Journal Description
Current Oncology
Current Oncology
is an international, peer-reviewed, open access journal published online by MDPI (from Volume 28 Issue 1-2021). Established in 1994, the journal represents a multidisciplinary medium for clinical oncologists to report and review progress in the management of this disease. The Canadian Association of Medical Oncologists (CAMO), the Canadian Association of Psychosocial Oncology (CAPO), the Canadian Association of General Practitioners in Oncology (CAGPO), the Cell Therapy Transplant Canada (CTTC), the Canadian Leukemia Study Group (CLSG) and others are affiliated with the journal and their members receive a discount on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Oncology)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 19.8 days after submission; acceptance to publication is undertaken in 2.4 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
3.4 (2024);
5-Year Impact Factor:
3.3 (2024)
Latest Articles
Cannabidiol (CBD) and Colorectal Tumorigenesis: Potential Dual Modulatory Roles via the Serotonergic Pathway
Curr. Oncol. 2025, 32(7), 375; https://doi.org/10.3390/curroncol32070375 - 26 Jun 2025
Abstract
The 2018 Farm Bill legalized hemp-derived cannabidiol (CBD) products containing less than 0.3% tetrahydrocannabinol (THC) in the United States. This legislative shift catalyzed both public and scientific interest in CBD’s potential health benefits. However, the rapid expansion of the CBD market has considerably
[...] Read more.
The 2018 Farm Bill legalized hemp-derived cannabidiol (CBD) products containing less than 0.3% tetrahydrocannabinol (THC) in the United States. This legislative shift catalyzed both public and scientific interest in CBD’s potential health benefits. However, the rapid expansion of the CBD market has considerably outpaced rigorous scientific research, leaving many health claims largely unsubstantiated. While preclinical studies suggest that CBD may exert antitumorigenic effects in colorectal cancer (CRC) by modulating cell proliferation, apoptosis, and inflammation, clinical evidence supporting these effects remains limited. This review critically examines the current evidence on the role of CBD in colorectal tumorigenesis, with particular attention to its molecular mechanisms and interactions with the serotonergic system—a signaling pathway implicated in the development of CRC and possessing potential dual anti- and pro-tumorigenic properties. By influencing the serotonergic system, CBD may confer both protective and potentially deleterious effects during CRC development. This review underscores the need for further research to elucidate the complex mechanisms of CBD in colorectal tumorigenesis and to evaluate its therapeutic potential in clinical settings. Understanding these interactions could pave the way for novel prevention and treatment strategies, optimizing the anticancer efficacy of CBD while mitigating unintended risks.
Full article
(This article belongs to the Special Issue Bridging Borders: A Global Perspective on Colorectal Cancer Research and Prevention)
►
Show Figures
Open AccessArticle
Preoperative Chemoradiation (Modified Eilber Protocol) Versus Preoperative/Postoperative Radiotherapy for Soft Tissue Sarcomas: A Population-Based Analysis
by
Greg M. Padmore, Elizabeth C. Kurien, Michael J. Monument, Lloyd Mack, Antoine Bouchard-Fortier and on behalf of the ISARP Group
Curr. Oncol. 2025, 32(7), 374; https://doi.org/10.3390/curroncol32070374 - 26 Jun 2025
Abstract
Background: Local recurrence for high-risk extremities/trunk soft tissue sarcoma (STS) after treatment can range from 15 to 30%. The modified Eilber protocol (MEP) using low-dose intravenous chemotherapy with a reduced dosage of radiation in the preoperative setting has demonstrated excellent local control and
[...] Read more.
Background: Local recurrence for high-risk extremities/trunk soft tissue sarcoma (STS) after treatment can range from 15 to 30%. The modified Eilber protocol (MEP) using low-dose intravenous chemotherapy with a reduced dosage of radiation in the preoperative setting has demonstrated excellent local control and reduced wound complications in these patients. The aim of the current study was to assess long-term local control and overall survival in patients with STS treated with the MEP versus standard preoperative or postoperative radiotherapy. Methods: Patients diagnosed with STS from 2004 to 2016 were identified using the Alberta Cancer Registry. Patients with STS treated with the MEP, preoperative or postoperative radiotherapy, were included. Patient and tumor characteristics, treatments and outcomes were abstracted from the registry and primary chart review. Characteristics were compared using one-way ANOVA for continuous variable and chi-square test and Fisher test for the categorical outcomes. Local recurrence-free survival and overall survival were analyzed using Kaplan–Meier Analysis with Log-rank test. Results: A total of 242 patients with STS were included, among which 100 (41.3%) received the MEP prior to surgery, 91 (37.6%) had preoperative radiation, and 51 (21.1%) had postoperative radiation. After a median follow up of 4.9 years, there were no significant differences in local recurrence or local recurrence-free survival between patients treated with the MEP vs. preoperative or postoperative radiotherapy (10 vs. 6.6% and 7.8%, respectively, p-value NS). There were also no significant differences between groups for recurrence-free survival and overall survival. Conclusions: This study demonstrates that the use of the MEP has non-inferior oncologic outcomes compared to standard preoperative or postoperative radiation in a population-based analysis despite reducing the overall dosage of radiation administered. The modified Eilber preoperative chemoradiation protocol may be considered as an additional option for patients with STS.
Full article
(This article belongs to the Special Issue Sarcoma Surgeries: Oncological Outcomes and Prognostic Factors)
►▼
Show Figures
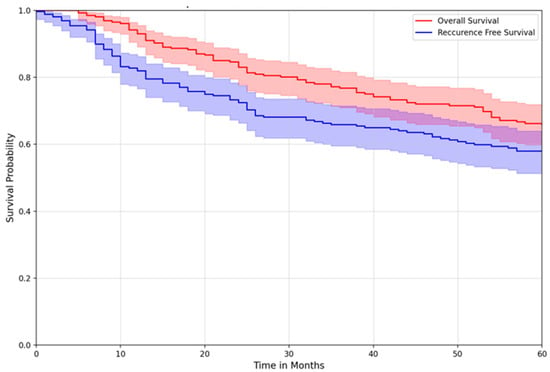
Figure 1
Open AccessReview
Role of Circulating Tumor DNA in Adapting Immunotherapy Approaches in Breast Cancer
by
Sudhir Kumar and Rossanna C. Pezo
Curr. Oncol. 2025, 32(7), 373; https://doi.org/10.3390/curroncol32070373 - 26 Jun 2025
Abstract
Immunotherapy has a defined role in the treatment of both early- and late-stage triple-negative breast cancer (TNBC) and is under active exploration in human epidermal receptor 2-positive as well as high-risk hormone-receptor-positive subtypes. It is critical to balance the efficacy and toxicity of
[...] Read more.
