Prevalence of Radial Artery Variants and Their Relationship with Clinical Considerations of the Antebrachial Region: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Electronic Search
2.4. Study Selection
2.5. Data Collection Process
2.6. Assessment of the Methodological Quality of the Included Studies
2.7. Statistical Methods
2.8. Subgroup Analysis
3. Results
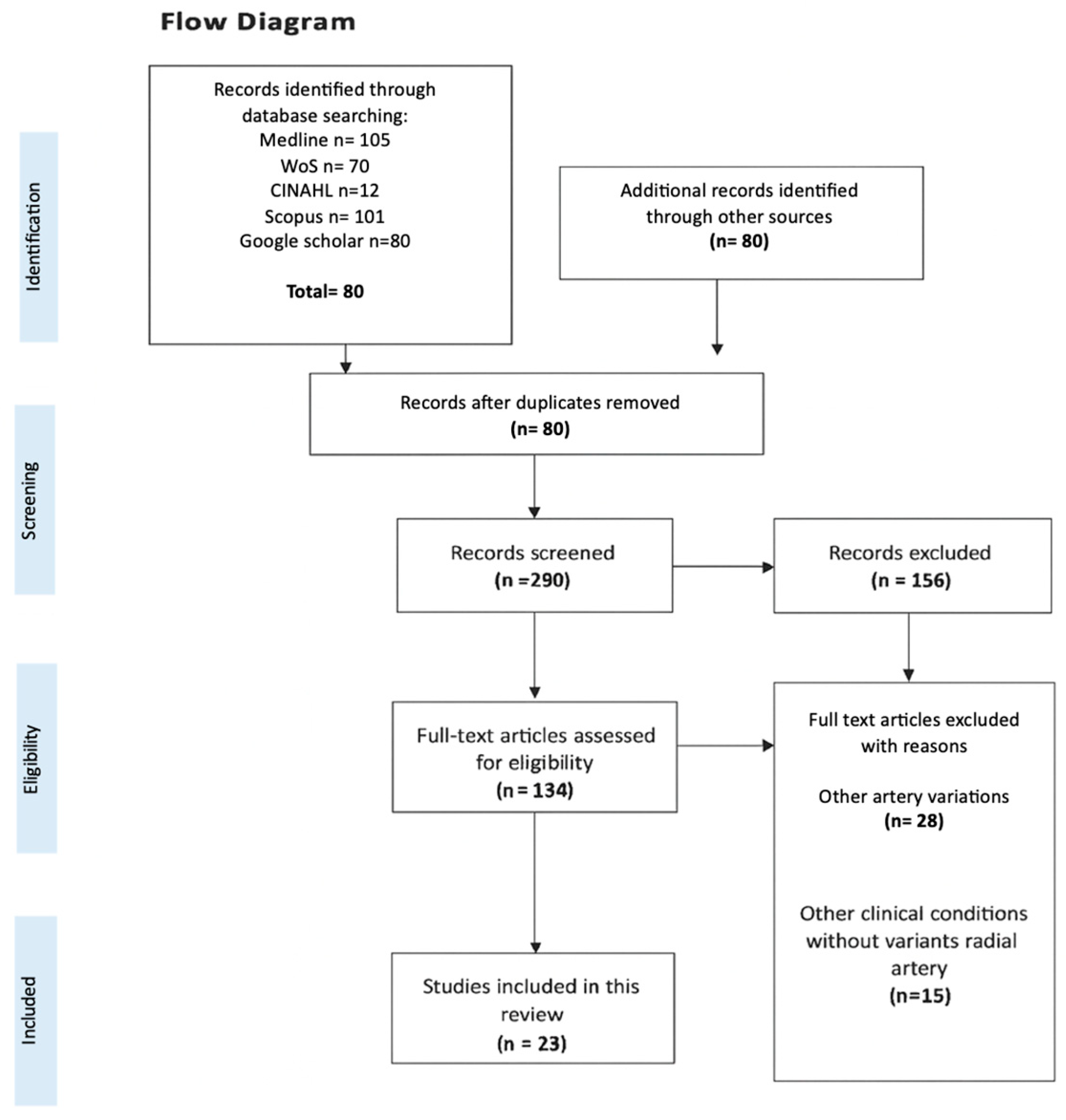
3.1. Included Articles
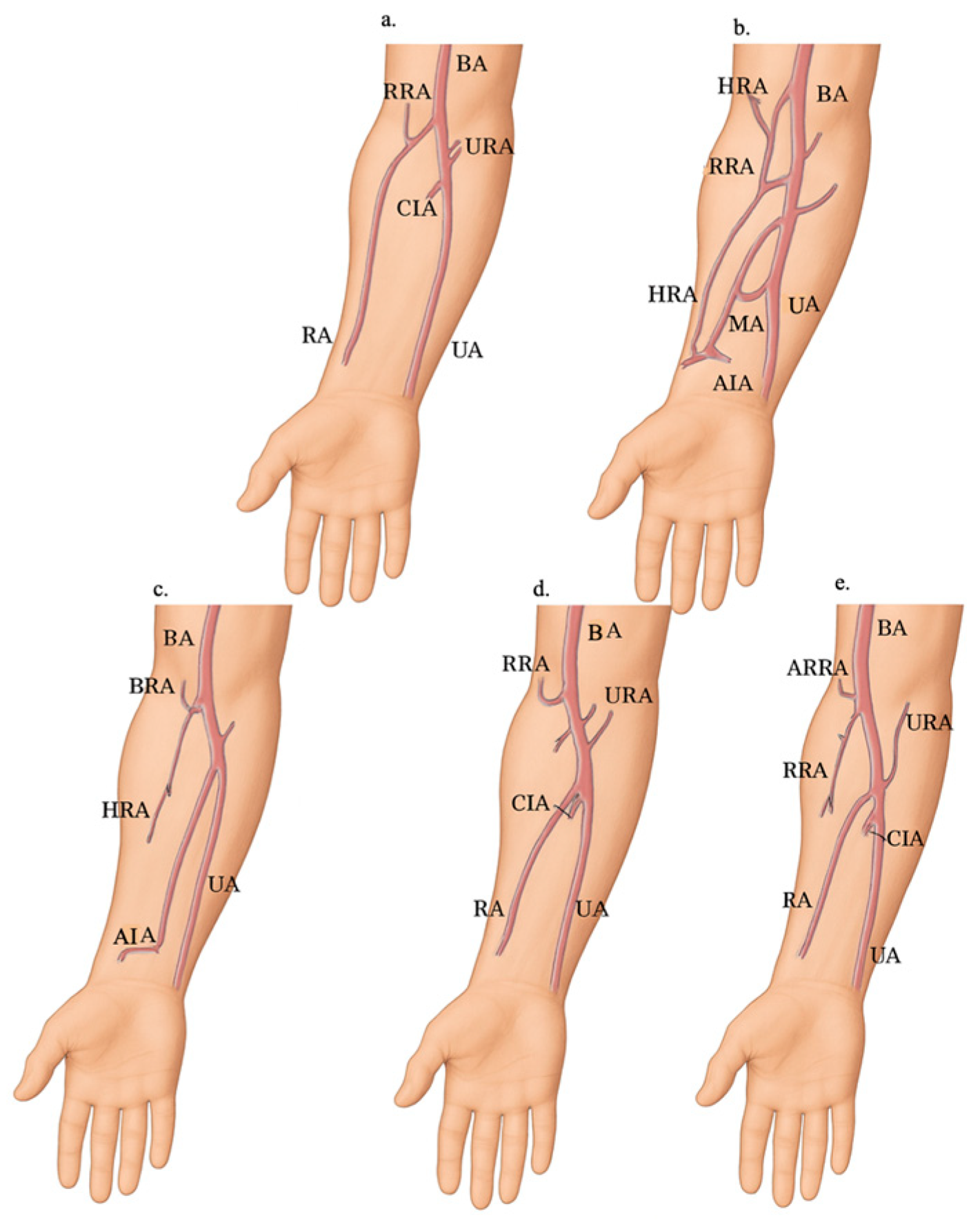
3.2. Variant Descriptions and Anatomy
3.2.1. Variants in the Origin of the Radial Artery
3.2.2. Variants in the Course of the Radial Artery
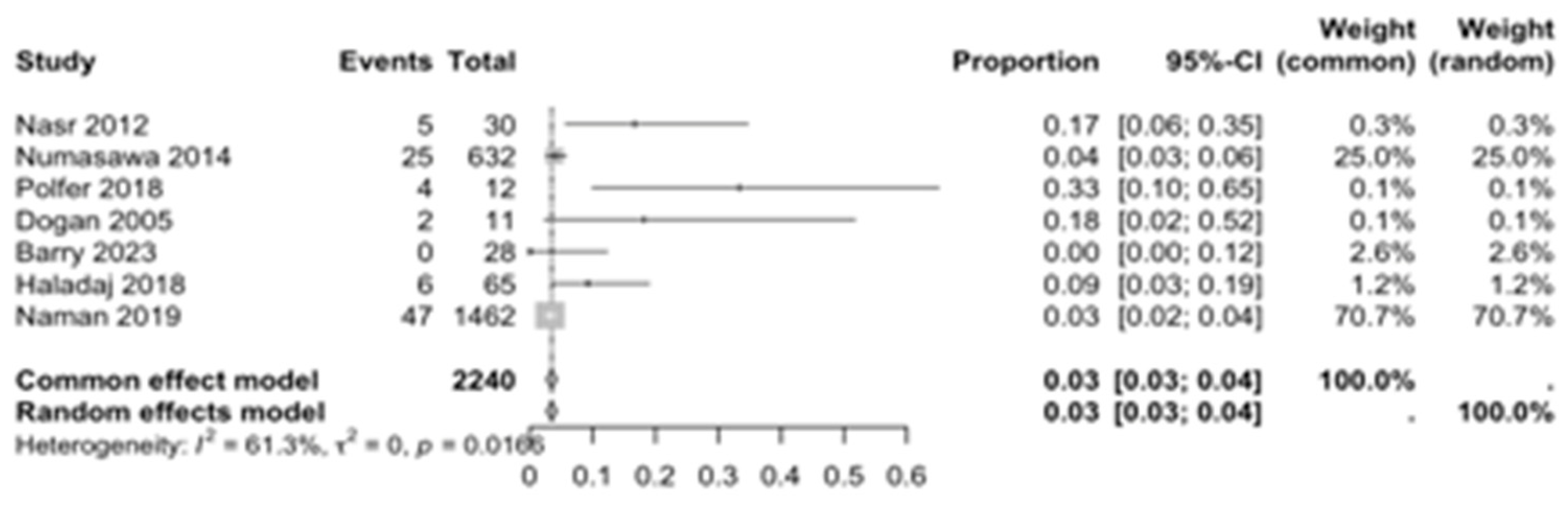
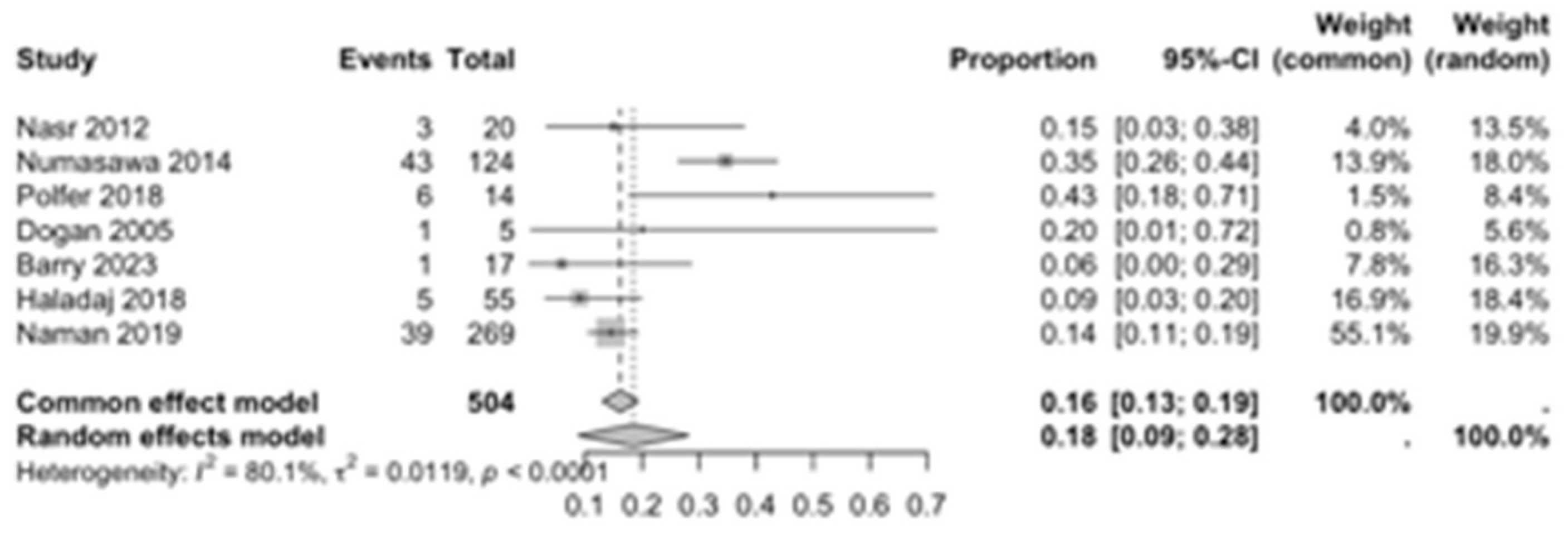
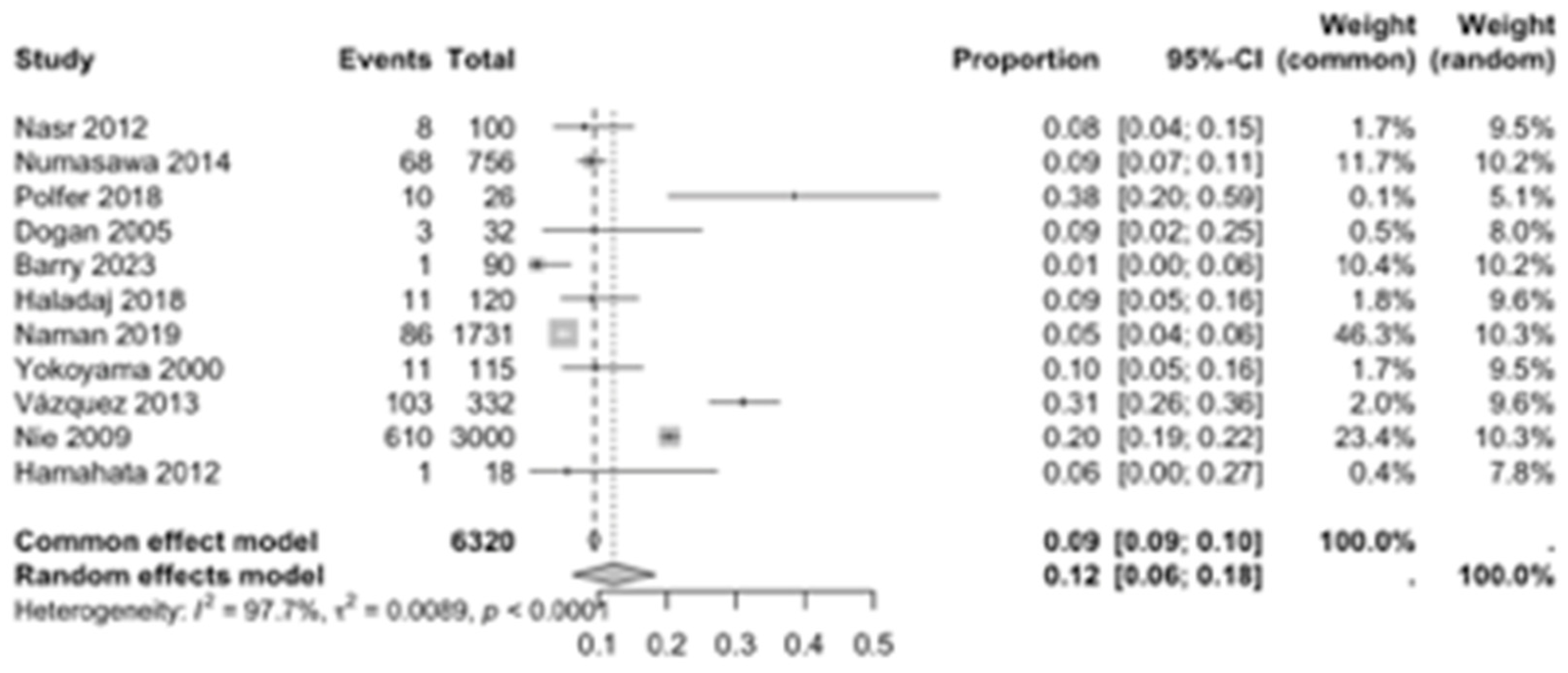
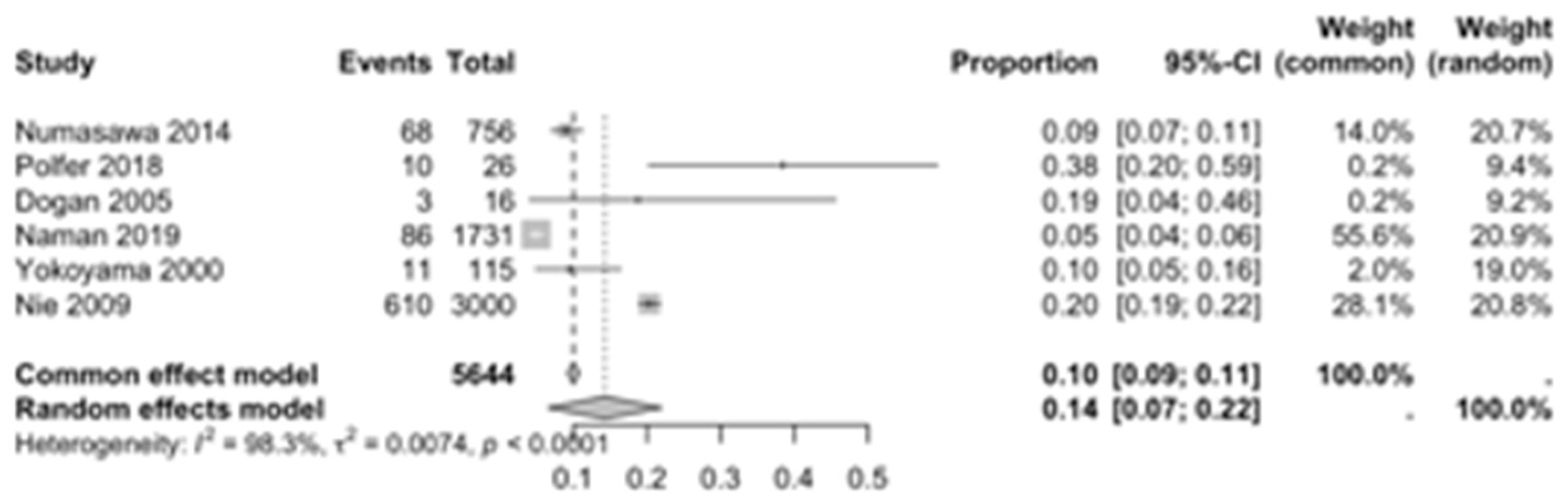
3.3. Analysis of Prevalence and Subgroups
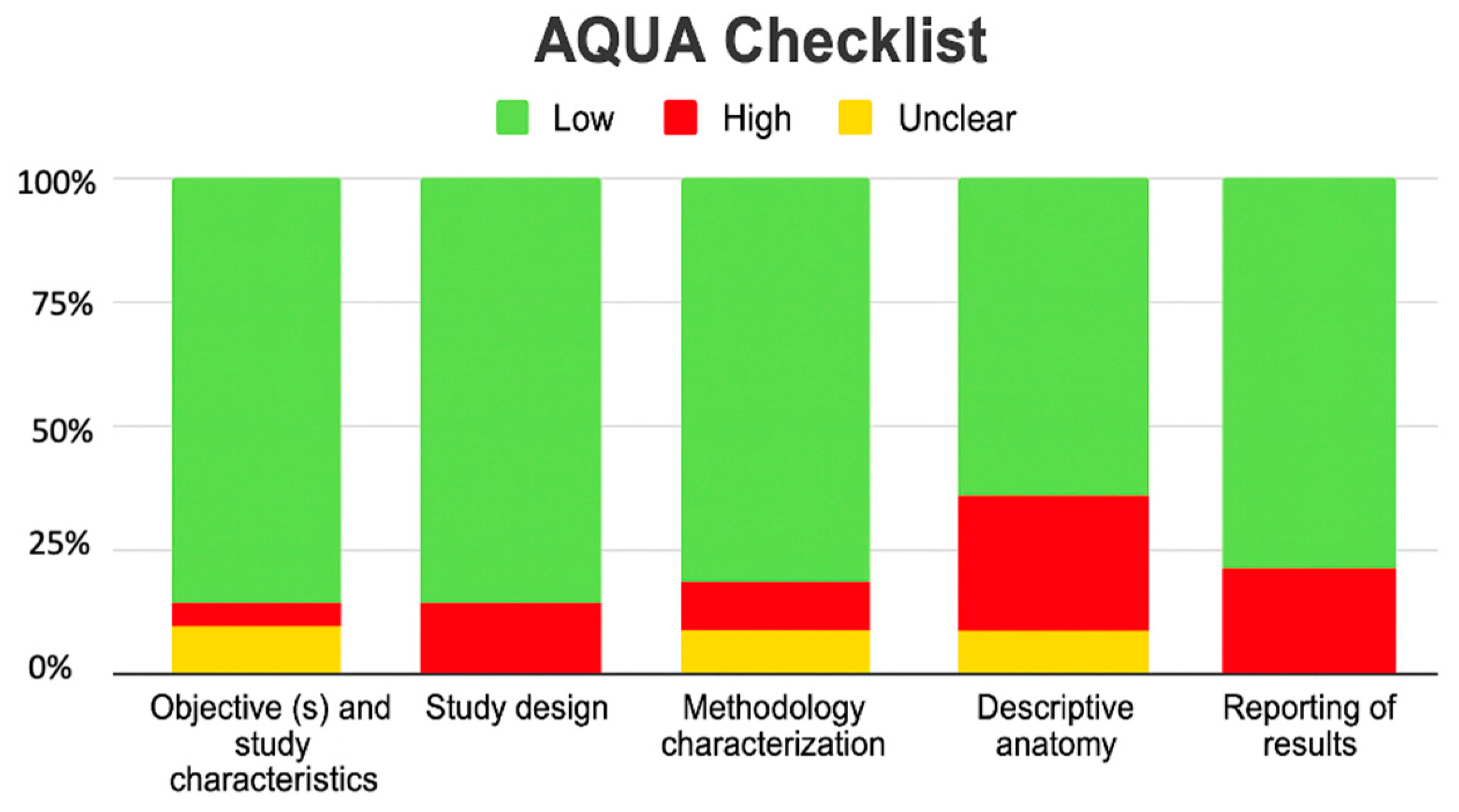
3.4. Risk of Bias of Included Articles
4. Discussion
4.1. Previous Studies
4.2. Anatomical Characteristics
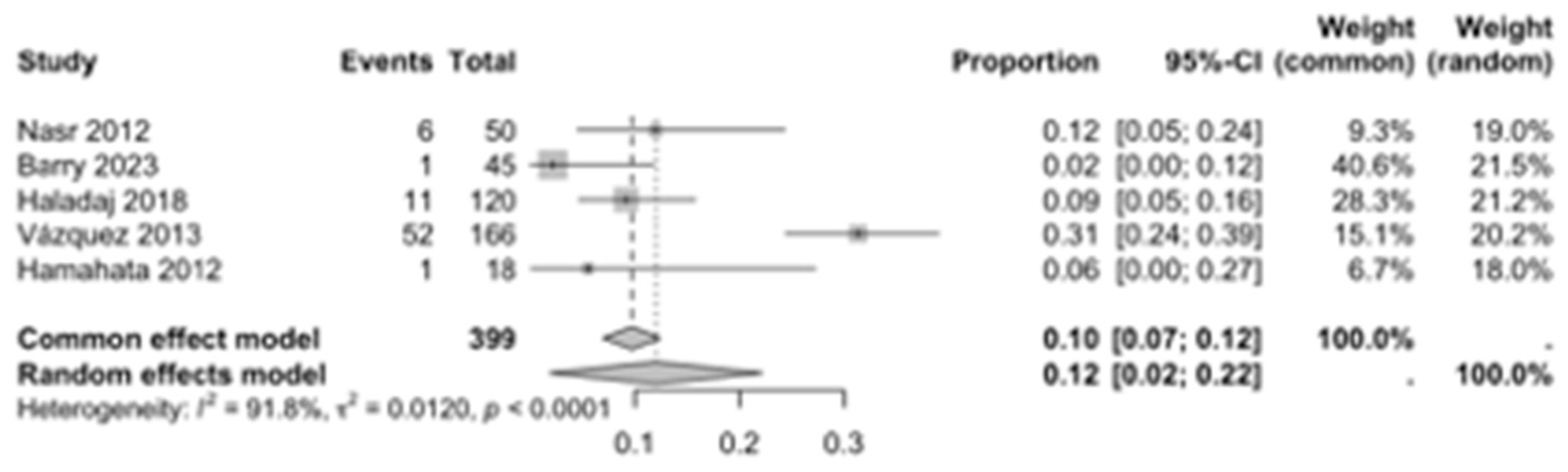
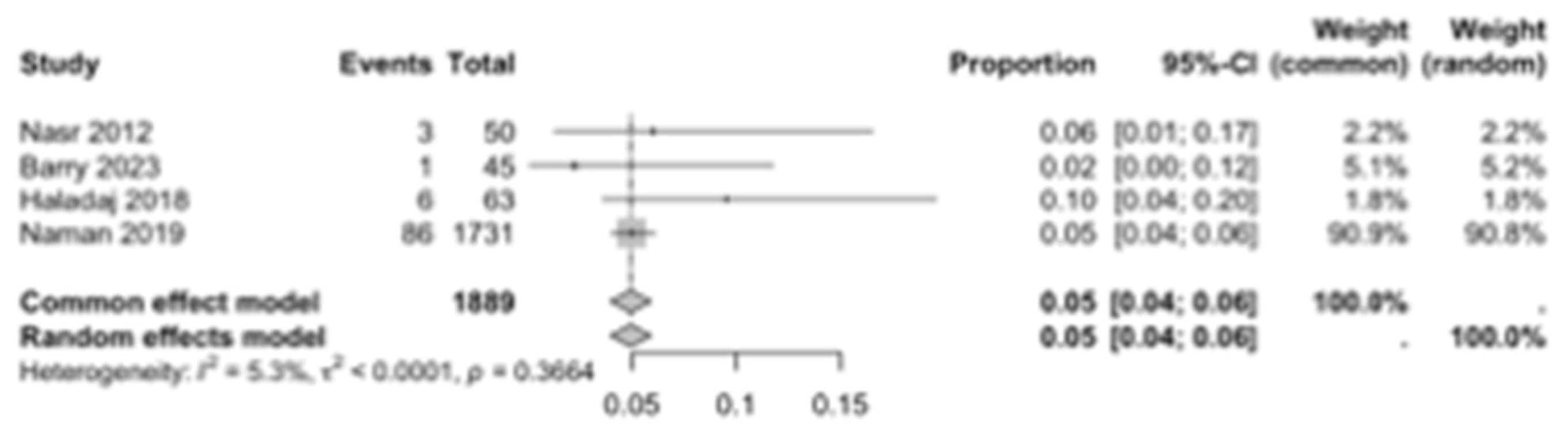
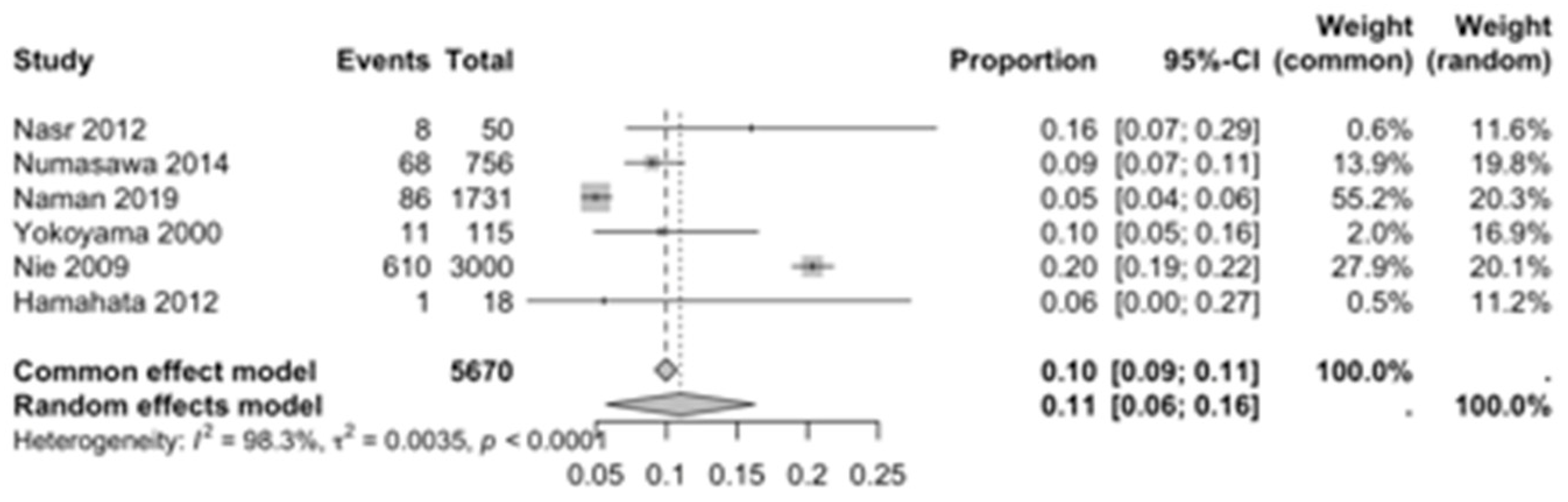
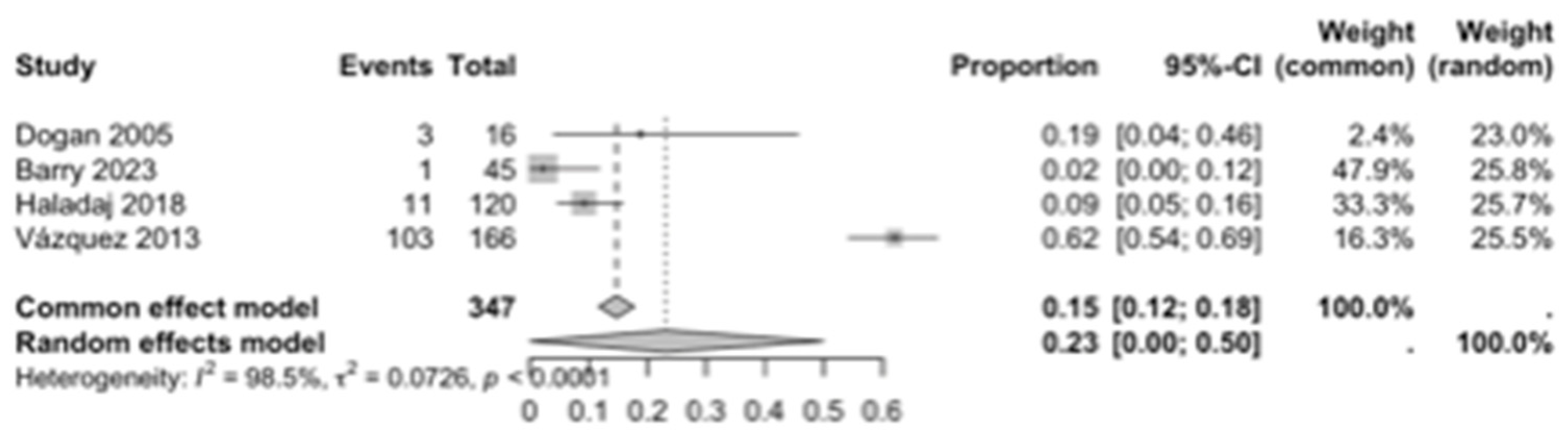
4.3. Forest Analysis
4.4. Clinical Considerations
4.5. Embryological Association
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marchese, R.M.; Launico, M.V.; Geiger, Z. Anatomy, Shoulder and Upper Limb, Forearm Radial Artery. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK546626/ (accessed on 19 November 2025).
- Nasr, A.Y. The radial artery and its variations: Anatomical study and clinical implications. Folia Morphol. 2012, 71, 252–262. [Google Scholar] [PubMed]
- Ostojić, Z.; Bulum, J.; Ernst, A.; Strozzi, M.; Marić-Bešić, K. Frequency of radial artery anatomic variations in patients undergoing transradial heart catheterization. Acta Clin. Croat. 2015, 54, 65–72. [Google Scholar] [PubMed]
- Orellana-Donoso MValenzuela-Fuenzalida, J.J.; Gold-Semmler, M.; Garcia-Gorigoitia, G.; Shane-Tubbs, R.; Santana-Machuca, E. Neural entrapments associated with musculoskeletal anatomical variations of the upper limb: Literature review. Transl. Res. Anat. 2021, 22, 100094. [Google Scholar] [CrossRef]
- Narsinh, K.H.; Mirza, M.H.; Duvvuri, M.; Caton, M.T., Jr.; Baker, A.; Winkler, E.A.; Higashida, R.T.; Halbach, V.V.; Amans, M.R.; Cooke, D.L.; et al. Radial artery access anatomy: Considerations for neuroendovascular procedures. J. Neurointerv Surg. 2021, 13, 1139–1144. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, V.J.; Marchand, K.E.; Viana, F.F.; Stuklis, R.; Cullen, H.; Tatoulis, J. The radial artery: Open harvesting technique. Multimed. Man. Cardiothorac. Surg. 2021, 2021. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. (Engl. Ed.) 2021, 74, 790–799. Erratum in Rev. Esp. Cardiol. (Engl. Ed.) 2022, 75, 192. https://doi.org/10.1016/j.rec.2021.10.019. [CrossRef] [PubMed]
- Tomaszewski, K.A.; Henry, B.M.; Kumar Ramakrishnan, P.; Roy, J.; Vikse, J.; Loukas, M.; Tubbs, R.S.; Walocha, J.A. Development of the Anatomical Quality Assurance (AQUA) checklist: Guidelines for reporting original anatomical studies. Clin. Anat. 2017, 30, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Von Hippel, P.T. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med. Res. Methodol. 2015, 15, 35. [Google Scholar] [CrossRef]
