-
 Burden of Infected Diabetic Foot Ulcers on Hospital Admissions and Costs in a Third-Level Center
Burden of Infected Diabetic Foot Ulcers on Hospital Admissions and Costs in a Third-Level Center -
 Exploration of Foundational Models for Blood Glucose Forecasting in Type-1 Diabetes Pediatric Patients
Exploration of Foundational Models for Blood Glucose Forecasting in Type-1 Diabetes Pediatric Patients -
 Lifestyle Medicine Case Manager Nurses for Type Two Diabetes Patients: An Overview of a Job Description Framework—A Narrative Review
Lifestyle Medicine Case Manager Nurses for Type Two Diabetes Patients: An Overview of a Job Description Framework—A Narrative Review -
 The Main Risk Factors in Type 2 Diabetes for Cognitive Dysfunction, Depression, and Psychosocial Problems: A Systematic Review
The Main Risk Factors in Type 2 Diabetes for Cognitive Dysfunction, Depression, and Psychosocial Problems: A Systematic Review -
 Exosome-Derived microRNAs: Bridging the Gap Between Obesity and Type 2 Diabetes in Diagnosis and Treatment
Exosome-Derived microRNAs: Bridging the Gap Between Obesity and Type 2 Diabetes in Diagnosis and Treatment
Journal Description
Diabetology
Diabetology
is an international, peer-reviewed, open access journal on diabetes research published monthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, EBSCO, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 26.3 days after submission; acceptance to publication is undertaken in 5.8 days (median values for papers published in this journal in the first half of 2025).
- Journal Rank: CiteScore - Q2 (Medicine (miscellaneous))
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
2.2 (2024);
5-Year Impact Factor:
2.5 (2024)
Latest Articles
Glucagon-like Peptide-1 Receptor Agonists and Survival in Advanced Chronic Kidney Disease and Type 2 Diabetes
Diabetology 2025, 6(12), 161; https://doi.org/10.3390/diabetology6120161 - 9 Dec 2025
Abstract
►
Show Figures
Background/Objectives: In populations with type 2 diabetes mellitus (T2DM), it is unknown whether the survival benefits of glucagon-like peptide-1 receptor agonists (GLP-1 RA) differ by estimated glomerular filtration rate (eGFR). To address this question and in the absence of definitive randomized controlled trials,
[...] Read more.
Background/Objectives: In populations with type 2 diabetes mellitus (T2DM), it is unknown whether the survival benefits of glucagon-like peptide-1 receptor agonists (GLP-1 RA) differ by estimated glomerular filtration rate (eGFR). To address this question and in the absence of definitive randomized controlled trials, we performed a retrospective observational study of US Veterans with T2DM to evaluate mortality hazard ratios associated with GLP-1 RA use at different eGFR levels. Methods: This administrative claims-based cohort included 1,188,052 U.S. Veterans with T2DM as of 1 January 2020. Initiation of GLP-1 RA was treated as a time-dependent variable and vital status of Veterans was followed until 31 December 2023. Results: A total of 31,676 Veterans met inclusion criteria. Over the study timeframe, 6.1% initiated treatment with GLP-1 RA and 57.7% died. Older age and eGFR < 15 mL/min/1.73 m2 were associated with a decreased likelihood of GLP-1 RA initiation. In contrast, younger age and lower comorbidity burden were associated with decreased mortality, a finding that persisted even after adjustment for several baseline covariates. Conclusions: Among those with T2DM and eGFR < 25 mL/min/1.73 m2, initiation of GLP-1 RA was associated with improved survival. This association remained significant with decreasing levels of kidney function, as well as among those receiving kidney replacement therapy (KRT). In conclusion, longer survival was observed both in participants on KRT and in those with eGFR 15–24 mL/min/1.73 m2 not on KRT, but these findings were not observed among those with eGFR ≤ 15 mL/min/1.73 m2.
Full article
Open AccessCorrection
Correction: del Río Pascual et al. Therapeutic Adherence and Glycemic Control in the Population with Diabetes in Ceuta (Spain), a Multicultural City: A Cross-Sectional Study. Diabetology 2025, 6, 100
by
Brieba del Río Pascual, Antolí Jover Ana María, Vázquez Lara Juana María, Ruger Navarrete Azahara, Vázquez Lara María Dolores, Palomo Gómez Rocio, Artero García Alejandro, Rodríguez Díaz Luciano and Fernández Carrasco Francisco Javier
Diabetology 2025, 6(12), 160; https://doi.org/10.3390/diabetology6120160 - 9 Dec 2025
Abstract
Text Correction [...]
Full article
Open AccessArticle
Knowledge and Self-Efficacy as Key Determinants of Transition Readiness in Adolescents with Type 1 Diabetes: Insights from Adolescents, Parents, and Clinicians
by
Ailsa Marshall, Nghi H. Bui, Ann Nillsen, Lena Lim, Gillian Burke, Amelia Christie, Sandeep Kaur, Karina Pearce, Jack Ho, Sharon Youde, Kim A. Ramjan, Amy Wanaguru, Ohn Nyunt, Louise Baczkowski, Debra Waite, Sally Duke, Darshika Christie David and Shihab Hameed
Diabetology 2025, 6(12), 159; https://doi.org/10.3390/diabetology6120159 - 8 Dec 2025
Abstract
Aim: Assess transition readiness of adolescents with Type 1 Diabetes (T1D) from adolescent, parental, and clinician perspectives. Methods: Cross-sectional study (n = 36, 20 Male/16 Female, 16–18 years, June 2023–June 2024, metropolitan paediatric centre). Adolescents had diabetes knowledge, self-efficacy, and diabetes distress measured.
