Cancer Treatment Patterns Among Yukon Residents Referred to British Columbia for Care: A 13-Year Retrospective Study
Simple Summary
Abstract
1. Introduction
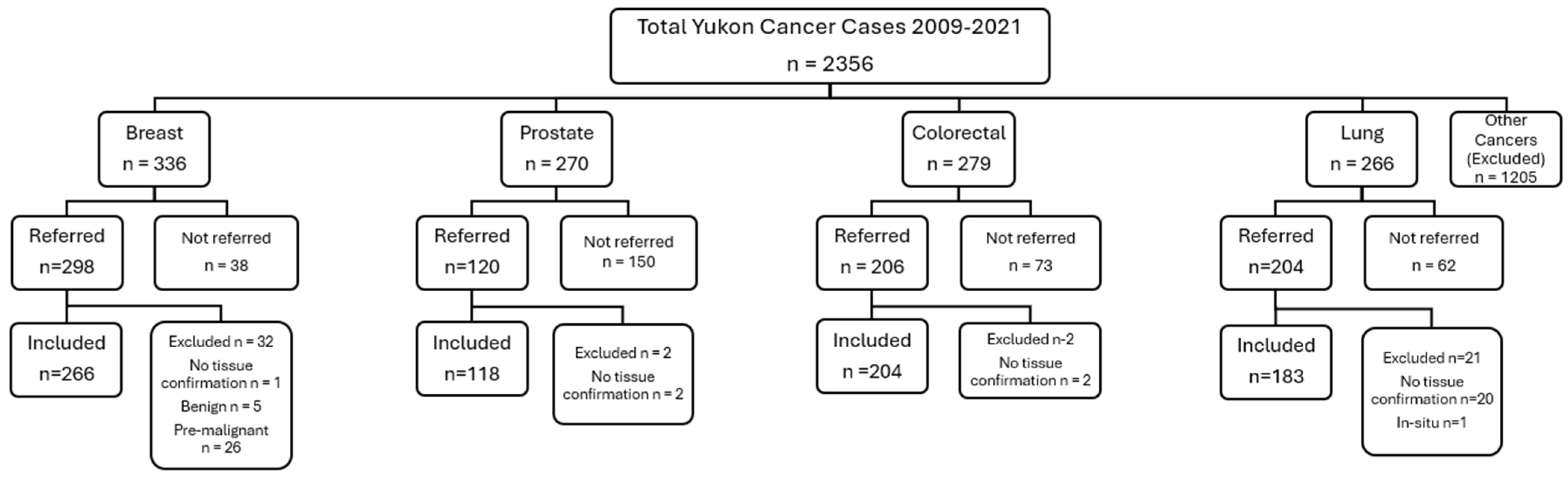
2. Materials and Methods
3. Results
3.1. Study Cohort Characteristics
3.2. Non-Referred Cases
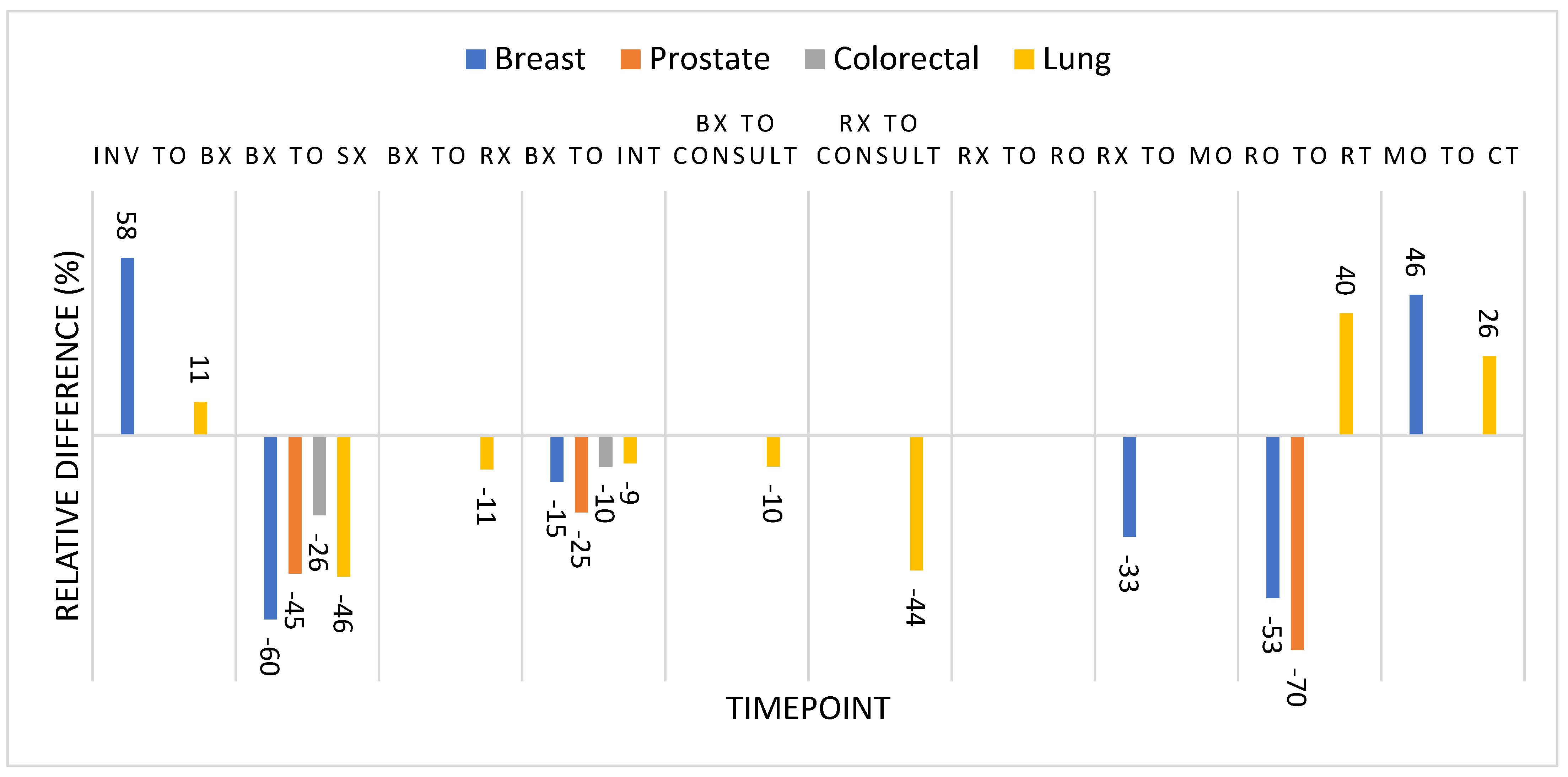
3.3. Timepoints of Cancer Care
4. Discussion
4.1. Referral Patterns
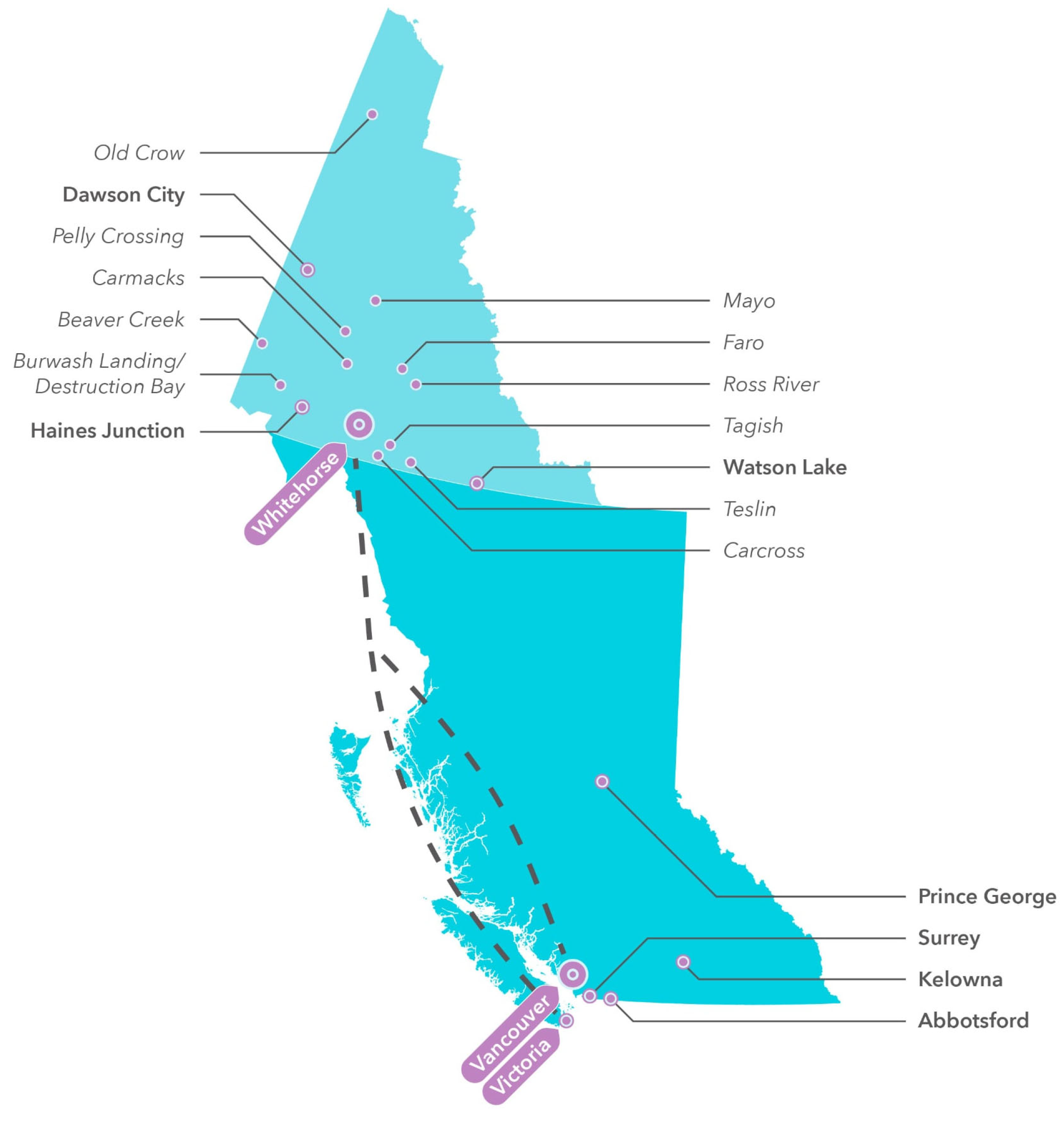
4.2. Geography
4.3. Timepoints
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BC | British Columbia |
| NSCLC | Non-small cell lung cancer |
| HER2 | Human epidermal growth factor receptor 2 |
| KRAS | Kirsten rat sarcoma virus |
| MMR | Mismatch repair |
| EGFR | Epidermal growth factor receptor |
| PDL1 | Programmed death ligand 1 |
| PSA | Prostate specific antigen |
| GPO | General Practitioners in Oncology |
References
- Government of Canada. Population Estimates on July 1, by Age and Gender. Statistics Canada. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501 (accessed on 23 November 2024).