- Fu, R.; Gartlehner, G.; Grant, M.; Shamliyan, T.; Sedrakyan, A.; Wilt, T.J.; Griffith, L.; Oremus, M.; Raina, P.; Ismaila, A.; et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the Effective Health Care Program. J. Clin. Epidemiol. 2011, 64, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Numasawa, Y.; Kawamura, A.; Kohsaka, S.; Takahashi, M.; Endo, A.; Arai, T.; Ohno, Y.; Yuasa, S.; Maekawa, Y.; Fukuda, K. Anatomical variations affect radial artery spasm and procedural achievement of transradial cardiac catheterization. Heart Vessels. 2014, 29, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Polfer, E.M.; Sabino, J.M.; Giladi, A.M.; Higgins, J.P. Anatomical Variation of the Radial Artery Associated with Clinically Significant Ischemia. J. Hand Surg. Am. 2018, 43, e1–e952. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Kim, S.; Kim, S.; Song, W.C.; Kim, H.J. The radial artery running over the anatomical snuff-box: A case report. Surg. Radiol. Anat. 2022, 44, 659–663. [Google Scholar] [CrossRef] [PubMed]
- Dogan, O.F.; Karcaaltincaba, M.; Duman, U.; Akata, D.; Besim, A.; Boke, E. Assessment of the radial artery and hand circulation by computed tomography angiography: A pilot study. Heart Surg. Forum 2005, 8, E28–E33. [Google Scholar] [CrossRef] [PubMed]
- Singer, G.; Marterer, R.; Till, H.; Schmidt, B. A rare anatomic variation of the superficial palmar branch of the radial artery causing pain. Surg. Radiol. Anat. 2018, 40, 349–352. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rojas-Marte, G.; Chen, O.; Verma, S.; Rao, A.; Shani, J.; Ayzenberg, S. An avulsed radial artery with a high take-off. Vascular 2015, 23, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Venkatanarasimha, N.; Manghat, N.E.; Wells, I.P. Unusual presentation of ulnar artery aneurysm and dissection with associated anomalous radial artery: Appearances on multi-detector row CT angiography. Emerg. Radiol. 2007, 14, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Barry, M.; Gun, M.; Chabry, Y.; Harmouche, M.; Padurean, P.; Peltier, J.; Caus, T.; Havet, E. Anatomical and biometric study of the radial artery on human cadavers dissected in the anatomy laboratory. Surg. Radiol. Anat. 2023, 45, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Haładaj, R.; Wysiadecki, G.; Dudkiewicz, Z.; Polguj, M.; Topol, M. The High Origin of the Radial Artery (Brachioradial Artery): Its Anatomical Variations, Clinical Significance, and Contribution to the Blood Supply of the Hand. BioMed Res. Int. 2018, 2018, 1520929. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, L.; Zeng, Z.Y.; Zhong, J.M.; Wu, X.H.; Zeng, S.Y.; Tang, E.W.; Chen, W.; Sun, Y.H. Features and variations of a radial artery approach in southern Chinese populations and their clinical significance in percutaneous coronary intervention. Chin. Med. J. (Engl.) 2013, 126, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Naman, T.; Li, G.Q.; Cheng, H.; Hu, B. Anatomical features of the radial artery in the Xinjiang population in China and its impact on the transradial coronary intervention procedure. Folia Morphol. 2020, 79, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, N.; Takeshita, S.; Ochiai, M.; Koyama, Y.; Hoshino, S.; Isshiki, T.; Sato, T. Anatomic variations of the radial artery in patients undergoing transradial coronary intervention. Catheter. Cardiovasc. Interv. 