[...] Read more.
Aim: Assess transition readiness of adolescents with Type 1 Diabetes (T1D) from adolescent, parental, and clinician perspectives. Methods: Cross-sectional study (n = 36, 20 Male/16 Female, 16–18 years, June 2023–June 2024, metropolitan paediatric centre). Adolescents had diabetes knowledge, self-efficacy, and diabetes distress measured. Parents had an assessment of knowledge, diabetes-related distress, and estimated the adolescent’s self-efficacy. Clinicians estimated adolescent self-efficacy. Results: Median HbA1c was 7.4% (IQR 6.6–8.4). One adolescent met the guidelines for multidisciplinary team (MDT) appointments. Paired sample t-tests showed that adolescents’ knowledge was comparable to parent levels (t(24) = −1.69, p = 0.10). Adolescents’ knowledge was strongly associated with higher self-efficacy (r = 0.80 p < 0.001). Higher adolescent self-efficacy was associated with lower adolescent distress (r = −0.368, p = 0.03). Adolescent distress was lower than parent distress (t(24) = −3.13, p = 0.005). Although adolescent self-efficacy was strongly correlated with parent and clinician evaluation (r = 0.76, p < 0.001; r = 0.80, p < 0.001), adolescents reported higher self-efficacy than estimates by parents (t(24) = 4.76, p < 0.001) or clinicians (t(24) = 8.39, p < 0.001). Parent knowledge was moderately correlated with adolescent self-efficacy (r = 0.62, p = 0.001). Conclusions: Diabetes knowledge may confer greater self-efficacy and reduce diabetes distress in adolescents. Distress levels are higher in parents than in adolescents. Engagement with MDT is poor. Transition efforts should focus on parents and adolescents while increasing engagement with MDT.
Full article
(This article belongs to the Special Issue Healthy Habits of Diabetes: Prevention, Intervention and Management Strategies)
Open AccessArticle
Management of Type 2 and Post-Transplant Diabetes in Kidney Transplant Recipients: A Single-Center Clinical Experience with GLP-1 Receptor Agonists and SGLT-2 Inhibitors
by
Ricardo E. T. Navarrete, Joana C. Freitas, Isabel Fonseca, Ana Cunha, Joao Roberto Sa and La Salete Martins
Diabetology 2025, 6(12), 158; https://doi.org/10.3390/diabetology6120158 - 5 Dec 2025
Abstract
►▼
Show Figures
Objective: The aim was to characterize the real-world use of GLP-1 receptor agonists (GLP-1 RAs) and/or SGLT2 inhibitors in kidney transplant recipients (KTRs) with diabetes and to compare the clinical management, safety, and effectiveness between patients with type 2 diabetes mellitus (T2DM) and
[...] Read more.
Objective: The aim was to characterize the real-world use of GLP-1 receptor agonists (GLP-1 RAs) and/or SGLT2 inhibitors in kidney transplant recipients (KTRs) with diabetes and to compare the clinical management, safety, and effectiveness between patients with type 2 diabetes mellitus (T2DM) and post-transplant diabetes mellitus (PTDM). Methods: This retrospective longitudinal cohort study included 141 adult KTRs (T2DM: 52; PTDM: 89) who initiated GLP-1 RA and/or SGLT2 inhibitor (SGLT2i) therapy between August 2013 and April 2024. Metabolic control, medication use, and safety outcomes were assessed from baseline to end follow-up, with a mean treatment exposure of 2.4 years. Results: Overall, 69% were treated with an SGLT2i and 59% with a GLP-1 RA; because the groups were not mutually exclusive, 28% received both agents. Treatment was associated with significant reductions in body weight (−3.38 kg; p < 0.001) and BMI (−1.28 kg/m2; p < 0.001) in both subgroups. HbA1c showed a non-significant overall decline (−0.31%; p = 0.21), with a greater reduction in the T2DM subgroup (−0.50%; p < 0.01). Significant improvements were also observed in lipid profile and blood pressure. Renal allograft function remained stable in both groups. The overall safety profile of the therapies was favorable, with mild urinary tract infections (18%) and manageable nausea (6%) reported in the entire cohort. No episodes of acute rejection or severe hypoglycemia occurred during the study period. Conclusions: In real-world practice, GLP-1 RAs and SGLT2is were associated with improved cardiometabolic parameters and stable renal function in KTRs, with a manageable safety profile. Similar effectiveness and safety across T2DM and PTDM support the use of these agents throughout the spectrum of diabetes in transplant recipients.
Full article
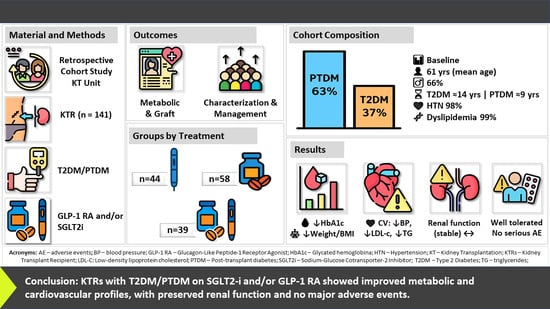
Graphical abstract
Open AccessArticle
Implementing the Physical Activity Vital Sign in a Pediatric Diabetes Center
by
Margaret M. McCarthy, Jeniece Ilkowitz, Jinyu Hu and Mary Pat Gallagher
Diabetology 2025, 6(12), 157; https://doi.org/10.3390/diabetology6120157 - 4 Dec 2025
Abstract
►▼
Show Figures
Aims: The purpose of this quality improvement (QI) initiative at a pediatric diabetes center was to integrate physical activity (PA) assessment into routine clinical care. This project had two aims: (1) to collect self-reported PA in youth and young adults with type 1
[...] Read more.
