Factors Influencing Stroke Severity Based on Collateral Circulation, Clinical Markers and Machine Learning
Abstract
1. Introduction
- •
- Confirmed that unilateral–bilateral stroke classification is a critical prognostic determinant, providing new evidence on the importance of lesion laterality in outcome prediction.
- •
- Demonstrated that insufficient or absent collateral circulation is strongly associated with greater stroke severity, emphasizing the clinical relevance of collateral status in acute stroke evaluation.
- •
- Showed that under small and imbalanced sample conditions, SMOTE combined with tree-based models yields the most robust and reliable predictive performance, offering practical methodological guidance for modeling in limited clinical datasets.
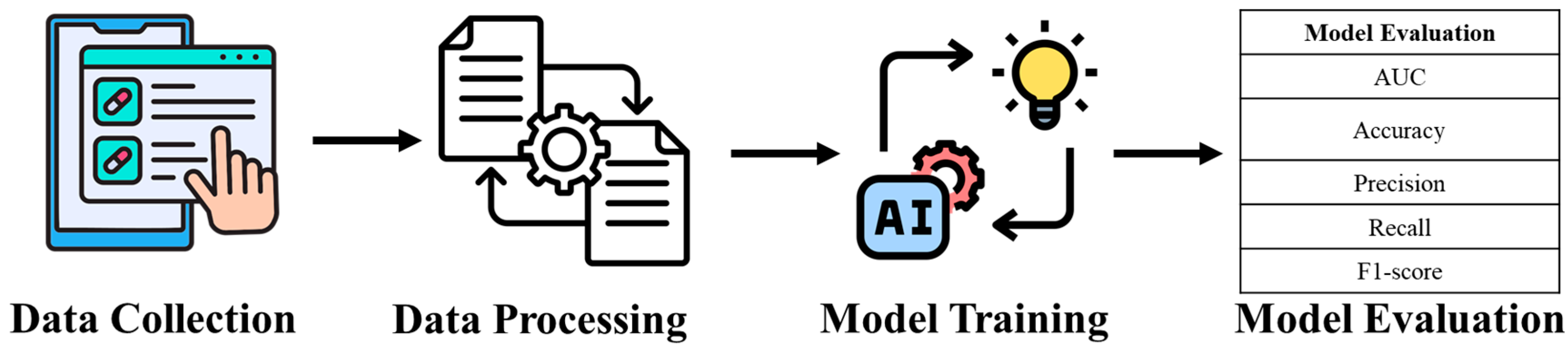
2. Materials and Methods
2.1. Ethical Approval
2.2. Study Setting, Design, and Ethical Considerations
2.3. Experimental Environment
2.4. Statistical Analysis
2.5. Model Training
3. Results
Descriptive Statistic
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnson, W.; Onuma, O.; Owolabi, M.; Sachdev, S. Stroke: A global response is needed. Bull. World Health Organ. 2016, 94, 634. [Google Scholar] [CrossRef]
- Hsieh, F.I.; Chiou, H.Y. Stroke: Morbidity, risk factors, and care in Taiwan. J. Stroke 2014, 16, 59. [Google Scholar] [CrossRef]
- Chang, Y.J.; Lin, S.K.; Ryu, S.J.; Wai, Y.Y. Common carotid artery occlusion: Evaluation with duplex sonography. Am. J. Neuroradiol. 1995, 16, 1099–1105. [Google Scholar] [PubMed]
- Gupta, A.; Gialdini, G.; Lerario, M.P.; Baradaran, H.; Giambrone, A.; Navi, B.B.; Marshall, R.S.; Iadecola, C.; Kamel, H. Magnetic resonance angiography detection of abnormal carotid artery plaque in patients with cryptogenic stroke. J. Am. Heart Assoc. 2015, 4, e002012. [Google Scholar] [CrossRef]
- Hedera, P.; Bujdakova, J.; Traubner, P.; Pancak, J. Stroke risk factors and development of collateral flow in carotid occlusive disease. Acta Neurol. Scand. 1998, 98, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Wu, O.; Cloonan, L.; Mocking, S.J.; Bouts, M.J.; Copen, W.A.; Cougo-Pinto, P.T.; Fitzpatrick, K.; Kanakis, A.; Schaefer, P.W.; Rosand, J.; et al. Role of acute lesion topography in initial ischemic stroke severity and long-term functional outcomes. Stroke 2015, 46, 2438–2444. [Google Scholar] [CrossRef] [PubMed]
- Døli, H.; Andersen Helland, W.; Helland, T.; Næss, H.; Hofstad, H.; Specht, K. Associations between stroke severity, aphasia severity, lesion location, and lesion size in acute stroke, and aphasia severity one year post stroke. Aphasiology 2023, 37, 307–329. [Google Scholar] [CrossRef]
- Tolles, J.; Meurer, W.J. Logistic regression: Relating patient characteristics to outcomes. Jama 2016, 316, 533–534. [Google Scholar] [CrossRef]
- Paciaroni, M.; RAF and ESTREM Studies Investigators. Risk of recurrence following acute cardioembolic stroke according to lesion size and NIHSS on admission. J. Neurol. Sci. 2025, 473, 123488. [Google Scholar] [CrossRef] [PubMed]
