Anatomical Insights into the Lateral Meniscus and Anterolateral Ligament: A Cadaveric Study
Abstract
1. Introduction
2. Materials and Methods
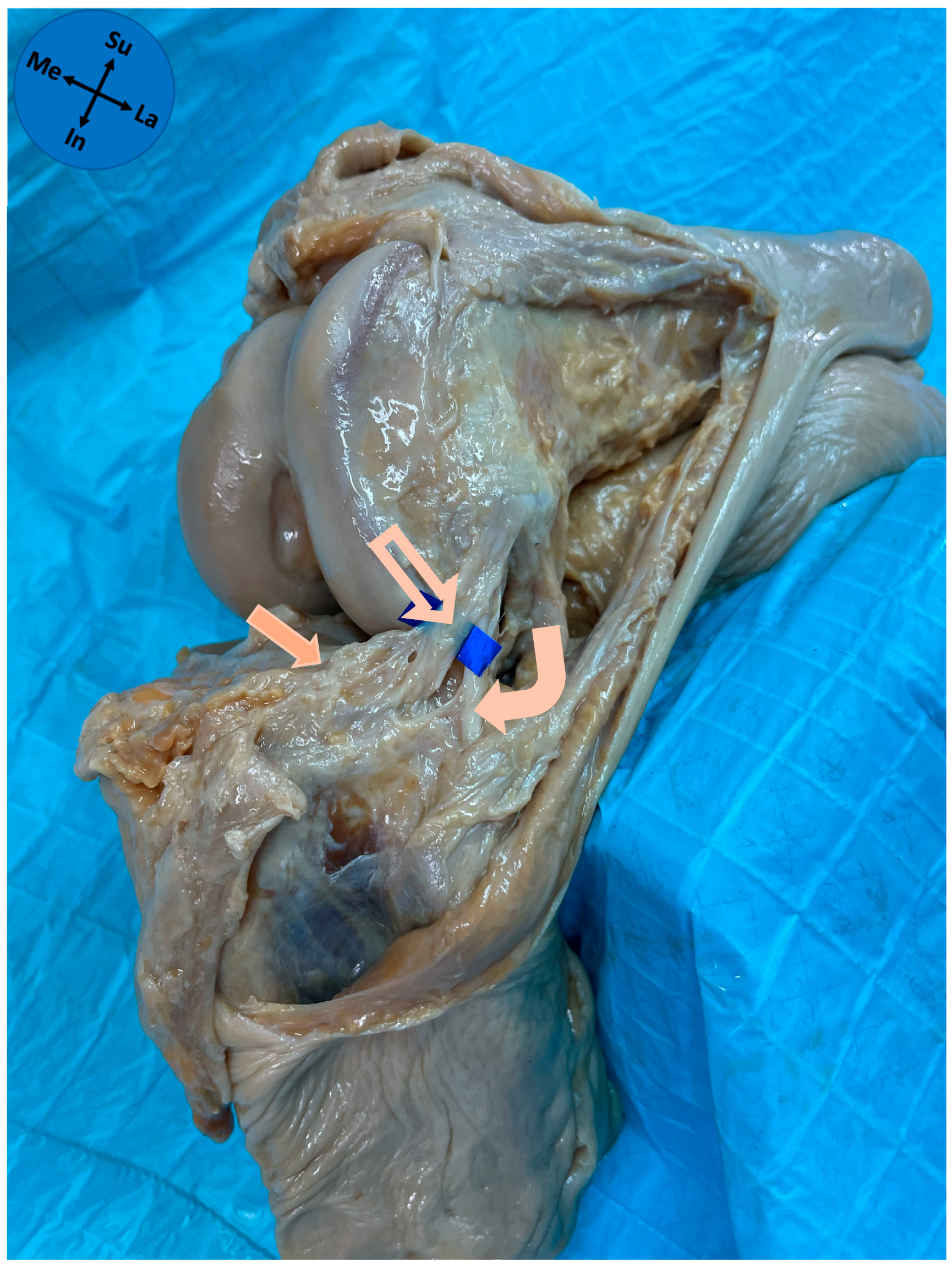
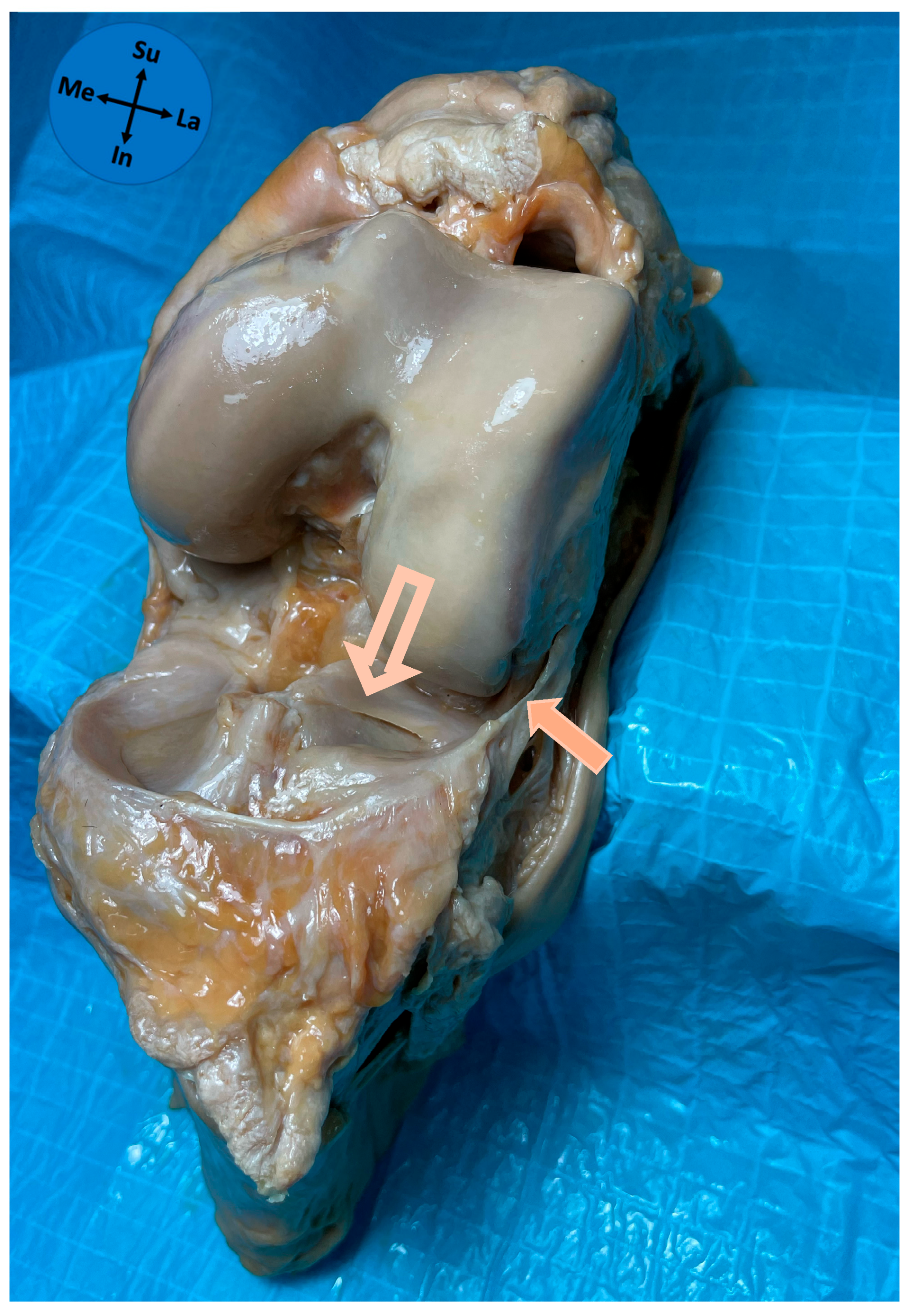
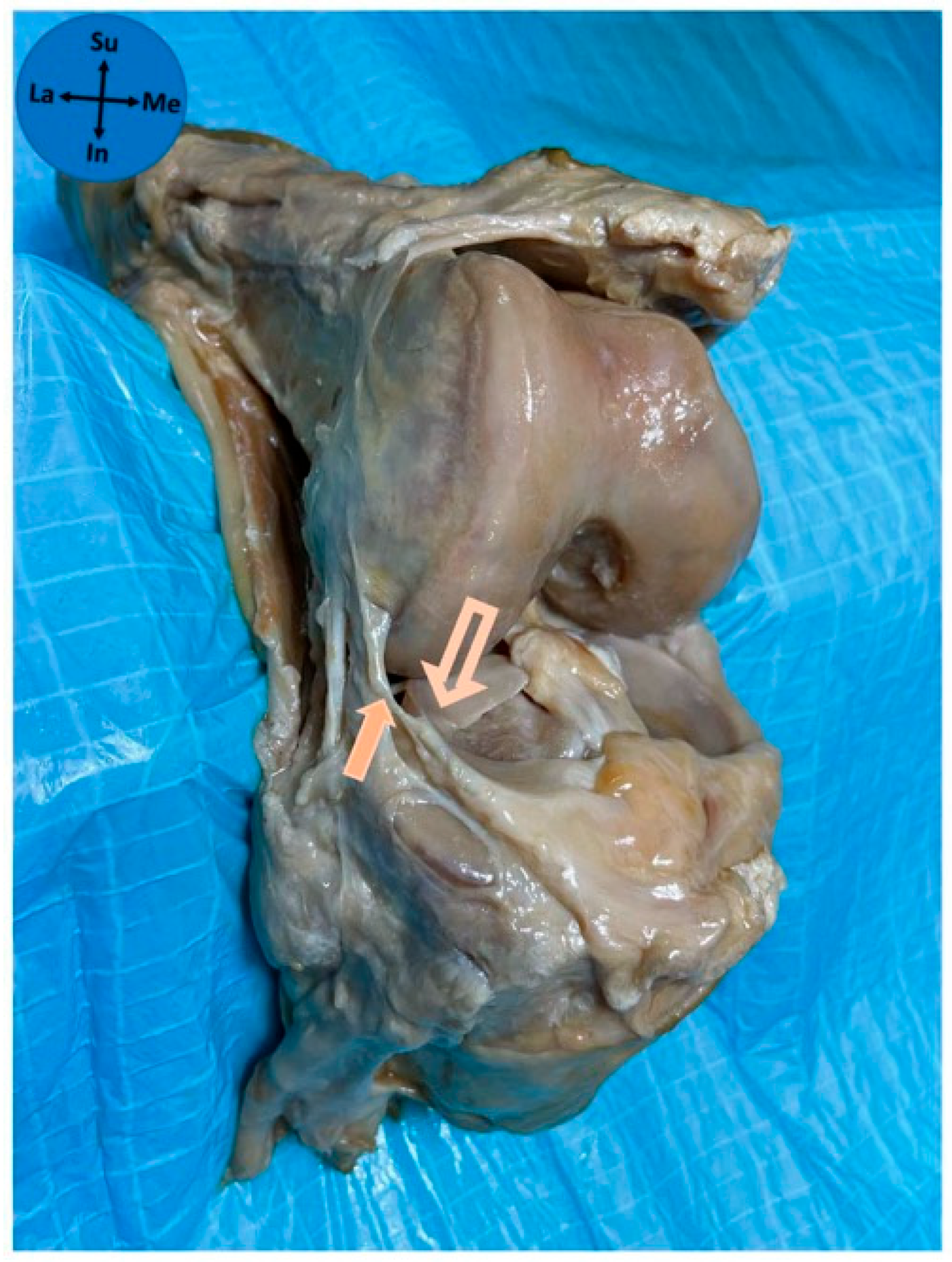
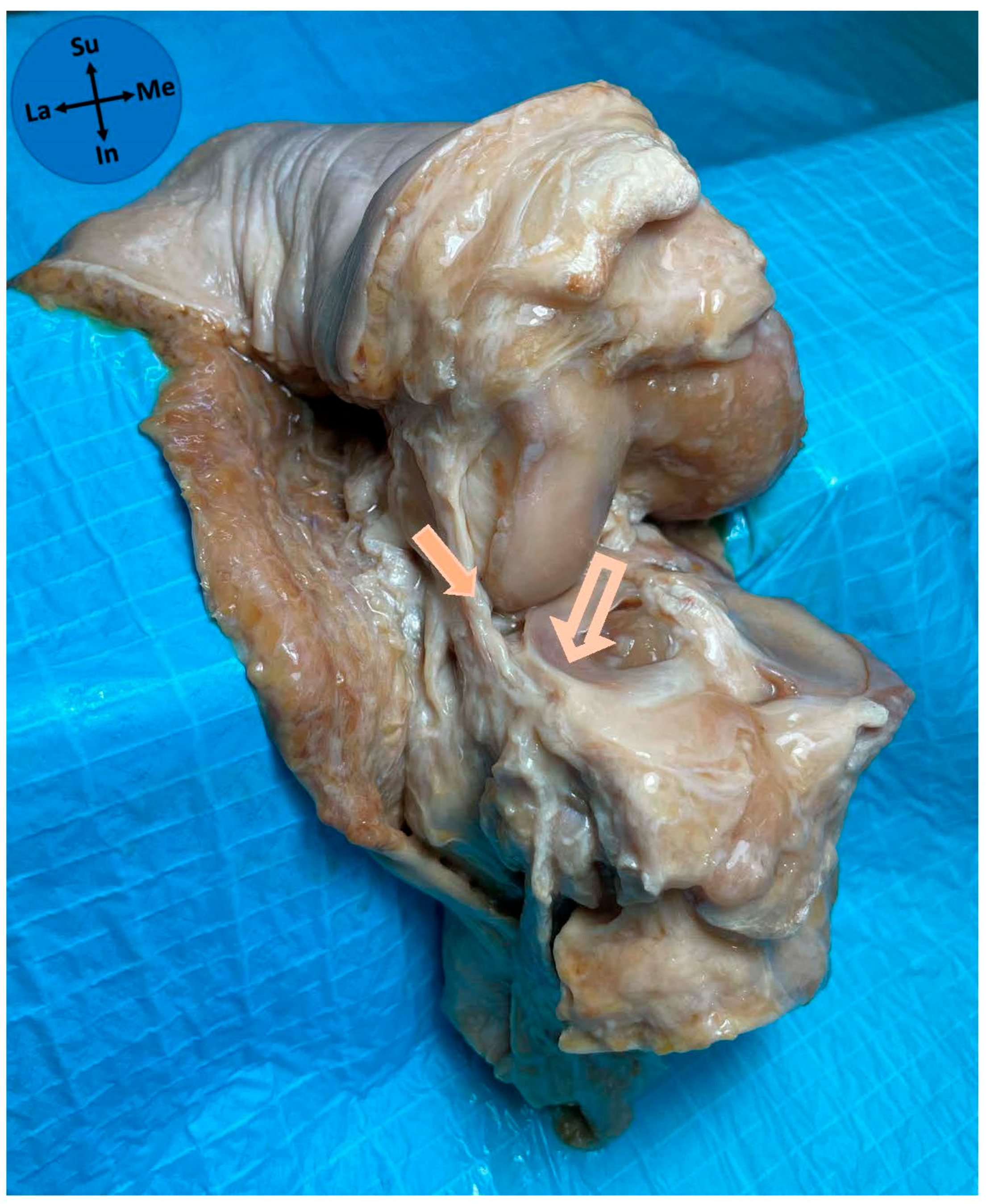
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ALL | Anterolateral ligament |
| P25–P75 | 25th–75th percentiles |
| ACL | Anterior cruciate ligament |
| ITT | Iliotibial tract |
| FCL | Fibular collateral ligament |
References
- Segond, P. Recherches cliniques et experimentales sur les épanchements sanguins du genou par entorse. Prog. Med. 1879, 7, 297–341. [Google Scholar]
- Moorman, C.T., III; LaPrade, R.F. Anatomy and biomechanics of the posterolateral corner of the knee. J. Knee Surg. 2005, 18, 137–145. [Google Scholar] [CrossRef]
- Vincent, J.P.; Magnussen, R.A.; Gezmez, F.; Uguen, A.; Jacobi, M.; Weppe, F.; Al-Saati, M.F.; Lustig, S.; Demey, G.; Servien, E.; et al. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 147–152. [Google Scholar] [CrossRef]