- Department of Health and Social Services, Government of Yukon. Yukon Cancer Incidence Report 2009–2016. 2019. Available online: https://yukon.ca/sites/default/files/yukoncancerincidencereport.pdf (accessed on 23 November 2024).
- BC Cancer. Centre & Clinic Locations. Available online: http://www.bccancer.bc.ca/our-services/centres-clinics/locations (accessed on 23 November 2024).
- Yukon Hospital Corporation. Cancer Care|Yukon Hospital Corporation. Available online: https://yukonhospitals.ca/en/whitehorse-general-hospital/programs-and-services/cancer-care (accessed on 23 November 2024).
- Yukon Bureau of Statistics. Population Report First Quarter. 2021. Available online: https://yukon.ca/sites/default/files/ybs/populationq1_2021.pdf (accessed on 5 July 2025).
- Government of Canada. Population Growth in Canada’s Rural Areas, 2016 to 2021. Statistics Canada. Available online: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/98-200-x/2021002/98-200-x2021002-eng.cfm (accessed on 23 November 2024).
- Dixon, C. Cancer Care in the Northwest Territories. Can. Oncol. Nurs. J. 2024, 34, 574–577. [Google Scholar]
- Chan, J.; Linden, K.; McGrath, C.; Renaud, J.; Doering, P.; MacDonald, S.; Gaudet, M.; Pantarotto, J.R.; Asmis, T.; Slotman, B.; et al. Time to Diagnosis and Treatment with Palliative Radiotherapy among Inuit Patients with Cancer from the Arctic Territory of Nunavut, Canada. Clin. Oncol. 2020, 32, 60–67. [Google Scholar] [CrossRef]
- Canadian Partnership Against Cancer. Inuit Cancer Control in Canada Baseline Report. 2014. Available online: https://s22457.pcdn.co/wp-content/uploads/2018/12/inuit_cc_baseline_report_EN.pdf (accessed on 15 December 2024).
- Canadian Partnership Against Cancer. Examining Disparities in Cancer Control. 2014. Available online: https://s22457.pcdn.co/wp-content/uploads/2019/01/Examining-disparities-in-cancer-control-EN.pdf (accessed on 23 November 2024).
- Chan, J.; Friborg, J.; Chernov, M.; Cherkashin, M.; Grau, C.; Brundage, M.; Slotman, B. Access to Radiotherapy among Circumpolar Inuit Populations. Lancet Oncol. 2019, 20, e590–e600. [Google Scholar] [CrossRef]
- Gillan, C.; Briggs, K.; Goytisolo Pazos, A.; Maurus, M.; Harnett, N.; Catton, P.; Wiljer, D. Barriers to Accessing Radiation Therapy in Canada: A Systematic Review. Radiat. Oncol. 2012, 7, 167. [Google Scholar] [CrossRef]
- Governement of Yukon. Find Out Which Medical Travel Costs Our Health Plan Covers. Available online: https://yukon.ca/en/medical-treatment-travel (accessed on 2 January 2025).
- Government of Canada; Indigenous Services. Medical Transportation Benefits for First Nations and Inuit. Available online: https://www.sac-isc.gc.ca/eng/1574177172364/1574177196509 (accessed on 2 January 2025).
- Government of Canada. The Daily—Indigenous Population Continues to Grow and Is Much Younger than the Non-Indigenous Population, Although the Pace of Growth Has Slowed. Statistics Canada. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/220921/dq220921a-eng.htm (accessed on 23 November 2024).
