Journal Description
Current Oncology
Current Oncology
is an international, peer-reviewed, open access journal published online by MDPI (from Volume 28 Issue 1-2021). Established in 1994, the journal represents a multidisciplinary medium for clinical oncologists to report and review progress in the management of this disease. The Canadian Association of Medical Oncologists (CAMO), the Canadian Association of Psychosocial Oncology (CAPO), the Canadian Association of General Practitioners in Oncology (CAGPO), the Cell Therapy Transplant Canada (CTTC), the Canadian Leukemia Study Group (CLSG) and others are affiliated with the journal and their members receive a discount on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, Embase, and other databases.
- Journal Rank: JCR - Q2 (Oncology)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.5 days after submission; acceptance to publication is undertaken in 2.5 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Clusters of Oncology: Cancers, Current Oncology, Onco and Targets.
Impact Factor:
3.4 (2024);
5-Year Impact Factor:
3.3 (2024)
Latest Articles
Systematic Literature Review on Economic Evaluations and Health Economic Models in Metastatic Castration-Sensitive Prostate Cancer
Curr. Oncol. 2025, 32(8), 412; https://doi.org/10.3390/curroncol32080412 - 22 Jul 2025
Abstract
At diagnosis, metastatic prostate cancer (PC) is sensitive to androgen deprivation therapy (ADT), and patients are usually referred to as having castration-sensitive prostate cancer (mCSPC). The combination of ADT and androgen receptor pathway inhibitors (ARPI) is the current standard of care for mCSPC.
[...] Read more.
At diagnosis, metastatic prostate cancer (PC) is sensitive to androgen deprivation therapy (ADT), and patients are usually referred to as having castration-sensitive prostate cancer (mCSPC). The combination of ADT and androgen receptor pathway inhibitors (ARPI) is the current standard of care for mCSPC. This study aimed to review the literature on economic evaluations and health economic models related to mCSPC. A literature search was performed covering Medline, Embase, and Scopus with additional grey literature sources. Studies with data on health economic evaluations focusing on Europe or North America were relevant. 18 peer-reviewed articles and 10 grey literature documents were included. The majority (n = 23) had a deterministic Markov structure and applied either Markov cohort or partitioned survival models. Evaluations investigated various types of ADT-based combinations, comparing the addition of ARPI, chemotherapy agents, or radiation therapy to ADT alone. We concluded that economic evaluations in the field of PC are widely published, and there are a large number of publications even in the specific subgroup of mCSPC. Regardless of the investigated interventions, most studies applied similar methodologies and simulated patients from the mCSPC state until the development of mCRPC or death.
Full article
(This article belongs to the Section Health Economics)
►
Show Figures
Open AccessCase Report
Novel Surgical Reconstruction Using a 3D Printed Cement Mold Following Resection of a Rare Case of Proximal Ulna Osteosarcoma: A Case Report and Description of the Surgical Technique
by
Abdulrahman Alaseem, Hisham A. Alsanawi, Waleed Albishi, Ibrahim Alshaygy, Sara Alhomaidhi, Mohammad K. Almashouq, Abdulaziz M. AlSudairi, Yazeed A. Alsehibani and Abdulaziz O. Almuhanna
Curr. Oncol. 2025, 32(8), 411; https://doi.org/10.3390/curroncol32080411 - 22 Jul 2025
Abstract
Osteosarcoma is one of the most common primary bone malignancies, typically occurring around the knee. However, the forearm is a rare site, with tumors in the proximal ulna being extremely uncommon. Primary sarcoma in this location presents a surgical challenge due to the
[...] Read more.
Osteosarcoma is one of the most common primary bone malignancies, typically occurring around the knee. However, the forearm is a rare site, with tumors in the proximal ulna being extremely uncommon. Primary sarcoma in this location presents a surgical challenge due to the complex anatomy and limited reconstructive options. We report a rare case of a 19-year-old female with non-metastatic, high-grade giant cell-rich osteosarcoma involving the right proximal ulna. To our knowledge, this is only the second reported adult case of this histological subtype in this location. The patient was treated at a specialized oncology center with neoadjuvant and adjuvant chemotherapy, along with wide intra-articular resection for local tumor control. Reconstruction was achieved using a novel, customized 3D-printed articulating cement spacer mold with plate osteosynthesis. Artificial elbow ligamentous reconstruction was performed using FiberTape and FiberWire sutures passed through drill holes, and the triceps tendon was reattached to the cement mold using an endobutton. This cost-effective and personalized surgical approach allowed successful joint reconstruction while maintaining elbow stability and function. Our case highlights a feasible reconstructive option for rare and anatomically challenging osteosarcoma presentations, contributing to the limited literature on proximal ulna giant cell-rich osteosarcoma.
Full article
(This article belongs to the Section Bone and Soft Tissue Oncology)
Open AccessReview
Old Tools in a New Era: The Continued Relevance of Chemotherapy in Pediatric Neuro-Oncology
by
Kathleen Felton, Lucie Lafay-Cousin and Sylvia Cheng
Curr. Oncol. 2025, 32(7), 410; https://doi.org/10.3390/curroncol32070410 - 20 Jul 2025
Abstract
Conventional chemotherapy continues to form the backbone of treatment for many pediatric central nervous system (CNS) tumors. Advances have been made especially in the molecular underpinning of certain pediatric CNS tumors, allowing for advancement and consideration in incorporating this molecular information in molecular
[...] Read more.
Conventional chemotherapy continues to form the backbone of treatment for many pediatric central nervous system (CNS) tumors. Advances have been made especially in the molecular underpinning of certain pediatric CNS tumors, allowing for advancement and consideration in incorporating this molecular information in molecular targeted therapy or appropriate de-escalation or escalation of therapy. In very young children with embryonal CNS tumors, intensive high-dose chemotherapy approaches have been used with varied increased survival in medulloblastoma, atypical teratoid rhabdoid tumor (ATRT), and rare embryonal subtypes, but there are certain molecular risk groups that require new therapies, such as the ATRT MYC subtype. Some CNS tumors remain resistant or refractory to conventional chemotherapy, especially in relapsed disease. Strategies to explore combination therapies with chemotherapy, novel agents, and novel approaches are needed to improve survival in this population in the future.