Immunotherapy has a defined role in the treatment of both early- and late-stage triple-negative breast cancer (TNBC) and is under active exploration in human epidermal receptor 2-positive as well as high-risk hormone-receptor-positive subtypes. It is critical to balance the efficacy and toxicity of immunotherapy while keeping the cost and duration of treatment in check. In addition to the immunohistochemistry testing of PD-L1 expression, which only predicts the efficacy of immunotherapy in metastatic TNBC, there is a lack of biomarkers that are better standardized to predict efficacy and treatment response, detect early relapse, and guide prognosis in breast cancer patients treated with immunotherapy. Circulating tumor DNA (ctDNA) is a minimally invasive, dynamic, real-time, blood-based biomarker that has shown promising value in the management of solid tumors, including breast cancer. This review discusses the emerging evidence for the potential application of ctDNA to further refine patient-centered care and personalize treatment based on a molecularly defined risk assessment for breast cancer patients treated with immunotherapy-based approaches. We further discuss the challenges and barriers to widespread adoption of this promising tool in the management of breast cancer patients requiring immunotherapy.
Full article
(This article belongs to the Special Issue Advances in Immunotherapy for Breast Cancer)
►▼
Show Figures
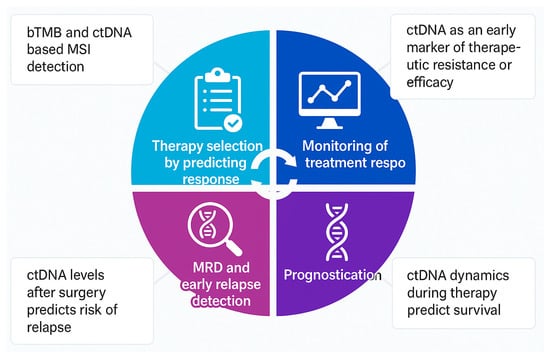
Figure 1
Open AccessArticle
Insights into the Prognostic Efficacy of the Geriatric Nutritional Risk Index for Nasopharyngeal Carcinoma in the Era of Volumetric Modulated Arc Therapy: A Nomogram for Predicting Long-Term Survival Outcomes
by
Xiang Lin, Wei Wang, Jianming Ding, Zhaodong Fei and Chuanben Chen
Curr. Oncol. 2025, 32(7), 372; https://doi.org/10.3390/curroncol32070372 - 26 Jun 2025
Abstract
Background: The geriatric nutritional risk index (GNRI), a composite metric of serum albumin and body weight, has emerged as a prognostic tool in various cancers. However, its relevance in nasopharyngeal carcinoma (NPC) patients treated with volumetric modulated arc therapy (VMAT) remains unexplored. The
[...] Read more.
Background: The geriatric nutritional risk index (GNRI), a composite metric of serum albumin and body weight, has emerged as a prognostic tool in various cancers. However, its relevance in nasopharyngeal carcinoma (NPC) patients treated with volumetric modulated arc therapy (VMAT) remains unexplored. The aim of this study was to assess the effect of the GNRI in the prediction of the prognosis of nasopharyngeal carcinoma in the era of VMAT. Methods: This retrospective study analyzed 498 newly diagnosed, non-metastatic NPC patients treated with VMAT between 2010 and 2011. The GNRI was calculated using serum albumin and body weight ratios, with receiver operating characteristic (ROC) curve analysis determining its optimal prognostic cutoff. Patients were stratified into training (70%) and validation (30%) cohorts. Cox regression identified independent prognostic factors, which were integrated into a nomogram predicting 3- and 5-year overall survival (OS). Model performance was assessed via the concordance index (C-index), calibration curves, and decision curve analysis (DCA). Results: In the study, 348 patients were included in the training cohort and 150 patients were included in the validation cohort according to a ratio of 7:3. The median follow-up was 68 months, with 5-year OS rates of 79.3%. A GNRI > 102 independently predicted improved survival (HR = 0.64; p = 0.044), alongside tumor volume, age, and N-stage. The nomogram demonstrated strong discrimination (C-index: 0.757–0.762 for training; 0.737–0.744 for validation) and calibration, aligning closely with observed survival. DCA confirmed superior clinical utility over default strategies. NPC patients treated with VMAT with a high GNRI, female sex, and a lower N-stage exhibited significantly better OS (p < 0.05). Conclusions: The GNRI is a robust prognostic marker for NPC patients receiving VMAT, reflecting the interplay of nutrition, inflammation, and treatment response. The validated nomogram provides a practical tool for individualized risk stratification, enhancing clinical decision-making in the era of precision radiotherapy.
Full article
(This article belongs to the Special Issue The Evolving Landscape of Precision Medicine in Radiation Oncology)
►▼
Show Figures
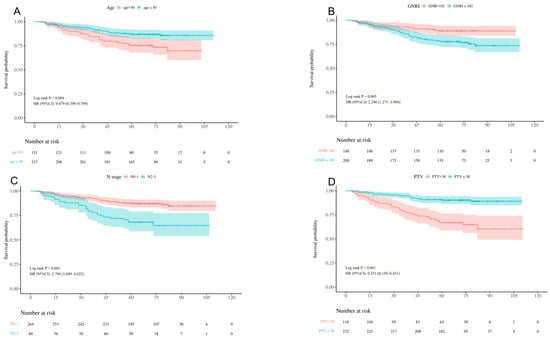
Figure 1
Open AccessArticle
The Impact of Adjuvant Chemotherapy on Clinical Outcomes in Locally Advanced Rectal Cancer: A CHORD Consortium Analysis
by
Kaveh Farrokhi, Horia Marginean, Anas Al Ghamdi, Essa Al Mansor, Shaan Dudani, Rachel A. Goodwin, Timothy R. Asmis, Erin Powell, Patricia A. Tang, Richard Lee-Ying and Michael M. Vickers
Curr. Oncol. 2025, 32(7), 371; https://doi.org/10.3390/curroncol32070371 - 26 Jun 2025
Abstract
Background: The impact of adjuvant chemotherapy (AC) on outcomes in real-world patients with locally advanced rectal cancer (LARC) remains uncertain. Methods: Consecutive patients with LARC (stage II/III) undergoing neoadjuvant chemoradiation before curative-intent surgery from 2005 to 2013 were identified in the Canadian Health
[...] Read more.
