Tibial Nerve Palsy Secondary to Spontaneous Isolated Popliteus Muscle Rupture and Localized Compartment Syndrome
Abstract
1. Introduction
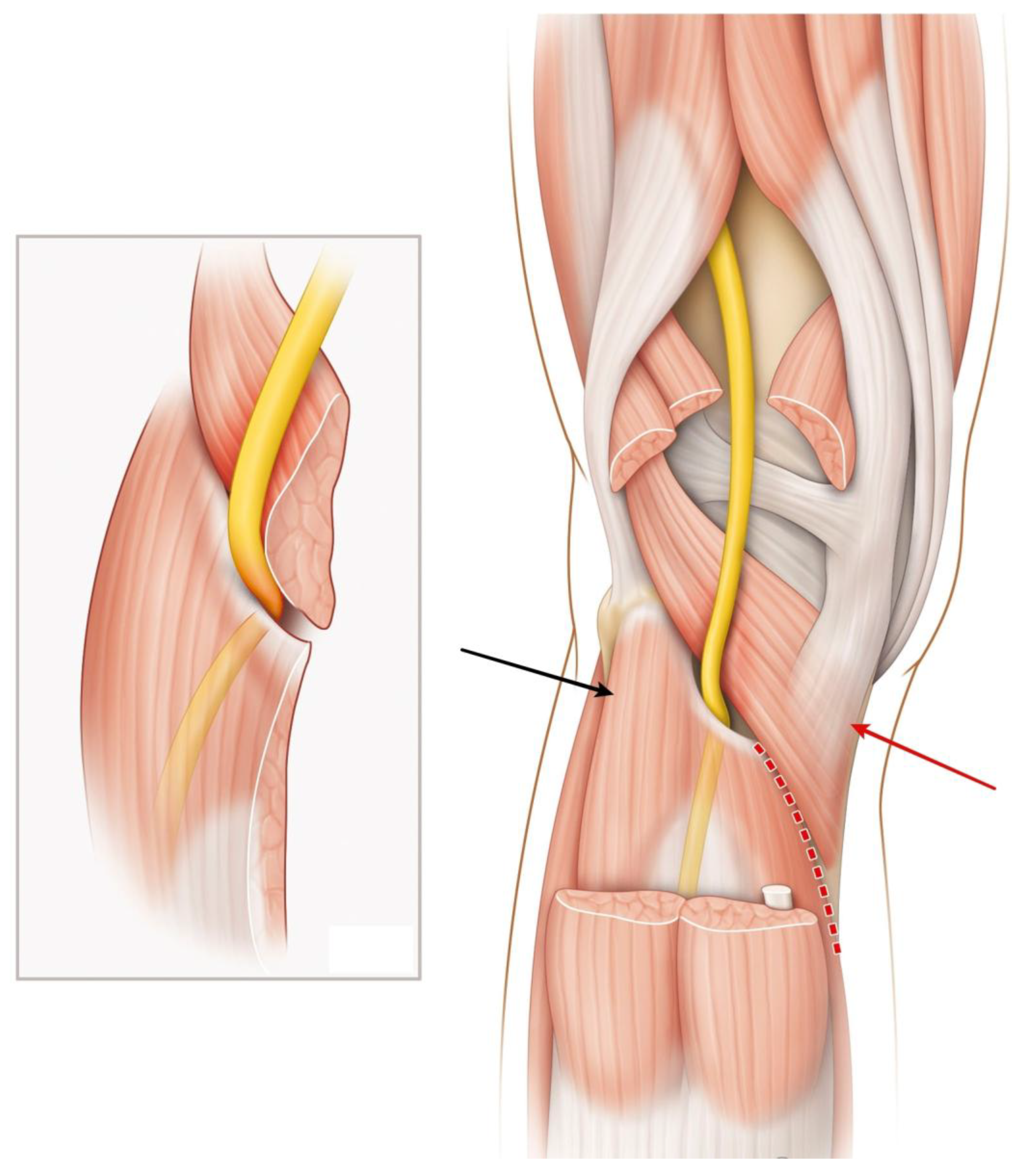
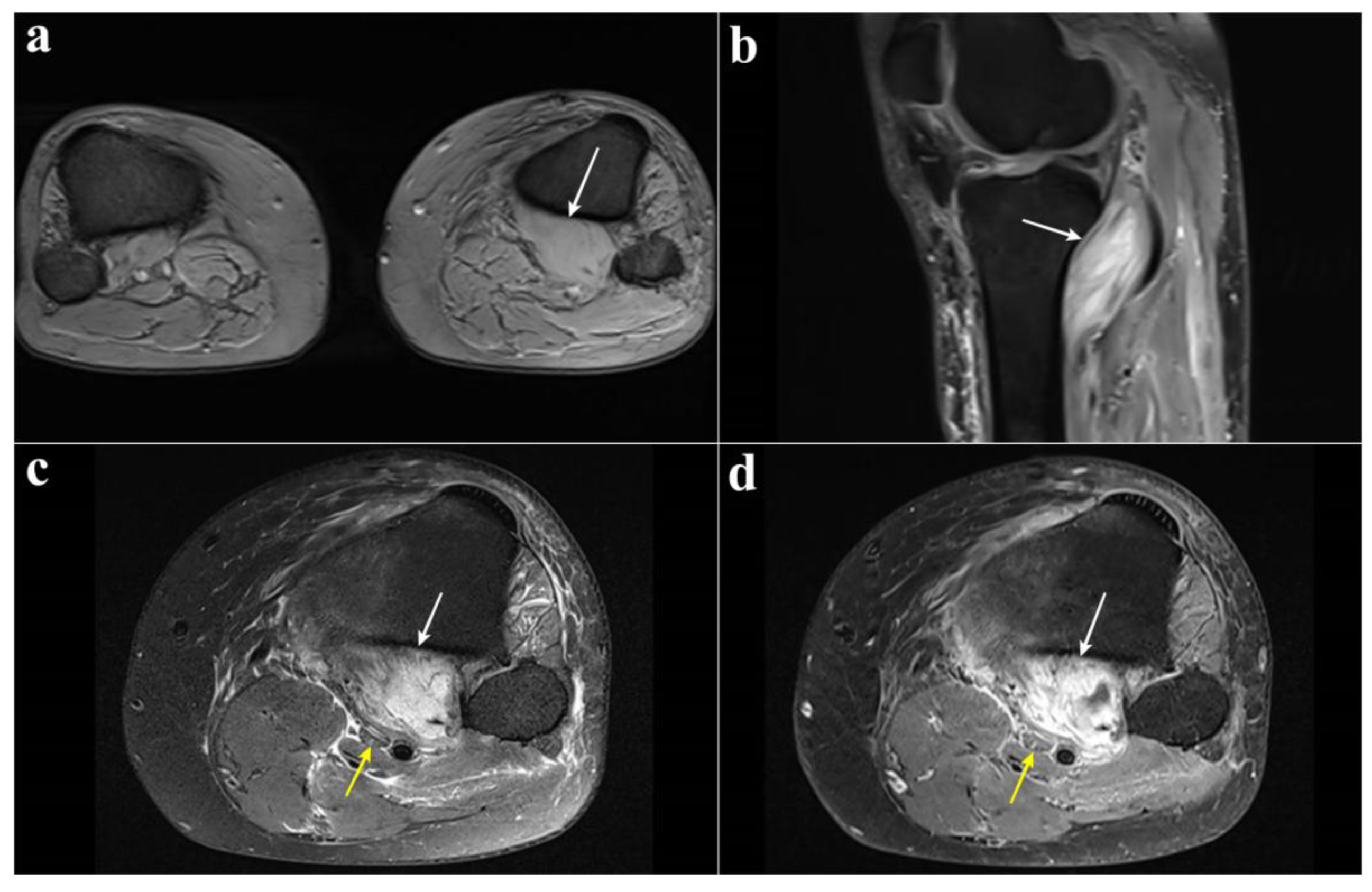
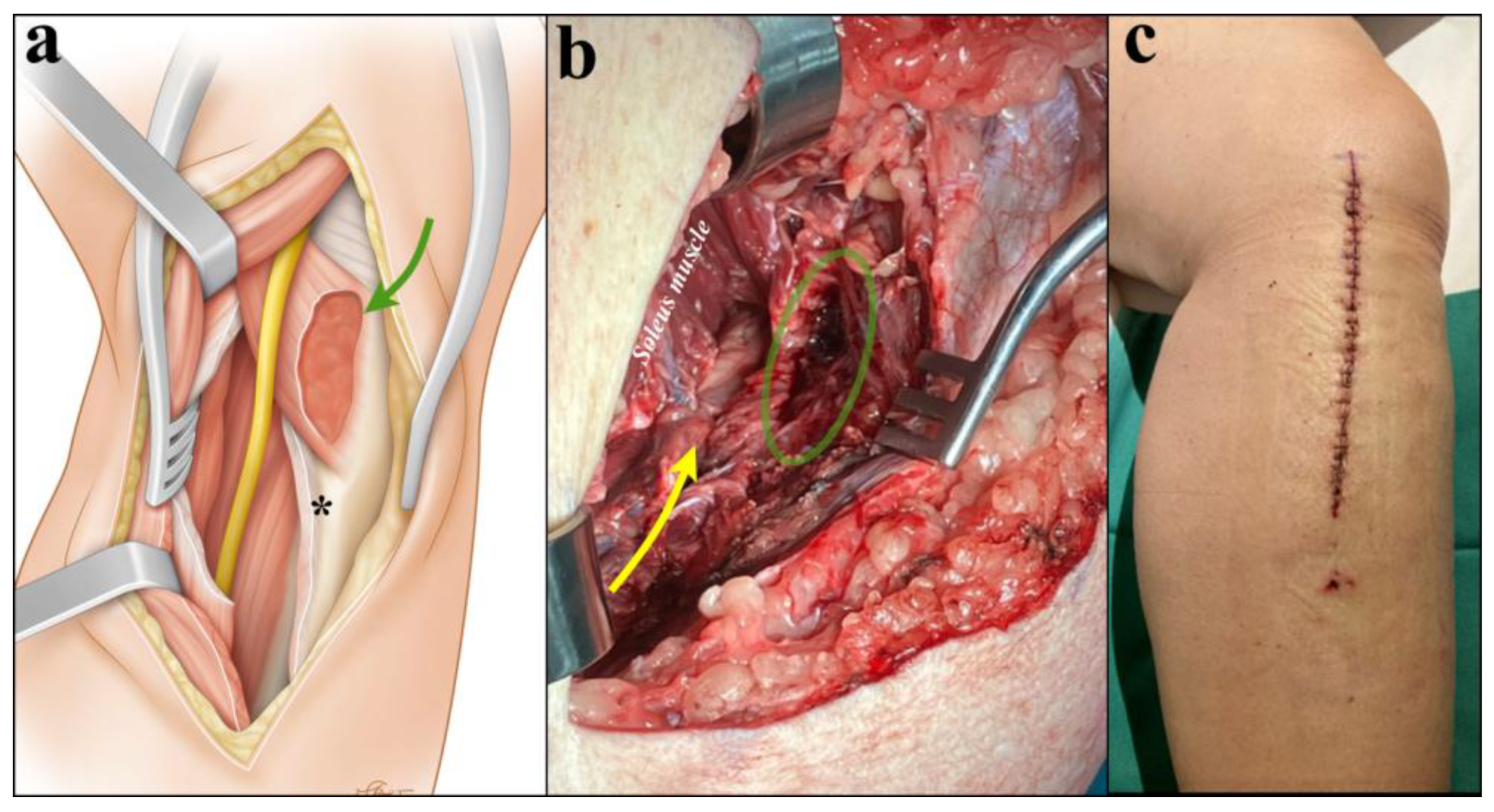
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MRI | Magnetic resonance imaging (MRI) |
| TP | Tibialis posterior |
| FDL | Flexor digitorum longus |
| FHL | Flexor hallucis longus |
| PM | Popliteus muscle |
| TN | Tibial nerve |
References
- Burstein, D.B.; Fischer, D.A. Isolated rupture of the popliteus tendon in a professional athlete. Arthroscopy 1990, 6, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Geissler, W.B.; Corso, S.R.; Caspari, R.B. Isolated rupture of the popliteus with posterior tibial nerve palsy. J. Bone Jt. Surg. Br. 1992, 74, 811–813. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.R.; Quinn, S.F.; Wensel, J.P.; Kim, J.H.; Demlow, T. Diagnosis of popliteus injuries with MR imaging. Skelet. Radiol. 1995, 24, 511–514. [Google Scholar] [CrossRef] [PubMed]
- Ortiguera, C.J.; Bremner, B.R.B.; Peterson, J.J. Popliteus Strain Causing Tibial Nerve Palsy with a Permanent Partial Deficit: A Case Report. Am. J. Sports Med. 2006, 34, 1176–1180. [Google Scholar] [CrossRef] [PubMed]
- Iida, T.; Kobayashi, M. Tibial nerve entrapment at the tendinous arch of the soleus: A case report. Clin. Orthop. Relat. Res. 1997, 334, 265–269. [Google Scholar] [CrossRef]