Full article
(This article belongs to the Special Issue Clinical Outcomes and New Treatments in Pediatric Brain Tumors)
Open AccessArticle
Unique Biological Characteristics of Patients with High Gleason Score and Localized/Locally Advanced Prostate Cancer Using an In Silico Translational Approach
by
Shiori Miyachi, Masanori Oshi, Takeshi Sasaki, Itaru Endo, Kazuhide Makiyama and Takahiro Inoue
Curr. Oncol. 2025, 32(7), 409; https://doi.org/10.3390/curroncol32070409 - 18 Jul 2025
Abstract
Gleason score (GS) is one of the best predictors of prostate cancer (PCa) aggressiveness; however, its biological features need to be elucidated. This study aimed to explore the biological characteristics of localized/locally advanced PCa stratified using in silico GS analysis. Biological features were
[...] Read more.
Gleason score (GS) is one of the best predictors of prostate cancer (PCa) aggressiveness; however, its biological features need to be elucidated. This study aimed to explore the biological characteristics of localized/locally advanced PCa stratified using in silico GS analysis. Biological features were analyzed using gene set variation analysis and the xCell algorithm with mRNA expression in two independent public databases: The Cancer Genome Atlas (TCGA) (n = 493; radical prostatectomy cohort) and GSE116918 (n = 248; radiation therapy cohort). GS levels were positively correlated with the activity levels of cell proliferation-related gene sets, including E2F targets, the G2M checkpoint, the mitotic spindle, and MYC targets v1 and v2 in both cohorts. Furthermore, GS levels were positively associated with the activity levels of immune-related gene sets and infiltrating fractions of immune cells, including CD4+ memory T cells, dendritic cells, M1 macrophages, and Th2 cells, in both cohorts. Notably, GS levels were positively associated with the score levels of homologous recombination defects, intratumor heterogeneity, fraction genome alteration, neoantigens, and mutation rates in the TCGA cohort. In conclusion, PCa with high GS levels was associated with cancer cell proliferation, immune cell infiltration, and high mutation rates, which may reflect worse clinical outcomes.
Full article
(This article belongs to the Section Genitourinary Oncology)
►▼
Show Figures

Figure 1
Open AccessReview
Surgical Management of Desmoid Tumors—Patient Selection, Timing, and Approach
by
Catherine Sarre Lazcano and Alessandro Gronchi
Curr. Oncol. 2025, 32(7), 408; https://doi.org/10.3390/curroncol32070408 - 18 Jul 2025
Abstract
Desmoid tumors are rare, deep-seated myofibroblastic tumors with an unpredictable course, ranging from spontaneous regression to infiltrative growth and locally aggressive behavior, but without metastatic potential. Over the past few decades, advances in understanding their natural history, underlying molecular pathways, and patient care
[...] Read more.
Desmoid tumors are rare, deep-seated myofibroblastic tumors with an unpredictable course, ranging from spontaneous regression to infiltrative growth and locally aggressive behavior, but without metastatic potential. Over the past few decades, advances in understanding their natural history, underlying molecular pathways, and patient care priorities have shifted the treatment paradigm from upfront surgical resection to initial active surveillance, with further treatment dictated by continuous disease progression or associated symptoms. However, there are still specific scenarios where surgery continues to play an important role in locoregional treatment and symptom control. This article will focus on current treatment strategies and surgical indications in adult patients with desmoid tumors, emphasizing patient selection, anatomic site-specific considerations, and surgical technique. Understanding the nuanced role of surgery within the growing treatment landscape is key for individualized patient care in a multidisciplinary setting to optimize quality of life and long-term outcomes.
Full article
(This article belongs to the Special Issue An In-Depth Review of Desmoid Tumours)
►▼
Show Figures

Figure 1
Open AccessReview
Cervical Cancer Screening Cascade: A Framework for Monitoring Uptake and Retention Along the Screening and Treatment Pathway
by
Sara Izadi-Najafabadi, Laurie W. Smith, Anna Gottschlich, Amy Booth, Stuart Peacock and Gina S. Ogilvie
Curr. Oncol. 2025, 32(7), 407; https://doi.org/10.3390/curroncol32070407 - 17 Jul 2025
Abstract
Background: Cervical cancer is a major global health concern, causing approximately 350,000 deaths annually. It is also preventable through effective prevention and early detection. To facilitate elimination, the World Health Organization (WHO) set targets for HPV vaccination, screening, and treatment. Achieving these goals
[...] Read more.
Background: Cervical cancer is a major global health concern, causing approximately 350,000 deaths annually. It is also preventable through effective prevention and early detection. To facilitate elimination, the World Health Organization (WHO) set targets for HPV vaccination, screening, and treatment. Achieving these goals requires frameworks to monitor screening program performance. As many regions transition to HPV primary screening, a standardized Cervical Cancer Screening Cascade can track performance, identify gaps in follow-up, and optimize resource allocation. Methods: This paper introduces a structured cascade developed to monitor uptake, retention, and outcomes in HPV-based screening programs. The Cascade was created through collaboration between public health experts, clinicians, and researchers at the University of British Columbia (UBC), the Women’s Health Research Institute, and BC Cancer. Results: The Cascade outlines four phases: screening, triage, detection, and treatment. Each phase includes two substages: “uptake” and “results,” with an additional substage in screening (“invitation”). “Screening” assesses invitation effectiveness and participation. “Triage” tracks follow-up after a positive screen. “Detection” evaluates attendance at diagnostic appointments, and “Treatment” measures the treatment rate for those with precancerous lesions. Conclusions: The Cascade can guide emerging and existing HPV screening programs within Canada and other similarly resourced settings and serve as a benchmark tool for programs to assess their progress towards cervical cancer elimination.
