-
 Coenzyme Q10 and Cognition: A Review
Coenzyme Q10 and Cognition: A Review -
 Curcumin’s Neuroprotective Role: From Molecular Mechanisms to Clinical Translation
Curcumin’s Neuroprotective Role: From Molecular Mechanisms to Clinical Translation -
 Maternal Folate Excess, Placental Hormones, and Gestational Diabetes Mellitus: Findings from Prospective Cohorts Before and After Mandatory Folic Acid Food Fortification
Maternal Folate Excess, Placental Hormones, and Gestational Diabetes Mellitus: Findings from Prospective Cohorts Before and After Mandatory Folic Acid Food Fortification -
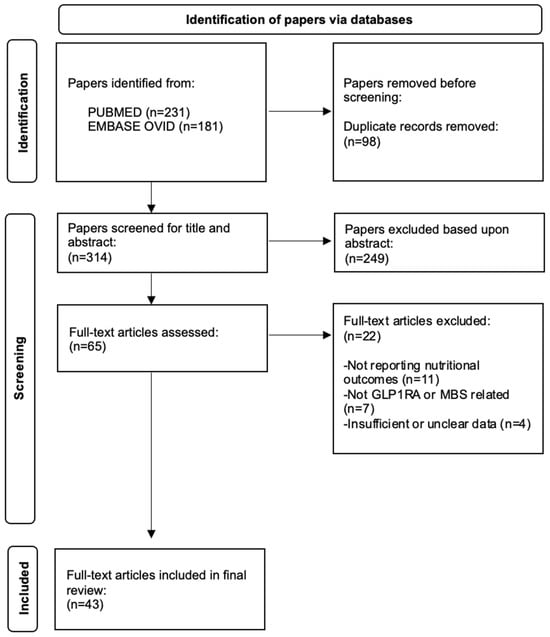
 Were Our Grandmothers Right? Soup as Medicine—A Systematic Review of Preliminary Evidence for Managing Acute Respiratory Tract Infections
Were Our Grandmothers Right? Soup as Medicine—A Systematic Review of Preliminary Evidence for Managing Acute Respiratory Tract Infections
Journal Description
Nutrients
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, Embase, PubAg, AGRIS, and other databases.
- Journal Rank: JCR - Q1 (Nutrition and Dietetics) / CiteScore - Q1 (Nutrition and Dietetics)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 12.9 days after submission; acceptance to publication is undertaken in 2.3 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
- Companion journal: Dietetics.
- Journal Cluster of Food, Nutrition, and Health Science: Beverages, Dietetics, Foods, Nutraceuticals, Nutrients and Obesities.
Latest Articles
E-Mail Alert
News
Topics
Deadline: 24 November 2025
Deadline: 15 December 2025
Deadline: 31 December 2025
Deadline: 30 January 2026
Conferences
Special Issues
Deadline: 25 November 2025
Deadline: 25 November 2025
Deadline: 25 November 2025
Deadline: 25 November 2025