- Cavaignac, E.; Ancelin, D.; Chiron, P.; Tricoire, J.L.; Wytrykowski, K.; Faruch, M.; Chantalat, E. Historical perspective on the “discovery” of the anterolateral ligament of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 991–996. [Google Scholar] [CrossRef]
- Claes, S.; Vereecke, E.; Maes, M.; Victor, J.; Verdonk, P.; Bellemans, J. Anatomy of the anterolateral ligament of the knee. J. Anat. 2013, 223, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Musahl, V.; Rahnemai-Azar, A.A.; van Eck, C.F.; Guenther, D.; Fu, F.H. Anterolateral ligament of the knee, fact or fiction? Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Moroz, P.A.; Quick, E.E.; Horner, N.S.; Duong, A.; Simunovic, N.; Ayeni, O.R. What Is the State of the Evidence in Anterolateral Ligament Research? Clin. Sports Med. 2018, 37, 137–159. [Google Scholar] [CrossRef] [PubMed]
- Sonnery-Cottet, B.; Daggett, M.; Fayard, J.M.; Ferretti, A.; Helito, C.P.; Lind, M.; Monaco, E.; de Pádua, V.B.C.; Thaunat, M.; Wilson, A.; et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament—deficient knee. J. Orthop. Traumatol. 2017, 18, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Caterine, S.; Litchfield, R.; Johnson, M.; Chronik, B.; Getgood, A. A cadaveric study of the anterolateral ligament: Re-introducing the lateral capsular ligament. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3186–3195. [Google Scholar] [CrossRef]