- Merriman, J.; Villacis, D.; Kephart, C.; Yi, A.; Romano, R.; Hatch, G.F.R. Acute Compartment Syndrome after Non-Contact Peroneus Longus Muscle Rupture. Clin. Orthop. Surg. 2015, 7, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Schumer, E.D. Isolated compartment syndrome of the pronator quadratus compartment: A case report. J. Hand Surg. Am. 2004, 29, 299–301. [Google Scholar] [CrossRef] [PubMed]
- Mastaglia, F.L.; Venerys, J.; Stokes, B.A.; Vaughan, R. Compression of the tibial nerve by the tendinous arch of origin of the soleus muscle. Clin. Exp. Neurol. 1981, 18, 81–85. [Google Scholar] [PubMed]
- Saal, J.A.; Dillingham, M.F.; Gamburd, R.S.; Fanton, G.S. The pseudoradicular syndrome: Lower extremity peripheral nerve entrapment masquerading as lumbar radiculopathy. Spine 1988, 13, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Podore, P.C. Popliteal entrapment syndrome: A report of tibial nerve entrapment. J. Vasc. Surg. 1985, 2, 335–336. [Google Scholar] [CrossRef] [PubMed]
- Bollier, M.; Ream, T.; Hodgman, G. Isolated popliteus muscle rupture with neurovascular compression requiring surgical decompression. Am. J. Orthop. 2010, 39, 588–591. [Google Scholar] [PubMed]
- Bowditch, M.G.; Kay, N.R. Painful swollen calf due to isolated rupture of popliteus. Injury 1994, 25, 200–201. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.J.; Kang, S.; Ko, S.; Baek, J.; Kim, Y.; Park, N.K. Neurovascular Compression Caused by Popliteus Muscle Enlargement Without Discrete Trauma. Ann. Rehabil. Med. 2016, 40, 545–550. [Google Scholar] [CrossRef] [PubMed]