2000, 49, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, T.; Sañudo, J.R.; Carretero, J.; Parkin, I.; Rodríguez-Niedenführ, M. Variations of the radial recurrent artery of clinical interest. Surg. Radiol. Anat. 2013, 35, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Alameddine, A.K.; Alimov, V.K.; Engelman, R.M.; Rousou, J.A.; Flack, J.E., 3rd; Deaton, D.W.; Engelman, D.T. Anatomic variations of the radial artery: Significance when harvesting for coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 2004, 127, 1825–1827. [Google Scholar] [CrossRef] [PubMed]
- Belbl, M.; Steyerova, P.; Kachlik, D. Two arterial variations of the hand and wrist present bilaterally (persistent median artery and superficial dorsal branch of the radial artery): Ultrasound findings. Surg. Radiol. Anat. 2024, 46, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Shao, L.; Mao, J.Y. Bilaterally symmetrical congenital absence of radial artery: A case report. BMC Surg. 2014, 14, 15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Narayanan, S.; Murugan, S. Bifurcation of brachial artery into a common radial-interosseous trunk and superficial ulnar artery: A rare variation. Anat. Sci. Int. 2018, 93, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Nie, B.; Zhou, Y.J.; Li, G.Z.; Shi, D.M.; Wang, J.L. Clinical study of arterial anatomic variations for transradial coronary procedure in Chinese population. Chin. Med. J. 2009, 122, 2097–2102. [Google Scholar] [PubMed]
- Hamahata, A.; Nakazawa, H.; Takeuchi, M.; Sakurai, H. Usefulness of radial recurrent artery in transplant of radial forearm flap: An anatomical and clinical study. J. Reconstr. Microsurg. 2012, 28, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.T.; Wang, P.J.; Young, C.; Lai, M.W.; Shen, Y.Z. Thenar hypoplasia in Klippel-Feil syndrome due to aberrant radial artery. Pediatr. Neurol. 1995, 13, 343–345. [Google Scholar] [CrossRef] [PubMed]
- Vollala, V.R.; Nagabhooshana, S.; Bhat, S.M. Trifurcation of brachial artery with variant course of radial artery: Rare observation. Anat. Sci. Int. 2008, 83, 307–309. [Google Scholar] [CrossRef] [PubMed]
- Schena, S.; Crabtree, T.D.; Baker, K.A.; Guthrie, T.J.; Curci, J.; Damiano, R.J.; Barner, H.B. Absence of deterioration of vascular function of the donor limb at late follow-up after radial artery harvesting. J. Thorac. Cardiovasc. Surg. 2011, 142, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Gruber, W. Dreiwurzelige Arteria radialis. Arch. Für Anat. Physiol. Und Wiss. Med. 1870, 37, 501–522. [Google Scholar]
- Hoffman, R.D.; Danos, D.M.; Lin, S.J.; Lau, F.H.; Kim, P.S. Prevalence of Accessory Branches and Other Anatomical Variations in the Radial Artery Encountered during Radial Forearm Flap Harvest: A Systematic Review and Meta-analysis. J. Reconstr. Microsurg. 2020, 36, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, G.; Chemaitelly, H.; Abu-Raddad, L.J.; Rücker, G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res. Synth. Methods 2019, 10, 476–483. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tian, Y.; Bai, B.; Zhang, Y.; Che, L.; Wang, J.; Wang, Y.; Yu, C.; Huang, Y. The Improved Catheterization Is Associated with the Deeper Radial Arteries in Ultrasound-Guided Dynamic Needle Tip Positioning Technique. Front. Med. 2022, 9, 803124. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brzezinski, M.; Luisetti, T.; London, M.J. Radial artery cannulation: A comprehensive review of recent anatomic and physiologic investigations. Anesth. Analg. 2009, 109, 1763–1781. [Google Scholar] [CrossRef] [PubMed]