- Horrill, T.C.; Linton, J.; Lavoie, J.G.; Martin, D.; Wiens, A.; Schultz, A.S.H. Access to Cancer Care among Indigenous Peoples in Canada: A Scoping Review. Soc. Sci. Med. 2019, 238, 112495. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.D.; Song, X.; Furgal, C.M. A Systematic Literature Review of Cancer Communication with Indigenous Populations in Canada and the United States. J. Canc. Educ. 2021, 36, 310–324. [Google Scholar] [CrossRef] [PubMed]
- Beckett, M.; Cole, K.; White, M.; Chan, J.; McVicar, J.; Rodin, D.; Clemons, M.; Bourque, J.-M. Decolonizing Cancer Care In Canada. J. Cancer Policy 2021, 30, 100309. [Google Scholar] [CrossRef]
- Carrière, G.M.; Tjepkema, M.; Pennock, J.; Goedhuis, N. Cancer Patterns in Inuit Nunangat: 1998–2007. Int. J. Circumpolar Health 2012, 71, 18581. [Google Scholar] [CrossRef]
- Galloway, T.; Horlick, S.; Cherba, M.; Cole, M.; Woodgate, R.L.; Healey Akearok, G. Perspectives of Nunavut Patients and Families on Their Cancer and End of Life Care Experiences. Int. J. Circumpolar Health 2020, 79, 1766319. [Google Scholar] [CrossRef]
- Government of Canada; Canadian Cancer Society. Canadian Cancer Statistics: A 2022 Special Report on Cancer Prevelance. Canadian Cancer Society. Available online: https://cdn.cancer.ca/-/media/files/research/cancer-statistics/2022-statistics/2022-special-report/2022_prevalence_report_final_en.pdf?rev=7755f9f350e845d58e268a59e3be608e&hash=3F3F30CADD8CAF0049636B5A41EDBB13&_gl=1*21rw8e*_ga*MTI5OTE3MTQ0Ni4xNjQzMzA0MDMz*_ga_23YMKBE2C3*MTY2NzkxMDY0My4zMTcuMS4xNjY3OTEwNjQ2LjU3LjAuMA. (accessed on 23 November 2024).
- Simkin, J.; Woods, R.; Elliott, C. Cancer Mortality in Yukon 1999–2013: Elevated Mortality Rates and a Unique Cancer Profile. Int. J. Circumpolar Health 2017, 76, 1324231. [Google Scholar] [CrossRef] [PubMed]
- BC Cancer. Referrals. Available online: https://www.bccancer.bc.ca:443/health-professionals/referrals (accessed on 2 November 2025).
- BC Cancer. Distribution of Cancer Cases Diagnosed in 2017, Referred to BC Cancer Within 1 Year of Diagnosis Date By Cancer Subgroup and BC Cancer Centre. 2019. Available online: http://www.bccancer.bc.ca/statistics-and-reports-site/Documents/referral_rates_2017_20200309.pdf (accessed on 23 November 2024).
- Asmis, T.R.; Febbraro, M.; Alvarez, G.G.; Spaans, J.N.; Ruta, M.; Lalany, A.; Osborne, G.; Goss, G.D. A Retrospective Review of Cancer Treatments and Outcomes among Inuit Referred from Nunavut, Canada. Curr. Oncol. 2015, 22, 246–251. [Google Scholar] [CrossRef]
- Government of Yukon. Find information on Colon Cancer. Government of Yukon. Available online: https://yukon.ca/colon-check (accessed on 23 November 2024).
- Simkin, J.; Ogilvie, G.; Hanley, B.; Elliott, C. Differences in Colorectal Cancer Screening Rates across Income Strata by Levels of Urbanization: Results from the Canadian Community Health Survey (2013/2014). Can. J. Public Health 2018, 110, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Kerner, J.; Liu, J.; Wang, K.; Fung, S.; Landry, C.; Lockwood, G.; Zitzelsberger, L.; Mai, V. Canadian Cancer Screening Disparities: A Recent Historical Perspective. Curr. Oncol. 2015, 22, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Faulds, J.; McGahan, C.E.; Phang, P.T.; Raval, M.J.; Brown, C.J. Differences between Referred and Nonreferred Patients in Cancer Research. Can. J. Surg. 2013, 56, E135–E141. [Google Scholar] [CrossRef] [PubMed]
- Nostedt, M.C.; McKay, A.M.; Hochman, D.J.; Wirtzfeld, D.A.; Yaffe, C.S.; Yip, B.; Silverman, R.; Park, J. The Location of Surgical Care for Rural Patients with Rectal Cancer: Patterns of Treatment and Patient Perspectives. Can. J. Surg. 2014, 57, 398–404. [Google Scholar] [CrossRef]
- El-Haouly, A.; Dragomir, A.; El-Rami, H.; Liandier, F.; Lacasse, A. Treatment Decision-Making in Men with Localized Prostate Cancer Living in a Remote Area: A Cross-Sectional, Observational Study. Can. Urol. Assoc. J. 2021, 15, E160–E168. [Google Scholar] [CrossRef]
- Government of Canada, S.C. Focus on Geography Series, 2016 Census—Yukon. Available online: https://www12.statcan.gc.ca/census-recensement/2016/as-sa/fogs-spg/Facts-PR-Eng.cfm?TOPIC=9&LANG=Eng&GK=PR&GC=60 (accessed on 5 July 2025).
