A.; Kusch, M.; Hentschel, L.; Herschbach, P.; Hönig, K.; Hornemann, B.; Maatouk, I.; Senf, B.; et al. Best Practice: Psychoonkologisches Screening an Comprehensive Cancer Centers. Forum 2021, 36, 278–283. [Google Scholar] [CrossRef]
- Breidenbach, C.; Kowalski, C.; Ansmann, L.; Schult, S.; Sibert, N.T.; Neupert, I.; Zimmermann, T.; Wesselmann, S. Incorporating psychosocial care into routine oncological care: Insights into challenges and strategies from certified cancer centers’ audit data. Psycho-Oncology 2022, 31, 1331–1339. [Google Scholar] [CrossRef]
- Sender, A.; Friedrich, M.; Leuteritz, K.; Stuckenberg, E.; Richter, D.; Stöbel-Richter, Y.; Lordick, F.; Geue, K. Psychosocial aftercare of adolescent and young adult cancer survivors in Germany: Awareness, utilisation, satisfaction and associated factors. Psycho-Oncology 2021, 30, 1311–1321. [Google Scholar] [CrossRef] [PubMed]
- Norman, C.D.; A Skinner, H. eHEALS: The eHealth Literacy Scale. J. Med. Internet Res. 2006, 8, e27. [Google Scholar] [CrossRef]
- On Behalf of Working Group Prevention and Integrative Oncology of the German Cancer Society; Heiman, H.; Keinki, C.; Huebner, J. EHealth literacy in patients with cancer and their usage of web-based information. J. Cancer Res. Clin. Oncol. 2018, 144, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- Slev, V.N.; Mistiaen, P.; Pasman, H.R.W.; Leeuw, I.M.V.-D.; van Uden-Kraan, C.F.; Francke, A.L. Effects of eHealth for patients and informal caregivers confronted with cancer: A meta-review. Int. J. Med. Inform. 2016, 87, 54–67. [Google Scholar] [CrossRef]
- van Deursen, L.; Versluis, A.; van der Vaart, R.; Standaar, L.; Struijs, J.; Chavannes, N.; Aardoom, J.J. eHealth Interventions for Dutch Cancer Care: Systematic Review Using the Triple Aim Lens. JMIR Cancer 2022, 8, e37093. [Google Scholar] [CrossRef]
- Huang, G.; Wu, R.; Xu, X.; Song, Y.; Zheng, R.; Chen, X.; Hong, J. Effect of eHealth Interventions on Body Image of Patients with Cancer: Systematic Review. J. Med. Internet Res. 2025, 27, e55564. [Google Scholar] [CrossRef]
- Singleton, A.C.; Raeside, R.; Hyun, K.K.; Partridge, S.R.; Di Tanna, G.L.; Hafiz, N.; Tu, Q.; Tat-Ko, J.; Sum, S.C.M.; Sherman, K.A.; et al. Electronic Health Interventions for Patients With Breast Cancer: Systematic Review and Meta-Analyses. J. Clin. Oncol. 2022, 40, 2257–2270. [Google Scholar] [CrossRef]
- Jackson, S.R.; Yu, P.; Armany, D.; Occhipinti, S.; Chambers, S.; Leslie, S.; Patel, M.I. eHealth literacy in prostate cancer: A systematic review. Patient Educ. Couns. 2024, 123, 108193. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Mishel, M.; Bensen, J.T.; Chen, R.C.; Knafl, G.J.; Blackard, B.; Farnan, L.; Fontham, E.; Su, L.J.; Brennan, C.S.; et al. How does health literacy affect quality of life among men with newly diagnosed clinically localized prostate cancer? Cancer 2011, 118, 3842–3851. [Google Scholar] [CrossRef] [PubMed]
