Journal Description
Obesities
Obesities
is an international, peer-reviewed, open access journal on all aspects of obesity published bimonthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 13.4 days after submission; acceptance to publication is undertaken in 2.9 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Cluster of Food, Nutrition, and Health Science: Beverages, Dietetics, Foods, Nutraceuticals, Nutrients and Obesities.
Impact Factor:
1.3 (2024);
5-Year Impact Factor:
1.2 (2024)
Latest Articles
Is Crime Associated with Obesity and High Blood Pressure? Repeated Cross-Sectional Evidence from a Peruvian Study
Obesities 2025, 5(4), 95; https://doi.org/10.3390/obesities5040095 - 17 Dec 2025
Abstract
Violence is an emerging social determinant of health in Latin America; however, empirical evidence from Peru remains limited. This study examined the association between crime rates and the prevalence of obesity and high blood pressure in Peru from 2019 to 2023. Using a
[...] Read more.
Violence is an emerging social determinant of health in Latin America; however, empirical evidence from Peru remains limited. This study examined the association between crime rates and the prevalence of obesity and high blood pressure in Peru from 2019 to 2023. Using a repeated cross-sectional design with department–year aggregates, we analyzed nationally representative data from the Demographic and Family Health Survey, adjusting for sociodemographic, mental health, and geographic factors. Regional statistics on crime were incorporated into the analysis. The findings revealed a significant association between higher levels of crime and increased prevalence of self-reported high blood pressure and obesity. The association with obesity was particularly pronounced in border regions such as Tumbes, Madre de Dios, and Callao, where criminal activity is more prevalent. The findings indicate that prolonged exposure to violence may negatively impact biological stress responses, limit physical activity, and encourage the emergence of detrimental behaviors, consequently increasing the cardiometabolic risk burden in affected populations.
Full article
(This article belongs to the Special Issue Obesity in the 21st Century: Public Health Perspectives and Population Solutions)
►
Show Figures
Open AccessArticle
Assessment of Dietary Protein Sources Among Post-Sleeve Gastrectomy Patients in Saudi Arabia
by
Mashael T. Kharnoub, Randah M. Alqurashi, Samar M. Abdalla and Sultan Al Temyatt
Obesities 2025, 5(4), 94; https://doi.org/10.3390/obesities5040094 - 16 Dec 2025
Abstract
Obesity is a significant global health challenge, with prevalence rising steadily worldwide. Effective management often involves bariatric surgery, such as sleeve gastrectomy (SG), which has proven effective in reducing weight and improving comorbid conditions. This study aimed to evaluate nutritional status and protein
[...] Read more.
Obesity is a significant global health challenge, with prevalence rising steadily worldwide. Effective management often involves bariatric surgery, such as sleeve gastrectomy (SG), which has proven effective in reducing weight and improving comorbid conditions. This study aimed to evaluate nutritional status and protein source awareness and its impact on muscle mass among patients post SG surgery in Saudi Arabia. A cross-sectional study was conducted among 98 adults (aged 18–51 years) who underwent SG at the Department of Metabolic and Bariatric Surgery (Badana Clinic)/Mouwasat Hospital in Dammam from December 2023 to February 2024. Data were collected using an electronic questionnaire that covered demographics, dietary habits, physical activity, protein knowledge (from food and supplements), and a 24 h dietary recall. Body composition, including muscle mass, was assessed using the InBody270 Body Composition Analyzer. The results revealed that participants exhibited a high level of awareness regarding the importance of protein sources. However, muscle mass decreased by an average of 4.11 kg after surgery. This decline was attributed to insufficient protein intake, which ranged between 30 and 60 g per day, below recommended levels. Taste aversion and dietary limitations post-surgery contributed to this inadequate protein consumption. In conclusion, while participants understood the significance of protein for muscle maintenance, practical challenges in achieving adequate protein sources led to muscle mass loss. These findings underscore the importance of tailored nutritional strategies and education to optimize recovery and long-term health outcomes for SG surgery patients.
Full article
Open AccessArticle
Anthropometric Indicators of Obesity as Screening Tools for Hypertriglyceridemia in Older Adults: A Cross-Sectional Study
by
Max Wolfgang Farias Paiva, Caio Felipe de Sousa Miranda, Gabriel Alves Godinho, Carlos Daniel Dutra Lopes, Tony Souza Queiroz, Débora Jesus da Silva, Sabrina da Silva Caires, Paulo da Fonseca Valença Neto, Claudio Bispo de Almeida, Cezar Augusto Casotti, Beatriz Cardoso Roriz, Francisco Dimitre Rodrigo Pereira Santos, Octavio Luiz Franco, Danieli Fernanda Buccini, Arthur Barros Fernandes, Hellen Dayanny Ferreira Silva Pinheiro and Lucas dos Santos
Obesities 2025, 5(4), 93; https://doi.org/10.3390/obesities5040093 - 14 Dec 2025
Abstract
►▼
Show Figures
Background: Hypertriglyceridemia is a lipid disorder characterized by elevated plasma triglyceride levels, and its prevalence increases with aging. This condition contributes substantially to morbidity and mortality in older adults. In settings with limited access to laboratory testing, especially in developing countries such as
[...] Read more.