- Fairchild, A.; Ghosh, S.; Baker, J. Patterns of Referral and Knowledge of Palliative Radiotherapy in Alberta. Can. Fam. Physician 2012, 58, e113–e122. [Google Scholar]
- Lengoc, S.; Soo, J.; McGahan, C.E.; French, J.; Tyldesley, S.; Olson, R. Referral Patterns of Patients for Palliative Radiation Therapy in British Columbia: A Comparison Between Rural and Urban Family Physicians. J. Med. Imaging Radiat. Sci. 2012, 43, 161–167. [Google Scholar] [CrossRef]
- Albers, P.; Huang, G.; Bashir, S.; Mookerji, N.; Bennett, J.; Broomfield, S.; Martín, A.M.; Ghosh, S.; Kinnaird, A. The Rural Disadvantage—Prostate Cancer Outcomes of Rural and Urban Patients over 25 Years. J. Rural. Health 2025, 41, e70008. [Google Scholar] [CrossRef]
- Santi, S.A.; Caswell, J.M.; Beruar, A.S.; Conlon, M.S.C.; Carlson, R.G.; Pearce, A.G. A Comparison Between the Rates of Radiation Oncologist and Urologist Consultations in Men Diagnosed With Prostate Cancer in Northern Ontario, Canada. Adv. Radiat. Oncol. 2023, 8, 101131. [Google Scholar] [CrossRef]
- Jooya, A.; Qureshi, D.; Phillips, W.J.; Leigh, J.; Webber, C.; Aggarwal, A.; Tanuseputro, P.; Morgan, S.; Macrae, R.; Ong, M.; et al. Variation in Access to Palliative Radiotherapy in Prostate Cancer: A Population-Based Study in Canada. Cureus 2024, 16, e54582. [Google Scholar] [CrossRef]
- Andkhoie, M.; Szafron, M. The Impact of Geographic Location on Saskatchewan Prostate Cancer Patient Treatment Choices: A Multilevel and Spatial Analysis. J. Rural. Health 2020, 36, 564–576. [Google Scholar] [CrossRef] [PubMed]
- Soo, J.; French, J.; McGahan, C.E.; Duncan, G.; Lengoc, S. A Retrospective Study on Accessibility of Palliative Radiation Therapy in the Management of Prostate Cancer in British Columbia. J. Radiother. Pract. 2011, 10, 159–172. [Google Scholar] [CrossRef]
- Tyldesley, S.; McGahan, C. Utilisation of Radiotherapy in Rural and Urban Areas in British Columbia Compared with Evidence-Based Estimates of Radiotherapy Needs for Patients with Breast, Prostate and Lung Cancer. Clin. Oncol. 2010, 22, 526–532. [Google Scholar] [CrossRef]
- Cho, C.-K.J.; Sunderland, K.; Pickles, T.; Bachand, F.; Chi, K.N.; Tyldesley, S. A Population-Based Study of Palliative Radiation Therapy for Bone Metastases in Patients Dying of Prostate Cancer. Pract. Radiat. Oncol. 2019, 9, e274–e282. [Google Scholar] [CrossRef]
- Quon, H.; Suderman, D.; Guilbert, K.; Lambert, P.; Bucher, O.; Ong, A.; Chowdhury, A. Population-Based Referrals for Adjuvant Radiotherapy After Radical Prostatectomy in Men With Prostate Cancer: Impact of Randomized Trials. Clin. Genitourin. Cancer 2014, 12, e1–e5. [Google Scholar] [CrossRef][Green Version]
- Cary, C.; Odisho, A.Y.; Cooperberg, M.R. Variation in Prostate Cancer Treatment Associated with Population Density of the County of Residence. Prostate Cancer Prostatic Dis. 2016, 19, 174–179. [Google Scholar] [CrossRef]
- Pandit, A.A.; Patil, N.N.; Mostafa, M.; Kamel, M.; Halpern, M.T.; Li, C. Rural-Urban Disparities in Patient Care Experiences among Prostate Cancer Survivors: A SEER-CAHPS Study. Cancers 2023, 15, 1939. [Google Scholar] [CrossRef]
- Baldwin, L.-M.; Andrilla, C.H.A.; Porter, M.P.; Rosenblatt, R.A.; Patel, S.; Doescher, M.P. Treatment of Early-Stage Prostate Cancer among Rural and Urban Patients. Cancer 2013, 119, 3067–3075. [Google Scholar] [CrossRef] [PubMed]
- Jackson, E.B.; Simmons, C.E.; Chia, S.K. Current Challenges and Disparities in the Delivery of Equitable Breast Cancer Care in Canada. Curr. Oncol. 2023, 30, 7263–7274. [Google Scholar] [CrossRef] [PubMed]
- Maddison, A.R.; Asada, Y.; Urquhart, R. Inequity in Access to Cancer Care: A Review of the Canadian Literature. Cancer Causes Control 2011, 22, 359–366. [Google Scholar] [CrossRef]
- Olson, R.A.; Nichol, A.; Caron, N.R.; Olivotto, I.A.; Speers, C.; Chia, S.; Davidson, A.; Coldman, A.; Bajdik, C.; Tyldesley, S. Effect of Community Population Size on Breast Cancer Screening, Stage Distribution, Treatment Use and Outcomes. Can. J. Public Health 2012, 103, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Cadili, L.; DeGirolamo, K.; Ma, C.S.-Y.; Chen, L.; McKevitt, E.; Pao, J.-S.; Dingee, C.; Bazzarelli, A.; Warburton, R. The Breast Cancer Patient Experience of Telemedicine During COVID-19. Ann. Surg. Oncol. 2022, 29, 2244–2252. [Google Scholar] [CrossRef] [PubMed]
- Weinerman, B.H.; Barnett, J.; Loyola, M.; den Duyf, J.; Robertson, S.; Ashworth, V.; Apland, L.; Kazanjian, A. Telehealth—A Change in a Practice Model in Oncology. Telemed. J. e-Health 2012, 18, 391–393. [Google Scholar] [CrossRef] [PubMed]
- Izadi-Najafabadi, S.; McTaggart-Cowan, H.; Halperin, R.; Lambert, L.; Mitton, C.; Peacock, S. The Impact of the COVID-19 Pandemic on Health-Related Quality of Life of Cancer Patients in British Columbia. J. Patient Rep. Outcomes 2024, 8, 100. [Google Scholar] [CrossRef]
- Izadi-Najafabadi, S.; McQuarrie, L.; Peacock, S.; Halperin, R.; Lambert, L.; Mitton, C.; McTaggart-Cowan, H. Cancer Patients’ Experiences with Telehealth before and during the COVID-19 Pandemic in British Columbia. Curr. Oncol. 2022, 29, 4199–4211. [Google Scholar] [CrossRef]
- Seto, E.; Smith, D.; Jacques, M.; Morita, P.P. Opportunities and Challenges of Telehealth in Remote Communities: Case Study of the Yukon Telehealth System. JMIR Med. Inform. 2019, 7, e11353. [Google Scholar] [CrossRef]
- Harnett, C.B.C. Premier Says Faster Progress Needed on Cancer Care Delivery. Times Colonist. Available online: https://www.timescolonist.com/local-news/premier-says-faster-progress-needed-on-cancer-care-delivery-8042767 (accessed on 23 November 2024).