- Baud, J.; Stanciu, D.; Yeung, J.; Maurizot, A.; Chabay, S.; de Malherbe, M.; Chadenat, M.-L.; Bachelet, D.; Pico, F. Contrast enhanced ultrasound of carotid plaque in acute ischemic stroke (CUSCAS study). Rev. Neurol. 2021, 177, 115–123. [Google Scholar] [CrossRef]
- Hu, X.; Bao, Y.; Li, M.; Zhang, W.; Chen, C. The role of ferroptosis and its mechanism in ischemic stroke. Exp. Neurol. 2024, 372, 114630. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, F.; Duo, K.; Liu, Y.; Yu, J.; Wu, Q.; Cai, Z. The role of necroptosis in cerebral ischemic stroke. Mol. Neurobiol. 2024, 61, 3882–3898. [Google Scholar] [CrossRef]
- Ravindran, A.V.; Killingsworth, M.C.; Bhaskar, S. Cerebral collaterals in acute ischaemia: Implications for acute ischaemic stroke patients receiving reperfusion therapy. Eur. J. Neurosci. 2021, 53, 1238–1261. [Google Scholar] [CrossRef] [PubMed]
- Bąk, M.; Antończak, J.; Frąszczak, M.; Leus, M.; Mazgaj, M.; Gawłowicz, J.; Pietura, R. Assessment of collateral circulation in patients with anterior circulation stroke treated with mechanical thrombectomy as a predictor of long-term clinical outcomes. Acta Radiol. 2025, 66, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Crown, W.H. Real-world evidence, causal inference, and machine learning. Value Health 2019, 22, 587–592. [Google Scholar]
- Sinha, A.; Gupta, M.; Bhaskar, S.M. Evolucollateral dynamics in stroke: Evolutionary pathophysiology, remodelling and emerging therapeutic strategies. Eur. J. Neurosci. 2024, 60, 6779–6798. [Google Scholar] [CrossRef]
- Zikos, D.; DeLellis, N. CDSS-RM: A clinical decision support system reference model. BMC Med. Res. Methodol. 2018, 18, 137. [Google Scholar] [CrossRef]
- Huang, K.-Y.; Hsu, Y.-L.; Chung, C.-L.; Chen, H.-C.; Horng, M.-H.; Lin, C.-H.; Liu, C.-S.; Xu, J.-L. Enhancing healthcare AI stability with edge computing and machine learning for extubation prediction. Sci. Rep. 2025, 15, 17858. [Google Scholar] [CrossRef]
- Huang, K.-Y.; Hsu, Y.-L.; Chen, H.-C.; Horng, M.-H.; Chung, C.-L.; Lin, C.-H.; Xu, J.-L.; Hou, M.-H. Developing a machine-learning model for real-time prediction of successful extubation in mechanically ventilated patients using time-series ventilator-derived parameters. Front. Med. 2023, 10, 1167445. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Luo, X.-Y.; Chang, C.-H.; Kuo, C.-T.; Shih, S.-J.; Chang, M.-Y.; Weng, M.-R.; Chen, I.-C.; Hsu, Y.-L.; Xu, J.-L. Post-surgical fall risk prediction: A machine learning approach for spine and lower extremity procedures. Front. Med. 2025, 12, 1574305. [Google Scholar] [CrossRef]
- Chen, Y.H.; Xu, J.L. Applying artificial intelligence to predict falls for inpatient. Front. Med. 2023, 10, 1285192. [Google Scholar] [CrossRef]
- Su, P.Y.; Shih, H.J.; Xu, J.L. Rapid Liver Fibrosis Evaluation Using the UNet-ResNet50-32× 4d Model in Magnetic Resonance Elastography: Retrospective Study. JMIR Med. Inform. 2025, 13, e80351. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wen, Z.; Wang, Y.; Zhong, Y.; Wang, J.; Hu, Y.; Zhou, P.; Guo, S. Artificial intelligence in ischemic stroke images: Current applications and future directions. Front. Neurol. 2024, 15, 1418060. [Google Scholar] [CrossRef]