- Fernandes, J.C.; Pinho, A.R.; Pereira, P.A.; Madeira, M.D.; Raposo, F.A.; Sousa, A.N.; Lobo, J.M. Anterolateral ligament of the knee-Cadaver study in a Caucasian population. Rev. Esp. Cir. Ortop. Traumatol. 2023, 67, 134–138. [Google Scholar] [CrossRef]
- Stijak, L.; Bumbaširević, M.; Radonjić, V.; Kadija, M.; Puškaš, L.; Milovanović, D.; Filipović, B. Anatomic description of the anterolateral ligament of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.I.; Claes, S.; Fuso, F.A.; Williams, B.T.; Goldsmith, M.T.; Turnbull, T.L.; Wijdicks, C.A.; LaPrade, R.F. The Anterolateral Ligament: An Anatomic, Radiographic, and Biomechanical Analysis. Am. J. Sports Med. 2015, 43, 1606–1615. [Google Scholar] [CrossRef] [PubMed]
- Vap, A.R.; Schon, J.M.; Moatshe, G.; Cruz, R.S.; Brady, A.W.; Dornan, G.J.; Turnbull, T.L.; LaPrade, R.F. The Role of the Peripheral Passive Rotation Stabilizers of the Knee with Intact Collateral and Cruciate Ligaments: A Biomechanical Study. Orthop. J. Sports Med. 2017, 5, 2325967117708190. [Google Scholar] [CrossRef] [PubMed]