Background: Hypertriglyceridemia is a lipid disorder characterized by elevated plasma triglyceride levels, and its prevalence increases with aging. This condition contributes substantially to morbidity and mortality in older adults. In settings with limited access to laboratory testing, especially in developing countries such as Brazil, identifying low-cost and easily applicable screening tools is essential. Objective: To investigate the discriminatory capacity of anthropometric indicators of obesity for screening hypertriglyceridemia in older adults. Methods: A population-based cross-sectional study was conducted with 223 community-dwelling older adults (57% women). Independent variables included body mass index (BMI), waist circumference (WC), abdominal circumference (AC), triceps skinfold thickness (TSF), body adiposity index (BAI), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR), and conicity index (CI). Hypertriglyceridemia was defined as triglyceride levels ≥ 150 mg/dL. Discriminatory performance was assessed using receiver operating characteristic (ROC) curves, and associations were examined using Poisson regression with robust variance. Results: The prevalence of hypertriglyceridemia was 35%. Among older men, AC and CI showed the highest sensitivities (88.90% and 77.40%), while WHR and BMI demonstrated the highest specificities (83.10% and 76.90%). In older women, AC and BMI had the highest sensitivities (95.70% and 87.20%), whereas CI and WHtR exhibited the highest specificities (72.50% and 68.80%). All anthropometric indicators were positively associated with hypertriglyceridemia after adjustment for confounders. Conclusions: AC and CI demonstrated the strongest discriminatory capacity for screening older men with a higher probability of presenting hypertriglyceridemia, while AC and BMI showed the greatest discriminatory capacity among older women. In contrast, WHR and BMI had the highest ability to rule out the condition in older men, whereas CI and WHtR performed this role more effectively in older women. These findings show that low-cost anthropometric indicators can be used in a complementary manner, combining the most sensitive and the most specific measures to support an optimized triage process for hypertriglyceridemia in older adults, particularly in resource-limited settings.
Full article

Figure 1
Open AccessReview
Genetic and Epigenetic Modifiers of Ketogenic Diet Responses: Roles of Sex and Age
by
Marko Sablić, Viktoria Čurila, Senka Blažetić, Marta Balog, Marija Heffer, Antonio Kokot and Vedrana Ivić
Obesities 2025, 5(4), 92; https://doi.org/10.3390/obesities5040092 - 10 Dec 2025
Abstract
►▼
Show Figures
The ketogenic diet (KD) is a metabolic intervention characterized by high fat and very low carbohydrate intake, showing significant metabolic, neuroprotective, and therapeutic effects. However, its efficacy varies widely due to individual genetic and epigenetic factors. This review synthesizes current knowledge of genes
[...] Read more.
The ketogenic diet (KD) is a metabolic intervention characterized by high fat and very low carbohydrate intake, showing significant metabolic, neuroprotective, and therapeutic effects. However, its efficacy varies widely due to individual genetic and epigenetic factors. This review synthesizes current knowledge of genes most strongly associated with KD response, including polymorphisms in FTO, APOA2, PPAR, SCN1A, KCNQ2, STXBP1, CDKL5, the MODY gene group, and SLC2A1, which shape outcomes across lipid metabolism, energy expenditure, inflammation, and neurotransmission. Epigenomic modifications induced by a KD, such as changes in DNA methylation and histone acetylation involving BDNF, SLC12A5, KLF14, and others, modulate functional metabolic and neurological effects. Sex and age further modulate KD effects through distinct patterns of gene activation and hormonal interactions. These variables together impact metabolic and neurological outcomes and are critical for developing personalized nutrition and disease management strategies. Based on the reviewed evidence, genetic and epigenetic profiling can help identify patients who are likely to benefit from a KD (e.g., GLUT1DS, PDH deficiency) and those in whom a KD may be ineffective or harmful (e.g., SCOT or SLC2A1-independent defects). The review concludes that genetic and epigenetic profiling is recommended for personalized dietary interventions.
Full article

Graphical abstract
Open AccessArticle
The Interplay of Diet, Lifestyle, and Metabolic Risk Among Saudi Adults with Metabolic Syndrome
by
Maryam S. Hafiz, Wala I. Alzahrani, Sarah N. Alsharif, Doaa A. Alyoubi, Amal M. Alrizqi and Hanan Alwassam
Obesities 2025, 5(4), 91; https://doi.org/10.3390/obesities5040091 - 8 Dec 2025
Abstract
Metabolic syndrome (MetS) is a multifactorial condition characterized by central obesity, hypertension, dyslipidaemia, and hyperglycaemia, predisposing individuals to cardiovascular disease and type 2 diabetes. This cross-sectional study investigated the relationship between dietary intake, sociodemographic factors, and components of MetS among Saudi adults aged
[...] Read more.
Metabolic syndrome (MetS) is a multifactorial condition characterized by central obesity, hypertension, dyslipidaemia, and hyperglycaemia, predisposing individuals to cardiovascular disease and type 2 diabetes. This cross-sectional study investigated the relationship between dietary intake, sociodemographic factors, and components of MetS among Saudi adults aged 30 years and older attending King Abdulaziz University Hospital. Fifty-three participants meeting MetS diagnostic criteria were assessed through anthropometric measurements, biochemical markers, and two-day dietary recalls analyzed using MyFood24 software. Descriptive and correlation analyses were conducted using SPSS 26.0. The majority of participants (73.6%) were aged over 50 years, were obese (75.5%), and exhibited a high waist circumference (94.3%). Low fibre (6.6 g/day) and high fat (41.8 g/day) intake patterns were evident. Salt intake showed a significant inverse correlation with systolic blood pressure (ρ = −0.36, p < 0.01), potentially reflecting under-reporting or dietary adjustments following diagnosis. Higher BMI correlated positively with waist circumference and diastolic pressure, while frequent physical activity correlated negatively with these parameters. These findings emphasize the influence of diet and lifestyle on metabolic risk and underscore the need for culturally tailored interventions promoting balanced macronutrient intake, increased fibre consumption, and enhanced physical activity to mitigate MetS prevalence among Saudi adults.
Full article
(This article belongs to the Special Issue Obesity and Its Comorbidities: Prevention and Therapy 2026)
Open AccessArticle
Evaluating Dose Titration in Semaglutide and Tirzepatide for Weight Loss: A Retrospective Academic Call Center Study
by
Goar Alvarez, Lianette Veliz, Stephanie Michaels, David Pino and Jun Wu
Obesities 2025, 5(4), 90; https://doi.org/10.3390/obesities5040090 - 5 Dec 2025
Abstract
Obesity affects approximately 40% of U.S. adults and is associated with increased cardiometabolic risk. While lifestyle interventions remain fundamental, pharmacologic therapies such as Semaglutide and tirzepatide have demonstrated significant weight reduction in clinical trials when titrated to maintenance doses. However, real-world adherence to
[...] Read more.