- Caliandro, P.; Lenkowicz, J.; Reale, G.; Scaringi, S.; Zauli, A.; Uccheddu, C.; Fabiole-Nicoletto, S.; Patarnello, S.; Damiani, A.; Tagliaferri, L.; et al. Artificial intelligence to predict individualized outcome of acute ischemic stroke patients: The SIBILLA project. Eur. Stroke J. 2024, 9, 1053–1062. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.I.; Bhatti, I.A.; Gillani, S.A.; Fakih, R.; Gomez, C.R.; Kwok, C.S. Factors and outcomes associated with National Institutes of Health stroke scale scores in acute ischemic stroke patients undergoing thrombectomy in United States. J. Stroke Cerebrovasc. Dis. 2025, 34, 108292. [Google Scholar] [CrossRef]
- Chu, T.; Guo, Z.; Zhang, Y.; Liu, Y.; Gu, Y. Study on the correlation between carotid plaque calcification types and acute ischemic stroke. Front. Neurol. 2025, 16, 1550014. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.; Nahar, K.M.O.; Gharaibeh, H.; Al Mamlook, R.E.; Nasayreh, A.; Atitallah, N.; Gharaibeh, A.; Hamad, R.; Abu Zitar, R.; Smerat, A.; et al. A Hybrid Brain Stroke Prediction Framework: Integrating Feature Selection, Classification, and Hyperparameter Optimization. Eng. Rep. 2025, 7, e70213. [Google Scholar] [CrossRef]
- Alabduljabbar, K.; Elabd, K.; Alsaif, A.; Basudan, L. Prevalence of stroke and associated risk factors among elderly patients in a primary care setting: A retrospective cohort study. J. Fam. Med. Prim. Care 2025, 14, 749–756. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Ho, T.K. Random decision forests. In Proceedings of the 3rd International Conference on Document Analysis and Recognition, Montreal, QC, Canada, 14–16 August 1995; Volume 1, pp. 278–282. [Google Scholar]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Ovbiagele, B.; Diener, H.-C.; Yusuf, S.; Martin, R.H.; Cotton, D.; Vinisko, R.; Donnan, G.A.; Bath, P.M.; for the PROFESS Investigators. Level of systolic blood pressure within the normal range and risk of recurrent stroke. Jama 2011, 306, 2137–2144. [Google Scholar] [CrossRef]
- Adams, H.P., Jr.; Davis, P.H.; Leira, E.C.; Chang, K.C.; Bendixen, B.H.; Clarke, W.R.; Woolson, R.F.; Hansen, M.D. Baseline NIH Stroke Scale score strongly predicts outcome after stroke: A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 1999, 53, 126. [Google Scholar] [CrossRef]
- Yin, H.C.; Lei, R.L.; Xu, J.L.; Lin, C.M.; Hsu, Y.L. Enhancing Stroke Prognosis Prediction Using Deep Convolution Neural Networks. J. Mech. Med. Biol. 2025, 25, 2540039. [Google Scholar] [CrossRef]
- Marilena, M.; Romana, P.F.; Guido, A.; Gianluca, D.R.; Sebastiano, F.; Enrico, P.; Sabrina, A. From “time is brain” to “time is collaterals”: Updates on the role of cerebral collateral circulation in stroke. J. Thromb. Thrombolysis 2025, 58, 821–832. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Vannan, M. It takes two to tango: Statistical modeling and machine learning. J. Glob. Sch. Mark. Sci. 2021, 31, 296–317. [Google Scholar] [CrossRef]