Aims: The purpose of this quality improvement (QI) initiative at a pediatric diabetes center was to integrate physical activity (PA) assessment into routine clinical care. This project had two aims: (1) to collect self-reported PA in youth and young adults with type 1 diabetes (T1D) and (2) to analyze levels of PA (none, some PA, at-goal PA, and at-goal vs. not-at-goal PA) and their relationship with demographics and clinical outcomes. PA goals were 60 min/day for youth and 150 min/week of moderate-to-vigorous aerobic PA for young adults. Methods: During clinical visits, a pediatric diabetes center used a three-question Physical Activity Vital Sign (PAVS) to assess and document PA, which was recorded as total minutes per week with intensity (light, moderate, and vigorous). We analyzed PAVS data from January 2020 to July 2022. Clinical variables were compared across the levels of PA. Results: This was a sample of 304 youth and young adults living with T1D: 87 young adults (29%) and 217 youth (71%), with a mean age of 14.2 (4.8) years. Half had an HbA1c between 7% (53.01 mmol/mol) and 9% (74.87 mmol/mol), and 56% used both continuous glucose monitoring and an insulin pump. Overall, 78% of the sample did not meet PA goals. LDL and blood pressure were significantly different across the two groups of PA achievement (not at goal vs. at goal). Only LDL levels remained significantly different across the three groups (none, some PA, and at-goal PA). Conclusions: Implementing PA assessment is feasible in a pediatric diabetes center. Next steps may include incorporating exercise prescriptions as part of routine clinical care.
Full article

Graphical abstract
Open AccessArticle
Glycemic Variability Before and After Hypoglycemia Across Different Timeframes in Type 1 Diabetes with and Without Automated Insulin Delivery
by
Ahtsham Zafar, Abiodun A. Solanke, Dana M. Lewis and Arsalan Shahid
Diabetology 2025, 6(12), 156; https://doi.org/10.3390/diabetology6120156 - 4 Dec 2025
Abstract
►▼
Show Figures
Background: Managing Type 1 diabetes (T1D) aims to optimize glucose within the target range while minimizing hyperglycemia and hypoglycemia, yet exercise complicates glycemic outcomes. Despite advances, evidence is limited on how exercise relates to glycemic variability (GV) and hypoglycemia in automated insulin delivery
[...] Read more.
Background: Managing Type 1 diabetes (T1D) aims to optimize glucose within the target range while minimizing hyperglycemia and hypoglycemia, yet exercise complicates glycemic outcomes. Despite advances, evidence is limited on how exercise relates to glycemic variability (GV) and hypoglycemia in automated insulin delivery (AID) and non-AID users, including evidence on GV’s temporal course before and after hypoglycemia, especially following long episodes. Objective: We aimed to characterize −48 to +48 h CGM trajectories around hypoglycemia, compare commercial AID and non-AID users, and assess modifiers (exercise, episode duration/severity, gender). Methods: This study analyzes the Type 1 Diabetes and Exercise Initiative (T1DEXI) dataset, assessing GV, hypoglycemia, gender, and exercise interactions in AID (n = 222) and non-AID (n = 276) users. The study examined patterns of glycemic metrics, including time below range (TBR) and glycemic variability surrounding hypoglycemia events, focusing on the 48 h before and after these events. We further assessed the impact of different hypoglycemia levels (41–50 mg/dL, 51–60 mg/dL, and 61–70 mg/dL) on post-event glucose stability. Results: Glycemic variability increased before and after hypoglycemia for up to 48 h in both AID and non-AID users, with statistically significant differences in GV metrics. TBR elevation persisted across all groups, peaking around hypoglycemic episodes. Notably, females using AID achieved significantly improved glucose stability compared to non-AID females, which is a larger within-group difference than that observed in males. Individual-level AID analyses revealed that long-duration hypoglycemia episodes (>40 min) resulted in prolonged TBR elevation, suggesting a slower recovery period despite AID intervention. Conclusions: GV trends may aid in predicting hypoglycemia over extended time periods. Integrating GV patterns into AID systems could improve glucose stability and mitigate hypoglycemia cycles, especially with the possible evaluation of hypoglycemia duration. Future research should explore hormonal influences (e.g., menstrual cycle effects) and inter-individual variability for optimized individual diabetes management.
Full article

Figure 1
Open AccessEssay
Advancing Diabetes Technology Implementation Through Team-Based Care
by
Jordin Millward and Elaine Nguyen
Diabetology 2025, 6(12), 155; https://doi.org/10.3390/diabetology6120155 - 4 Dec 2025
Abstract
►▼
Show Figures
Introduction: Advancements in diabetes technology have transformed diabetes management, yet technology implementation remains inconsistent due to barriers at both the clinician and patient levels. Team-based collaborative care offers a promising strategy to bridge these gaps. Framework: The Practical, Robust Implementation and Sustainability Model
[...] Read more.