Obesity affects approximately 40% of U.S. adults and is associated with increased cardiometabolic risk. While lifestyle interventions remain fundamental, pharmacologic therapies such as Semaglutide and tirzepatide have demonstrated significant weight reduction in clinical trials when titrated to maintenance doses. However, real-world adherence to recommended titration schedules remains unclear. This retrospective observational study evaluated adults prescribed Semaglutide (Wegovy®) or Tirzepatide (Zepbound®) for weight management between January 2021 and April 2025 through ICUBAcares, a pharmacist-led call center. Primary outcomes included the proportion of patients reaching the recommended maintenance dose and time required to do so. Secondary outcomes examined prescriber specialty patterns and monthly plan costs for non-optimized dosing. Among 739 medication courses, 52.9% of Semaglutide users reached the 2.4 mg dose versus 77.6% of tirzepatide users reaching 15 mg (p < 0.001). Median time to maintenance was significantly shorter for tirzepatide (32 days) than Semaglutide (143 days) (p < 0.001). Endocrinologists had the highest success rate for Tirzepatide (88.2%), while family medicine had the highest volume for both. Non-optimized dosing was associated with higher estimated monthly plan costs. These findings underscore the importance of improving adherence to titration protocols in real-world settings to maximize both clinical and economic outcomes in obesity pharmacotherapy.
Full article
(This article belongs to the Special Issue Obesity and Its Comorbidities: Prevention and Therapy 2026)
►▼
Show Figures

Figure 1
Open AccessArticle
Trends in Anthropometric and Cardiometabolic Risk Factor Changes Among Health Professionals: A 3-Year Follow-Up Study in Taiwan
by
Yi-Ru Chen, Nain-Feng Chu, Der-Min Wu and Wen-Chuan Shen
Obesities 2025, 5(4), 89; https://doi.org/10.3390/obesities5040089 - 4 Dec 2025
Abstract
Objectives: The purpose of this study is to evaluate the trend of anthropometric and cardiometabolic risk (CMRs) changes among health professionals over a three-year period at a medical center in Taiwan. Study Design: A 3-year follow-up cohort study design. Methods: This cohort study
[...] Read more.
Objectives: The purpose of this study is to evaluate the trend of anthropometric and cardiometabolic risk (CMRs) changes among health professionals over a three-year period at a medical center in Taiwan. Study Design: A 3-year follow-up cohort study design. Methods: This cohort study was conducted from 2019 to 2022 in a single healthcare center. The participants underwent annual physical check-ups for three consecutive years. CMRs were measured using standard methods and weight status change was measured using BMI. We used McNemar test and Wilcoxon Sign Rank test to evaluate the differences within and between subgroups. We used logistic regression to examine the risk of increased CMRs among subgroups of different weight status changes. Results: A total of 2217 participants (1641 females and 576 males) were included in this study, with a mean age of 40.2 ± 10.2 years. During this period, 72 (4.4%) female participants’ weight status changed from normal weight to overweight or obese and 530 (32.3%) remained overweight or obese. Among males, the proportion was 6.8% and 61.1%, respectively (p < 0.01). Participants who remained overweight or obese have more adverse CMRs. Compared to remained normal weight male subjects, the mean systolic blood pressure (131.0 ± 18.1 mmHg) and fasting blood glucose (94.4 ± 13.5 mg/dL) were higher in remained overweight or obese subjects (p < 0.001). Among females, those who remained overweight or obese have 4.01 (95% CI 2.92–5.51) times higher risk for abnormal diastolic blood pressure and 2.98 (95% CI 2.05–4.32) times higher risk for abnormal blood glucose compared to those with remained normal weight. Conclusions: Participants who remained overweight or became obese had more adverse CMRs such as high blood pressure, hyperglycemia, and dyslipidemia during the 3-year follow-up period.
Full article
Open AccessReview
Nutritional Approaches to Enhance GLP-1 Analogue Therapy in Obesity: A Narrative Review
by
Denise Deo Dias, Andrea Rodrigues Vasconcelos, Ana Carolina Remondi Souza, Caroline de Menezes, Isabella Sobral Teixeira e Silva and José João Name
Obesities 2025, 5(4), 88; https://doi.org/10.3390/obesities5040088 - 2 Dec 2025
Abstract
►▼
Show Figures
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are highly effective in the management of obesity; however, their efficacy and tolerability may be further optimized through complementary nutritional strategies. Such interventions may address key challenges associated with GLP-1RA therapy, including gastrointestinal adverse effects, lean mass loss,
[...] Read more.
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are highly effective in the management of obesity; however, their efficacy and tolerability may be further optimized through complementary nutritional strategies. Such interventions may address key challenges associated with GLP-1RA therapy, including gastrointestinal adverse effects, lean mass loss, and reduced long-term adherence leading to weight regain. Evidence from preclinical and clinical studies indicates that omega-3 polyunsaturated fatty acids may enhance the metabolic benefits of GLP-1RAs and attenuate lean mass loss, primarily via anti-inflammatory pathways and modulation of protein synthesis. Synergistic effects have also been reported with other bioactive compounds—such as flavonoids and anthocyanins, which improve metabolic outcomes; probiotics and prebiotics, which may alleviate gastrointestinal intolerance; and high-quality protein sources, which support body composition preservation. Collectively, these findings suggest that nutritional adjuncts may complement GLP-1RA therapies through convergent physiological mechanisms, including the regulation of inflammation, gut microbiome composition, and cellular metabolism. While current data highlight the promise of integrated pharmaco-nutritional strategies as adjuncts to GLP-1-based obesity therapy, further randomized controlled trials are needed to establish the most effective interventions and protocols.
Full article

Figure 1
Open AccessArticle
Cardiovascular Risk Assessment Across Different Obesity Phenotypes
by
Sergii Vernygorodskyi, Tetiana Sekret, Anton B. Tonchev, Kameliya Zhechkova Bratoeva and Viktor Vernihorodskii
Obesities 2025, 5(4), 87; https://doi.org/10.3390/obesities5040087 - 2 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Obesity is a major risk factor for cardiovascular disease (CVD), but traditional risk calculators such as Systematic COronary Risk Evaluation (SCORE2) may not fully capture the elevated risks in individuals with obesity, especially when metabolic health is considered. This study aimed to
[...] Read more.