- De Ruiter, G.C.W.; Torchia, M.E.; Amrami, K.K.; Spinner, R.J. Neurovascular compression following isolated popliteus muscle rupture: A case report. J. Surg. Orthop. Adv. 2005, 14, 129–132. [Google Scholar] [PubMed]
- Dimberg, E.L.; Rubin, D.I.; Ortiguera, C.J.; Kennelly, K.D. Popliteus muscle hemorrhage as a rare cause of a proximal tibial neuropathy. J. Clin. Neurosci. 2014, 21, 520–521. [Google Scholar] [CrossRef] [PubMed]
- Channabasappa, S.M.; Shankarnarayana, P. A comparative study of hemodynamic changes between prone and supine emergence from anesthesia in lumbar disc surgery. Anesth. Essays Res. 2013, 7, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Kwee, M.M.; Ho, Y.H.; Rozen, W.M. The prone position during surgery and its complications: A systematic review and evidence-based guidelines. Int. Surg. 2015, 100, 292–303. [Google Scholar] [CrossRef] [PubMed]


| Patient [Ref.] | Trauma | Clinical Presentation | Imaging/EMG Findings | Treatment | Outcome |
|---|---|---|---|---|---|
| 59 yo man [2] | Twisting of knee while playing tennis | Pain and swelling right calf; FHL, FDL, and TP: M0; ↓ sensation sole of foot | Venogram: obstruction; X-ray: degenerative changes; MRI: PM rupture and hematoma and TN compression; EMG: TN axonotmesis | Conservative | At 6 months: toe flexion recovered; no further details |