Background: The impact of adjuvant chemotherapy (AC) on outcomes in real-world patients with locally advanced rectal cancer (LARC) remains uncertain. Methods: Consecutive patients with LARC (stage II/III) undergoing neoadjuvant chemoradiation before curative-intent surgery from 2005 to 2013 were identified in the Canadian Health Outcomes Research Database. The impact of AC on clinical outcomes, including disease-free survival (DFS) and overall survival (OS), was evaluated using the Kaplan–Meier method and Cox proportional hazards modeling. Results: A total of 1448 patients had sufficient data available to be included for analysis with 1085 (74.9%) receiving AC. Of AC patients, 40.5% received oxaliplatin-based treatments. With a median follow-up of 66.43 months, the 5-year DFS rate was 67.7% (95% CI: 64.5–70.1%) vs. 58.7% (95% CI: 52.8–64.2%) in the AC group and non-AC group, respectively (p < 0.001). The 5-year OS rate of the whole cohort was 74.3% (95% CI: 71.5–76.85%) while the 5-year OS rate of the AC group was 77.8% (95% CI: 74.7–80.6%) compared with 63.8% (95% CI: 57.9–69.2%) for the non-AC group (p < 0.001). On multivariate analysis, patients who received AC had improved DFS (HR 0.6, 95% CI: 0.49–0.73, p < 0.001) and OS (HR 0.46, 95% CI: 0.36–0.58, p < 0.001). Conclusions: This large multi-institutional database analysis supports the use of AC in real-world LARC patients treated with nCRT followed by surgical resection.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures
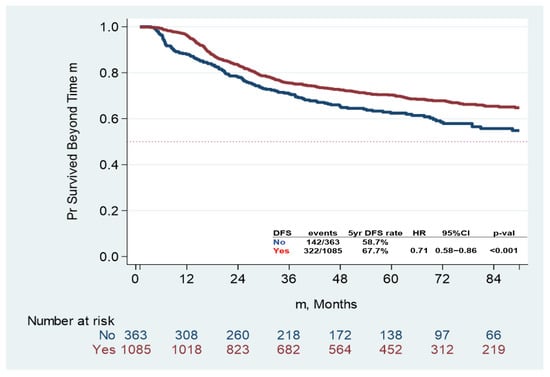
Figure 1
Open AccessCase Report
Unveiling ctDNA Response: Immune Checkpoint Blockade Therapy in a Patient with POLE Mutation-Associated Early-Onset Colon Cancer
by
Ramya Ramachandran, Marisa Cannon, Supriya Peshin, Madappa Kundranda and Aaron J. Scott
Curr. Oncol. 2025, 32(7), 370; https://doi.org/10.3390/curroncol32070370 - 25 Jun 2025
Abstract
Colorectal cancer (CRC) is the third most common malignancy worldwide and the second leading cause of cancer-related mortality in the United States. The incidence of early-onset colorectal cancer (EOCRC) has been increasing over the past several decades. While the etiologies for this rising
[...] Read more.
Colorectal cancer (CRC) is the third most common malignancy worldwide and the second leading cause of cancer-related mortality in the United States. The incidence of early-onset colorectal cancer (EOCRC) has been increasing over the past several decades. While the etiologies for this rising incidence remain unclear, genetic factors likely play an important role. DNA polymerase epsilon (POLE) mutations occur at a higher rate than average-onset colorectal cancer (AOCRC). DNA polymerase epsilon (Pol ε) is a high-fidelity, processive polymerase that is a promising target for immune checkpoint inhibitors due to its association with various human malignancies, including colorectal cancer. EOCRC remains a major area of focus, and POLE mutations leading to the high-TMB subtype constitute a potential therapeutic target.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Artificial Reproductive Technology Use and Family-Building Experiences of Female Adult Childhood Cancer Survivors: A Qualitative Study
by
Selena Banser, A. Fuchsia Howard, Sally Thorne and Karen J. Goddard
Curr. Oncol. 2025, 32(7), 369; https://doi.org/10.3390/curroncol32070369 - 25 Jun 2025
Abstract
Purpose: Cancer treatments can result in subfertility or infertility in female adult childhood cancer survivors (ACCSs). While ACCSs may utilize assisted reproductive technology (ART) or other family-building options, the limited evidence describing their experiences remains a hindrance to developing and implementing appropriate patient-centered
[...] Read more.
Purpose: Cancer treatments can result in subfertility or infertility in female adult childhood cancer survivors (ACCSs). While ACCSs may utilize assisted reproductive technology (ART) or other family-building options, the limited evidence describing their experiences remains a hindrance to developing and implementing appropriate patient-centered supports. The study’s aim is to describe the challenges female ACCSs experienced while navigating ART and family-building options, to inform improvements in clinical practice in a western Canadian province. Methods: In this qualitative Interpretive Description study, interviews were conducted with 15 female ACCSs and data were analyzed using an interpretive thematic approach and constant comparative techniques. Results: ACCSs’ narratives suggest they experienced five prominent challenges while navigating ART and family-building options, including (1) confronting unexpected, impaired fertility, (2) grieving loss and redefining identity, (3) encountering unsupportive healthcare, (4) exploring alternative paths of adoption and international family-building, and (5) facing financial strain. Conclusions: This exploratory study provides initial insights into the significant and multifaceted challenges female ACCSs experience related to family building and highlights gaps in healthcare services. Further research is warranted to articulate these challenges across contexts and the development and implementation of mitigating approaches. Implications for Cancer Survivors: The integration of comprehensive informational, psychosocial, and financial supports into existing cancer survivor and family-building services is vital to meeting female ACCSs’ unmet needs.
Full article
(This article belongs to the Special Issue Quality of Life and Management of Pediatric Cancer)
Open AccessArticle
Evaluating the Feasibility and Acceptability of a Community-Based, Co-Created Yoga Program for Women with Gynecologic Cancer: A Series N-of-1 Feasibility Study
by
Jenson Price, Brooklyn Westlake and Jennifer Brunet
Curr. Oncol. 2025, 32(7), 368; https://doi.org/10.3390/curroncol32070368 - 24 Jun 2025
Abstract
Purpose: Current yoga programs for cancer survivors do not meet participants’ needs and are rarely implemented in community-based settings, despite reported benefits. The aim of the current study was to implement a co-created 12-week bi-modal Hatha-based yoga program for adults diagnosed with gynecologic
[...] Read more.