Background/Objectives: Obesity is a major risk factor for cardiovascular disease (CVD), but traditional risk calculators such as Systematic COronary Risk Evaluation (SCORE2) may not fully capture the elevated risks in individuals with obesity, especially when metabolic health is considered. This study aimed to evaluate the effectiveness of QRESEARCH risk estimator version 3 (QRISK3) in estimating 10-year cardiovascular risk in individuals with varying obesity phenotypes compared to SCORE2. Methods: A total of 88 participants (25 men, 63 women; mean age 37.4 ± 11.8 years) were categorized into four obesity phenotypes according to metabolic and anthropometric criteria. The 10-year CVD risk was calculated using SCORE2 and QRISK3 algorithms. Functional cardiovascular assessment included blood pressure (BP) measurement and electrocardiogram (ECG) interpretation for conduction abnormalities and left ventricular hypertrophy (LVH). Biochemical analysis included carbohydrate metabolism (fasting glucose, postprandial glucose, HbA1c) and lipid profile (total cholesterol, LDL-C, HDL-C, triglycerides, atherogenic index). Results: SCORE2 underestimated CVD risk (3–8%), whereas QRISK3 predicted higher values (6–16%), particularly in metabolically unhealthy phenotypes. LVH occurred in 26–45% of participants, with elevated BP and early subclinical ECG changes even in metabolically healthy obesity individuals. Carbohydrate metabolism disturbances were observed in metabolically unhealthy participants with normal or elevated BMI, while lipid abnormalities—including elevated total cholesterol, LDL-C, triglycerides, and atherogenic index—were prominent in these metabolically unhealthy phenotypes. Insulin resistance, assessed via the triglyceride–glucose index, exceeded reference ranges in all obesity phenotypes, with the highest values seen in metabolically unhealthy individuals. Conclusions: QRISK3 provides a more precise and thorough assessment of 10-year cardiovascular risk in individuals with obesity than SCORE2. These findings highlight the importance of incorporating anthropometric and metabolic data into cardiovascular risk assessments and support the clinical use of QRISK3 for more personalized risk stratification, especially in populations with obesity and metabolic disturbances. Early identification of high-risk individuals using QRISK3 could lead to more timely and targeted preventive interventions, improving long-term cardiovascular outcomes.
Full article

Figure 1
Open AccessReview
Obesity: Genetic Insights, Therapeutic Strategies, Pharmacoeconomic Impact, and Psychosocial Dimensions
by
Gladious Naguib El-hadidy, Youssef Basem, Mahmoud M. Mokhtar, Salma A. Hamed, Sara M. Abdelstar, Abdelrhman R. Nasef and Rehab Abdelmonem
Obesities 2025, 5(4), 86; https://doi.org/10.3390/obesities5040086 - 28 Nov 2025
Abstract
Obesity has emerged as one of the most complex and urgent public health challenges of the twenty-first century, driven by genetic, environmental, metabolic, and psychosocial determinants that collectively disturb energy homeostasis and systemic health. It is characterized by adipose tissue dysfunction, insulin resistance,
[...] Read more.
Obesity has emerged as one of the most complex and urgent public health challenges of the twenty-first century, driven by genetic, environmental, metabolic, and psychosocial determinants that collectively disturb energy homeostasis and systemic health. It is characterized by adipose tissue dysfunction, insulin resistance, chronic low-grade inflammation, and gut microbiota dysbiosis, all of which interact to perpetuate metabolic and cardiovascular diseases. Beyond the biological dimension, obesity profoundly affects mental health, being closely linked to depression, anxiety, body-image dissatisfaction, and stigma, which further reduce adherence to treatment. Current therapeutic strategies rely on a stepped-care approach, beginning with lifestyle interventions encompassing dietary modification, physical activity, and behavioral therapy. Pharmacologic treatments, particularly incretin-based agents such as semaglutide, liraglutide, and tirzepatide have transformed medical management through substantial and sustained weight loss, while bariatric surgery remains the most effective long-term option for severe obesity. Emerging approaches, including gene therapy, microbiome modulation, and nanomedicine, offer mechanistically targeted and potentially safer alternatives, though they remain largely experimental. Pharmacoeconomic analyses support the cost-effectiveness of combining behavioral, pharmacological, and surgical modalities, highlighting the economic advantage of integrated care models. Meanwhile, artificial intelligence and machine learning are redefining obesity research and management, enhancing cancer risk prediction, personalizing pharmacotherapy, optimizing resource allocation, and enabling precision medicine through multi-omics and imaging integration. Collectively, these insights support a shift toward a learning health-system paradigm that unites mechanistically anchored therapies with digital and AI-driven personalization to achieve sustainable weight reduction, reduce cardiometabolic and cancer burden, and improve global health outcomes.
Full article
Open AccessArticle
Time Since Bariatric and Metabolic Surgery Is Associated with Ultra-Processed Food Intake and Food Addiction but Not with Culinary Abilities in Adults
by
André Eduardo da Silva-Júnior, Natália Gomes da Silva Lopes, Jennifer Mikaella Ferreira Melo, Maria Clara Tavares Farias da Silva, Mateus de Lima Macena and Nassib Bezerra Bueno
Obesities 2025, 5(4), 85; https://doi.org/10.3390/obesities5040085 - 28 Nov 2025
Abstract
►▼
Show Figures
To evaluate the consumption of ultra-processed foods (UPFs), culinary abilities, and food addiction (FA) in adults after different periods since bariatric and metabolic surgery, this cross-sectional study recruited and collected data via social media from adults who underwent metabolic and bariatric surgery. The
[...] Read more.