| 41 yo female [12] | Running | Pain and swelling right calf; partial TN palsy; altered sensation sole of foot | X-ray: normal; MRI: PM rupture and fluid collection | Conservative | Not specified |
| 58 yo female [5] | No trauma | Pain sole of left foot aggravated by ankle motion; FHL and FDL: M0; altered sensation sole of foot | CT and MRI: PM hypertrophy and high-signal lesion on T2-weighted; EMG: denervation FHL and FDL | Neurolysis posterior approach | At 12 months: No pain; Normal sensation sole; FHL and FDL: M4 |
| 59 yo man [14] | Fall from a horse | Biphasic progressive onset; complete TN palsy | X-ray: unremarkable; MRI: PM rupture and hemorrhage and edema and TN Compression | Conservative | At 24 months: toe flexion deficit; intrinsic palsy; protective sensation sole of the foot |
| 57 yo man [4] | Tennis match/no trauma | Biphasic progressive onset; numbness of the sole of the foot; partial palsy; FHL and FDL: M3 | X-ray: degenerative changes; MRI: PM enlargement and TN compression | Conservative | At 8 months: sole numbness FHL and FDL: M4 |
| 34 yo man [11] | Twisting injury | Biphasic progressive onset; immediate posterior knee pain; altered sensation sole of foot; toes flexion: M0 | X-ray: unremarkable; MRI: PM rupture and necrosis and compression popliteal vein and TN | Neurolysis posterior approach | At 9 months: medial sensation recovered; FHL: M1; plantar flexion: M5 |
| 54 yo man [15] | Jump with knee hyperextension | Biphasic progressive onset; posterior knee pain; toe flexion weakness; loss sensation sole of foot; absent Achilles reflex | MRI: PM thickness, edema, and hemorrhage; EMG: TN palsy | Conservative | At 15 months: moderate improvement toe flexion, persistent pain, and sensory loss |