- Keles, A.; Kose, M.; Somun, U.F.; Culpan, M.; Yaksi, N.; Yıldırım, A. Impact of health and digital health literacy on quality of life following radical prostatectomy for prostate cancer: Prospective single-center cohort study. World J. Urol. 2024, 42, 241. [Google Scholar] [CrossRef]
- Qan’Ir, Y.; Song, L. Systematic review of technology-based interventions to improve anxiety, depression, and health-related quality of life among patients with prostate cancer. Psycho-Oncology 2019, 28, 1601–1613. [Google Scholar] [CrossRef] [PubMed]
- Forbes, C.C.; Finlay, A.; McIntosh, M.; Siddiquee, S.; Short, C.E. A systematic review of the feasibility, acceptability, and efficacy of online supportive care interventions targeting men with a history of prostate cancer. J. Cancer Surviv. 2019, 13, 75–96. [Google Scholar] [CrossRef]
- Fugmann, D.; Holsteg, S.; Schäfer, R.; Kreuznacht, L.; Speer, D.; Niegisch, G.; Dinger, U.; Karger, A. Use of Follow-Up Psycho-Oncology Consultations in Urological Cancer after Transition from Inpatient to Outpatient Care. Oncol. Res. Treat. 2024, 48, 4–13. [Google Scholar] [CrossRef]
- Huang, Y.; Qi, F.; Wang, R.; Jia, X.; Wang, Y.; Lin, P.; Geng, M.; Li, S. The effect of health literacy on health status among residents in Qingdao, China: A path analysis. Environ. Health Prev. Med. 2021, 26, 78. [Google Scholar] [CrossRef]
- Sun, S.; Lu, J.; Wang, Y.; Wang, Y.; Wu, L.; Zhu, S.; Zheng, X.; Lu, X.; Xu, H. Gender differences in factors associated with the health literacy of hospitalized older patients with chronic diseases: A cross-sectional study. Front. Public Health 2022, 10, 944103. [Google Scholar] [CrossRef]
- Liu, Y.-B.; Liu, L.; Li, Y.-F.; Chen, Y.-L. Relationship between Health Literacy, Health-Related Behaviors and Health Status: A Survey of Elderly Chinese. Int. J. Environ. Res. Public Health 2015, 12, 9714–9725. [Google Scholar] [CrossRef]
- McAnally, K.; Hagger, M.S. Health literacy, social cognition constructs, and health behaviors and outcomes: A meta-analysis. Health Psychol. 2023, 42, 213–234. [Google Scholar] [CrossRef]
- Mehnert, A.; Müller, D.; Lehmann, C.; Koch, U. Die deutsche Version des NCCN Distress-Thermometers. Z. Fur Psychiatr. Psychol. Und Psychother. 2006, 54, 213–223. [Google Scholar] [CrossRef]
- Study Protocol: Use and Acceptance of Psycho-Oncological Online Help for Urogenital Cancers. 2021. German Clinical Trials Register. Available online: https://www.drks.de/search/de/trial/DRKS00024012/details (accessed on 31 March 2025).
- Herschbach, P.; Book, K.; Brandl, T.; Keller, M.; Marten-Mittag, B. The Basic Documentation for Psycho-Oncology (PO-Bado)—An Expert Rating Scale for the Psychosocial Experience of Cancer Patients. Oncol. Res. Treat. 2008, 31, 591–596. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; De Haes, J.C.J.M.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A Quality-of-Life Instrument for Use in International Clinical Trials in Oncology. JNCI J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Psych: Procedures for Psychological, Psychometric, and Personality Research. Available online: https://personality-project.org/r/psych/psych-manual.pdf (accessed on 31 March 2025).