- Monaco, E.; Maestri, B.; Conteduca, F.; Mazza, D.; Iorio, C.; Ferretti, A. Extra-articular ACL Reconstruction and Pivot Shift: In Vivo Dynamic Evaluation With Navigation. Am. J. Sports Med. 2014, 42, 1669–1674. [Google Scholar] [CrossRef]
- Fox, A.J.; Wanivenhaus, F.; Burge, A.J.; Warren, R.F.; Rodeo, S.A. The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat. 2015, 28, 269–287. [Google Scholar] [CrossRef]
- Totlis, T.; Tishukov, M.; Piagkou, M.; Vasiliadis, A.V.; Tsiouris, C.; Domashenko, P.; Tsakotos, G.; Natsis, K. The Anterolateral Ligament of the Knee Is a Nonisometric Thin Ligament with High Prevalence and Almost Constant Attachment to the Lateral Meniscus: A Systematic Review with Meta-analysis. Arthroscopy 2024, 40, 1288–1299. [Google Scholar] [CrossRef]
- Helito, C.P.; Bonadio, M.B.; Soares, T.Q.; da Mota e Albuquerque, R.F.; Natalino, R.J.; Pécora, J.R.; Camanho, G.L.; Demange, M.K. The meniscal insertion of the knee anterolateral ligament. Surg. Radiol. Anat. 2016, 38, 223–228. [Google Scholar] [CrossRef]
- Eisma, R.; Lamb, C.; Soames, R.W. From formalin to Thiel embalming: What changes? One anatomy department’s experiences. Clin. Anat. 2013, 26, 564–571. [Google Scholar] [CrossRef]