Purpose: Current yoga programs for cancer survivors do not meet participants’ needs and are rarely implemented in community-based settings, despite reported benefits. The aim of the current study was to implement a co-created 12-week bi-modal Hatha-based yoga program for adults diagnosed with gynecologic cancer in the community and assess the feasibility and acceptability of the program and study methods. Methods: Using a mixed methods series N-of-1 A1BA2 research design, participants were recruited from The Ottawa Hospital. Participants self-selected a morning or evening program, completed surveys 9 to 11 times and were interviewed post-program. The yoga instructor was interviewed post-program about her experience delivering the program. Quantitative feasibility outcomes were tracked throughout the study. Qualitative acceptability outcomes were explored during post-program semi-structured interviews. Audio and video recordings of the yoga classes and data from the instructor interview were used to assess fidelity outcomes to determine whether the protocol could be adhered to consistently. Results: Forty-one individuals were screened for eligibility and 20 consented (48.7%). Seventeen participants (85.0%) completed the final survey. Participants attended 83.1% (19.9/24) of classes with varied engagement with optional features. The instructor was 61.3% adherent to the prescribed protocol, using recommended behaviors 44.6% of the time. Participants shared barriers and facilitators that influenced the success of the trial methods and program. Conclusions: The program was well-received and trial methods were moderately successful, but refinements are warranted before a large-scale trial. Community-based yoga programs could be feasible and acceptable for women with gynecologic cancer.
Full article
(This article belongs to the Section Psychosocial Oncology)
►▼
Show Figures
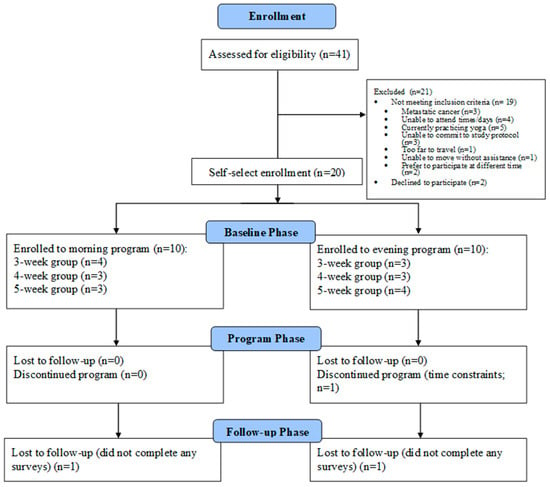
Figure 1
Open AccessReview
Targeting DNA Damage Response-Mediated Resistance in Non-Small Cell Lung Cancer: From Mechanistic Insights to Drug Development
by
Xue Gong, Yongzhao Zhou and Yi Deng
Curr. Oncol. 2025, 32(7), 367; https://doi.org/10.3390/curroncol32070367 - 23 Jun 2025
Abstract
Non-small cell lung cancer (NSCLC) remains a major contributor to cancer-related deaths worldwide, with therapeutic resistance presenting a critical clinical hurdle. The DNA damage response (DDR) constitutes a sophisticated cellular framework that detects, signals, and repairs genetic lesions to preserve genomic stability. While
[...] Read more.
Non-small cell lung cancer (NSCLC) remains a major contributor to cancer-related deaths worldwide, with therapeutic resistance presenting a critical clinical hurdle. The DNA damage response (DDR) constitutes a sophisticated cellular framework that detects, signals, and repairs genetic lesions to preserve genomic stability. While the DDR plays a crucial role in determining the efficacy of radiotherapy and chemotherapy, current research primarily focuses on direct DDR inhibitors, often overlooking the broader regulatory networks that modulate DDR activity. This review aims to comprehensively analyze the upstream and downstream pathways governing DDR in NSCLC, highlighting key molecular regulators, signaling interactions, and potential feedback mechanisms contributing to therapy resistance. By identifying novel regulatory targets and clinically relevant biomarkers, we propose innovative therapeutic strategies to enhance treatment efficacy. Our approach seeks to bridge the gap between DDR dysregulation and precision oncology, offering new perspectives on overcoming resistance and improving patient outcomes in NSCLC.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures
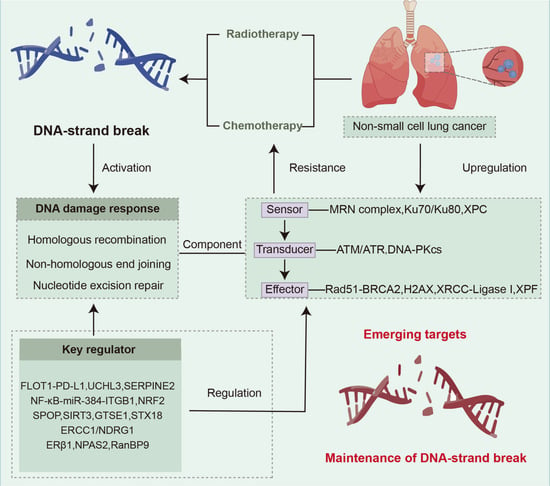
Graphical abstract
Open AccessCase Report
A Neuropsychiatric Prelude to Unveiling Small Cell Lung Cancer with Suspected Paraneoplastic Limbic Encephalitis: A Case Report
by
Jessa Letargo, X. Melody Qu, Timothy K. Nguyen, Alexander V. Louie, Sara Kuruvilla and Enxhi Kotrri
Curr. Oncol. 2025, 32(6), 366; https://doi.org/10.3390/curroncol32060366 - 19 Jun 2025
Abstract
Small cell lung cancer (SCLC) is an aggressive form of lung cancer characterized by rapid growth and early metastases. As a neuroendocrine tumour, SCLC is especially notorious for various paraneoplastic syndromes, one of which is a rare neurological syndrome called paraneoplastic limbic encephalitis
[...] Read more.
Small cell lung cancer (SCLC) is an aggressive form of lung cancer characterized by rapid growth and early metastases. As a neuroendocrine tumour, SCLC is especially notorious for various paraneoplastic syndromes, one of which is a rare neurological syndrome called paraneoplastic limbic encephalitis (PLE) that manifests with amnestic cognitive impairment and seizures. Here, we describe a case of a 53-year-old female who presented with neuropsychiatric symptoms of delusions, hallucinations, and cognitive impairment that started months prior to being diagnosed with extensive-stage SCLC. With no previous neuropsychiatric history, this raised the question of whether her presentation was related to PLE rather than a primary psychiatric condition, as initially diagnosed. Her symptoms improved with chemotherapy and radiation treatment of the underlying cancer, favouring a paraneoplastic etiology. Overall, this case underscores the importance of considering paraneoplastic syndromes in patients presenting with new neuropsychiatric symptoms, as early recognition and treatment can improve prognosis.