To evaluate the consumption of ultra-processed foods (UPFs), culinary abilities, and food addiction (FA) in adults after different periods since bariatric and metabolic surgery, this cross-sectional study recruited and collected data via social media from adults who underwent metabolic and bariatric surgery. The Brazil Food and Nutritional Surveillance System markers of dietary consumption and the NOVA-UPF screener assessed dietary patterns and UPF consumption, the modified Yale Food Addiction Scale 2.0 assessed FA, and the Cooking Skills Index (CSI) assessed culinary abilities. 1525 participants were included, with a mean age of 38 ± 8 years and a mean time since surgery of 37 ± 54 months. Individuals with longer postoperative time showed a higher NOVA-UPF score and higher consumption of hamburgers/sausages, sweetened beverages, and instant noodles (p < 0.01 for all), without a corresponding decrease in fresh fruit and vegetable consumption. Each year since surgery increased NOVA-UPF score by 0.67 [CI95%: 0.57; 0.76] points. CSI showed no association with time (−0.41; [CI95%: −1.33; 0.50]), while FA prevalence was lowest at 48 months and increased thereafter (p < 0.01). FA prevalence initially decreased up to 4 years post-surgery, followed by a partial increase beyond 4 years, although remaining below levels observed within the first 6 months. Time since surgery is associated with higher UPF consumption and a non-linear trajectory of FA prevalence, but not with culinary abilities.
Full article

Figure 1
Open AccessArticle
How Can Lockdown Influence Eating Habits? The Spanish Case During the COVID Pandemic
by
José I. Baile, María J. González-Calderón, María F. Rabito-Alcón and Eva Izquierdo-Sotorrío
Obesities 2025, 5(4), 84; https://doi.org/10.3390/obesities5040084 - 27 Nov 2025
Abstract
Background and Objectives: Previous research shows that stress can alter eating habits. This study analyzed the impact of COVID-19 confinement on eating behaviors and weight in Spanish adults, as well as related factors. Methods: A total of 2834 adults (69.3% women, Mean age:
[...] Read more.
Background and Objectives: Previous research shows that stress can alter eating habits. This study analyzed the impact of COVID-19 confinement on eating behaviors and weight in Spanish adults, as well as related factors. Methods: A total of 2834 adults (69.3% women, Mean age: 41.36) completed an online questionnaire assessing eating habits, weight, and sociodemographic variables. Results: Strict lockdown in Spain was linked to a general worsening of eating habits, particularly increased food intake and weight gain. Risk factors for less healthy eating and weight gain included being female (p < 0.001), under 35 years old (p < 0.001), overweight or obese (p < 0.001), caring for minors (p = 0.002), and experiencing nervousness or anxiety (p < 0.001). Conversely, maintaining pre-confinement eating habits and weight was more common among men (p < 0.001), individuals aged 50 years or older (p < 0.001), those with normal or underweight BMI (p < 0.001), those working outside the home (p < 0.013), and those without minors in their care (p = 0.001). Conclusions: Prolonged lockdowns associated with high stress may negatively influence diet and weight. Prevention strategies should therefore promote healthy eating during such periods, particularly targeting groups at higher risk of worsening habits and weight gain.
Full article
Open AccessArticle
Effects of Obesity Treatment Type on Emotional Eating and Weight/Waist Circumference Changes in Women Through Interrelations of Induced Self-Regulation and Self-Efficacy
by
James J. Annesi and Steven B. Machek
Obesities 2025, 5(4), 83; https://doi.org/10.3390/obesities5040083 - 22 Nov 2025
Abstract
►▼
Show Figures
Obesity is a medical issue of increasing prevalence, with emotional eating being a key contributor to the problem, particularly in women. Theory and previous research suggest that obesity treatment participants’ self-regulatory abilities and self-efficacy to control eating are viable targets for improving emotional
[...] Read more.
Obesity is a medical issue of increasing prevalence, with emotional eating being a key contributor to the problem, particularly in women. Theory and previous research suggest that obesity treatment participants’ self-regulatory abilities and self-efficacy to control eating are viable targets for improving emotional eating and related impacts on an unhealthy body composition. However, an improved understanding of interrelations between self-regulatory and self-efficacy changes are needed to inform behavioral treatments, which have had mostly negligible effects beyond the short term. Women were randomized into 6-month community-based obesity treatment conditions of (a) cognitive–behavioral methods with attention on emotional eating (n = 48), (b) cognitive–behavioral methods with no specific attention on emotional eating (n = 48), and (c) weight loss education (n = 50). Study-related improvements were greater in the merged cognitive–behavioral condition (n = 96; aggregated because the two corresponding treatment conditions demonstrated no significant differences). Using data aggregated across all study participants, early change in eating-related self-regulation was a significantly stronger predictor of longer-term change in eating-related self-efficacy than vice versa. Consistent with that finding, paths from treatment condition→change in self-regulation→change in self-efficacy→change in emotional eating over both 6 and 12 months were significant but not where change in self-efficacy was, instead, entered as a predictor of self-regulation change. Lessened emotional eating was significantly associated with concurrent reductions in weight and waist circumference. Consistent with self-regulation theory, findings suggest benefits for cognitive–behavioral obesity treatments over the more common education-based approaches, as well as benefits for first focusing on self-regulation that could empower increases in self-efficacy. Consistent with self-efficacy theory, such induced increases might promote favorable behavioral changes.
Full article

Figure 1
Open AccessArticle
Effect of D-β-Hydroxybutyric Acid on Body Fat in Japanese Adults: A Randomized, Double-Blind, Placebo-Controlled Study
by
Shohei Katsuya, Yoshikazu Kawata, Jun Kawamura, Tsuyoshi Goto, Tsuyoshi Takara and Jun Tsubota
Obesities 2025, 5(4), 82; https://doi.org/10.3390/obesities5040082 - 14 Nov 2025
Abstract
Ketone metabolism is currently being spotlighted for its health benefits. Strict dietary carbohydrate restriction is required to increase plasma ketone levels, which can be achieved with D-β-hydroxybutyric acid (D-BHB) supplementation as well. Although 2.9 g/day of D-BHB may reduce body fat without dieting
[...] Read more.