- Cuminetti, G.; Bonadei, I.; Vizzardi, E.; Sciatti, E.; Lorusso, R. On-Pump Coronary Artery Bypass Graft: The State of the Art. Rev. Recent. Clin. Trials. 2019, 14, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Athanasiou, T.; Saso, S.; Rao, C.; Vecht, J.; Grapsa, J.; Dunning, J.; Lemma, M.; Casula, R. Radial artery versus saphenous vein conduits for coronary artery bypass surgery: Forty years of competition—Which conduit offers better patency? A systematic review and meta-analysis. Eur. J. Cardiothorac. Surg. 2011, 40, 208–220. [Google Scholar] [CrossRef] [PubMed]
- Ramírez Vélez, A.; Gaviria Valencia, S.; Jaramillo Gómez, N.; Contreras Martínez, H.; Cardona Vélez, J. Accesos vasculares femoral y radial en intervenciones coronarias percutáneas en síndrome coronario agudo y enfermedad crónica inestabilizada. Rev. Colomb. Cardiol. 2018, 25, 257–263. [Google Scholar] [CrossRef]
- Carmona Monge, F.J.; Martínez Lareo My Núñez Reiz, A. Canalización arterial radial guiada por ultrasonidos: Descripción de la técnica y revisión de la literatura. Enferm. Intensiva 2011, 22, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Wysiadecki, G.; Polguj, M.; Haładaj, R.; Topol, M. Low origin of the radial artery: A case study including a review of literature and proposal of an embryological explanation. Anat. Sci. Int. 2017, 92, 293–298. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Database | Search Strategy | Results | |
|---|---|---|---|
| 25 February 2020 | 25 July 2025 | ||
| Medline | ((((“radial artery” [MeSH Terms] OR (“radial” [All Fields] AND “artery” [All Fields]) OR “radial artery” [All Fields]) AND (“variation” [All Fields] OR “variations” [All Fields])) OR ((“aberrance” [All Fields] OR “aberrances” [All Fields] OR “aberrancies” [All Fields] OR “aberrancy” [All Fields] OR “aberrant” [All Fields] OR “aberrants” [All Fields] OR “aberrated” [All Fields] OR “aberrating” [All Fields] OR “aberration” [All Fields] OR “aberrational” [All Fields] OR “aberrations” [All Fields] OR “aberrator” [All Fields] OR “aberrators” [All Fields]) AND (“radial artery” [MeSH Terms] OR (“radial” [All Fields] AND “artery” [All Fields]) OR “radial artery” [All Fields]))) AND (“clin anat” [Journal] OR (“clinical” [All Fields] AND “anatomy” [All Fields]) OR “clinical anatomy” [All Fields])) NOT (“review” [Publication Type] OR “review literature as topic” [MeSH Terms] OR “review” [All Fields]) | 104 | 105 |
| Wos | radial artery variations OR aberrant radial artery AND clinical anatomy NOT review | 70 | 70 |
| CINAHL | radial artery variations OR aberrant radial artery AND clinical anatomy NOT review | 12 | 12 |
| SCOPUS | radial artery variations OR aberrant radial artery AND clinical anatomy NOT review | 100 | 101 |
| Google Scholar | radial artery variations OR aberrant radial artery AND clinical anatomy NOT review | 80 | 80 |
| Total | 366 | 368 | |
| Author and Year | Geographic | N and Sample | N and Prevalence | RA Variant | Laterality of Variant | RA Type Variant or Classification | Sex and Age | Clinical Considerations |