Introduction: Advancements in diabetes technology have transformed diabetes management, yet technology implementation remains inconsistent due to barriers at both the clinician and patient levels. Team-based collaborative care offers a promising strategy to bridge these gaps. Framework: The Practical, Robust Implementation and Sustainability Model (PRISM), which incorporates the reach, effectiveness, adoption, implementation, and maintenance (RE-AIM) framework, was applied to identify clinician and patient-level barriers to technology implementation and guide development of team-based strategies for improvement. Application of this framework is illustrated through a rural primary care clinic implementing a remote patient monitoring program. Results: Analysis across RE-AIM domains identified team-based, interprofessional strategies for enhancing technology implementation and sustainability. Recommended strategies include structured onboarding and digital literacy support for both patients and clinicians, clear delineation of team roles and intentional integration of workflows, continuous quality improvement through feedback and huddles, and sustained organizational and policy support that ensures security, reimbursement, and equitable access. Conclusions: Application of the PRISM framework to improve diabetes technology implementation allows for translation of technological innovation into meaningful outcomes.
Full article

Figure 1
Open AccessArticle
The Role of Social Determinants of Health and Diabetes Self-Management on Glycemic Indices: A Cross-Sectional Analysis
by
Cherlie Magny-Normilus, Sangchoon Jeon, Jeffrey L. Schnipper, Bei Wu and Robin Whittemore
Diabetology 2025, 6(12), 154; https://doi.org/10.3390/diabetology6120154 - 2 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Type 2 diabetes (T2D) is a substantial health burden on foreign-born Haitian Americans (FBHAs) in the United States, who experience poorer health outcomes for T2D, in particular, cardiovascular disease and diabetes nephropathy. Understanding the factors that contribute to these disparities is essential.
[...] Read more.
Background/Objectives: Type 2 diabetes (T2D) is a substantial health burden on foreign-born Haitian Americans (FBHAs) in the United States, who experience poorer health outcomes for T2D, in particular, cardiovascular disease and diabetes nephropathy. Understanding the factors that contribute to these disparities is essential. The purpose of this study was to examine the association between demographic, clinical, diabetes self-management, and social determinants of health (SDoH) factors with continuous glucose monitor (CGM-derived) glycemic indices in adult FBHAs with T2D. Methods: A cross-sectional exploratory correlation study was conducted in two urban health clinics, focusing on FBHAs aged 21 or older who had T2D for at least one year. Data were analyzed using SAS 6.4, employing descriptive statistics, bivariate correlations, and multiple regression models. Results: The study included 59 participants (49.2% male; mean age = 51.7 years, SD = 9.9), with an average T2D duration of 7.7 years (SD = 6.8) and an average of 1.63 (SD = 1.30) chronic diseases. A total of 29% were overweight while 21% had obesity with a mean HbA1c of 58 mmol/mol (7.5%). A higher body weight and poorer dietary habits were associated with elevated glucose levels (standardized β ≈ 0.25 and −0.24). Greater race-related stress was correlated with greater glucose variability (β ≈ 0.46). Conclusions: These findings highlight the importance of addressing SDoH, such as race-related stress and food insecurity, to improve T2D self-management among FBHAs. Assessing and mitigating these risk factors can enhance glycemic control and health outcomes. Additionally, the findings demonstrate that CGM is feasible and acceptable for this population, showing exploratory findings and preliminary effect sizes that provide a strong basis for future, large-scale investigations.
Full article

Graphical abstract
Open AccessArticle
Visual Acuity and Beyond: Sociodemographic Determinants of Quality of Life in Diabetic Retinopathy
by
Elitsa Hristova, Lidiya Zaduryan, Gabriela Vasileva, Iliyana Petkova, Mladena Radeva and Zornitsa Zlatarova
Diabetology 2025, 6(12), 153; https://doi.org/10.3390/diabetology6120153 - 1 Dec 2025
Abstract
►▼
Show Figures
Background: Diabetic retinopathy (DR) is a leading cause of vision-related disability worldwide. Evidence on how clinical and sociodemographic factors jointly shape vision-related quality of life (VRQoL) in Eastern European settings remains limited. Methods: We conducted a cross-sectional study of 151 adults
[...] Read more.
Background: Diabetic retinopathy (DR) is a leading cause of vision-related disability worldwide. Evidence on how clinical and sociodemographic factors jointly shape vision-related quality of life (VRQoL) in Eastern European settings remains limited. Methods: We conducted a cross-sectional study of 151 adults with ophthalmologically confirmed DR attending a tertiary ophthalmology clinic in Northeastern Bulgaria (June 2023–February 2025). Best-corrected visual acuity (BCVA; decimal, better-seeing eye), glycated hemoglobin (HbA1c; ordinal categories), duration of diabetes, age, sex, DR subtype, and education were recorded. VRQoL was assessed using the NEI VFQ-25 questionnaire. Non-parametric tests were applied as appropriate; multiple linear regression identified independent predictors of NEI VFQ-25 composite scores. Results: Median age was 62 years (IQR 12.5); 53.0% were female. NEI VFQ-25 median was 77.2 (IQR 37.8). BCVA correlated positively with VRQoL (Spearman’s ρ = 0.455, p < 0.001). VRQoL differed by educational level (Kruskal–Wallis χ2 = 37.3, p < 0.001, ε2 = 0.249), but not by sex (Mann–Whitney U = 2740, p = 0.711); a trend was observed across DR subtypes (H = 5.386, p = 0.067). The multivariable model was significant (F(7, 132) = 10.64, p < 0.001; adjusted R2 = 0.336). Higher VRQoL was independently associated with better BCVA (B = 35.38, 95% CI 25.81–44.95, p < 0.001), higher educational attainment (B = −10.15, 95% CI from −13.92 to −6.38, p < 0.001; coded such that lower education predicts lower scores), and DR subtype (B = 6.63, 95% CI 1.91–11.36, p = 0.007). Age, sex, HbA1c, and diabetes duration were not significant. Conclusions: In this Bulgarian cohort, functional vision (BCVA), education, and DR subtype are the principal determinants of VRQoL, highlighting the need for patient-centered strategies that integrate clinical and social factors.