Full article
(This article belongs to the Special Issue Clinical Advances and Therapeutic Challenges in Small-Cell Lung Cancer and Rare Thoracic Cancers)
►▼
Show Figures

Figure 1
Open AccessSystematic Review
KRAS Mutations as Predictive Biomarkers for First-Line Immune Checkpoint Inhibitor Monotherapy in Advanced NSCLC: A Systematic Review and Meta-Analysis
by
Filip Marković, Jelena Milin-Lazović, Nikola Nikolić, Aleksa Golubović, Mihailo Stjepanović and Milica Kontić
Curr. Oncol. 2025, 32(6), 365; https://doi.org/10.3390/curroncol32060365 - 19 Jun 2025
Abstract
Recent research suggests a link between KRAS mutations and the effectiveness of ICIs, as KRAS-driven tumors may possess unique immunogenic features that influence the tumor microenvironment. These mutations can increase tumor mutation burden (TMB) and neoantigen load, potentially leading to improved responses to
[...] Read more.
Recent research suggests a link between KRAS mutations and the effectiveness of ICIs, as KRAS-driven tumors may possess unique immunogenic features that influence the tumor microenvironment. These mutations can increase tumor mutation burden (TMB) and neoantigen load, potentially leading to improved responses to ICIs. This meta-analysis aims to consolidate existing evidence on the impact of KRAS mutations as a predictive factor for survival and treatment outcomes in patients with advanced NSCLC treated with ICIs. A comprehensive search strategy was designed by a biostatistician and pulmonologist, targeting PubMed, Web of Science, and Scopus databases up to May 2022. The outcomes assessed included overall survival (OS) and progression-free survival (PFS), reported as log hazard ratios (HRs) with corresponding standard errors (SEs). A pooled estimate of the HR effect size was calculated using Review Manager (RevMan, Cochrane Collaboration, London, UK). Heterogeneity among studies was evaluated using the Cochran Q test and the I2 statistic. Ultimately, 10 articles were deemed suitable for inclusion in the systematic review from a total of 8722 screened titles and abstracts. The presence of KRAS+ mutations had a significant prognostic factor for better OS in NSCLC patients treated with checkpoint inhibitors (HR = 0.89, 95% CI: 0.79–0.99) and for better PFS in NSCLC patients treated with checkpoint inhibitors (HR = 0.72, 95% CI: 0.59–0.87). In conclusion, our study indicates that KRAS mutations may serve as a potential positive predictive biomarker in patients with advanced non-small-cell lung cancer treated with immune checkpoint inhibitor monotherapy.
Full article
(This article belongs to the Section Thoracic Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Textbook Outcomes for Retroperitoneal Sarcoma Resection: A Multi-Centre Review
by
Skyle Murphy, Christopher Allan, Andrew Barbour, Victoria Donoghue and B. Mark Smithers
Curr. Oncol. 2025, 32(6), 364; https://doi.org/10.3390/curroncol32060364 - 19 Jun 2025
Abstract
For patients with retroperitoneal sarcomas (RPSs), en-bloc resection with macroscopically negative margins remains the only potentially curative treatment. Textbook outcomes (TOs) are composite measures developed to compare ideal surgical outcomes for complex oncologic resections. The aims of this study were as follows: to
[...] Read more.
For patients with retroperitoneal sarcomas (RPSs), en-bloc resection with macroscopically negative margins remains the only potentially curative treatment. Textbook outcomes (TOs) are composite measures developed to compare ideal surgical outcomes for complex oncologic resections. The aims of this study were as follows: to define TO for RPS resections; to investigate the impact of treating service and other variables on TO; and to investigate the impact of treating service on achieving a TO. Population-based data from the Queensland Oncology Repository (QOR) was used to perform a retrospective review of all adult patients who underwent resection for primary RPS in Queensland between 2012 and 2022. TO was defined as follows: en-bloc resection; macroscopically negative margins; no unplanned ICU admission, no Clavien–Dindo III or greater complications; hospital length of stay of 14 days or less; no readmission within 30 days; and no 90-day mortality. A TO was achieved in 82 (56.94%) of the 144 patients included in the study. A high-grade histological subtype, the resection of three or more contiguous organs, major vascular resection and treatment outside of a high-volume sarcoma centre (HVSC) were significant negative predictors of achieving TOs (p < 0.05). On multivariate analysis, treatment at a high-volume sarcoma centre was independently associated with a 2.6-fold increase in TO (1.18–5.88, p = 0.02). Achieving a TO was associated with higher five-year DFS (61.5% vs. 41.3%, p = 0.03) and OS (76% vs. 59.4%, p = 0.02). In our state, TOs provide a measure of the quality of RPS resection across multiple health services, with patients treated at high-volume sarcoma centres more likely to achieve a TO. TO rates are associated with improved five-year DFS and OS.
Full article
(This article belongs to the Special Issue Sarcoma Surgeries: Oncological Outcomes and Prognostic Factors)
►▼
Show Figures

Figure 1
Open AccessArticle
Combined Predictive Value of GLIM-Defined Malnutrition and Preoperative Adipose Tissue 18F-FDG Uptake for Recurrence-Free Survival After Radical Gastrectomy in Patients with Gastric Cancer
by
Xuan Zhou, Kailai Yin, Huanhuan Hong, Heqing Yi and Linfa Li
Curr. Oncol. 2025, 32(6), 363; https://doi.org/10.3390/curroncol32060363 - 19 Jun 2025
Abstract
Background: The Global Leadership Initiative on Malnutrition (GLIM) criteria provide a standardized approach for assessing the nutritional status of patients and demonstrate strong predictive value for the prognosis of patients with gastric cancer. However, these criteria do not incorporate indicators of adipose tissue
[...] Read more.