|---|---|---|---|---|---|---|---|---|
| Nasr, 2012 [2] | Saudi Arabia | 50 donors | 8/50 | Variations in branching pattern of RA | 5 rights 3 left | The RA originated from the medial aspect of the upper third of BA The RA originated from the lateral of the upper part of BA | 30 males 20 females Age: NA | Variation in branching pattern of RA has great importance in cardiac catheterization for angioplasty, pedicled flaps or arterial grafts, where any abnormal position or division should be identified before surgery. Thus, physicians should be aware of this variation before starting the procedure. |
| Numasawa et al., 2014 [12] | Japan | 756 patients | 68/756 | Variation in the origin of Radioulnar loop and tortuous configuration | 706 rights 50 lefts | Bifurcated BA proximal to the intercondylar line of the humerus is considered an abnormal origin of the RA | 632 males 124 females Mean age: 67.6 to 11.5 years | Some patients with anatomic variation in RA had significantly larger ulnar arteries than RA. In some of these difficult transradial cases with anatomic variation, transulnar approach might be a safe alternative to transradial procedure if the reverse Allen test result is normal. |
| Polfer et al., 2018 [13] | United States | 26 patients | 10/26 | Variations in RA origin | 16 right 10 lefts | The RA originated in proximal BA The RA originated in mid-BA | 12 males 14 females Mean age: 52 years | High-origin radial arteries may have variations in the density and adequacy of the most terminal part of the vessel and its branches, which increases the risk of ischemia. Alternatively, the proximal origin of the RA may affect distal perfusion through its impact on flow characteristics in the other vessels to the upper limb. |
| Park et al., 2022 [14] | South Korea | 1 donor | 1/1 | Atypical topographic relationship RA | NA | Superficial RA runs over tendons (0.52%) Deep RA is thin and penetrates the tendons of the anatomical snuff-box | 1 male 91 years old | Clinical classification of RA variants is vital as they are the main cause of technical failure when performing transradial catheterization. If well documented, problems with the transradial approach are minimized. |
| Dogan et al., 2005 [15] | Ankara, Turkey | 16 patients | 3/16 | Severe RA calcification (1/16) and variation in forearm arterial anatomy | NA | Mild stenosis, occlusion and diffuse calcification of the distal RA | 5 females 11 males Mean age: 60 years | A severely calcified RA is a risk factor because the long-term patency of this vessel is questionable. Few studies have examined the prevalence of pre-existing disease in this vessel, using Doppler ultrasound [Pola 1996, Ruengsakulrach 2001, Nicholosi 2002] or histologically [Kaufer 1997]. |
| Singer et al., 2018 [16] | Graz, Austria | 1 patient | 1/1 | Variant course of superficial palmar branch of RA | Right | Superficial palmar branch of RA superficial to thenar muscles | Female 17 years old | The vast majority of reports describing variant courses of the superficial palmar branch of RA are limited to post-mortem anatomical studies. Therefore, it can be assumed that irregular courses of the artery rarely cause clinical problems requiring intervention. |