Full article

Graphical abstract
Open AccessReview
Complications and Comorbidities in Individuals >80 Years with Diabetes: A Scoping Review
by
Christian Ward-Bradley, Adam Erwin, Tunde Peto, Laura N. Cushley and Katie Curran
Diabetology 2025, 6(12), 152; https://doi.org/10.3390/diabetology6120152 - 1 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Diabetes mellitus is increasingly prevalent among adults aged over 80 years; however, this population remains substantially underrepresented in clinical research on diabetes complications. This scoping review synthesises current evidence on diabetes-related complications and comorbidities in this older age group (>80 years), reported
[...] Read more.
Background/Objectives: Diabetes mellitus is increasingly prevalent among adults aged over 80 years; however, this population remains substantially underrepresented in clinical research on diabetes complications. This scoping review synthesises current evidence on diabetes-related complications and comorbidities in this older age group (>80 years), reported prevalence, and key evidence gaps. Methods: A systematic search of MEDLINE, Embase, and Web of Science was conducted for studies published between 1992 and 2024 reporting diabetes-related complications in individuals aged ≥80 years. Two reviewers independently screened titles, abstracts, and full texts. Data were extracted and summarised using narrative synthesis, and descriptive statistics (SPSS v29) were conducted. Results: Fifty-one studies were included, comprising 17,630,083 individuals aged ≥80 years. Macrovascular complications were most frequently reported, followed by microvascular and peripheral outcomes. Hypertension was the most reported comorbidity. Macrovascular outcomes were assessed in over 17 million individuals, while microvascular complications were studied in fewer than 400,000. Only five studies focused exclusively on adults aged ≥80 years. Reporting was also limited by retrospective designs, heterogeneity in definitions, and frequent omission of key variables, including diabetes duration, HbA1c, frailty, and cognitive status. Conclusions: There is a critical mismatch between research focus and the complications most relevant to function and quality of life in older populations with diabetes. Easily measurable yet clinically impactful outcomes, such as retinopathy, neuropathy, nephropathy, and foot disease, remain under-investigated in this cohort. Standardised, age-stratified reporting that incorporates functional and geriatric domains is needed to inform person-centred care in this expanding population.
Full article

Figure 1
Open AccessArticle
Perinatal Outcomes of Type 1 and Type 2 Diabetes in Pregnancy: A 10-Year Single-Centre Cohort Study
by
Paul Lawton, Jean Lu, Ryan Endall, Jing Luo, Rebecca Foskey, Dev Kevat, Peter S. Hamblin, Joanne M. Said, Glyn Teale, Christopher J. Yates and I-Lynn Lee
Diabetology 2025, 6(12), 151; https://doi.org/10.3390/diabetology6120151 - 1 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Previous studies have examined perinatal outcomes in women with type 1 (T1DM) or type 2 diabetes (T2DM) in pregnancy compared with the general population, but few have directly assessed the impact of T1DM and T2DM on pregnancy outcomes both against each other
[...] Read more.
Background/Objectives: Previous studies have examined perinatal outcomes in women with type 1 (T1DM) or type 2 diabetes (T2DM) in pregnancy compared with the general population, but few have directly assessed the impact of T1DM and T2DM on pregnancy outcomes both against each other and the general population. The aim of this study is to compare the perinatal outcomes between women with pre-existing T1DM and T2DM in pregnancy and women without diabetes in pregnancy. Methods: This is a retrospective single-centre cohort study from January 2010 through December 2019, including 2050 singleton pregnancies with T2DM (n = 317), T1DM (n = 92) and controls (n = 1641). Results: Women with T2DM were older (T2DM vs. T1DM, 33.4 vs. 29.7 yrs, p < 0.001), had higher BMI (35.4 vs. 26.8 kg/m2, p < 0.001), and were more likely multiparous (75.4 vs. 55.4%, p < 0.001). T1DM was associated with poorer glycaemic control throughout pregnancy. Infants of mothers with T1DM had increased rates of large for gestational age (45.0 vs. 26.1%, p = 0.005) and neonatal hypoglycaemia (38.0 vs. 20.8%, p < 0.001). The risk of perinatal death was nine-fold higher for T1DM (OR 9.27, p = 0.01) and 13-fold for T2DM (OR 13.5, p < 0.001) compared to controls, with no significant difference between diabetes types. Conclusions: Women with pre-existing diabetes had poorer perinatal outcomes compared to women without diabetes. Women with T2DM compared to T1DM had a similar risk of perinatal death, despite better glycaemic control and shorter duration of diabetes.
Full article

Graphical abstract
Open AccessArticle
Metabolic Syndrome and Risk of New-Onset Type 2 Diabetes Mellitus: An Eight-Year Follow-Up Study in Southern Israel
by
Tsafnat Test, Yan Press, Tamar Freud, Ruth Kannai and Robert Satran
Diabetology 2025, 6(12), 150; https://doi.org/10.3390/diabetology6120150 - 1 Dec 2025
Abstract
►▼
Show Figures
Background: Metabolic syndrome (MetS) comprises a cluster of metabolic abnormalities that increase the risk of type 2 diabetes mellitus (T2DM) and cardiometabolic morbidity. Although widely recognized, evidence on its documentation and follow-up in primary care is limited. This study aimed to evaluate
[...] Read more.