Full article
(This article belongs to the Section Gynecologic Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Collecting Data on the Social Determinants of Health to Advance Health Equity in Cancer Care in Canada: Patient and Community Perspectives
by
Jacqueline L. Bender, Eryn Tong, Ekaterina An, Zhihui Amy Liu, Gilla K. Shapiro, Jonathan Avery, Alanna Chu, Christian Schulz-Quach, Sarah Hales, Alies Maybee, Ambreen Sayani, Andrew Pinto and Aisha Lofters
Curr. Oncol. 2025, 32(7), 406; https://doi.org/10.3390/curroncol32070406 - 16 Jul 2025
Abstract
Despite advances in cancer care, disparities persist. The collection of the social determinants of health (SDOH) is fundamental to addressing disparities. However, SDOH are inconsistently collected in many regions of the world. This two-phase multiple methods study examined patient and community perspectives regarding
[...] Read more.
Despite advances in cancer care, disparities persist. The collection of the social determinants of health (SDOH) is fundamental to addressing disparities. However, SDOH are inconsistently collected in many regions of the world. This two-phase multiple methods study examined patient and community perspectives regarding SDOH data collection in Canada. In phase 1, a survey was administered to patients at a cancer centre (n = 549) to assess perspectives on an SDOH data collection tool. In phase 2, broader perspectives were sought through a community consultation with patient partners experiencing structural inequality (n = 15). Most participants were comfortable with SDOH data collection. Of survey respondents, 95% were comfortable with the collection of language, birthplace, sex, gender, education, and disability, and 82% to 94% were comfortable with SES, sexual orientation, social support, and race/ethnicity. Discomfort levels did not differ across subgroups, except women were more uncomfortable disclosing SES (OR: 2.00; 95%CI: 1.26, 3.19). Most (71%) preferred face-to-face data collection with a healthcare professional and only half were comfortable with storage of SDOH in electronic health records. Open-ended survey responses (n = 1533) and the community consultation revealed concerns about privacy, discrimination, relevance to care, and data accuracy. SDOH data collection efforts should include a clear rationale for patients, training for providers, strong data privacy and security measures, and actionable strategies to address needs.
Full article
(This article belongs to the Special Issue Health Disparities and Outcomes in Cancer Survivors)
►▼
Show Figures

Figure 1
Open AccessArticle
Pemigatinib in the Real-World Management of Cholangiocarcinoma Through a Canadian Patient Support Program
by
Philip Q. Ding, Vincent C. Tam, Ravi Ramjeesingh, Jamil Asselah, Brandon S. Sheffield, Taylor Mitchell, Anne-Julie Gaudreau, Jennifer J. Knox and Winson Y. Cheung
Curr. Oncol. 2025, 32(7), 405; https://doi.org/10.3390/curroncol32070405 - 16 Jul 2025
Abstract
Background: In September 2021, pemigatinib received Health Canada approval for previously treated locally advanced/metastatic cholangiocarcinoma (CCA) with FGFR2 rearrangements/fusions. This retrospective study aimed to characterize the real-world management and outcomes of patients with CCA receiving pemigatinib through a Canadian patient support program (PSP).
[...] Read more.
Background: In September 2021, pemigatinib received Health Canada approval for previously treated locally advanced/metastatic cholangiocarcinoma (CCA) with FGFR2 rearrangements/fusions. This retrospective study aimed to characterize the real-world management and outcomes of patients with CCA receiving pemigatinib through a Canadian patient support program (PSP). Methods: We evaluated a multi-centre case series of Canadian patients who were prescribed pemigatinib between September 2021 and January 2023 for eligible CCA diagnoses and enrolled in the PSP. The retrospective study data included demographic and disease-, treatment-, and outcome-related information, and these were collected using a survey of prescribing physicians. Results: Of the 26 patients who initiated pemigatinib in the PSP, we received survey responses for 18 (69%). Their median age was 57 years, 67% were female, 61% had stage IV disease, and 83% had intrahepatic CCA. Prior to pemigatinib, a partial hepatectomy was performed in 44% of the patients, and 66% of the patients received 2–4 prior lines of systemic therapy. All patients were treated with platinum-based regimens as the first-line treatment for unresectable/metastatic disease. The median follow-up time on pemigatinib was 12.6 (range: 2.3–28.4) months, and their median real-world progression-free survival (rwPFS) was 12.1 months (95% CI 7.2-NR). The physician-assessed objective response and disease control rates were 56% and 89%, respectively. For the nine patients who discontinued pemigatinib, the median treatment duration was 10.6 months (range: 0.8–21.7). Disease progression was the most common reason for discontinuation (89%). None discontinued due to adverse events. Conclusions: Objective response rates, disease control rates, and a PFS comparable to that in the phase 2 FIGHT-202 trial was reported with pemigatinib use in this Canadian PSP cohort.
Full article
(This article belongs to the Special Issue Biliary Tract Cancer Updates: Advancements and Insights)
►▼
Show Figures

Figure 1
Open AccessArticle
Differential BACH1 Expression in Basal-like Breast Tumors of Black Women Identified via Immunohistochemistry
by
N. M. Dowling, Galina Khramtsova, Olufunmilayo Olopade, Shabnam Samankan, Bok-Soon Lee and Jiyoung Lee
Curr. Oncol. 2025, 32(7), 404; https://doi.org/10.3390/curroncol32070404 - 14 Jul 2025
Abstract
BACH1 has been identified as a functional regulator of cancer metastasis and metabolic signaling in breast cancer cells. However, the clinical relevance of BACH1 expression in breast tumors remains poorly understood. Using a tissue microarray from a cohort of 130 patients, we assessed
[...] Read more.