- Schaper, W. Collateral circulation: Past and present. Basic Res. Cardiol. 2009, 104, 5–21. [Google Scholar] [CrossRef]
- Rutgers, D.R.; Klijn, C.J.M.; Kappelle, L.J.; Van Der Grond, J. Recurrent stroke in patients with symptomatic carotid artery occlusion is associated with high-volume flow to the brain and increased collateral circulation. Stroke 2004, 35, 1345–1349. [Google Scholar] [CrossRef]
- Cheng, X.Q.; Tian, J.M.; Zuo, C.J.; Liu, J.; Zhang, Q.; Lu, G.M. Quantitative perfusion computed tomography measurements of cerebral hemodynamics: Correlation with digital subtraction angiography identified primary and secondary cerebral collaterals in internal carotid artery occlusive disease. Eur. J. Radiol. 2012, 81, 1224–1230. [Google Scholar] [CrossRef]
- Roka, A.; Landeta, J.; Webb, A.; Patel, S.; Banerjee, P.; Ganti, L. 345 Impact of Emergency Department Blood Pressure on Stroke Severity. Ann. Emerg. Med. 2018, 72, S136–S137. [Google Scholar] [CrossRef]
- Peng, R.; Liu, K.; Li, W.; Yuan, Y.; Niu, R.; Zhou, L.; Xiao, Y.; Gao, H.; Yang, H.; Zhang, C.; et al. Blood urea nitrogen, blood urea nitrogen to creatinine ratio and incident stroke: The Dongfeng-Tongji cohort. Atherosclerosis 2021, 333, 1–8. [Google Scholar] [CrossRef]
- Stead, L.G.; Enduri, S.; Bellolio, M.F.; Jain, A.R.; Vaidyanathan, L.; Gilmore, R.M.; Kashyap, R.; Weaver, A.L.; Brown, R.D. The impact of blood pressure hemodynamics in acute ischemic stroke: A prospective cohort study. Int. J. Emerg. Med. 2012, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic minority over-sampling technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- Autret, A.L.D.C.P.S.; Saudeau, D.; Bertrand, P.H.; Pourcelot, L.; Marchal, C.; De Boisvilliers, S. Stroke risk in patients with carotid stenosis. Lancet 1987, 329, 888–890. [Google Scholar] [CrossRef]
- Azar, A.S.; Samimi, T.; Tavassoli, G.; Naemi, A.; Rahimi, B.; Hadianfard, Z.; Wiil, U.K.; Nazarbaghi, S.; Mohasefi, J.B.; Afshar, H.L. Predicting stroke severity of patients using interpretable machine learning algorithms. Eur. J. Med. Res. 2024, 29, 547. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; He, J.; Tan, D.; Han, X.; Feng, R.; Xiong, H.; Peng, X.; Pu, X.; Zhang, L.; Li, Y.; et al. The clinical and imaging data fusion model for single-period cerebral CTA collateral circulation assessment. J. X-Ray Sci. Technol. 2024, 32, 953–971. [Google Scholar] [CrossRef]
- Ali, N.H.; Abdullah, A.R.; Saad, N.M.; Muda, A.S.; Noor, E.E.M. Automated classification of collateral circulation for ischemic stroke in cone-beam ct images using vgg11: A deep learning approach. BioMedInformatics 2024, 4, 1692–1702. [Google Scholar] [CrossRef]
- Scavasine, V.C.; Stoliar, G.A.; de Almeida Teixeira, B.C.; Zétola, V.D.H.F.; Lange, M.C. Automated evaluation of collateral circulation for outcome prediction in acute ischemic stroke. J. Stroke Cerebrovasc. Dis. 2024, 33, 107584. [Google Scholar] [CrossRef]
- Alemseged, F.; Rocco, A.; Arba, F.; Schwabova, J.P.; Wu, T.; Cavicchia, L.; Ng, F.; Ng, J.L.; Zhao, H.; Williams, C.; et al. Posterior National Institutes of Health Stroke Scale improves prognostic accuracy in posterior circulation stroke. Stroke 2022, 53, 1247–1255. [Google Scholar] [CrossRef]