Background: Metabolic syndrome (MetS) comprises a cluster of metabolic abnormalities that increase the risk of type 2 diabetes mellitus (T2DM) and cardiometabolic morbidity. Although widely recognized, evidence on its documentation and follow-up in primary care is limited. This study aimed to evaluate the extent of MetS documentation in electronic medical records (EMRs), examine follow-up patterns and metabolic changes over time, and assess the incidence and predictors of new-onset T2DM according to baseline MetS severity. Methods: A retrospective cohort study was conducted on 8170 adults aged 30–50 years, insured by Clalit Health Services in Southern Israel, who met ATP III criteria for MetS in 2008 and were followed through 2015. MetS severity was classified as mild (three components), moderate (four), or severe (five). Changes in metabolic indices were assessed longitudinally, and predictors of T2DM were analyzed using Kaplan–Meier survival and multivariable Cox regression models. Results: Although all participants met the diagnostic criteria, only 1.6% had a recorded MetS diagnosis. Over the eight years of follow-up, 26% developed T2DM, with incidence increasing from 21% among those with mild MetS to 49% among those with severe MetS (p < 0.0001). Fasting plasma glucose rose significantly (median +13 mg/dL, p < 0.001), BMI remained stable, and modest improvements were observed in blood pressure and lipid levels. Elevated fasting glucose (HR 2.13, p < 0.001), higher BMI (HR 1.33, p = 0.010), and lower HDL (HR 1.26, p = 0.045) independently predicted diabetes onset. Conclusions: MetS remains markedly under-documented and insufficiently integrated into primary care follow-up. Despite regular clinical follow-up, improvements in metabolic indices were limited. These findings highlight the need for structured strategies to enhance MetS recognition and long-term management within routine practice.
Full article

Graphical abstract
Open AccessArticle
Glycemic Cluster Analysis of Non-Diabetic Japanese Individuals Using the Triglyceride-Glucose Index Identifies an At-Risk Group for Incident Cardiovascular Disease Independent of Impaired Glucose Tolerance
by
Makoto Daimon, Shinji Susa, Kota Ishii, Yurika Hada and Shigeru Karasawa
Diabetology 2025, 6(12), 149; https://doi.org/10.3390/diabetology6120149 - 1 Dec 2025
Abstract
►▼
Show Figures
Background/Objective: Type 2 diabetes mellitus (T2DM) is a known risk factor for cardiovascular disease (CVD); however, not all individuals with T2DM have the same CVD risk. Traditional glycemic cluster analyses of individuals with diabetes using the homeostatic model assessment estimate of insulin resistance
[...] Read more.
Background/Objective: Type 2 diabetes mellitus (T2DM) is a known risk factor for cardiovascular disease (CVD); however, not all individuals with T2DM have the same CVD risk. Traditional glycemic cluster analyses of individuals with diabetes using the homeostatic model assessment estimate of insulin resistance (HOMA-R) as an indicator of insulin resistance have identified severe insulin-resistant diabetes as a high-risk factor for incident CVD. To extend this observation, we further classified non-diabetic individuals to identify risk clusters for incident CVD. Methods: We performed hierarchical cluster analysis of 577 non-diabetic Japanese individuals using the glycated hemoglobin level, body mass index, homeostasis model assessment estimate of β-cell function, and the triglyceride-glucose (TyG) index instead of the HOMA-R to assess incident CVD risk over up to 188 months. Results: Analysis using a multiple risk factor-adjusted Cox proportional-hazard regression model showed that in addition to impaired glucose tolerance (IGT), among the four clusters observed, a cluster labeled “low insulin secretion (Low-IS (TyG))” was a risk factor for incident CVD (hazard ratio, [95% confidence interval]: 2.77 [1.11–6.91]). Furthermore, when the participants were stratified on the basis of the presence of IGT, the Low-IS (TyG) cluster was associated with an increased risk of CVD only in the non-IGT group (3.29 [1.32–8.18]), but not in the IGT group (1.66 [0.34–8.15]). Conclusions: Glycemic clustering incorporating the TyG index identified a novel at-risk group for incident CVD among non-diabetic individuals, offering a useful tool for early CVD risk stratification beyond traditional measures of glucose tolerance.
Full article

Graphical abstract
Open AccessArticle
Diabetes Mellitus and the Increased Risk of Acute Kidney Injury Following Acute Coronary Syndrome
by
Muhammad Usman Shah, Paul Edward Squires, Claire Elizabeth Hills and Kelvin Lee
Diabetology 2025, 6(12), 148; https://doi.org/10.3390/diabetology6120148 - 1 Dec 2025
Abstract
Background/objectives: Diabetes mellitus (DM) increases susceptibility to both cardiovascular and renal complications. Acute kidney injury (AKI) in the setting of acute coronary syndrome (ACS) is a frequent manifestation of acute cardiorenal syndrome (type 1); however, the impact of diabetes on the condition remains
[...] Read more.