Ketone metabolism is currently being spotlighted for its health benefits. Strict dietary carbohydrate restriction is required to increase plasma ketone levels, which can be achieved with D-β-hydroxybutyric acid (D-BHB) supplementation as well. Although 2.9 g/day of D-BHB may reduce body fat without dieting or exercise interventions, the lower effective intake limit of exogenous D-BHB remains unknown. In this randomized, double-blind, placebo-controlled study (UMIN000054231), we aimed to assess the safety and fat-reduction effects of a 12-week intake of D-BHB in healthy Japanese adults (low-dose [1.5 g/day, n = 33], normal-dose [2.9 g/day, n = 33], and placebo [n = 34] groups). Blood samples were collected pre- and post-intervention. Participants’ blood chemistry, anthropometric, and body composition parameters were investigated. The low-dose group had a lower visceral fat area and body mass index (BMI) and higher plasma ketone levels than the placebo group. The normal-dose group had a significantly lower visceral fat area than the placebo group. Significant between-group (normal-dose vs. placebo) differences were observed in body weight, BMI, body fat percentage, fat mass, and plasma ketone levels. Participants reported no D-BHB-related adverse effects or discomfort. In conclusion, 1.5 or 2.9 g/day of D-BHB may reduce body fat without dieting or exercise interventions.
Full article
(This article belongs to the Special Issue The Impact of Food Compounds on Obesity Mechanisms)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Evaluation of Adiponectin as a Metabolic Risk Indicator in the Panamanian Population
by
Orlando Serrano Garrido, Xenia Hernandez Adames, Ivonne Torres-Atencio, Ana Espinosa De Ycaza, Maria Fabiana Piran Arce, Ana Tejada Espinosa and Griselda Arteaga
Obesities 2025, 5(4), 81; https://doi.org/10.3390/obesities5040081 - 14 Nov 2025
Abstract
►▼
Show Figures
Adiponectin, an adipokine secreted by adipocytes with anti-inflammatory and insulin-sensitizing properties, circulates in several isoforms, of which total and high-molecular-weight (HMW) adiponectin are the most physiologically relevant. While adiponectin has been inversely associated with obesity and metabolic syndrome (MetS), evidence from Latin American
[...] Read more.
Adiponectin, an adipokine secreted by adipocytes with anti-inflammatory and insulin-sensitizing properties, circulates in several isoforms, of which total and high-molecular-weight (HMW) adiponectin are the most physiologically relevant. While adiponectin has been inversely associated with obesity and metabolic syndrome (MetS), evidence from Latin American populations remains scarce. To explore its role in this context, we conducted a case–control study in 310 Panamanian adults, including 77 individuals with MetS and 233 controls, diagnosed according to the Latin American Diabetes Association (ALAD) criteria. Serum adiponectin, lipid profile, glucose, HbA1c, and body composition were evaluated, with adiponectin quantified by chemiluminescent immunoassay (CLIA). Correlations with metabolic parameters were analyzed using GraphPad Prism 10.5. Participants with MetS exhibited significantly lower adiponectin concentrations compared with controls (7.75 ± 2.58 µg/mL vs. 9.53 ± 3.31 µg/mL, p = 0.0030). Adiponectin levels were significantly lower in males than in females (p = 0.0083) and showed inverse correlations with visceral fat (r = −0.26, p < 0.001), triglycerides (r = −0.25, p = 0.0062), insulin (r = −0.31, p < 0.0001), and HbA1c (r = −0.11, p = 0.046). Conversely, a positive association was observed with HDL cholesterol (r = 0.37, p < 0.0001). Individuals with HbA1c ≥ 6.5% or insulin ≥ 15 µU/mL exhibited markedly reduced adiponectin concentrations (p = 0.0006 and p < 0.0001, respectively). The ROC analysis yielded an AUC of 0.69, indicating a moderate discriminatory ability of adiponectin for identifying MetS in this population. These findings confirm that adiponectin is inversely associated with several metabolic risk factors, supporting its potential utility as a biomarker for early detection and risk stratification of metabolic syndrome in the Panamanian population.
Full article

Figure 1
Open AccessArticle
Prevalence of Arterial Hypertension and Associated Factors Among Female Workers in a Large Company in Southern Brazil
by
Yasmin Garcia Marinho, Harrison Canabarro Arruda, Ingrid Stähler Kohl, Janaína Cristina da Silva, Anderson Garcez and Maria Teresa Anselmo Olinto
Obesities 2025, 5(4), 80; https://doi.org/10.3390/obesities5040080 - 13 Nov 2025
Abstract
►▼
Show Figures
Background/Objectives: Systemic arterial hypertension (SAH) is a multifactorial condition strongly associated with increased morbidity and mortality. This study aimed to investigate the prevalence of SAH and its associated factors among female workers in a large company in Southern Brazil. Methods: A cross-sectional study
[...] Read more.
Background/Objectives: Systemic arterial hypertension (SAH) is a multifactorial condition strongly associated with increased morbidity and mortality. This study aimed to investigate the prevalence of SAH and its associated factors among female workers in a large company in Southern Brazil. Methods: A cross-sectional study was conducted with a sample of 451 female workers aged 18 years or older. Blood pressure (BP) was measured using an automated digital upper-arm device. SAH was defined as systolic BP and/or diastolic BP ≥ 140/90 mmHg or the use of antihypertensive medications. Prevalence ratios were estimated using Poisson regression with robust variance. Results: The mean age of the sample was 35 ± 10 years. The prevalence of SAH was 27.7% (95% CI: 23.6–31.9). Among workers with obesity (BMI ≥ 30 kg/m2), the prevalence of SAH reached 42.8%. In multivariable-adjusted models, workers aged ≥41 years had a 48% higher probability of having SAH (PR = 1.48; 95% CI: 1.01–2.18) compared with younger women (18–30 years). Conversely, a 52% lower probability of SAH was observed among workers with higher monthly per capita income (>2 minimum wages) compared with those earning <1 minimum wage (PR = 0.48; 95% CI: 0.28–0.80). Obesity was associated with an 85% increased probability of SAH (PR = 1.85; 95% CI: 1.30–2.47). Conclusions: The findings of this study revealed that SAH is prevalent in this specific population of female workers, particularly among older women and those with obesity.