- Loukas, M.; Tubbs, R.S.; Benninger, B. Gray’s Clinical Photographic Dissector of the Human Body, 2nd ed.; Elsevier: Philadelphia, PA, USA, 2019. [Google Scholar]
- Standring, S., Editor-in-Chief. Gray’s Anatomy—The Anatomical Basis of Clinical Practice, 42nd ed.; Elsevier: Philadelphia, PA, USA, 2021. [Google Scholar]
- Mameri, E.S.; Dasari, S.P.; Fortier, L.M.; Verdejo, F.G.; Gursoy, S.; Yanke, A.B.; Chahla, J. Review of Meniscus Anatomy and Biomechanics. Curr. Rev. Musculoskelet. Med. 2022, 15, 323–335. [Google Scholar] [CrossRef]
- Cho, H.J.; Kwak, D.S. Anatomical Consideration of the Anterolateral Ligament of the Knee. Biomed. Res. Int. 2019, 2019, 5740473. [Google Scholar] [CrossRef]
- Roessler, P.P.; Schüttler, K.F.; Stein, T.; Gravius, S.; Heyse, T.J.; Prescher, A.; Wirtz, D.C.; Efe, T. Anatomic dissection of the anterolateral ligament (ALL) in paired fresh-frozen cadaveric knee joints. Arch. Orthop. Trauma. Surg. 2017, 137, 249–255. [Google Scholar] [CrossRef]
- Fardin, P.B.A.; Lizardo, J.H.F.; Baptista, J.D.S. Study of the anterolateral ligament of the knee in formalin—Embedded cadavers. Acta Ortop. Bras. 2017, 25, 89–92. [Google Scholar] [CrossRef]