BACH1 has been identified as a functional regulator of cancer metastasis and metabolic signaling in breast cancer cells. However, the clinical relevance of BACH1 expression in breast tumors remains poorly understood. Using a tissue microarray from a cohort of 130 patients, we assessed the expression of BACH1 and its known target gene, MCT1 (encoded by SLC16A1), through immunohistochemistry (IHC). The expression data were then analyzed in relation to clinical variables, including breast cancer subtypes, tissue types, tumor size and grade, patient racial background, and age group. We found positive associations between BACH1 expression and tumor size, tumor grade, and the basal-like subtype. Importantly, BACH1 expression was significantly higher in tumors from Black women compared to those from White women, as well as in the basal-like subtype of breast tumors from Black women. Additionally, a positive correlation was observed between BACH1 and MCT1 IHC scores in tumors from Black women, while a weak association was noted in tumors from White women. Our study provides compelling evidence that BACH1 expression is evident based on the race and subtypes of breast cancer patients.
Full article
(This article belongs to the Topic From Basic Research to a Clinical Perspective in Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
MET Exon 14 Skipping Mutations in Lung Cancer: Clinical–Pathological Characteristics and Immune Microenvironment
by
Qianqian Xue, Yue Wang, Qiang Zheng, Ziling Huang, Yicong Lin, Yan Jin and Yuan Li
Curr. Oncol. 2025, 32(7), 403; https://doi.org/10.3390/curroncol32070403 - 14 Jul 2025
Abstract
MET exon 14 skipping mutations have emerged as significant driver alterations in non-small-cell lung cancer (NSCLC), contributing to tumor progression. This study examines the immune microenvironment in NSCLC patients with these mutations and its prognostic implications. We performed multiplex immunofluorescence (mIF) staining on
[...] Read more.
MET exon 14 skipping mutations have emerged as significant driver alterations in non-small-cell lung cancer (NSCLC), contributing to tumor progression. This study examines the immune microenvironment in NSCLC patients with these mutations and its prognostic implications. We performed multiplex immunofluorescence (mIF) staining on formalin-fixed paraffin-embedded (FFPE) tissue samples from nine NSCLC patients, including four recurrent/metastatic and five non-recurrent/non-metastatic patients. Two panels assessed immune cell markers (CD8, CD4, CD20, CD68, and FoxP3) and immune checkpoints (PD-L1, LAG3, and TIM3). Immune cell infiltration and checkpoint expression were analyzed using HALOTM software (version 3.6.4134.464). Nearest neighbor analysis was conducted to assess the proximity of immune cells to tumor cells. Univariate Cox regression analysis assessed factors associated with disease-free survival (DFS). CD8+TIM3+ and CD8+LAG3+ cells were predominantly located in the tumor parenchyma of recurrent/metastatic patients but localized to the stroma in non-recurrent/non-metastatic patients. Non-recurrent/non-metastatic patients exhibited a higher density of tertiary lymphoid structures and closer proximity of CD20+ B cells, CD8+TIM3+, and CD8+LAG3+ cells to tumor cells compared to recurrent/metastatic patients, though the differences were not statistically significant. Cox regression analysis suggested a potential association between higher densities of CD8+TIM3+ cells and improved DFS (HR = 0.89), though these findings did not reach statistical significance. Our findings suggest that differences in immune microenvironmental factors, particularly those related to immune checkpoint expression (TIM3 and LAG3), may influence clinical outcomes in NSCLC patients with MET exon 14 skipping mutations. Further studies are needed to validate these observations and explore potential therapeutic implications.
Full article
(This article belongs to the Special Issue Current State of Immunotherapy for Lung Cancer: Focusing on Real-World Evidence)
►▼
Show Figures
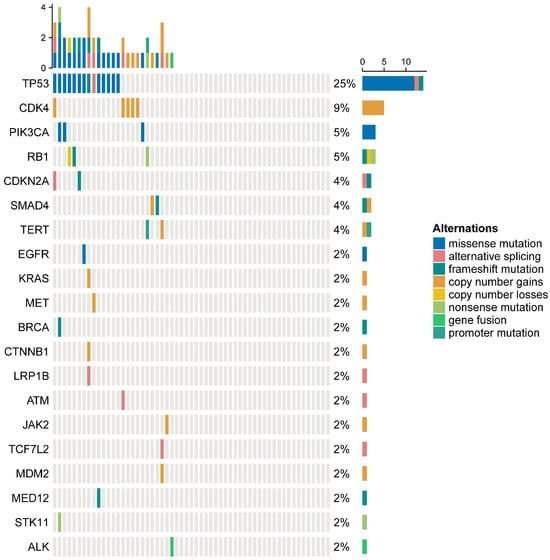
Figure 1
Open AccessPerspective
Optimizing Adjuvant Care in Early Breast Cancer: Multidisciplinary Strategies and Innovative Models from Canadian Centers
by
Angela Chan, Nancy Nixon, Muna Al-Khaifi, Alain Bestavros, Christine Blyth, Winson Y. Cheung, Caroline Hamm, Thomas Joly-Mischlich, Mita Manna, Tom McFarlane, Laura V. Minard, Sarah Naujokaitis, Christine Peragine, Cindy Railton and Scott Edwards
Curr. Oncol. 2025, 32(7), 402; https://doi.org/10.3390/curroncol32070402 - 14 Jul 2025
Abstract
The adjuvant treatment landscape for hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–) early breast cancer (EBC) is rapidly evolving, with a diverse range of therapeutic options—including endocrine therapies, bisphosphonates, ovarian function suppression, olaparib, CDK4/6 inhibitors, and emerging agents such as
[...] Read more.