Background/objectives: Diabetes mellitus (DM) increases susceptibility to both cardiovascular and renal complications. Acute kidney injury (AKI) in the setting of acute coronary syndrome (ACS) is a frequent manifestation of acute cardiorenal syndrome (type 1); however, the impact of diabetes on the condition remains incompletely characterised. This study aimed to evaluate the real-world incidence, severity, and recurrence of AKI in individuals with ACS, focusing on the additional risk conferred by DM, and to assess the adequacy of post-discharge renal monitoring. Methods: We conducted a single-centre, retrospective observational study of 990 ACS admissions between July 2020 and June 2021 at the United Lincolnshire Hospitals NHS Trust. Acute kidney injury was defined using Kidney Disease Improving Global Outcomes criteria and stratified by severity. Outcome measures included incidence of AKI during admission, recurrence of AKI, and renal function monitoring within 12 months post-discharge. Results: Of 990 individuals recruited, 315 (31.8%) had DM. Overall, 14.2% individuals developed AKI during admission, being more frequently observed in those with DM (20.0% vs. 11.6%; RR 1.7, p < 0.001). Severe AKI (stage 3) was higher in those with diabetes (2.9% vs. 0.7%, p = 0.017). Recurrent AKI within 12 months occurred in 9.7%, with a higher incidence in those with DM (15.8% vs. 6.9%, p < 0.001). Post-discharge renal follow-up was performed in 88.7% of persons with AKI and similar in those with and without DM. Conclusions: Acute kidney injury is a common and serious complication of ACS, with DM substantially increasing the risk and severity of the condition during acute events and post-discharge. Despite this, individuals with DM receive similar monitoring in the post-discharge period. Improved systems for post-discharge renal monitoring and early initiation of protective therapies are required to mitigate long-term risk.
Full article
Open AccessArticle
Exploring the Relationship Between Health Biomarkers and Performance on a Novel Color Perimetry Device in Prediabetes and Type 2 Diabetes
by
Liam Burhans, Bismark Owusu-Afriyie, Christopher S. Wu, Jennyffer D. Smith, Daniel R. Coates and Wendy W. Harrison
Diabetology 2025, 6(12), 147; https://doi.org/10.3390/diabetology6120147 - 1 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Type 2 diabetes (T2DM) is a leading cause of vision loss. Functional measurements (color vision and contrast sensitivity) are sensitive to early changes in eyes even before retinopathy is present. This study evaluates a novel color perimetry device as an indicator
[...] Read more.
Background/Objectives: Type 2 diabetes (T2DM) is a leading cause of vision loss. Functional measurements (color vision and contrast sensitivity) are sensitive to early changes in eyes even before retinopathy is present. This study evaluates a novel color perimetry device as an indicator of diabetic eye disease. Methods: 40 (age-matched) subjects were divided into three groups by HbA1c or previous diagnosis (control ≤ 5.6%, prediabetes 5.7–6.4%, and diabetes ≥ 6.5%). Additional health metrics gathered included BMI, body fat %, total cholesterol, HDL/LDL levels, blood glucose, and blood pressure. Novel color perimetry which measures chromatic thresholds at four locations, three degrees from the fovea, for five colors (achromatic, red, green, blue, and yellow) was completed. Mars contrast and L’Anthony D15 color testing were also completed. Lens photos excluded those with cataracts. Results: There were differences between the groups for HbA1c (p < 0.001), BMI (p = 0.046), body fat % (p = 0.020), and color perimetry for the yellow condition only (p = 0.013). The achromatic condition was highly associated with Mars contrast sensitivity (p < 0.001). HbA1c was associated with both parvocellular (average of red and green) (p = 0.014) and koniocellular (average of blue and yellow) color perimetry performance (p = 0.022). Conclusions: HbA1c is associated with color perimetry across both retinal pathways. The yellow condition in particular holds promise as a biomarker for the presence of functional changes in diabetes prior to the onset of retinopathy. Other health metrics did not influence chromatic thresholds. More research needs to be conducted to evaluate color perimetry in these patient groups to understand these relationships.
Full article

Graphical abstract
Open AccessArticle
A Real-World Comparison of Three Deep Learning Systems for Diabetic Retinopathy in Remote Australia
by
Jocelyn J. Drinkwater, Qiang Li, Kerry Woods, Emma Douglas, Mark Chia, Yukun Zhou, Steve Bartnik, Yachana Shah, Vaibhav Shah, Pearse A. Keane and Angus W. Turner
Diabetology 2025, 6(12), 146; https://doi.org/10.3390/diabetology6120146 - 1 Dec 2025
Abstract
Background/objective: Deep learning systems (DLSs) may improve access to screening for diabetic retinopathy (DR), a leading cause of vision loss. Therefore, the aim was to prospectively compare the performance of three DLSs, Google ARDA, Thirona RetCADTM, and EyRIS SELENA+, in the
[...] Read more.
Background/objective: Deep learning systems (DLSs) may improve access to screening for diabetic retinopathy (DR), a leading cause of vision loss. Therefore, the aim was to prospectively compare the performance of three DLSs, Google ARDA, Thirona RetCADTM, and EyRIS SELENA+, in the detection of referable DR in a real-world setting. Methods: Participants with self-reported diabetes presented to a mobile facility for DR screening in the remote Pilbara region of Western Australia, which has a high proportion of First Nations people. Sensitivity, specificity, and other performance indicators were calculated for each DLS, compared to grading by an ophthalmologist adjudication panel. Results: Single field colour fundus photographs from 188 eyes of 94 participants (51% male, 70% First Nations Australians, and mean ± SD age of 60.3 ± 12.0 years) were assessed; 39 images had referable DR, 135 had no referable DR, and 14 images were ungradable. The sensitivity/specificity of ARDA was 100% (95% CI: 91.03–100%)/94.81% (89.68–97.47%), RetCAD was 97.37% (86.50–99.53%)/97.01% (92.58–98.83%) and SELENA+ was 91.67% (78.17–97.13%)/80.80% (73.02–86.74%). Conclusions: In a small, real-world service evaluation, comprising majority First Nations people from remote Western Australia, DLSs had high sensitivity and specificity for detecting referable DR. A comparative service evaluation can be useful to highlight differences between DLSs, especially in unique settings or with minority populations.