- Shea, K.G.; Polousky, J.D.; Jacobs, J.C., Jr.; Yen, Y.M.; Ganley, T.J. The Anterolateral Ligament of the Knee: An Inconsistent Finding in Pediatric Cadaveric Specimens. J. Pediatr. Orthop. 2016, 36, e51–e54. [Google Scholar] [CrossRef]
- Helito, C.P.; Miyahara, H.S.; Bonadio, M.B.; Tirico, L.E.P.; Gobbi, R.G.; Demange, M.K.; Angelini, F.J.; Pecora, J.R.; Camanho, G.L. Anatomical study on the anterolateral ligament of the knee. Rev. Bras. Ortop. 2013, 48, 368–373. [Google Scholar] [CrossRef]
- Kosy, J.D.; Mandalia, V.I.; Anaspure, R. Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skelet. Radiol. 2015, 44, 1647–1653. [Google Scholar] [CrossRef] [PubMed]
- Monaco, E.; Ferretti, A.; Labianca, L.; Maestri, B.; Speranza, A.; Kelly, M.J.; D’Arrigo, C. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Helito, C.P.; Helito, P.V.; Bonadio, M.B.; da Mota e Albuquerque, R.F.; Bordalo-Rodrigues, M.; Pecora, J.R.; Camanho, G.L.; Demange, M.K. Evaluation of the Length and Isometric Pattern of the Anterolateral Ligament with Serial Computer Tomography. Orthop. J. Sports Med. 2014, 2, 2325967114562205. [Google Scholar] [CrossRef] [PubMed]