The adjuvant treatment landscape for hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–) early breast cancer (EBC) is rapidly evolving, with a diverse range of therapeutic options—including endocrine therapies, bisphosphonates, ovarian function suppression, olaparib, CDK4/6 inhibitors, and emerging agents such as immunotherapy. While these advances have markedly improved patient outcomes, they also introduce challenges related to implementation, monitoring, and resource allocation. Notably, therapies like CDK4/6 inhibitors require particularly close monitoring, creating logistical and capacity challenges for medical oncologists, whose workloads are already stretched due to rising cancer incidence and treatment complexities. These challenges underscore the need for innovative care delivery solutions to ensure patients with EBC continue to receive optimal care. This paper offers a comprehensive guide—a playbook—of multidisciplinary-team-based care models designed to optimize adjuvant treatment delivery in EBC. Drawing on real-world evidence and successful applications across Canadian centers, we explore models led by nurses, nurse practitioners (NPs), general practitioners in oncology (GPO), and pharmacists. Each model leverages the unique expertise of its team to manage treatment toxicities, facilitate adherence, and enhance patient education, thereby promoting effective and sustainable care delivery. Importantly, these models are not intended to compete with one another, but rather to serve as a flexible recipe book from which breast cancer care teams can draw strategies tailored to their local resources and patient needs. By detailing implementation strategies, benefits, and challenges—in many instances supported by quantitative metrics and economic evaluations—this work aims to inspire care teams nationwide to optimize the adjuvant management of patients with HR+, HER2– EBC.
Full article
(This article belongs to the Section Breast Cancer)
►▼
Show Figures
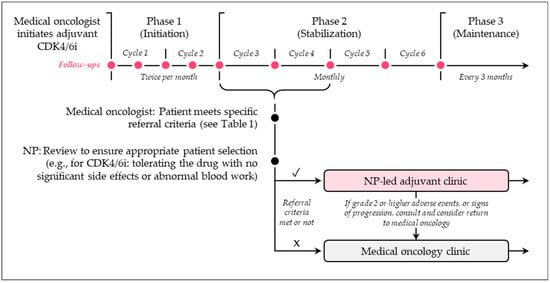
Figure 1
Open AccessArticle
A Matched Case-Control Study Examining the Association Between Exposure to Depot Medroxyprogesterone Acetate and Cerebral Meningioma Using an Active Comparator
by
Russell Griffin and Rebecca Arend
Curr. Oncol. 2025, 32(7), 401; https://doi.org/10.3390/curroncol32070401 - 13 Jul 2025
Abstract
The recent literature has reported an increased association between the use of depot medroxyprogesterone acetate (dMPA) and cerebral meningioma (CM). Prior studies have been limited in generalizability and did not use an active comparator as a control. The current matched case–control study utilized
[...] Read more.
The recent literature has reported an increased association between the use of depot medroxyprogesterone acetate (dMPA) and cerebral meningioma (CM). Prior studies have been limited in generalizability and did not use an active comparator as a control. The current matched case–control study utilized a bootstrapped sampling design, matching 241 CM cases with controls (i.e., women diagnosed with non-meningioma brain, breast, or skin tumor, one control per type for three total) on age ± 5 years and diagnosis date ± 3 months. Conditional logistic regression was used to estimate odds ratios (ORs) compared with an active (norethindrone or levonorgestrel) and non-active control group. Exposure to dMPA at any time point was not associated with the diagnosis of cerebral meningioma (OR 1.75, 95% CI 0.81–4.95). Exposure to dMPA within a year of diagnosis was associated with the diagnosis of CM compared to both an active control (OR 3.38, 95% CI 1.13–9.70) and a non-active control (OR 6.90, 95% CI 2.31–17.58). This association was also present for those who were exposed within two years prior when compared to a non-active control (OR 3.54, 95% CI 1.50–11.88) but not an active control. Combined with the prior literature, the current results suggest that future research is warranted to understand this association.
Full article
(This article belongs to the Section Neuro-Oncology)
►▼
Show Figures
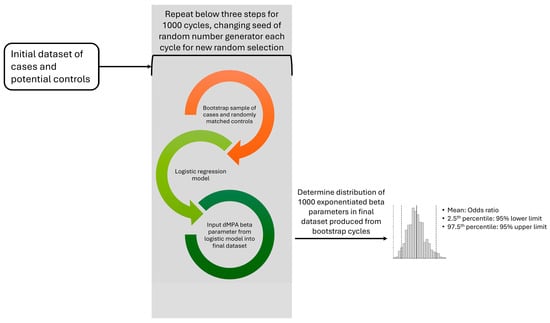
Figure 1
Open AccessArticle
Effects of Gratitude Journaling on Patients with Breast Cancer: A Randomized Controlled Trial
by
Minjeong You and Eunjung Kim
Curr. Oncol. 2025, 32(7), 400; https://doi.org/10.3390/curroncol32070400 - 12 Jul 2025
Abstract
Gratitude journaling is a simple and effective way to improve emotional well-being. However, its impact on people with breast cancer in South Korea has not been clearly understood. This study explored how writing a gratitude journal can help patients with breast cancer feel
[...] Read more.
Gratitude journaling is a simple and effective way to improve emotional well-being. However, its impact on people with breast cancer in South Korea has not been clearly understood. This study explored how writing a gratitude journal can help patients with breast cancer feel more grateful, resilient, and satisfied with life. Sixty patients from a university hospital in Jeollanam-do were randomly assigned to either a gratitude journaling group or a control group. The journaling group received guidance and wrote at least ten journal entries over three weeks, with weekly phone check-ins. The control group received no intervention. Before and after the program, the participants completed surveys. The results showed that those who kept gratitude journals had higher levels of gratitude, resilience, and quality of life than those who did not. These findings suggest that gratitude journaling can be a valuable and easy-to-use nursing strategy to support the emotional health of breast cancer patients.
Full article
(This article belongs to the Section Breast Cancer)
►▼
Show Figures

Figure 1
Open AccessArticle
Continuity of Cancer Care: Female Participants’ Report of Healthcare Experiences After Conclusion of Primary Treatment
by
Mirna Becevic, Garren Powell, Allison B. Anbari and Jane A. McElroy
Curr. Oncol. 2025, 32(7), 399; https://doi.org/10.3390/curroncol32070399 - 11 Jul 2025
Abstract
Background: Understanding patient perceptions of cancer care is crucial for improving treatment experiences and health outcomes. This study explores female patient-reported experiences with cancer care. Our aim was to identify areas for improvement and enhance patient-centered approaches in specialty and primary care settings.
[...] Read more.