| Rojas-Marte et al., 2015 [17] | NY, USA | 1 patient | 1/1 | High takeoff RA | Right | Severe aortic stenosis | Female 63 years | Although vascular complications with TRA are less common than with TFA, the main problems include asymptomatic occlusion, spasm, and perforation of the RA, with the formation of hematomas and pseudoaneurysms. Other complications have also been described, such as compartment syndrome, perforation of arteries beyond the BA and catheter retention. |
| Venkatanarasimha, et al., 2007 [18] | United Kingdom | 1 patient | 1/1 | Hypoplastic small caliber radial artery right | Right | Small caliber RA had a high proximal origin with relatively sharp angulation at its BA origin | Female 30 years old | A high origin RA is the most common variation, arising from the axillary artery in 4% and from the BA in 1.6%. Variations and absence of the RA in the forearm are less than 0.03%. |
| Barry, et al., 2023 [19] | Amiens, France | 45 donors | 1/45 | Origin of RA | Right | High origin of RA “BRA” | 28 males 17 females Average age 79.2 ± 9.2 | This knowledge can ensure greater safety and reliability of the harvesting technique for use as a graft. |
| Haładaj, et al., 2018 [20] | Lodz, Poland | 120 isolated upper limbs | 11/120 BRA: 11 Axillary BRA: 2 BA BRA: 9 Anastomosis: 6/11, 6/120 | BRA anatomical variations regarding: Origin, Presence, Anastomosis, Pattern of RRA | BRA: 6 Right, 5 Left Axillary BRA: 2 Right BA BRA: Dominant anastomosis: 1 Right Balanced: 1 Right and 1 Left (M), and 1 Right (F) Minimal: 1 Left (M), 1 Right (F) Abscent: 1 left and 1 right (M), 2 left and 1 right (F). | BRA in 9.2% (from axillary artery in 2 cases and from the BA in 9 cases). 54.6% anastomosis between BRA and BA in the cubital fossa, in 1 case, balanced in 3, minimal in 2 and absent in 5. division (trifurcation of the BA) in 9.2% (11/120), from the BRA in 5% (6/120) and from the cubital crossing in 4.2% (5/120). | ABR: 6M and 5F ABR axillary: 2M ABR BA: 4M and 5F Dominant anastomosis: 1M Balanced: 2M and 1F Minimal: 1M and 1F Absent: 2M, 3F 65M, 55F | The presence of BRA “contributed significantly to the development of tortuosity,” which may increase the risk of failure of transradial catheterization. |
| Li, et al., 2013 [21] | Guangxi, China | 1400 patients | 57/1400 origin 170/1400 with tortuosity | Tortuosity, Origin | NA | RA tortuosity (3.6%), ARB (1.7%), RA loop (0.6%) BA branches: Double RA (0.1%), double BA (0.1%) | 1072 male 328 females age ≥18 | Patients with tortuous RA tended to present with more classic chest pain. RA tortuosity and variation have become the leading cause of failure in coronary interventions through the RA, with the main factors for tortuosity being advanced age, female sex, short stature, etc. |
| Naman, et al., 2020 [22] | Xinjiang, China | 1731 patients | 86/1731 | Origin, radioulnar loop and tortuosity. | NA | Variations origin of the RA (bifurcation of the BA proximal to the intercondylar line of the humerus) | 1462 male 269 females Age: NA | Sex, occupation and internal diameter of the RA are significantly associated with the incidence of variation in the RA. |