Background: The Global Leadership Initiative on Malnutrition (GLIM) criteria provide a standardized approach for assessing the nutritional status of patients and demonstrate strong predictive value for the prognosis of patients with gastric cancer. However, these criteria do not incorporate indicators of adipose tissue metabolic activity, which may reflect pro-tumor microenvironmental factors. This study investigated the combined predictive value of malnutrition, defined by the GLIM criteria, and preoperative adipose tissue 18F-fluorodeoxyglucose (18F-FDG) uptake for recurrence-free survival (RFS) in patients with gastric cancer following radical surgery. Methods: A total of 105 patients were retrospectively enrolled and classified into malnourished and non-malnourished groups based on the GLIM criteria. Preoperative 18F-FDG positron emission tomography/computed tomography (18F-FDG PET/CT) was used to measure the mean standardized uptake value (SUVmean) of visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT). The predictive values of these indicators for RFS in patients with gastric cancer were assessed. Results: Multivariate survival analysis was used to identify GLIM-defined malnutrition (p = 0.020) and increased preoperative VAT SUVmean (p = 0.042) as independent risk factors for RFS. The combined analysis revealed that patients with both malnutrition and a high preoperative VAT SUVmean had the poorest RFS (HR = 18.41, p < 0.001). The predictive model integrating GLIM criteria and VAT SUVmean outperformed the GLIM criteria alone. Conclusions: This study demonstrated that combining malnutrition defined by the GLIM criteria with preoperative visceral adipose tissue 18F-FDG uptake optimizes recurrence risk stratification and exhibits superior prognostic predictive efficacy compared to using the GLIM criteria alone. This approach provides new insights into individualized prognostic assessment and intervention strategies.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
►▼
Show Figures

Figure 1
Open AccessReview
The Relationship Between Obesity and Cancer: Epidemiology, Pathophysiology, and the Effect of Obesity Treatment on Cancer
by
Yasmin Ingram, Oluwasegun Olujide, Nabiha Sheikh, Alice Robinson, Jan Hoong Ho, Akheel A. Syed and Safwaan Adam
Curr. Oncol. 2025, 32(6), 362; https://doi.org/10.3390/curroncol32060362 - 19 Jun 2025
Abstract
There is growing evidence relating to the risk of cancer in people with obesity. Obesity is already established as one of the strongest predisposing factors to cancer, and ‘obesity-related’ cancers have been defined in previous studies. In this review article, we examine the
[...] Read more.
There is growing evidence relating to the risk of cancer in people with obesity. Obesity is already established as one of the strongest predisposing factors to cancer, and ‘obesity-related’ cancers have been defined in previous studies. In this review article, we examine the epidemiological relationship and describe the potential pathophysiological mechanisms that underpin the association between obesity and cancer. These include hormonal and growth factors that are in abundance in persons living with obesity and thereby increase cancer risk. Additionally, the increased disposition towards chronic inflammation in obesity also confers cancer risk. We also examine the impact of obesity on cancer treatment outcomes, focusing on surgery, chemotherapy, and immunotherapy. Conversely, we underline the impact of weight loss on cancer risk by examining different weight loss strategies.
Full article
(This article belongs to the Special Issue Diet and Physical Activity Management during Cancer)
►▼
Show Figures

Figure 1
Open AccessArticle
SUPPORT MY WAY: Supporting Young People After Treatment for Cancer: What Is Needed, When This Is Needed and How This Can Be Best Delivered
by
Nicole Collaço, Charlotte Ralph, Peter Dawes, Anne-Sophie Darlington, Andrew Davies, Ramya Ramanujachar, Louise Hooker and Samantha Sodergren
Curr. Oncol. 2025, 32(6), 361; https://doi.org/10.3390/curroncol32060361 - 19 Jun 2025
Abstract
As survival rates for teenagers and young adults (TYAs) with cancer exceed 80%, they are living longer post treatment, yet often experience prolonged health and quality of life concerns. Many TYAs also experience unmet support needs. This study aimed to identify TYAs support
[...] Read more.
As survival rates for teenagers and young adults (TYAs) with cancer exceed 80%, they are living longer post treatment, yet often experience prolonged health and quality of life concerns. Many TYAs also experience unmet support needs. This study aimed to identify TYAs support needs following treatment at a UK hospital and explore how and when TYAs prefer to receive support. This study involved two phases: Phase 1 involved semi-structured interviews with 16 TYAs, 1–6 years post-treatment, aged 16–25 years at time of treatment completion and examined their experiences of support services, and preferences for future care. Phase 2 consisted of co-design workshops with eight TYAs and feedback from five healthcare/allied professionals (HCAPs) to refine and develop recommendations. Phase 1 findings revealed six key themes: (1) survivorship as disrupted continuity; (2) negotiating legitimacy and relational safety in help seeking; (3) support offered vs. support sought: pathways of referral and self-initiation; (4) emotional readiness as context dependent and non-linear; (5) support as an ecosystem, not a moment; and (6) personalised autonomy in support engagement. Phase 2 findings informed recommendations that emphasise the importance of flexible, personalised, and accessible post-treatment support, with pathways of care/support that can adapt to TYAs changing needs and preferences over time.
Full article
(This article belongs to the Special Issue Quality of Life and Follow-Up Care Among AYA Cancer Survivors)
►▼
Show Figures

Figure 1
Open AccessArticle
Dosimetric Comparison of VMAT Alone and VMAT with HDR Brachytherapy Boost Using Clinical and Biological Dose Models in Localized Prostate Cancer
by
Manuel Guhlich, Olga Knaus, Arne Strauss, Laura Anna Fischer, Jann Fischer, Stephanie Bendrich, Sandra Donath, Leif Hendrik Dröge, Martin Leu, Stefan Rieken, Annemarie Uhlig, Markus Anton Schirmer and Andrea Hille
Curr. Oncol. 2025, 32(6), 360; https://doi.org/10.3390/curroncol32060360 - 19 Jun 2025
Abstract
Background: Combining external beam radiotherapy (EBRT) with high-dose-rate (HDR) brachytherapy (BT) enables biologically effective dose escalation in prostate cancer. However, comparative evaluation of such regimens using radiobiological modeling remains limited. Methods: Dose regimens based on clinical practice were analyzed using α/β values of
[...] Read more.
Background: Combining external beam radiotherapy (EBRT) with high-dose-rate (HDR) brachytherapy (BT) enables biologically effective dose escalation in prostate cancer. However, comparative evaluation of such regimens using radiobiological modeling remains limited. Methods: Dose regimens based on clinical practice were analyzed using α/β values of 1.5 and 3 Gy for the prostate. Ten patients with available planning CT, pelvic MRI, and ultrasound-guided BT plans were retrospectively evaluated. Physical and biological dose distributions were recalculated for various EBRT and HDR-BT combinations. Biological effective dose (BED) values were determined for the prostate and organs at risk (OARs: anterior rectal wall, bladder base, urethra). Regimens yielding the highest ΔBED between prostate and OARs were considered most favorable. Results: All regimens met clinical dose constraints. The most favorable ΔBED profiles for bladder and rectum were observed with HDR-BT regimens (2 × 15 Gy) combined with either 23 × 2 Gy or 15 × 2.5 Gy EBRT, independent of the assumed α/β value. EBRT-only regimens achieved superior urethral sparing, while higher HDR doses led to increased urethral exposure. Conclusions: This study underscores the value of radiobiological modeling in differentiating and optimizing prostate cancer radiotherapy strategies. While the trade-offs between dose escalation and OAR sparing are clinically known, our biologically driven analysis provides a more quantitative foundation for selecting and tailoring combined EBRT/HDR-BT regimens in practice.