Background: Understanding patient perceptions of cancer care is crucial for improving treatment experiences and health outcomes. This study explores female patient-reported experiences with cancer care. Our aim was to identify areas for improvement and enhance patient-centered approaches in specialty and primary care settings. Methods: This was a prospective observational study using ResearchMatch. Our eligibility criteria were 40 years or older adult cancer diagnosis, female, and treated for cancer in the United States. Results: Among the eligible participants (n = 1224), 64 responded to the invitation and 57 completed the survey (89% participation proportion). The majority of the respondents were not receiving treatment during the study period (68%). Of those, 89% completed the recommended treatment, and 10% stopped the treatment before completion. Nearly 80% of respondents saw the same oncologist during the treatment at every appointment, and only 8% reported changing clinicians during their primary cancer treatment. Over 63% of respondents were not seeing the same primary care clinician as they did when they were first diagnosed. Respondents reported facing challenges with employment and ability to return to work (26%), being able to afford medication (21%), and paying medical bills (15%). Discussion: This study, albeit for a small number of participants (n = 57) identified strengths and challenges in cancer care. Consistent oncologist involvement and proximity to care centers was consistently reported during active treatment. Discontinuity with primary care, however, may warrant further inquiry. Reported financial, employment and access issues support previous studies that identified these as major challenges during and after active cancer treatment. Our study underscored the need to enhance patient-centered coordination and support to improve cancer and survivorship care outcomes.
Full article
(This article belongs to the Section Psychosocial Oncology)
Open AccessConference Report
Report from the 26th Annual Western Canadian Gastrointestinal Cancer Consensus Conference on Hepatocellular and Biliary Tract Cancer, Saskatoon, Saskatchewan, 17–18 October 2024
by
Deepti Ravi, Shahid Ahmed, Blaire Anderson, Brady Anderson, Bryan Brunet, Haji Chalchal, Arun Elangovan, Georgia Geller, Vallerie Gordon, Branawan Gowrishankar, Edward Hardy, Mussawar Iqbal, Duc Le, Richard Lee-Ying, Shazia Mahmood, Karen Mulder, Maged Nashed, Killian Newman, Maurice Ogaick, Vibhay Pareek, Jennifer Rauw, Ralph Wong and Adnan Zaidiadd
Show full author list
remove
Hide full author list
Curr. Oncol. 2025, 32(7), 398; https://doi.org/10.3390/curroncol32070398 - 10 Jul 2025
Abstract
The 26th annual Western Canadian Gastrointestinal Cancer Consensus Conference (WCGCCC) was held in Saskatoon, Saskatchewan, on 17–18 October 2024. The WCGCCC is an interactive multidisciplinary conference that was attended by healthcare professionals from across Western Canada (British Columbia, Alberta, Saskatchewan, and Manitoba) who
[...] Read more.
The 26th annual Western Canadian Gastrointestinal Cancer Consensus Conference (WCGCCC) was held in Saskatoon, Saskatchewan, on 17–18 October 2024. The WCGCCC is an interactive multidisciplinary conference that was attended by healthcare professionals from across Western Canada (British Columbia, Alberta, Saskatchewan, and Manitoba) who are involved in the care of patients with hepatocellular and biliary tract cancers. Specialists from the fields of medical and radiation oncology, interventional radiology, pathology and laboratory medicine, and general and hepatobiliary surgery participated in presentations and discussions for the purpose of developing the recommendations presented here. This consensus statement addresses current issues in the management of hepatocellular and biliary tract cancers.
Full article
(This article belongs to the Section Gastrointestinal Oncology)
Open AccessReview
Perioperative Chemo/Immunotherapies in Lung Cancer: A Critical Review on the Value of Perioperative Sequences
by
Thoma’ Dario Clementi, Francesca Colonese, Stefania Canova, Maria Ida Abbate, Luca Sala, Francesco Petrella, Gabriele Giuseppe Pagliari and Diego Luigi Cortinovis
Curr. Oncol. 2025, 32(7), 397; https://doi.org/10.3390/curroncol32070397 - 10 Jul 2025
Abstract
Resectable non-small cell lung cancer (NSCLC) continues to pose significant challenges with high recurrence and mortality rates, despite traditional platinum-based chemotherapy yielding only an approximate 5% improvement in 5-year overall survival when administered preoperatively or postoperatively. In recent years, the integration of immune
[...] Read more.
Resectable non-small cell lung cancer (NSCLC) continues to pose significant challenges with high recurrence and mortality rates, despite traditional platinum-based chemotherapy yielding only an approximate 5% improvement in 5-year overall survival when administered preoperatively or postoperatively. In recent years, the integration of immune checkpoint inhibitors (ICIs), such as nivolumab, durvalumab and pembrolizumab, with platinum-based regimens in the perioperative setting has emerged as a transformative strategy. Our comprehensive review, based on a systematic bibliographic search of PubMed, Google Scholar, EMBASE, Cochrane Library, and clinicaltrials.gov, targeting pivotal clinical trials from the past two decades, examines the impact of these neoadjuvant and adjuvant chemoimmunotherapy approaches on major pathological response rates and overall survival in early-stage NSCLC. Although these perioperative strategies represent a paradigm shift in treatment, promising durable responses are offset by persistent recurrence, emphasizing the necessity for optimized treatment sequencing, duration, and the identification of predictive biomarkers. Collectively, our findings underscore the critical role of the perioperative schema, particularly the neoadjuvant component, which enables the evaluation of novel biomarkers as surrogates for overall survival, in improving patient outcomes and delineating future research directions aimed at reducing mortality and enhancing the quality of life for patients with resectable NSCLC.