| 57 yo man [13] | No trauma | Pain left calf; numbness sole of foot; FHL: M1; progressive worsening of symptoms | AngioCT: popliteal artery stenosis; MRI: PM edema and enlargement; EMG: TN palsy | Neurolysis posterior approach | Immediate pain relief after surgery. At 2 months: partial deficit; FHL still impaired |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jolliet, S.; Harder, Y.; Durand, S. Tibial Nerve Palsy Secondary to Spontaneous Isolated Popliteus Muscle Rupture and Localized Compartment Syndrome. Diagnostics 2025, 15, 2990. https://doi.org/10.3390/diagnostics15232990
Jolliet S, Harder Y, Durand S. Tibial Nerve Palsy Secondary to Spontaneous Isolated Popliteus Muscle Rupture and Localized Compartment Syndrome. Diagnostics. 2025; 15(23):2990. https://doi.org/10.3390/diagnostics15232990
Chicago/Turabian StyleJolliet, Sophie, Yves Harder, and Sébastien Durand. 2025. "Tibial Nerve Palsy Secondary to Spontaneous Isolated Popliteus Muscle Rupture and Localized Compartment Syndrome" Diagnostics 15, no. 23: 2990. https://doi.org/10.3390/diagnostics15232990
APA StyleJolliet, S., Harder, Y., & Durand, S. (2025). Tibial Nerve Palsy Secondary to Spontaneous Isolated Popliteus Muscle Rupture and Localized Compartment Syndrome. Diagnostics, 15(23), 2990. https://doi.org/10.3390/diagnostics15232990