- Wait Time Alliance. Unfinished Business Report Card on Wait Times in Canada. 2009. Available online: https://caro-acro.ca/wp-content/uploads/2016/10/Wait-Time-Alliance-Report-Card-1.pdf (accessed on 23 November 2024).
- Wong, F.; Manpower-and-Standards-of-Care-in-Radiation-Oncology-Committee-Definition-of-RT-Waiting-September-2000. Canadian Association of Radiation Oncologists. Available online: https://caro-acro.ca/wp-content/uploads/2016/10/Manpower-and-Standards-of-Care-in-Radiation-Oncology-Committee-Definition-of-RT-Waiting-September-2000.pdf (accessed on 23 November 2024).
- Moir, M.; Barua, B.; Waiting Your Turn: Wait Times for Health Care in Canada, 2022 Report. Fraser Institute. Available online: https://bit.ly/3I1dgRx (accessed on 23 November 2024).
- Canadian Partnership Against Cancer. Pan-Canadian Standards: Breast Cancer Surgery. 2019. Available online: https://s22457.pcdn.co/wp-content/uploads/2019/04/Breast-Cancer-Surgery-Standards-Reports-EN-2019.pdf (accessed on 23 November 2024).
- Prashad, A.; Mitchell, M.; Argent-Katwala, M.; Daly, C.; Earle, C.C.; Finley, C. Pan-Canadian Standards for Cancer Surgery. Can. J. Surg. 2019, 62 (Suppl. S3), S171–S183. [Google Scholar] [CrossRef]
- Chaudhry, M.; Kandasamy, S.; Habbous, S.; Chan, C.; Barisic, A.; Faisa, A.; Walker, M.; Haque, M.; Sheppard, A.; Uri, E.; et al. Cancer System Quality Index 2021: Ontario Cancer System Performance, 2021. Available online: https://ontariohealth.ca/content/dam/ontariohealth/documents/csqi-report-2021.pdf (accessed on 23 November 2024).
- Chiarelli, A.M.; Muradali, D.; Blackmore, K.M.; Smith, C.R.; Mirea, L.; Majpruz, V.; O’Malley, F.P.; Quan, M.L.; Holloway, C.M. Evaluating Wait Times from Screening to Breast Cancer Diagnosis among Women Undergoing Organised Assessment vs Usual Care. Br. J. Cancer 2017, 116, 1254–1263. [Google Scholar] [CrossRef]
- Plotogea, A.; Chiarelli, A.M.; Mirea, L.; Prummel, M.V.; Chong, N.; Shumak, R.S.; O’Malley, F.P.; Holloway, C.M.B. Factors Associated with Wait Times across the Breast Cancer Treatment Pathway in Ontario. Springerplus 2013, 2, 388. [Google Scholar] [CrossRef]
- Grunfeld, E.; Watters, J.M.; Urquhart, R.; O’Rourke, K.; Jaffey, J.; Maziak, D.E.; Morash, C.; Patel, D.; Evans, W.K. A Prospective Study of Peri-Diagnostic and Surgical Wait Times for Patients with Presumptive Colorectal, Lung, or Prostate Cancer. Br. J. Cancer 2009, 100, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Van de Vosse, D.; Chowdhury, R.; Boyce, A.; Halperin, R. Wait Times Experienced by Lung Cancer Patients in the BC Southern Interior to Obtain Oncologic Care: Exploration of the Intervals from First Abnormal Imaging to Oncologic Treatment. Cureus 2015, 7, e330. [Google Scholar] [CrossRef] [PubMed]
- Common, J.L.; Mariathas, H.H.; Parsons, K.; Greenland, J.D.; Harris, S.; Bhatia, R.; Byrne, S.C. Reducing Wait Time for Lung Cancer Diagnosis and Treatment: Impact of a Multidisciplinary, Centralized Referral Program. Can. Assoc. Radiol. J. 2018, 69, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Byrne, S.C.; Barrett, B.; Bhatia, R. The Impact of Diagnostic Imaging Wait Times on the Prognosis of Lung Cancer. Can. Assoc. Radiol. J. 2015, 66, 53–57. [Google Scholar] [CrossRef]