- Halwas, N.; Griebel, L.; Huebner, J. eHealth literacy, Internet and eHealth service usage: A survey among cancer patients and their relatives. J. Cancer Res. Clin. Oncol. 2017, 143, 2291–2299. [Google Scholar] [CrossRef]
- Hoogland, A.I.; Mansfield, J.; Lafranchise, E.A.; Bulls, H.W.; Johnstone, P.A.; Jim, H.S. eHealth literacy in older adults with cancer. J. Geriatr. Oncol. 2020, 11, 1020–1022. [Google Scholar] [CrossRef]
- De Santis, K.K.; Jahnel, T.; Sina, E.; Wienert, J.; Zeeb, H. Digitization and Health in Germany: Cross-sectional Nationwide Survey. JMIR Public Health Surveill. 2021, 7, e32951. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, N.E.; Herrera, P.C.; Hudson, S.; Revenson, T.A.; Lee, C.T.; Quale, D.Z.; Zarcadoolas, C.; Hall, S.J.; Diefenbach, M.A. Muscle Invasive Bladder Cancer: Examining Survivor Burden and Unmet Needs. J. Urol. 2014, 191, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Derry, H.M.; Reid, M.C.; Prigerson, H.G. Advanced cancer patients’ understanding of prognostic information: Applying insights from psychological research. Cancer Med. 2019, 8, 4081–4088. [Google Scholar] [CrossRef] [PubMed]
- van der Vaart, R.; Drossaert, C. Development of the Digital Health Literacy Instrument: Measuring a Broad Spectrum of Health 1.0 and Health 2.0 Skills. J. Med. Internet Res. 2017, 19, e27. [Google Scholar] [CrossRef]
- Liu, H.-X.; Chow, B.-C.; Liang, W.; Hassel, H.; Huang, Y.W. Measuring a Broad Spectrum of eHealth Skills in the Web 3.0 Context Using an eHealth Literacy Scale: Development and Validation Study. J. Med. Internet Res. 2021, 23, e31627. [Google Scholar] [CrossRef]
- Cai, W.; Liang, W.; Liu, H.; Zhou, R.; Zhang, J.; Zhou, L.; Su, N.; Zhu, H.; Yang, Y. Electronic Health Literacy Scale-Web3.0 for Older Adults with Noncommunicable Diseases: Validation Study. J. Med. Internet Res. 2024, 26, e52457. [Google Scholar] [CrossRef]
- Galinkala, P.; Atkinson, E.; Campos-Castillo, C. Age Variation Among US Adults’ Social Media Experiences and Beliefs About Who Is Responsible for Reducing Health-Related Falsehoods: Secondary Analysis of a National Survey. JMIR Aging 2024, 7, e56761. [Google Scholar] [CrossRef]
- Zhang, C.; Mohamad, E.; Azlan, A.A.; Wu, A.; Ma, Y.; Qi, Y. Social Media and eHealth Literacy Among Older Adults: Systematic Literature Review. J. Med. Internet Res. 2025, 27, e66058. [Google Scholar] [CrossRef]

| Total (n = 108) | LH (n = 35) | HH (n = 72) | Between Groups | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Levels | M | SD | M | SD | M | SD | W | p | ||
| Age | Years | 58.53 | 17.16 | 64.17 | 15.88 | 56.14 | 17.09 | 907 | 0.019 | * | |
| eHealth literacy | eHEALS score | 26.95 | 7.95 | 17.51 | 5.39 | 31.58 | 3.89 | ||||
| N | % | N | % | N | % | χ2 | df | p | |||
| Partner | Yes | 77 | 71.30 | 25 | 71.43 | 52 | 72.22 | ||||