- Chernykh, E.M.; Khasanova, N.M.; Karyakin, A.A.; Jafarova, Z.E.; Klyukas, A.A. Machine Learning for Predicting Early Functional Outcomes in Patients with Stroke. Physical and rehabilitation medicine. Med. Rehabil. 2025, 7, 82–94. [Google Scholar]

| Variables | Variables (91) | NIHSS Score > 16 | p-Value | |||
|---|---|---|---|---|---|---|
| 0 (66) | 1 (25) | |||||
| Personal Information | Sex-Man | 52 (57.14) | 37 (56.06) | 15 (60.00) | 0.735 | |
| Sex-Female | 39 (42.86) | 29 (43.94) | 10 (40.00) | |||
| Smoking | 25 (27.47) | 18 (27.47) | 7 (28.00) | 0.829 | ||
| Alcohol consumption | 17 (18.68) | 11 (16.67) | 6 (24.00) | 0.496 | ||
| Disease | Diabetes Mellitus (DM) | 22 (24.18) | 13 (19.70) | 9 (36.00) | 0.105 | |
| Hypertension (HTN) | 49 (53.85) | 36 (54.55) | 13 (52.00) | 0.828 | ||
| Mixed Hyperlipidemia | 13 (14.29) | 10 (15.15) | 3 (12.00) | 0.962 | ||
| Stroke history | 16 (17.58) | 12 (18.18) | 4 (16.00) | 0.918 | ||
| Atrial fibrillation AF | 24 (26.37) | 16 (24.24) | 8 (32.00) | 0.454 | ||
| Imaging Examination | Ipsilateral MCAS | 63 (69.23) | 47 (71.21) | 16 (64.00) | 0.506 | |
| Contralateral MCAS | 30 (32.97) | 16 (24.24) | 14 (56.00) | 0.004 | ||
| Unilateral–bilateral stroke | 90 (98.90) | 65 (98.48) | 25 (100.00) | 0.024 | ||
| Ipsilateral collateral circulation on MRA | 46 (50.55) | 38 (57.58) | 8 (32.00) | 0.021 | ||
| Personal information | Age | 65.16 (25–88) | 64.30 (25–87) | 60.77 (31–88) | 0.213 | |
| Systolic blood pressure | 165.70 (62–272) | 161.38 (112–272) | 187.56 (62–253) | 0.050 | ||
| Diastolic blood pressure | 87.00 (42–134) | 85.52 (48–134) | 90.92 (42–133) | 0.609 | ||
| Total cholesterol | 161.35 (11–265) | 159.94 (11–241) | 162.10 (95–265) | 0.505 | ||
| HsCRP | 5.15 (0.1–31.98) | 4.27 (0.1–21) | 7.77 (0.3–31.98) | 0.239 | ||
| BUN | 20.43 (6–98) | 19.91 (6–98) | 22.60 (11–59) | 0.074 | ||
| Creatinine | 0.96 (0.26–3.12) | 0.90 (0.26–3.12) | 0.94 (0.45–2.57) | 0.118 | ||
| Uric acid | 6.20 (2.5–66) | 6.29 (2.5–66) | 5.66 (3.6–9.2) | 0.106 | ||
| FPG | 144.24 (67–438) | 136.09 (67–321) | 153.08 (89–438) | 0.077 | ||
| Imaging Examination | CCA RI | Ipsilateral side | 0.81 (0.34–1) | 0.80 (0.34–1) | 0.84 (0.61–1) | 0.192 |
| Contralateral side | 0.81 (0.45–1) | 0.80 (0.45–1) | 0.85 (0.62–0.99) | 0.092 | ||
| ICA RI | Ipsilateral side | 0.73 (0.51–1.77) | 0.70 (0.52–1) | 0.74 (0.51–1) | 0.010 | |
| Contralateral side | 0.71 (0.41–1) | 0.70 (0.41–1) | 0.72 (0.5–0.89) | 0.086 | ||
| Plaque Index | Ipsilateral side | 2.30 (0–11) | 1.89 (0–11) | 2.54 (0–11) | 0.012 | |
| Contralateral side | 2.45 (0–10) | 2.15 (0–10) | 2.92 (0–8) | 0.061 | ||
| Variable | Non-Smote | Smote | ||||
|---|---|---|---|---|---|---|
| 0 (N = 66) | 1 (N = 25) | p-Value | 0 (N = 66) | 1 (N = 66) | p-Value | |
| Contralateral MCA stenosis (CTA) | 16 (24.24) | 14 (56.00) | 0.004 | 16 (24.24) | 25 (37.88) | 0.132 |
| Unilateral–bilateral stroke | 65 (98.48) | 25 (100.00) | 0.024 | 65 (98.48) | 66 (100.00) | 0.000 |