Full article
(This article belongs to the Special Issue The Current Status of Lung Cancer Surgery)
Open AccessConference Report
Prioritizing the Timely Detection and Diagnosis of Early-Age Onset Cancer to Enable Optimal Disease Management and Outcomes
by
Michael J. Raphael, Petra Wildgoose, Darren Brenner, Christine Brezden-Masley, Ronald Burkes, Robert C. Grant, Alexandra Pettit, Cassandra Macaulay, Monika Slovinec D’Angelo and Filomena Servidio-Italiano
Curr. Oncol. 2025, 32(7), 396; https://doi.org/10.3390/curroncol32070396 - 10 Jul 2025
Abstract
In November 2024, the fourth annual Symposium focusing on early-age onset cancer (EAOC) was hosted by the Colorectal Cancer Resource & Action Network (CCRAN), assembling clinicians, researchers, and patients virtually to discuss challenges in early detection and diagnosis of individuals afflicted with EAOC
[...] Read more.
In November 2024, the fourth annual Symposium focusing on early-age onset cancer (EAOC) was hosted by the Colorectal Cancer Resource & Action Network (CCRAN), assembling clinicians, researchers, and patients virtually to discuss challenges in early detection and diagnosis of individuals afflicted with EAOC across tumour types. The meeting addressed the rising rates of EAOC and identified strategies to overcome barriers to timely detection and diagnosis by closing gaps in public and healthcare provider knowledge on symptoms of cancer in younger adults and reducing inequities in standard screening for younger age groups. Discussions also encompassed the various factors that serve as impediments to accessing diagnostic testing and obtaining results, as well as the critical need for access to diagnostics such as comprehensive genomic profiling (CGP), the results of which could be imperative in helping to guide clinical decisions regarding effective and well-tolerated targeted therapies. The Symposium generated key calls to action regarding increasing EAOC education and awareness among primary care providers and the public, re-evaluation of cancer screening programs’ eligibility criteria to include younger populations, and mechanisms to reduce waiting times for diagnostic testing by addressing technologist shortages and improving access to CGP through national collaborative strategies and increased funding.
Full article
Open AccessArticle
Pre-Implementation Assessment of a Sexual Health eClinic in Canadian Oncology Care
by
Taylor Incze, Dalia Peres, Steven Guirguis, Sarah E. Neil-Sztramko, Jackie Bender, Dean Elterman, Shabbir M. H. Alibhai, Antonio Finelli, Phil Vu Bach, Emily Belita, Gerald Brock, Julia Brown, Jeffrey Campbell, Trustin Domes, Andrew Feifer, Ryan Flannigan, Celestia Higano, Jesse Ory, Premal Patel, Monita Sundar, Luke Witherspoon and Andrew Matthewadd
Show full author list
remove
Hide full author list
Curr. Oncol. 2025, 32(7), 395; https://doi.org/10.3390/curroncol32070395 - 10 Jul 2025
Abstract
Sexual dysfunction is a prevalent and often under-addressed concern among prostate cancer survivors, significantly affecting quality of life for patients and their partners. The True North Sexual Health and Rehabilitation eClinic (SHAReClinic) is a virtual, biopsychosocial intervention developed to improve access to sexual
[...] Read more.
Sexual dysfunction is a prevalent and often under-addressed concern among prostate cancer survivors, significantly affecting quality of life for patients and their partners. The True North Sexual Health and Rehabilitation eClinic (SHAReClinic) is a virtual, biopsychosocial intervention developed to improve access to sexual health support for prostate cancer survivors and their partners. This study used a qualitative descriptive design to examine barriers and facilitators influencing the integration of SHAReClinic into oncology care across nine Canadian health care centres. Semi-structured interviews were conducted with 17 knowledge users, including health care providers and institutional leaders. Data were analyzed using a hybrid deductive–inductive thematic approach guided by the Consolidated Framework for Implementation Research (CFIR) 2.0. Participants described SHAReClinic as a much-needed resource, particularly in the absence of standardized sexual health pathways in oncology care. The virtual format was seen as accessible and well suited to addressing sensitive topics. However, limited funding, lack of institutional support, and workflow integration challenges emerged as primary barriers to implementation. Findings offer practical, theory-informed guidance for integrating SHAReClinic into oncology care and highlight key considerations for developing sustainable and scalable survivorship care models.
Full article
(This article belongs to the Section Genitourinary Oncology)
Open AccessArticle
Survival Outcomes in Patients with Squamous Cell Carcinoma of the Urinary Bladder: A Propensity Score-Matched Analysis
by
Alper Coskun, Ahmet Bilgehan Sahin, Selva Kabul, Muhammed Abdurrahman Celik, Mursel Sali, Ender Eren Ozcelik, Adem Deligonul, Erdem Cubukcu, Meral Kurt, Gursel Savci, Turkkan Evrensel and Ismet Yavascaoğlu
Curr. Oncol. 2025, 32(7), 394; https://doi.org/10.3390/curroncol32070394 - 10 Jul 2025
Abstract
Background and Objective: Bladder cancer (BC) is the ninth most common malignancy worldwide. Squamous cell carcinoma (SqCC), a rare histological variant, accounts for approximately 2–5% of all BC cases. Compared to urothelial carcinoma, the predominant subtype, research on SqCC remains limited and shows
[...] Read more.
Background and Objective: Bladder cancer (BC) is the ninth most common malignancy worldwide. Squamous cell carcinoma (SqCC), a rare histological variant, accounts for approximately 2–5% of all BC cases. Compared to urothelial carcinoma, the predominant subtype, research on SqCC remains limited and shows inconsistent findings regarding prognosis. This study aimed to compare survival outcomes between patients with SqCC and those with pure urothelial carcinoma (PUC). Methods: This retrospective, observational study analyzed pathology reports from 2549 transurethral resections of bladder tumors and 632 cystectomies performed at our institution between 1 December 2010 and 31 December 2023. Following pathological re-evaluation, 33 patients with SqCC and 132 with PUC were identified. After 1:3 propensity score matching, 20 patients with SqCC and 58 with PUC were included in the final analysis. Demographic, clinicopathological features, and survival outcomes were compared between groups. Results: The median follow-up was 2.31 years (range: 0.17–13.50). No significant differences in baseline demographic or clinical characteristics were observed, except for the type of surgery. Kaplan–Meier analysis demonstrated no significant differences in disease-free survival (DFS; p = 0.961) or overall survival (OS; p = 0.847) between SqCC and PUC groups. Multivariate Cox regression analysis identified T stage, nodal involvement, and adjuvant chemotherapy (CT) as independent predictors of DFS, while sex and metastasis at diagnosis were significant predictors of OS. Conclusion: Survival outcomes (DFS and OS) did not significantly differ between patients with SqCC and patients with PUC. Prognosis was more closely associated with disease stage at diagnosis, sex, and adjuvant CT. Further large-scale studies are warranted.