| No | 30 | 27.78 | 9 | 25.71 | 20 | 27.78 | |||||
| Unknown | 1 | 0.93 | 1 | 2.86 | 0 | 0 | 0.437 | ||||
| Sex | Male | 96 | 88.89 | 28 | 80.00 | 67 | 93.06 | ||||
| Female | 12 | 11.11 | 7 | 20.00 | 5 | 6.94 | 0.056 | ||||
| Education | ≤10 years | 54 | 50.00 | 23 | 65.71 | 31 | 43.06 | ||||
| >10 years | 50 | 46.30 | 12 | 34.29 | 37 | 51.39 | |||||
| n.a. | 4 | 3.70 | 0 | 0 | 4 | 5.56 | 2989 | 1 | 0.084 | ||
| Cancer type | Prostate | 33 | 30.56 | 10 | 28.57 | 23 | 31.94 | ||||
| Bladder | 26 | 24.07 | 13 | 37.14 | 13 | 18.06 | |||||
| Penis | 4 | 3.70 | 0 | 0 | 4 | 5.56 | |||||
| Testicular | 25 | 23.15 | 5 | 14.29 | 19 | 26.39 | |||||
| Kidney | 20 | 18.52 | 7 | 20.00 | 13 | 18.06 | 0.149 | ||||
| Metastases | Yes | 38 | 35.19 | 12 | 34.29 | 25 | 34.72 | ||||
| No | 54 | 50.00 | 15 | 42.86 | 39 | 54.17 | |||||
| Unknown | 15 | 13.89 | 8 | 22.86 | 7 | 9.72 | |||||
| n.a. | 1 | 0.93 | 0 | 0 | 1 | 1.39 | 0.186 | ||||
| Treatments in the past two months | Operation | 70 | 64.81 | 24 | 68.57 | 45 | 62.50 | 0.160 | 1 | 0.689 | |
| Chemotherapy | 29 | 26.58 | 9 | 25.71 | 19 | 26.39 | <0.001 | 1 | 1 | ||
| Radiotherapy | 4 | 3.70 | 1 | 2.86 | 3 | 4.17 | 1 | ||||
| Hormone therapy | 3 | 2.78 | 0 | 0 | 3 | 4.17 | 0.549 | ||||
| None | 20 | 18.52 | 6 | 17.14 | 14 | 19.44 | <0.001 | 1 | 0.982 | ||
| Performance status † | Low impairment | 79 | 73.15 | 22 | 62.86 | 56 | 77.78 | ||||
| High impairment | 26 | 24.07 | 13 | 37.14 | 13 | 18.06 | |||||
| n.a. | 3 | 2.78 | 0 | 0 | 3 | 4.17 | 3230 | 1 | 0.072 | ||
| History of psychological or psychiatric treatment | Yes | 33 | 30.56 | 10 | 28.57 | 23 | 31.94 | ||||
| No | 73 | 67.59 | 25 | 71.43 | 47 | 65.28 | |||||
| n.a. | 2 | 1.85 | 0 | 0 | 2 | 2.78 | 0.050 | 1 | 0.824 | ||
| Request for support (T0) | Yes | 83 | 76.85 | 28 | 80.00 | 54 | 75.00 | ||||
| No | 13 | 12.04 | 3 | 8.57 | 10 | 13.89 | |||||
| Not Specified | 11 | 10.19 | 3 | 8.57 | 8 | 11.11 | |||||
| n.a. | 1 | 0.93 | 1 | 2.56 | 0 | 0 | 0.717 | ||||
| Use of follow-up psycho-oncology consultations | Yes | 24 | 22.22 | 10 | 28.57 | 14 | 19.44 | ||||
| No | 84 | 77.78 | 25 | 71.43 | 58 | 80.56 | 0.664 | 1 | 0.415 | ||
| Group Comparison (Wilcoxon Rank Sum Test) | Group Comparison (Age-Adjusted via Residuals) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | LH | HH | Between Groups | LH | HH | Between Groups | |||||||||||||||
| Variable | N | M | SD | N | M | SD | N | M | SD | W | p | r | SD | MD | SD | MD | W | p | r | ||
| T1 | Distress Thermometer | 107 | 6.61 | 2.55 | 35 | 7.26 | 2.41 | 71 | 6.35 | 2.55 | 1536 | 0.047 | * | 0.19 | 2.38 | 0.64 | 2.55 | 0.64 | 1279 | 0.809 | 0.02 |
| Depression (PHQ-2) | 108 | 2.23 | 1.87 | 35 | 3.00 | 1.93 | 72 | 1.89 | 1.73 | 1683 | 0.004 | ** | 0.28 | 1.92 | −0.05 | 1.72 | <−0.01 | 1290 | 0.845 | 0.02 | |