Full article

Figure 1
Open AccessReview
Lifestyle Interventions for the Treatment of Obesity in Workers: An Integrative Review
by
Marcia Cristina Almeida Magalhães Oliveira, Julia Passo Machado Neto Viana, Sergio de Queiroz Braga and Magno Merces Weyll Pimentel
Obesities 2025, 5(4), 79; https://doi.org/10.3390/obesities5040079 - 11 Nov 2025
Abstract
Background: Obesity is a multifactorial disease with significant physical, psychological, and economic impacts on individuals and society. Workers are particularly vulnerable, as obesity is associated with reduced productivity, absenteeism, and premature mortality. Lifestyle interventions combining dietary, physical activity, and behavioural strategies have been
[...] Read more.
Background: Obesity is a multifactorial disease with significant physical, psychological, and economic impacts on individuals and society. Workers are particularly vulnerable, as obesity is associated with reduced productivity, absenteeism, and premature mortality. Lifestyle interventions combining dietary, physical activity, and behavioural strategies have been investigated as therapeutic approaches in this population. Objective: We aimed to conduct an integrative review assessing the effectiveness of workplace-based obesity treatment models involving dietary interventions, physical activity, and behavioural change. Methods: A search was conducted in PubMed for studies published between 2006 and 2024, with no language restrictions. Eligible studies included experimental or quasi-experimental longitudinal designs involving adult workers. After screening 95 articles, 18 were evaluated in full, and 8 met all inclusion criteria. Data extraction covered study design, intervention type, comparators, outcomes, and methodological quality, assessed using the Newcastle–Ottawa Scale. Results: Half of the included studies reported no significant reduction in body mass index after 6 or 12 months, while the others showed only modest decreases. Nevertheless, all interventions demonstrated improvements in dietary habits (reduced sugar-sweetened beverage intake, increased fruit, vegetable, and fibre consumption), physical activity (increased walking, reduced sedentary behaviour), and behavioural domains (adherence to healthy routines, self-monitoring, and family or employer support). Conclusions: Lifestyle-based workplace interventions for obesity show limited long-term effectiveness in weight reduction but promote healthier lifestyle habits, cardiometabolic health, and more supportive work environments. Future research should include diverse socioeconomic settings, particularly in developing countries, and apply robust designs, longer follow-ups, and innovative strategies to enhance adherence and outcomes.
Full article
(This article belongs to the Special Issue Obesity and Its Comorbidities: Prevention and Therapy)
►▼
Show Figures

Figure 1
Open AccessArticle
Stages of Change and Variation in Weight-Related Behaviors and Physical Activity: The Role of Motivation and Self-Efficacy in Adolescents
by
María Marentes-Castillo, Isabel Castillo, Inés Tomás and Octavio Álvarez
Obesities 2025, 5(4), 78; https://doi.org/10.3390/obesities5040078 - 30 Oct 2025
Abstract
The stages of change have been identified as a valuable framework for understanding the transition toward a healthy lifestyle. It is also important to recognize change through other psychosocial variables, such as motivation and self-efficacy. The objective of this study was to explore
[...] Read more.
The stages of change have been identified as a valuable framework for understanding the transition toward a healthy lifestyle. It is also important to recognize change through other psychosocial variables, such as motivation and self-efficacy. The objective of this study was to explore weight control over the course of an academic year (nine months) through three behaviors: the stage of change toward weight control (pre-contemplation, contemplation, preparation, action, maintenance), healthy and unhealthy eating behaviors for weight control, and the frequency of physical activity (PA). Furthermore, we wanted to ascertain whether the three distinct types of motivation (autonomous, controlled, and amotivation) and self-efficacy could account for fluctuations in weight control over time. The sample consisted of 303 adolescents (205 female and 98 male) between the ages of 15 and 23 (M = 17.26; SD = 1.65). Chi-square, t-test, and multiple linear stepwise regression analysis were employed. The results indicated that a higher proportion of adolescents were in the precontemplation and action stages at Time 2. Concurrently, an increase in the frequency of moderate-to-vigorous PA and an increase in healthy and unhealthy behaviors were observed during the school period. The present study posits that autonomous motivation, controlled motivation, and self-efficacy can explain healthy eating behaviors for weight control and the frequency of moderate-to-vigorous PA, while only controlled motivation explains unhealthy eating behaviors for weight control. The conclusion of the study points out that healthy behaviors can change over time due to individual regulation of motivation and increased self-perception of efficacy in one’s own abilities to perform a specific action to control weight.
Full article
Open AccessArticle
Impact of a Vegetarian Diet upon Premature Aging, Metabolic Syndrome, and Health
by
Oana Codruta Bacean Miloicov, Georgiana Patricia Sitaru, Gabriel Cristian Vacaru, Ciprian Ioan Borca, Mihaela Cristina Simbrac, Roxana Folescu, Daniela Gurgus and Mirabela Anca Ursadan
Obesities 2025, 5(4), 77; https://doi.org/10.3390/obesities5040077 - 27 Oct 2025
Abstract
►▼
Show Figures
Objective: This study aimed to evaluate the impact of an exclusively vegetarian diet, combined with physical activity and lifestyle interventions, on metabolic parameters in patients with metabolic syndrome, with a focus on preventing premature aging and improving overall health status. Materials and Methods:
[...] Read more.
Objective: This study aimed to evaluate the impact of an exclusively vegetarian diet, combined with physical activity and lifestyle interventions, on metabolic parameters in patients with metabolic syndrome, with a focus on preventing premature aging and improving overall health status. Materials and Methods: A total of 150 participants (82 females, 68 males; aged 36–80 years, with a mean age of 61.45 years) diagnosed with metabolic syndrome were enrolled. Participants followed an exclusively vegetarian diet (≈2100 kcal/day; 65% carbohydrates, 23% lipids, 15% proteins, 52.4 g dietary fiber, and 0 mg cholesterol) along with a structured lifestyle program that included physical activity (2.5 h/day, intensity 2–6 METs), psychological counseling, smoking cessation support, weight and blood pressure management, hydrotherapy, massage, phytotherapy, and stress-reduction sessions. Baseline and post-intervention assessments were performed to measure total cholesterol, LDL, HDL, triglycerides, glycemia, BMI, and blood pressure. Results: After 10 days of intervention, significant improvements were observed across all measured parameters: total cholesterol decreased by 41.21 mg/dL (−19.54%), triglycerides decreased by 72.86 mg/dL (−34.9%), LDL cholesterol decreased by 26.24 mg/dL (−19.71%), fasting glycemia decreased by 30.4 mg/dL (−21.61%), BMI decreased by 3%, systolic blood pressure decreased by 10.82 mmHg, and diastolic blood pressure decreased by 6.44 mmHg. Conclusions: Our findings demonstrate that a structured lifestyle intervention, centered on a vegetarian diet and physical activity, has a significant beneficial effect on metabolic health. This approach improves cardiovascular risk factors, glycemic control, and body composition, and may play a preventive role against premature aging.