Full article
(This article belongs to the Section Genitourinary Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
The Effect of Prophylactic Hepatoprotective Therapy on Drug-Induced Liver Injury in Patients Undergoing Chemotherapy for Cervical Cancer: A Retrospective Analysis Based on Propensity Score Matching
by
Zhe Liu, Dongliang Yuan, Jun Chang, Lei Shi, Jingmeng Li, Mei Zhao and Qi Yang
Curr. Oncol. 2025, 32(7), 393; https://doi.org/10.3390/curroncol32070393 - 9 Jul 2025
Abstract
This retrospective study aimed to assess the effectiveness of prophylactic hepatoprotective therapy in decreasing the incidence of drug-induced liver injury (DILI) among patients with cervical cancer undergoing chemotherapy. The analysis was performed on patients with cervical cancer who received chemotherapy at a tertiary
[...] Read more.
This retrospective study aimed to assess the effectiveness of prophylactic hepatoprotective therapy in decreasing the incidence of drug-induced liver injury (DILI) among patients with cervical cancer undergoing chemotherapy. The analysis was performed on patients with cervical cancer who received chemotherapy at a tertiary hospital between September 2019 and August 2020. Propensity score matching (PSM) was utilized to equilibrate baseline characteristics between the treatment group, which received prophylactic hepatoprotective drugs, and the control group, which did not receive prophylaxis. The incidence and severity of liver injury were evaluated using the Common Terminology Criteria for Adverse Events (CTCAE) version 5.0. Out of the 609 patients initially screened, 299 were included following PSM, with 105 in the treatment group and 194 in the control group. There were no significant differences in the incidence of liver injury (21.90% vs. 18.04%, p = 0.420) or its severity (p = 0.348) observed between the groups. Furthermore, none of the subgroups exhibited a significant reduction in DILI risk with prophylaxis. However, the number of patients experiencing an increase in their grade of liver injury was significantly higher in the treatment group (18.10% vs. 13.40%, p = 0.002), with these patients also exhibiting increased levels of alkaline phosphatase (ALP) and direct bilirubin (DBIL) post-chemotherapy (p < 0.05). Hepatoprotective drugs are not associated with a reduced risk of DILI and may in fact increase risk.
Full article
(This article belongs to the Topic Hepatobiliary and Pancreatic Diseases: Novel Strategies of Diagnosis and Treatments)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- Current Oncology Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal Browser-
arrow_forward_ios
Forthcoming issue
arrow_forward_ios Current issue - Volumes not published by MDPI
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Cancers, Diagnostics, JCM, Current Oncology, Gastrointestinal Disorders, Biomedicines, Therapeutics
Hepatobiliary and Pancreatic Diseases: Novel Strategies of Diagnosis and Treatments
Topic Editors: Alessandro Coppola, Damiano Caputo, Roberta Angelico, Domenech Asbun, Chiara MazzarelliDeadline: 20 August 2025
Topic in
Cancers, Current Oncology, JCM, Medicina, Onco
Cancer Biology and Radiation Therapy: 2nd Edition
Topic Editors: Chang Ming Charlie Ma, Ka Yu Tse, Ming-Yii Huang, Mukund SeshadriDeadline: 16 October 2025
Topic in
Biomedicines, Cancers, Current Oncology, Diagnostics, JCM
Advances in Magnetic Resonance Imaging (MRI) and Its Role in Radiation Therapy
Topic Editors: Indra J. Das, Minsong CaoDeadline: 31 October 2025
Topic in
Cancers, IJMS, Pharmaceuticals, Pharmaceutics, Sci. Pharm., Current Oncology, Molecules
Recent Advances in Anticancer Strategies, 2nd Edition
Topic Editors: Hassan Bousbaa, Zhiwei HuDeadline: 31 March 2026

Conferences
Special Issues
Special Issue in
Current Oncology
From Screening to Treatment: Technology’s Impact on Breast Cancer Care
Guest Editor: Jaroslaw SkokowskiDeadline: 31 July 2025
Special Issue in
Current Oncology
Building Hope for the Next Decade of Psychosocial Oncology: Optimizing the Integration of Supportive Care into Oncology Care
Guest Editors: Fredrick D. Ashbury, Jonathan Avery, Jackie Bender, Sylvie Lambert, Madeline Li, Gilla K. ShapiroDeadline: 31 July 2025
Special Issue in
Current Oncology
Feature Advancements in Section "Childhood, Adolescent and Young Adult Oncology"
Guest Editors: Katrin Scheinemann, Maria OtthDeadline: 31 July 2025
Special Issue in
Current Oncology
High-Grade Neuroendocrine Neoplasms
Guest Editor: Thorvardur HalfdanarsonDeadline: 31 July 2025
Topical Collections
Topical Collection in
Current Oncology
New Insights into Prostate Cancer Diagnosis and Treatment
Collection Editor: Sazan Rasul
Topical Collection in
Current Oncology
New Insights into Breast Cancer Diagnosis and Treatment
Collection Editors: Filippo Pesapane, Matteo Suter
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series in "Exercise and Cancer Management"
Collection Editors: Linda Denehy, Ravi Mehrotra, Nicole Culos-Reed
Topical Collection in
Current Oncology
Editorial Board Members’ Collection Series: Contemporary Perioperative Concepts in Cancer Surgery
Collection Editors: Vijaya Gottumukkala, Jörg Kleeff