| Anxiety (GAD-2) | 108 | 2.12 | 1.60 | 35 | 2.29 | 1.51 | 72 | 2.06 | 1.66 | 1401 | 0.342 | 0.09 | 1.48 | 0.01 | 1.64 | −0.18 | 1252 | 0.960 | <0.01 | ||
| Physical functioning | 103 | 71.07 | 30.42 | 35 | 56.76 | 31.53 | 68 | 78.43 | 27.24 | 742 | 0.001 | ** | 0.31 | 29.57 | 0.12 | 27.04 | 15.74 | 1204 | 0.925 | 0.01 | |
| Role functioning | 106 | 64.15 | 39.29 | 35 | 50.95 | 36.81 | 71 | 70.66 | 39.08 | 890 | 0.013 | * | 0.24 | 36.81 | −16.97 | 38.80 | 23.31 | 1218 | 0.872 | 0.02 | |
| Cognitive functioning | 107 | 74.61 | 27.22 | 35 | 61.90 | 29.31 | 72 | 80.79 | 24.01 | 778 | <0.001 | *** | 0.32 | 28.93 | 3.82 | 23.95 | 4.71 | 1206 | 0.722 | 0.03 | |
| Emotional functioning | 105 | 52.78 | 25.23 | 35 | 42.14 | 16.78 | 70 | 58.10 | 27.10 | 769 | 0.002 | ** | 0.30 | 16.76 | −0.86 | 27.06 | 3.27 | 1270 | 0.762 | 0.03 | |
| Social functioning | 107 | 69.16 | 30.18 | 35 | 61.90 | 30.94 | 72 | 72.69 | 29.38 | 989 | 0.064 | 0.18 | 28.98 | 5.86 | 29.28 | 7.60 | 1253 | 0.966 | <0.01 | ||
| Quality of life | 107 | 47.98 | 28.66 | 35 | 36.19 | 28.72 | 72 | 53.70 | 27.01 | 812 | 0.003 | ** | 0.29 | 27.85 | −12.08 | 26.95 | 2.15 | 1343 | 0.584 | 0.05 | |
| T2 | Distress Thermometer | 62 | 4.23 | 2.58 | 14 | 4.14 | 1.75 | 48 | 4.25 | 2.79 | 341 | 0.939 | 0.01 | 1.69 | −0.08 | 2.79 | −0.70 | 327 | 0.886 | 0.02 | |
| Depression (PHQ-2) | 68 | 1.65 | 1.31 | 16 | 1.88 | 1.26 | 52 | 1.58 | 1.33 | 477 | 0.370 | 0.09 | 1.23 | −0.14 | 1.33 | 0.32 | 437 | 0.767 | 0.04 | ||
| Anxiety (GAD-2) | 69 | 1.41 | 1.45 | 17 | 1.53 | 1.50 | 52 | 1.37 | 1.44 | 478 | 0.613 | 0.05 | 1.47 | −0.48 | 1.41 | −0.27 | 437 | 0.950 | <0.01 | ||
| Physical functioning | 71 | 74.37 | 26.13 | 17 | 58.82 | 28.21 | 54 | 79.26 | 23.66 | 263 | 0.007 | ** | 0.26 | 26.99 | 2.13 | 22.65 | 8.40 | 475 | 0.835 | 0.02 | |
| Role functioning | 70 | 65.48 | 30.47 | 17 | 53.92 | 31.47 | 53 | 69.18 | 29.49 | 319 | 0.066 | 0.18 | 31.45 | −2.66 | 28.29 | 2.58 | 452 | 0.989 | <0.01 | ||
| Cognitive functioning | 68 | 73.77 | 28.55 | 16 | 68.75 | 31.55 | 52 | 75.32 | 27.71 | 369 | 0.483 | 0.07 | 31.43 | 7.20 | 27.66 | 6.31 | 368 | 0.492 | 0.08 | ||
| Emotional functioning | 67 | 65.17 | 27.75 | 17 | 61.76 | 24.48 | 50 | 66.33 | 28.91 | 366 | 0.397 | 0.08 | 23.26 | 3.05 | 28.91 | 8.72 | 452 | 0.703 | 0.05 | ||
| Social functioning | 66 | 75.25 | 28.68 | 16 | 62.50 | 34.69 | 50 | 79.33 | 25.55 | 290 | 0.085 | 0.17 | 34.25 | 9.68 | 25.10 | 3.88 | 388 | 0.863 | 0.02 | ||
| Quality of life | 69 | 61.35 | 23.04 | 17 | 52.45 | 19.93 | 52 | 64.26 | 23.42 | 296 | 0.041 | * | 0.20 | 19.26 | −0.36 | 21.76 | 0.22 | 456 | 0.851 | 0.02 | |
| Domain | Main Effect eHEALS | Main Effect Age | Inter- Action Effect | SE Inter- Action | p Value Interaction | CI Lower | CI Upper | |
|---|---|---|---|---|---|---|---|---|