| Yokoyama, et al., 2000 [23] | Tokyo, Japan | 115 patients | 11/115 | Tortuosity, stenosis, hypoplasia of the RA and radioulnar loop. | NA | A tortuous RA was demonstrated on imaging in seven patients. Radial stenosis was observed (2/115) | 83 males 32 females Mean age: 64.5 ± 9.7 years | Of the 115 patients undergoing TRI, 11 presented anatomical variations, of which 3 presented hypoplasia of the RA (1.7%) and a radioulnar loop (0.9%) making access of the guidewire and the introducer sheath impossible, which was finally planned using the femoral artery. |
| Vazquez, et al., 2013 [24] | United Kingdom | 332 upper limbs from 166 donors separated into two groups | 103/332 83 from group one 20 from group two | Accessory branch of the RRA | NA | The accessory branch of the RRA originated from the BA and ran behind the bicipital tendon, supplying the brachioradialis, brachialis, and biceps brachii muscles. The main RRA in group one originated from RA (75%), posterior radioulnar division (9%), anterior (5.4%), BA (7.2%), and ulnar-interosseous trunk (2.7%). The main RRA in group two originated from BRAl (65%). | 79 male donors 87 female donors Age at death: Between 57 and 101 years. | Group one: normal pattern of the arteries of the upper limb, Group two: variations in the main arterial trunks of the upper limb |
| Alameddine, et al., 2004 [25] | Salem and Springfield, Massachusetts. | 1 | 1 | Accessory Branch or Duplication | Left | Accessory branch of the RA in the left arm, runs over the deep fascia of the forearm. | NA | In this case, we recommend that the incision be modified slightly and placed more medially along the medial border of the FCRM. |
| Belbl, et al., 2024 [26] | Czech Republic | 1 volunteer | 1 | NA | Bilateral | PMA and superficial dorsal branch of RA Type 1, according to Miletin classification | 1 Female 19 years old | Use of ultrasound before planning surgical procedures. |
| Zheng, et al., 2014 [27] | Nankai, Tianjin, China | 1 patient | 1 | Bilateral congenital absence of the RA | Bilateral | Both arms without RA and the ulnar arteries were small, while the anterior interosseous arteries were the dominant artery | 1 male 43 years old | Coronary angiography and percutaneous coronary intervention were performed through the BA, since transradial PCI failed. |
| Narayanan, et al., 2018 [28] | Puducherry, India | 1 donor | 1 | BA bifurcation | Right | BA bifurcation into a common radial-interosseous trunk and a superficial ulnar artery. | Male 63 years old | The superficial position of the UA may allow surgeons to raise a free ulnar flap for head and neck reconstructive surgeries. |
| Nie, et al., 2009 [29] | Beijing, China | 3000 patients | 610/3000 | Tortuosity, hypoplasia, radioulnar loop, origin, stenosis. | NA | RA: tortuous configurations (5.0%), hypoplasia (2.2%), radioulnar loop (1.1%) variations in origin (7. 7%), stenosis (1.4%); | M 65.9% (1977), F 34.1% (1023) 61 ± 8.1 years old | Anatomical variations in the RA are frequent and constitute an important limitation of the transradial approach. |
| Hamahata, et al., 2012 [30] | Japón | 18 limbs from 18 donors | 1/18 | Variations in the origin of the RRA | NA | The anatomical variation in the RRA was divided into its origin into the RA (type A, 61.1%), RA bifurcation (type B, 33%), BA (type C, 0%) and UA (type D, 5%) | 9 limbs from female donors 9 limbs from male donors Mean Age: NA | The use of radial forearm flaps plays an important role in head and neck operations. These involve performing anastomoses between the involved arteries where the RRA can be used instead of the RA to effectively transfer the flap. |