- Helito, C.P.; Demange, M.K.; Bonadio, M.B.; Tírico, L.E.; Gobbi, R.G.; Pécora, J.R.; Camanho, G.L. Anatomy and Histology of the Knee Anterolateral Ligament. Orthop. J. Sports Med. 2013, 1, 2325967113513546. [Google Scholar] [CrossRef]
- Dumont, G.D.; Hogue, G.D.; Padalecki, J.R.; Okoro, N.; Wilson, P.L. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: Relationship of treatment time and patient-specific factors. Am. J. Sports Med. 2012, 40, 2128–2133. [Google Scholar] [CrossRef]
- Claes, S.; Bartholomeeusen, S.; Bellemans, J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop. Belg. 2014, 80, 45–49. [Google Scholar]
- Willinger, L.; Athwal, K.K.; Holthof, S.; Imhoff, A.B.; Williams, A.; Amis, A.A. Role of the Anterior Cruciate Ligament, Anterolateral Complex, and Lateral Meniscus Posterior Root in Anterolateral Rotatory Knee Instability: A Biomechanical Study. Am. J. Sports Med. 2023, 51, 1136–1145. [Google Scholar] [CrossRef] [PubMed]
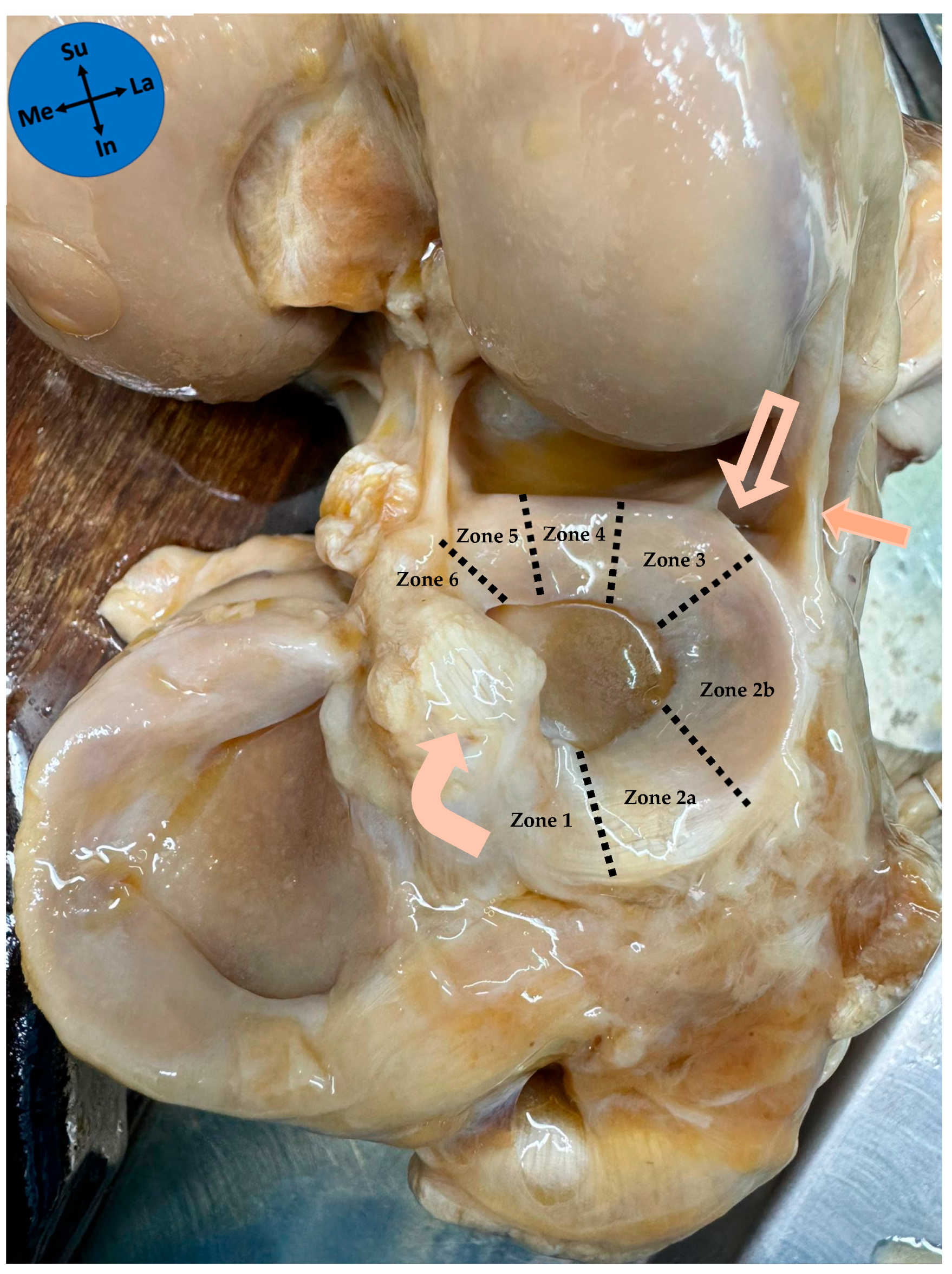

| Meniscal Zone of Attachment | n (%) |
|---|---|
| Zone 2a | 1 (3.2) |
| Zone 2b | 30 (96.8) |
| Pattern of meniscal attachment | n (%) |
| Full thickness | 13 (41.9) |
| Bipolar | 11 (35.5) |
| Superior-only | 4 (12.9) |