| Ipsilateral collateral flow (MRA) | 38 (57.58) | 8 (32.00) | 0.021 | 38 (57.58) | 12 (18.18) | 0.000 |
| SBP | 161.38 (112–272) | 187.56 (62–253) | 0.050 | 161.38 (112–272) | 171.86 (62–263) | 0.034 |
| BUN | 19.91 (6–98) | 22.60 (11–59) | 0.074 | 19.91 (6–98) | 20.14 (11–59) | 0.059 |
| FPG | 136.09 (67–321) | 153.08 (89–438) | 0.077 | 136.09 (67–321) | 153.73 (67–438) | 0.023 |
| Contralateral CCA resistance index | 0.80 (0.45–1) | 0.85 (0.62–0.99) | 0.092 | 0.80 (0.45–1) | 0.85 (0.62–1.0) | 0.001 |
| Ipsilateral ICA resistance index | 0.70 (0.52–1) | 0.74 (0.51–1) | 0.010 | 0.70 (0.52–1) | 0.79 (0.51–1.77) | 0.007 |
| Contralateral ICA resistance index | 0.70 (0.41–1) | 0.72 (0.5–0.89) | 0.086 | 0.70 (0.41–1) | 0.73 (0.5–0.91) | 0.297 |
| Plaque index (ipsilateral) | 1.89 (0–11) | 2.54 (0–11) | 0.012 | 1.89 (0–11) | 2.8 (0–11) | 0.002 |
| Plaque index (contralateral) | 2.15 (0–10) | 2.92 (0–8) | 0.061 | 2.15 (0–10) | 2.71 (0–9) | 0.066 |
| AUC | Accuracy | Precision | Recall | F1-Score | |
|---|---|---|---|---|---|
| Logictic Regression | 0.682 (CI: 0.605–0.759) | 69.1% (CI: 58.1–80.0%) | 49.7% (CI: 12.9–86.4%) | 24.0% (CI: 16.2–31.8%) | 30.3% (CI: 21.2–39.4%) |
| Random Forest | 0.682 (CI: 0.502–0.862) | 69.1% (CI: 58.3–80.0%) | 16.7% (CI: −12.6–45.9%) | 8.3% (CI: −6.3–23.0%) | 11.1% (CI: −8.4–30.6%) |
| XGBoost | 0.575 (CI: 0.412–0.738) | 64.8% (CI: 56.7–72.9%) | 22.0% (CI: −15.7–59.7%) | 16.7% (CI: −12.6–45.9%) | 18.9% (CI: −13.9–51.7%) |
| SVM | 0.432 (CI: 0.302–0.561) | 72.5% (CI: 65.2–79.7%) | NA | NA | NA |
| AUC | Accuracy | Precision | Recall | F1-Score | |
|---|---|---|---|---|---|
| Logistic Regression | 0.747 (CI: 0.588–0.905) | 71.3% (CI: 55.1–87.5%) | 71.2% (CI: 53.4–88.9%) | 70.7% (CI: 56.9–84.4%) | 70.8% (CI: 55.4–86.2%) |
| Random Forest | 0.94 (CI: 0.9–0.98) | 83.3% (CI: 79.1–87.6%) | 79.6% (CI: 71.6–87.7%) | 89.4% (CI: 81.8–97.1%) | 84.0% (CI: 79.1–88.9%) |
| XGBoost | 0.907 (CI: 0.847–0.966) | 80.2% (CI: 71.5–89.0%) | 78.3% (CI: 64.6–92.0%) | 86.6% (CI: 73.6–99.7%) | 81.4% (CI: 73.8–89.0%) |
| SVM | 0.398 (CI: 0.239–0.558) | 52.2% (CI: 37.5–67.0%) | 56.3% (CI: 38.2–74.4%) | 55.5% (CI: 20.9–90.1%) | 51.7% (CI: 36.6–66.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, J.-L. Factors Influencing Stroke Severity Based on Collateral Circulation, Clinical Markers and Machine Learning. Diagnostics 2025, 15, 2983. https://doi.org/10.3390/diagnostics15232983
Xu J-L. Factors Influencing Stroke Severity Based on Collateral Circulation, Clinical Markers and Machine Learning. Diagnostics. 2025; 15(23):2983. https://doi.org/10.3390/diagnostics15232983
Chicago/Turabian StyleXu, Jia-Lang. 2025. "Factors Influencing Stroke Severity Based on Collateral Circulation, Clinical Markers and Machine Learning" Diagnostics 15, no. 23: 2983. https://doi.org/10.3390/diagnostics15232983
APA StyleXu, J.-L. (2025). Factors Influencing Stroke Severity Based on Collateral Circulation, Clinical Markers and Machine Learning. Diagnostics, 15(23), 2983. https://doi.org/10.3390/diagnostics15232983