| Lee, et al., 1995 [31] | NA | 1 patient | 1/1 | Aberrant RA | Left | An aberrant RA in the left arm of a patient with Klippel-Feil syndrome had progressive atrophy of the left thenar eminence | 1 male patient 10 years old | Thoracic outlet syndrome should be considered for patients with KFS as compression of the subclavian artery may compromise blood supply and aggravate thenar atrophy. |
| Vollala et al., 2008 [32] | India | 1 donor | 1/1 | Variation in the course of the RA | Right | A trifurcation of the BA in which the RA follows a variation in the course passing deep to the PTM | 1 male donor 45 years old | Knowledge of arterial variations in the upper limb is necessary in research, orthopedic or surgical procedures and catheterization. The RA is used for cannulation, so its variation in course under the PTM can cause arterial compression and erroneous blood pressure values. The RA is used to replace the great saphenous vein as a CABG. |
| Schena et al., 2011 [33] | United States | 25 volunteers (sub cohort) | 25/25 | Absence of RA after surgery | NA | Absence of RA implies increased blood flow to the UA and therefore its diameter, which can generate shear stress | 21 males 4 females Mean age: 68.6 ± 8.6 years | In recent years, arterial grafts have been the main treatment for coronary artery disease, so the search for durable conduits to achieve better patency over time is of utmost importance. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanchis-Gimeno, J.; Loaiza-Giraldo, J.P.; Alruiz, Y.; Vergara, M.; Navia, M.F.; Roman, C.; Suazo-Santibañez, A.; Nova-Baeza, P.; Orellana-Donoso, M.; Oyanedel-Amaro, G.; et al. Prevalence of Radial Artery Variants and Their Relationship with Clinical Considerations of the Antebrachial Region: Systematic Review and Meta-Analysis. Diagnostics 2025, 15, 2984. https://doi.org/10.3390/diagnostics15232984
Sanchis-Gimeno J, Loaiza-Giraldo JP, Alruiz Y, Vergara M, Navia MF, Roman C, Suazo-Santibañez A, Nova-Baeza P, Orellana-Donoso M, Oyanedel-Amaro G, et al. Prevalence of Radial Artery Variants and Their Relationship with Clinical Considerations of the Antebrachial Region: Systematic Review and Meta-Analysis. Diagnostics. 2025; 15(23):2984. https://doi.org/10.3390/diagnostics15232984
Chicago/Turabian StyleSanchis-Gimeno, Juan, Jessica Paola Loaiza-Giraldo, Yael Alruiz, Maximiliano Vergara, Maria Fernanda Navia, Camila Roman, Alejandra Suazo-Santibañez, Pablo Nova-Baeza, Mathias Orellana-Donoso, Gustavo Oyanedel-Amaro, and et al. 2025. "Prevalence of Radial Artery Variants and Their Relationship with Clinical Considerations of the Antebrachial Region: Systematic Review and Meta-Analysis" Diagnostics 15, no. 23: 2984. https://doi.org/10.3390/diagnostics15232984
APA StyleSanchis-Gimeno, J., Loaiza-Giraldo, J. P., Alruiz, Y., Vergara, M., Navia, M. F., Roman, C., Suazo-Santibañez, A., Nova-Baeza, P., Orellana-Donoso, M., Oyanedel-Amaro, G., Rodriguez-Luengo, M., Bruna-Mejias, A., Valenzuela-Fuenzalida, J. J., León-Rojas, J. E., & Granite, G. (2025). Prevalence of Radial Artery Variants and Their Relationship with Clinical Considerations of the Antebrachial Region: Systematic Review and Meta-Analysis. Diagnostics, 15(23), 2984. https://doi.org/10.3390/diagnostics15232984