| T1 | Distress thermometer | 0.79 | 0 | 0.02 | 0.03 | 0.539 | −0.04 | 0.08 |
| Depression (PHQ-2) | 1.10 | 0.01 | −0.01 | 0.02 | 0.585 | −0.06 | 0.03 | |
| Anxiety (GAD-2) | 0.36 | −0.01 | 0 | 0.02 | 0.910 | −0.04 | 0.04 | |
| Physical functioning | −17.67 | −0.19 | −0.51 | 0.36 | 0.168 | −1.22 | 0.21 | |
| Role functioning | −19.23 | −0.27 | 0.32 | 0.49 | 0.521 | −0.65 | 1.29 | |
| Cognitive functioning | −17.03 | −0.1 | −0.20 | 0.33 | 0.551 | −0.85 | 0.45 | |
| Emotional functioning | −16.44 | 0.09 | −0.04 | 0.32 | 0.899 | −0.66 | 0.58 | |
| Social functioning | −14.84 | 0.14 | 0.54 | 0.38 | 0.157 | −0.20 | 1.28 | |
| Quality of life | −14.84 | −0.11 | −0.34 | 0.35 | 0.345 | −1.03 | 0.36 | |
| T2 | Distress thermometer | −0.22 | −0.01 | 0.04 | 0.05 | 0.482 | −0.07 | 0.14 |
| Depression (PHQ-2) | 0.40 | 0 | −0.02 | 0.02 | 0.389 | −0.07 | 0.03 | |
| Anxiety (GAD-2) | 0.35 | −0.02 | 0 | 0.03 | 0.943 | −0.05 | 0.05 | |
| Physical functioning | −16.05 | −0.40 | −0.14 | 0.44 | 0.750 | −1.01 | 0.73 | |
| Role functioning | −13.77 | −0.49 | 0.41 | 0.54 | 0.454 | −0.66 | 1.48 | |
| Cognitive functioning | −7.51 | −0.09 | 0.27 | 0.54 | 0.617 | −0.78 | 1.32 | |
| Emotional functioning | −7.70 | −0.03 | 0.54 | 0.52 | 0.306 | −0.48 | 1.56 | |
| Social functioning | −18.67 | −0.28 | 0.63 | 0.52 | 0.227 | −0.38 | 1.65 | |
| Quality of life | −8.50 | −0.50 | 0.16 | 0.40 | 0.686 | −0.61 | 0.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fugmann, D.; Holsteg, S.; Schäfer, R.; Niegisch, G.; Dinger, U.; Karger, A. Electronic Health Literacy, Psychological Distress, and Quality of Life in Urological Cancer Patients: A Longitudinal Study During Transition from Inpatient to Outpatient Care. Curr. Oncol. 2025, 32, 637. https://doi.org/10.3390/curroncol32110637
Fugmann D, Holsteg S, Schäfer R, Niegisch G, Dinger U, Karger A. Electronic Health Literacy, Psychological Distress, and Quality of Life in Urological Cancer Patients: A Longitudinal Study During Transition from Inpatient to Outpatient Care. Current Oncology. 2025; 32(11):637. https://doi.org/10.3390/curroncol32110637
Chicago/Turabian StyleFugmann, Dominik, Steffen Holsteg, Ralf Schäfer, Günter Niegisch, Ulrike Dinger, and André Karger. 2025. "Electronic Health Literacy, Psychological Distress, and Quality of Life in Urological Cancer Patients: A Longitudinal Study During Transition from Inpatient to Outpatient Care" Current Oncology 32, no. 11: 637. https://doi.org/10.3390/curroncol32110637
APA StyleFugmann, D., Holsteg, S., Schäfer, R., Niegisch, G., Dinger, U., & Karger, A. (2025). Electronic Health Literacy, Psychological Distress, and Quality of Life in Urological Cancer Patients: A Longitudinal Study During Transition from Inpatient to Outpatient Care. Current Oncology, 32(11), 637. https://doi.org/10.3390/curroncol32110637