- Denault, M.-H.; Labbé, C.; St-Pierre, C.; Fournier, B.; Gagné, A.; Morillon, C.; Joubert, P.; Simard, S.; Martel, S. Wait Times and Survival in Lung Cancer Patients across the Province of Quebec, Canada. Curr. Oncol. 2022, 29, 3187–3199. [Google Scholar] [CrossRef]
| Breast n = 266 | Prostate n = 118 | Colorectal n = 204 | Lung n = 183 | |||||
|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||
| Male | 0 | 0.0% | 118 | 100.0% | 119 | 58.3% | 99 | 54.1% |
| Female | 266 | 100.0% | 0 | 0.0% | 85 | 41.7% | 84 | 45.9% |
| Yukon Residence | ||||||||
| Whitehorse | 189 | 71.1% | 79 | 66.9% | 137 | 67.2% | 119 | 65.0% |
| Other | 77 | 28.9% | 39 | 33.1% | 67 | 32.8% | 64 | 35.0% |
| Age | ||||||||
| Mean | 59 | 67 | 64 | 68 | ||||
| Median | 59 | 67 | 64 | 68 | ||||
| Min | 27 | 51 | 26 | 47 | ||||
| Max | 95 | 84 | 98 | 89 | ||||
| BC Cancer Referral Site | ||||||||
| Vancouver | 234 | 88.0% | 106 | 89.8% | >198 | >97% | 169 | 92.3% |
| Other | 32 | 12.0% | 12 | 10.2% | <5 | <3% | 14 | 8.7% |
| Year of Diagnosis | ||||||||
| 2009–2010 | 40 | 15.0% | 25 | 21.2% | 20 | 9.8% | 35 | 19.1% |
| 2011–2012 | 36 | 13.5% | 20 | 16.9% | 23 | 11.3% | 21 | 11.5% |
| 2013–2014 | 35 | 13.2% | 23 | 19.5% | 26 | 12.7% | 27 | 14.8% |
| 2015–2016 | 56 | 21.1% | 8 | 6.8% | 33 | 16.2% | 33 | 18.0% |
| 2017–2019 | 63 | 23.7% | 29 | 24.6% | 64 | 31.4% | 43 | 23.5% |
| 2020–2021 | 36 | 13.5% | 13 | 11.0% | 38 | 18.6% | 24 | 13.1% |
| Stage | ||||||||
| Early | 247 | 92.9% | 97 | 82.2% | 147 | 72.1% | 84 | 45.9% |
| Late | 19 | 7.1% | 21 | 17.8% | 57 | 27.9% | 99 | 54.1% |
| Histologic Subtype | ||||||||
| Adeno | 118 | 100.0% | 204 | 100.0% | ||||
| IDC | 238 | 89.5% | ||||||
| ILC | 28 | 10.5% | ||||||
| Non-squam | 106 | 57.9% | ||||||
| Squamous | 42 | 23.0% | ||||||
| SCLC | 35 | 19.1% | ||||||
| Grade | ||||||||
| I | 54 | 20.3% | 18 | 8.8% | <5 | <3% | ||
| II | >125 | >47% | 109 | 53.4% | 8 | 4.4% | ||
| III | 81 | 30.5% | 18 | 8.8% | 15 | 8.2% | ||
| unknown | <5 | <2% | 5 | 4.2% | 59 | 28.9% | >155 | >85% |
| Low (≤6) | 5 | 4.2% | ||||||
| (3 + 4) | 38 | 32.2% | ||||||
| (4 + 3) | 19 | 16.1% | ||||||
| High (≥8) | 51 | 43.2% | ||||||
| Surgery | ||||||||
| Yes | 253 | 95.1% | 41 | 34.7% | 149 | 73.0% | 27 | 14.8% |
| No | 13 | 4.9% | 77 | 65.3% | 55 | 27.0% | 156 | 85.2% |
| Surgery Type (Colorectal only) | ||||||||
| HC | 60 | 40.3% | ||||||
| LAR | 20 | 13.4% | ||||||
| TME | 18 | 12.1% | ||||||
| APR | 11 | 7.4% | ||||||
| Other | 40 | 26.8% | ||||||
| Chemotherapy | ||||||||
| Yes | 125 | 47.0% | <5 | <4% | 127 | 62.3% | 80 | 43.7% |
| No | 141 | 53.0% | >113 | >96% | 77 | 37.7% | 103 | 56.3% |
| Chemotherapy Total Courses | ||||||||
| 133 | <5 | 159 | 83 | |||||
| Chemotherapy Course Intent | ||||||||
| Curative | 100 | 75.2% | 0 | 0.0% | 93 | 58.5% | 27 | 32.5% |
| Palliative | 33 | 24.8% | <5 | 100.0% | 66 | 41.5% | 56 | 67.5% |
| Chemotherapy Number of Lines of Palliative Courses | ||||||||
| Mean | 1.2 | 0.1 | 1.2 | 0.6 | 0.3% | |||
| Median | 1 | 1 | 1 | 1 | 0.5% | |||
| Max | 4 | 1 | 5 | 4 | 2.2% | |||
| Hormone Therapy | ||||||||
| Yes | 204 | 76.7% | 74 | 62.7% | ||||
| No | 17 | 6.4% | 44 | 37.3% | ||||
| N/A | 42 | 15.8% | 0 | 0.0% | 204 | 100.0% | 183 | 100.0% |
