- Article
Invasive Fungal Infections During Extracorporeal Membrane Oxygenation: A Case Series from Intensive Care Unit and Literature Review
- Francesca Serapide,
- Riccardo Serraino and
- Alessandro Russo
- + 8 authors
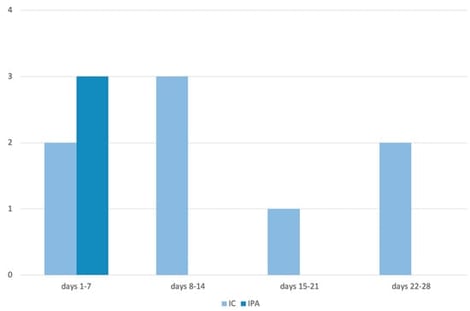
Background: Extracorporeal membrane oxygenation (ECMO) support is associated with potentially life-threatening complications, among which nosocomial infections play a significant role. The increasing incidence of fungi as causative agents of ECMO-associated infections is a growing concern. Methods: This case series includes all patients admitted to the Intensive Care Unit (ICU) of the “Renato Dulbecco” Teaching Hospital in Catanzaro who developed invasive fungal infections (IFIs) during ECMO support. Results: Of the 70 patients, 15.7% (N = 11) developed IFIs during ECMO. Among these, 91% (N = 10) died, while one patient survived and was discharged. Of the IFIs, 72.7% (N = 8) were cases of invasive candidiasis (IC), and 18.2% (N = 2) were cases of invasive pulmonary aspergillosis (IPA). One patient developed both IC and IPA during ECMO treatment. Additionally, 54.5% (N = 6) of the patients with IFIs also had bacterial co-infections, most of which were caused by multidrug-resistant (MDR) Gram-negative bacteria. Conclusions: This study highlights the high incidence and mortality of IFIs in ECMO patients. It underscores the urgent need for clear definitions, better diagnostic strategies, pharmacokinetic data on antifungal therapies, and the implementation of therapeutic drug monitoring (TDM) to optimize outcomes in this vulnerable population.
7 February 2026