Full article
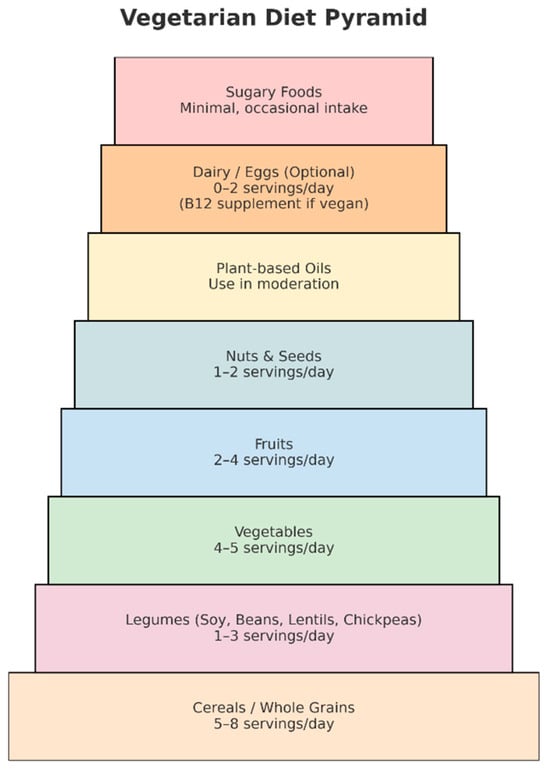
Figure 1
Open AccessArticle
The Prevalence and Correlates of Vitamin D Deficiency and Overweight/Obesity of School-Age Children in Colombia–Findings on the Double Burden of Malnutrition from Nationally-Representative Data
by
Edwin Guevara-Romero, Victor Florez-Garcia, Faith Ogungbe, Amy Harley and Alice Yan
Obesities 2025, 5(4), 76; https://doi.org/10.3390/obesities5040076 - 24 Oct 2025
Abstract
The double burden of malnutrition (DBM)—the coexistence of overweight/obesity and micronutrient deficiency—is an emerging public health concern among school-aged children. Using data from 6063 participants in Colombia’s 2015 National Survey of Nutritional Status (ENSIN), this study estimated DBM prevalence and identified factors associated
[...] Read more.
The double burden of malnutrition (DBM)—the coexistence of overweight/obesity and micronutrient deficiency—is an emerging public health concern among school-aged children. Using data from 6063 participants in Colombia’s 2015 National Survey of Nutritional Status (ENSIN), this study estimated DBM prevalence and identified factors associated with its occurrence among children aged 5–12 years. DBM was defined as concurrent overweight/obesity (BMI-for-age z-score > 1) and vitamin D deficiency, applying thresholds of <30, <37.5, and <50 nmol/L. The prevalence of DBM ranged from 0.7% to 6.9%. Firth’s penalized logistic regression models were conducted separately for (1) overweight/obese combined, (2) overweight-only, and (3) obesity-only groups. For DBM1, insufficient physical activity was linked to higher odds across all three models. For DBM2, smaller household size and higher maternal education were associated with greater odds in the combined model. Living in large urban areas was related to lower odds compared with major metropolitan areas, a pattern also observed in the overweight-only model. For DBM3, children from the second wealth quartile (Q2) showed higher odds than those from the poorest (Q1), with a similar pattern in the overweight-only analysis. Stricter DBM definitions tended to capture behavioral and household characteristics, whereas broader thresholds reflected structural and contextual conditions. Despite its relatively low prevalence, DBM remains a relevant public health issue among Colombian schoolchildren.
Full article
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Behavioral Sciences, Children, Healthcare, IJERPH, JFMK, Obesities
The Effect of Physical Activity on the Population's Health
Topic Editors: Stefania Paduano, Federica ValerianiDeadline: 31 August 2026
Topic in
Geriatrics, IJMS, Life, Sports, Neurology International, Obesities
Exercise and Human Aging: Physiological and Psychological Functions
Topic Editors: Samuel Da Silva Aguiar, Ismael Perez-SuarezDeadline: 20 September 2026
Topic in
Nutrients, Metabolites, Healthcare, Children, Obesities, Life
Non-Communicable Diseases Silent Killer: Metabolic and Obesity Risks of Sedentary Behaviors
Topic Editors: Kotsedi Daniel Monyeki, Machoene Derrick SekgalaDeadline: 30 September 2026
Topic in
Dietetics, Nutrients, Obesities, Diseases, IJMS, Metabolites
Dietary Habits in Liver Health and Disease: Preclinical and Clinical Studies
Topic Editors: Evelyn Nunes Goulart Da Silva Pereira, Rosane Harter Griep, Anissa DaliryDeadline: 31 December 2026

Special Issues
Special Issue in
Obesities
How to Prevent Obesity and Inflammatory Disease 2025
Guest Editor: Sara BaldassanoDeadline: 31 December 2025
Special Issue in
Obesities
Obesity in the 21st Century: Public Health Perspectives and Population Solutions
Guest Editors: Ritesh Chimoriya, Kritika RanaDeadline: 31 March 2026
Special Issue in
Obesities
Novel Technology-Based Exercise for Childhood Obesity Prevention
Guest Editors: Alessandra Amato, Sara BaldassanoDeadline: 31 May 2026
Special Issue in
Obesities
The Impact of Food Compounds on Obesity Mechanisms
Guest Editor: Nobuyuki TakahashiDeadline: 30 June 2026