Full article
(This article belongs to the Special Issue Radiotherapy for Genitourinary Cancer)
►▼
Show Figures

Figure 1
Open AccessReview
Molecular Genetics of Renal Cell Carcinoma: A Narrative Review Focused on Clinical Relevance
by
Braden Millan, Lauren Loebach, Ruben Blachman-Braun, Milan H. Patel, Jaskirat Saini, W. Marston Linehan and Mark W. Ball
Curr. Oncol. 2025, 32(6), 359; https://doi.org/10.3390/curroncol32060359 - 18 Jun 2025
Abstract
Molecular testing in renal cell carcinoma (RCC) has allowed for a better understanding of the biology of both sporadic and hereditary diseases, where genetic testing is currently recommended in the guidelines for a select population with risk factors. Historically, screening, surveillance, and management
[...] Read more.
Molecular testing in renal cell carcinoma (RCC) has allowed for a better understanding of the biology of both sporadic and hereditary diseases, where genetic testing is currently recommended in the guidelines for a select population with risk factors. Historically, screening, surveillance, and management decisions were based solely on clinicopathologic data; however, we now know that molecular profiling can enhance decision making, altering the treatment plan, approach, or selection of systemic therapy and enhancing the delivery of precision oncologic care. Advances and the increasing availability of next-generation sequencing technologies have improved the identification of germline and somatic variants in key RCC-associated genes. Given the molecular heterogeneity of RCC, these modern methods can identify unique genetic events that occur in a single individual, allowing for distinction between a metachronous tumor from metastases. Separate four-tier systems have been proposed to categorize germline and somatic variants according to their clinical significance, which should be highlighted. Additionally, emerging technologies, such as liquid biopsy, show potential for enhancing precision oncology in RCC. With this said, challenges, such as variant interpretation, ethical considerations, and accessibility, persist. This review examines the molecularly defined RCC, genetic testing methodologies currently available, their current clinical applications, limitations, and future directions.
Full article
(This article belongs to the Section Genitourinary Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Comparison of Mortality and Morbidity of Robotic Versus Laparoscopic Radical Nephrectomy for the Treatment of Renal Cell Carcinoma—An Analysis of the National Surgery Quality Improvement Program (NSQIP) Targeted Nephrectomy Database
by
Vatsala Mundra, Siqi Hu, Renil Sinu Titus, Eusebio Luna-Velazquez, Zachary Melchiode, Jiaqiong Xu, Carlos Riveros, Sanjana Ranganathan, Emily Huang, Brian J. Miles, Dharam Kaushik, Christopher J. D. Wallis and Raj Satkunasivam
Curr. Oncol. 2025, 32(6), 358; https://doi.org/10.3390/curroncol32060358 - 17 Jun 2025
Abstract
Objectives: To compare the perioperative complications between robot-assisted (RARN) and laparoscopic (LRN) radical nephrectomy for the treatment of renal cell carcinoma (RCC). Methods: We conducted a retrospective study using the National Surgical Quality Improvement Program (NSQIP) Nephrectomy-Targeted database from 2019 to 2021. After
[...] Read more.
Objectives: To compare the perioperative complications between robot-assisted (RARN) and laparoscopic (LRN) radical nephrectomy for the treatment of renal cell carcinoma (RCC). Methods: We conducted a retrospective study using the National Surgical Quality Improvement Program (NSQIP) Nephrectomy-Targeted database from 2019 to 2021. After using propensity score matching, we assessed the association between LRN vs. RARN and the outcomes of interest (primary outcomes of 30-day mortality, return to the operating room, myocardial infarction, and stroke; and secondary outcomes of perioperative complications and nephrectomy-specific outcomes). Results: Among the 1545 patients in the study (mean age: 62.9 ± 11.8 years), 722 underwent RARN and 823 underwent LRN. We did not observe any differences in the major complications between the two approaches. However, LRN was associated with an increased chance of surgical site infections compared with RARN (LRN 2.68% vs. RARN 1.19%, p = 0.047). LRN was also associated with a higher likelihood of a prolonged length of stay (OR 1.54, 95% CI: 1.15, 2.06, p = 0.004) and had a 2.7 times higher chance of conversion rate to open surgery (OR 3.70, 95% CI: 3.25, 4.15, p < 0.001) relative to RARN. However, RARN was associated with a longer operative time than LRN (estimated coefficient 30.67, p < 0.001). Conclusion: We found no significant difference in the major complications between RARN and LRN for patients undergoing radical nephrectomy. At the expense of a somewhat longer operative time, RARN was associated with a lower risk of SSI and a lower conversion rate to open RN. LRN and RARN should both be considered and selected on an individualized basis using tumor, patient, and physician factors.
Full article
(This article belongs to the Section Genitourinary Oncology)
►▼
Show Figures

Figure 1
Open AccessGuidelines
Postmastectomy Breast Reconstruction in Patients with Non-Metastatic Breast Cancer: An Ontario Health (Cancer Care Ontario) Clinical Practice Guideline
by
Toni Zhong, Glenn G. Fletcher, Muriel Brackstone, Simon G. Frank, Renee Hanrahan, Vivian Miragias, Christiaan Stevens, Danny Vesprini, Alyssa Vito and Frances C. Wright
Curr. Oncol. 2025, 32(6), 357; https://doi.org/10.3390/curroncol32060357 - 17 Jun 2025
Abstract
Several postmastectomy breast reconstruction techniques and procedures have been implemented, although with limited evaluation of benefits and adverse effects. We conducted a systematic review on the plane and timing of reconstruction, and on the use of nipple-sparing mastectomy, acellular dermal matrix, and autologous
[...] Read more.