| Inferior-only | 3 (9.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lobo, J.; Almeida, J.; Fernandes, J.; Alves, H.; Pinho, A.R.; Madeira, M.D.; Fernandes, L.; Esteves, A.; Pereira, P.A. Anatomical Insights into the Lateral Meniscus and Anterolateral Ligament: A Cadaveric Study. Diagnostics 2025, 15, 2987. https://doi.org/10.3390/diagnostics15232987
Lobo J, Almeida J, Fernandes J, Alves H, Pinho AR, Madeira MD, Fernandes L, Esteves A, Pereira PA. Anatomical Insights into the Lateral Meniscus and Anterolateral Ligament: A Cadaveric Study. Diagnostics. 2025; 15(23):2987. https://doi.org/10.3390/diagnostics15232987
Chicago/Turabian StyleLobo, João, Joana Almeida, José Fernandes, Hélio Alves, André Rodrigues Pinho, Maria Dulce Madeira, Levi Fernandes, Ana Esteves, and Pedro Alberto Pereira. 2025. "Anatomical Insights into the Lateral Meniscus and Anterolateral Ligament: A Cadaveric Study" Diagnostics 15, no. 23: 2987. https://doi.org/10.3390/diagnostics15232987
APA StyleLobo, J., Almeida, J., Fernandes, J., Alves, H., Pinho, A. R., Madeira, M. D., Fernandes, L., Esteves, A., & Pereira, P. A. (2025). Anatomical Insights into the Lateral Meniscus and Anterolateral Ligament: A Cadaveric Study. Diagnostics, 15(23), 2987. https://doi.org/10.3390/diagnostics15232987