| unknown | 3 | 1.1% | 0 | 0.0% | ||||
| Targeted Therapy | ||||||||
| Yes | 37 | 13.9% | 0 | 0.0% | 43 | 21.1% | 9 | 4.9% |
| No | 229 | 86.1% | 118 | 100.0% | 161 | 78.9% | 174 | 95.1% |
| Immunotherapy | ||||||||
| Yes | 0 | 0.0% | 0 | 0.0% | <5 | <3% | 18 | 9.8% |
| No | 266 | 100.0% | 118 | 100.0% | >199 | >97% | 165 | 90.2% |
| Radiotherapy | ||||||||
| Yes | 153 | 57.5% | 87 | 73.7% | 61 | 29.9% | 125 | 68.3% |
| No | 113 | 42.5% | 31 | 26.3% | 143 | 70.1% | 58 | 31.7% |
| Radiotherapy Total Completed Courses | ||||||||
| 296 | 137 | 95 | 202 | |||||
| Radiotherapy Course Intent | ||||||||
| Curative | 258 | 87.2% | 97 | 70.8% | 66 | 69.5% | 40 | 19.8% |
| Palliative | 38 | 12.8% | 40 | 29.2% | 29 | 30.5% | 162 | 80.2% |
| Radiotherapy Course Treatment Site | ||||||||
| Local/regional | 262 | 88.5% | 105 | 76.6% | 63 | 66.3% | 102 | 50.5% |
| Distant | 34 | 11.5% | 32 | 23.4% | 32 | 33.7% | 100 | 49.5% |
| All | Breast | Prostate | Colorectal | Lung | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-referred cases | 323 | 38 | 150 | 73 | 62 | |||||
| Sex | ||||||||||
| Male | 223 | 69.0% | 0 | 0% | 150 | 100% | 44 | 60.3% | 29 | 46.8% |
| Female | 100 | 31.0% | 38 | 100% | 0 | 0% | 29 | 39.7% | 33 | 53.2% |
| Yukon Residence | ||||||||||
| Whitehorse | 216 | 66.9% | 23 | 60.5% | 99 | 66.0% | 48 | 65.8% | 46 | 74.2% |
| Other | 90 | 27.9% | 7 | 18.4% | >45 | >30.0% | >20 | >27% | >10 | >16% |
| Unknown | 17 | 5.3% | 8 | 21.1% | <5 | <3% | <5 | <7% | <5 | <8% |
| Age | ||||||||||
| Mean | 68 | 66 | 67 | 68 | 69 | |||||
| Median | 68 | 64 | 67 | 68 | 71 | |||||
| Minimum | 32 | 37 | 48 | 32 | 40 | |||||
| Maximum | 91 | 91 | 87 | 87 | 86 | |||||
| Not referred with known stage at diagnosis | 250 | 25 | 120 | 57 | 48 | |||||
| Early-stage | 153 | 61.2% | 20 | 80.0% | 68 | 56.7% | 40 | 70.2% | 25 | 52.1% |
| Late-stage | 97 | 38.8% | 5 | 20.0% | 52 | 43.3% | 17 | 29.8% | 23 | 47.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Willemsma, K.; Simkin, J.; Lee, D.; Quinn, E.; Makuk, K.; Jackson, E.B.; Bang, A.; Chahal, M.; Wang, Y.; Chan, J. Cancer Treatment Patterns Among Yukon Residents Referred to British Columbia for Care: A 13-Year Retrospective Study. Curr. Oncol. 2025, 32, 641. https://doi.org/10.3390/curroncol32110641
Willemsma K, Simkin J, Lee D, Quinn E, Makuk K, Jackson EB, Bang A, Chahal M, Wang Y, Chan J. Cancer Treatment Patterns Among Yukon Residents Referred to British Columbia for Care: A 13-Year Retrospective Study. Current Oncology. 2025; 32(11):641. https://doi.org/10.3390/curroncol32110641
Chicago/Turabian StyleWillemsma, Kaylie, Jonathan Simkin, Debon Lee, Emma Quinn, Kira Makuk, Emily B. Jackson, Andrew Bang, Manik Chahal, Ying Wang, and Jessica Chan. 2025. "Cancer Treatment Patterns Among Yukon Residents Referred to British Columbia for Care: A 13-Year Retrospective Study" Current Oncology 32, no. 11: 641. https://doi.org/10.3390/curroncol32110641
APA StyleWillemsma, K., Simkin, J., Lee, D., Quinn, E., Makuk, K., Jackson, E. B., Bang, A., Chahal, M., Wang, Y., & Chan, J. (2025). Cancer Treatment Patterns Among Yukon Residents Referred to British Columbia for Care: A 13-Year Retrospective Study. Current Oncology, 32(11), 641. https://doi.org/10.3390/curroncol32110641