Several postmastectomy breast reconstruction techniques and procedures have been implemented, although with limited evaluation of benefits and adverse effects. We conducted a systematic review on the plane and timing of reconstruction, and on the use of nipple-sparing mastectomy, acellular dermal matrix, and autologous fat grafting as the evidence base for an updated clinical practice guideline on breast reconstruction for Ontario Health (Cancer Care Ontario). Both immediate and delayed reconstruction may be considered, with preferred timing depending on factors such as patient preferences, type of mastectomy, skin perfusion, comorbidities, pre-mastectomy breast size, and desired reconstructive breast size. Immediate reconstruction may provide greater psychological or quality of life benefits. In patients who are candidates for skin-sparing mastectomy and without clinical, radiological, and pathological indications of nipple-areolar complex involvement, nipple-sparing mastectomy is recommended provided it is technically feasible and acceptable aesthetic results can be achieved. Surgical factors including incision location are important to reduce necrosis by preserving blood supply and to minimize nerve damage. There is a role for both prepectoral and subpectoral implants; risks and benefits will vary, and decisions should be made during consultation between the patient and surgeons. In patients who are suitable candidates for implant reconstruction and have adequate mastectomy flap thickness and vascularity, prepectoral implants should be considered. Acellular dermal matrix (ADM) has led to an increased use of prepectoral reconstruction. ADM should not be used in case of poor mastectomy flap perfusion/ischemia that would otherwise be considered unsuitable for prepectoral reconstruction. Care should be taken in the selection and handling of acellular dermal matrix (ADM) to minimize risks of infection and seroma. Limited data from small studies suggest that prepectoral reconstruction without ADM may be feasible in some patients. Autologous fat grafting is recommended as a treatment for contour irregularities, rippling following implant-based reconstruction, and to improve tissue quality of the mastectomy flap after radiotherapy.
Full article
(This article belongs to the Section Breast Cancer)
Open AccessArticle
Prognostic Value of Multiple Manual Segmentation Methods for Diffuse Large B-Cell Lymphoma with 18F-FDG PET/CT
by
Andrej Doma, Andrej Studen and Barbara Jezeršek Novaković
Curr. Oncol. 2025, 32(6), 356; https://doi.org/10.3390/curroncol32060356 - 16 Jun 2025
Abstract
Quantitative 18F-FDG PET/CT-derived metabolic metrics are strongly associated with patient outcomes in diffuse large B-cell lymphoma (DLBCL), but the lack of consensus on optimal segmentation thresholds limits standardization. This study evaluated the prognostic value of various metabolic tumor volume (MTV) segmentation approaches
[...] Read more.
Quantitative 18F-FDG PET/CT-derived metabolic metrics are strongly associated with patient outcomes in diffuse large B-cell lymphoma (DLBCL), but the lack of consensus on optimal segmentation thresholds limits standardization. This study evaluated the prognostic value of various metabolic tumor volume (MTV) segmentation approaches in 140 stage II–IV DLBCL patients treated with standard immunochemotherapy. MTV was derived using fixed SUV (≥2.5, ≥4.0), relative (>41% SUVmax), and adaptive (liver-to-background) thresholds. Baseline MTV metrics significantly correlated with 3-year overall survival (OS3) in univariate analysis in overall cohort, with MTV41 showing the strongest association (HR: 1.27; p = 0.003). MTV25 and MTV41 remained significant in the stage 4 patient subgroup. However, in multivariate analysis, no MTV metric independently predicted OS3 when adjusted for the International Prognostic Index (IPI), which remained the dominant predictor (HR: 1.95; p < 0.0001). ROC analysis confirmed superior AUC for IPI (0.76) over PET-based metrics (0.64–0.69). Predictive models integrating IPI with PET metrics were robust but failed to improve prognostic accuracy beyond IPI alone. Although PET-derived MTV metrics provide prognostic value in univariate analysis, threshold selection has minimal impact, and their added value is limited when combined with IPI, reinforcing its role as the most reliable survival predictor in DLBCL.
Full article
(This article belongs to the Special Issue Application of Nuclear Medicine in Cancer Diagnosis and Treatment)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- Current Oncology Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal Browser-
arrow_forward_ios
Forthcoming issue
arrow_forward_ios Current issue - Volumes not published by MDPI
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomolecules, CIMB, Sci. Pharm., Cancers, Current Oncology, Cells
The Role of Extracellular Vesicles as Modulators of the Tumor Microenvironment
Topic Editors: Nils Ludwig, Miroslaw J SzczepanskiDeadline: 30 June 2025
Topic in
Cancers, Diagnostics, JCM, Current Oncology, Gastrointestinal Disorders, Biomedicines, Therapeutics
Hepatobiliary and Pancreatic Diseases: Novel Strategies of Diagnosis and Treatments
Topic Editors: Alessandro Coppola, Damiano Caputo, Roberta Angelico, Domenech Asbun, Chiara MazzarelliDeadline: 20 August 2025
Topic in
Cancers, Current Oncology, JCM, Medicina, Onco
Cancer Biology and Radiation Therapy: 2nd Edition
Topic Editors: Chang Ming Charlie Ma, Ka Yu Tse, Ming-Yii Huang, Mukund SeshadriDeadline: 16 October 2025
Topic in
Biomedicines, Cancers, Current Oncology, Diagnostics, JCM
Advances in Magnetic Resonance Imaging (MRI) and Its Role in Radiation Therapy
Topic Editors: Indra J. Das, Minsong CaoDeadline: 31 October 2025

Conferences
Special Issues
Special Issue in
Current Oncology
Surgery in Locally Advanced and Metastatic Renal Cell Carcinoma
Guest Editor: Shawn DasonDeadline: 30 June 2025
Special Issue in
Current Oncology
Updates on Diagnosis and Treatment for Pediatric Solid Tumors
Guest Editor: Nur P. DamayantiDeadline: 30 June 2025
Special Issue in
Current Oncology
Imaging-Based Early Diagnosis of Cancers Using Artificial Intelligence
Guest Editors: Timm Denecke, Anselm SchulzDeadline: 30 June 2025
Special Issue in
Current Oncology
2nd Edition: Treatment of Bone Metastasis
Guest Editor: Costantino ErraniDeadline: 15 July 2025
Topical Collections
Topical Collection in
Current Oncology
New Insights into Prostate Cancer Diagnosis and Treatment
Collection Editor: Sazan Rasul
Topical Collection in
Current Oncology
New Insights into Breast Cancer Diagnosis and Treatment
Collection Editors: Filippo Pesapane, Matteo Suter
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series in "Exercise and Cancer Management"
Collection Editors: Linda Denehy, Ravi Mehrotra, Nicole Culos-Reed
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series: Contemporary Perioperative Concepts in Cancer Surgery
Collection Editors: Vijaya Gottumukkala, Jörg Kleeff