Full article
(This article belongs to the Special Issue New Perspectives and Future Challenges in Diabetic Retinopathy)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Impact of Type 2 Diabetes Mellitus on Age at Death in the Hemodialysis Population: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
by
Ji Hong You, Kang Ju Son, Kyoung Sook Park, Byung-Wan Lee and Sun Ok Song
Diabetology 2025, 6(12), 145; https://doi.org/10.3390/diabetology6120145 - 1 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Diabetic nephropathy is the leading cause of end-stage kidney disease (ESKD) worldwide. ESKD individuals with type 2 diabetes are known to have poor prognosis of survival. We aimed to investigate whether the recent mortality trends of ESKD individuals treated with hemodialysis with
[...] Read more.
Background/Objectives: Diabetic nephropathy is the leading cause of end-stage kidney disease (ESKD) worldwide. ESKD individuals with type 2 diabetes are known to have poor prognosis of survival. We aimed to investigate whether the recent mortality trends of ESKD individuals treated with hemodialysis with or without type 2 diabetes have changed in South Korea. Methods: We used a cohort of 3,394,502 deceased people from the Korean National Health Insurance Service claims database from 2006 to 2018. We requested the National Statistical Information Service database to link the records about their cause of death. We collected a total of 79,792 deaths among individuals with ESKD receiving hemodialysis, including 31,907 with type 2 diabetes and 47,885 without type 2 diabetes. Results: The mean age at death significantly increased over the study period among individuals with ESKD receiving hemodialysis, both with and without type 2 diabetes (p < 0.001). However, the mean age at death was consistently lower in those with type 2 diabetes compared to those without diabetes in both men and women. Type 2 diabetes was significantly associated with younger age at death in individuals undergoing hemodialysis (β = −0.012, p < 0.0001). The age-standardized mortality rate remained higher in those with type 2 diabetes throughout the study period. Conclusions: This nationwide study revealed that Korean individuals with type 2 diabetes undergoing hemodialysis had a consistently lower age at death and higher age-standardized mortality than those without type 2 diabetes. Although the mean age at death increased in both groups, individuals undergoing hemodialysis with type 2 diabetes continued to show poorer survival outcomes. These findings highlight the need for targeted clinical approaches to improve survival in this high-risk population.
Full article

Graphical abstract
Open AccessReview
From Classic to Contemporary, Evolving Therapies in Diabetic Kidney Disease: The Point of View of the Nephrologist and the Diabetologist
by
Micaela Gentile, Marta D’Angelo, Maria Rosaria Varì, Andrea Mario Bolla, Maurizio Bianco and Roberto Scarpioni
Diabetology 2025, 6(12), 144; https://doi.org/10.3390/diabetology6120144 - 1 Dec 2025
Abstract
►▼
Show Figures
Diabetes mellitus represents a global health concern, which is expected to worsen over the years. The prevalence is estimated to increase up to 642 million people by 2040. Almost half of diabetic patients are at a high risk of developing kidney involvement up
[...] Read more.
Diabetes mellitus represents a global health concern, which is expected to worsen over the years. The prevalence is estimated to increase up to 642 million people by 2040. Almost half of diabetic patients are at a high risk of developing kidney involvement up to dialysis; moreover, macrovascular complication could be an obstacle to kidney transplant. Besides the classic albuminuric phenotype, non-albuminuric diabetic kidney disease was also discovered recently. Fortunately, compared with classic therapy with diet, oral hypoglycemic drugs, and insulin, current clinicians can rely on several new drugs that act with different pathways characterized by kidney and heart protection, as shown by several clinical trials and confirmed in clinical practice. Herein, we will review the therapies that nephrologist and diabetologist have available today and the future perspective.
Full article

Graphical abstract
Open AccessBrief Report
The Von Hippel–Lindau Protein (pVHL) Is Downregulated in the Pancreatic Islets of Mice with Type 2 Diabetes Induced by a High-Calorie Diet
by
Alma Nelly Diaz-Herreros, Alberto Granados-Galeana, Isaí Martínez-Torres, Elba Reyes-Maldonado, Erika Rosales-Cruz, Fernando Gómez-Chávez, Gabriel Betanzos-Cabrera, Amaranta Sarai Valdez-Guerrero, Juan Carlos Cancino-Diaz and Mario Eugenio Cancino-Diaz
Diabetology 2025, 6(12), 143; https://doi.org/10.3390/diabetology6120143 - 27 Nov 2025
Abstract
Background/Objectives: Knock-out mice lacking von Hippel–Lindau protein (pVHL) in pancreatic beta cells exhibit glucose intolerance and low insulin production, indicating a possible association between pVHL and diabetes mellitus (DM). It is currently unknown whether DM causes a decrease in pVHL expression. In
[...] Read more.
Background/Objectives: Knock-out mice lacking von Hippel–Lindau protein (pVHL) in pancreatic beta cells exhibit glucose intolerance and low insulin production, indicating a possible association between pVHL and diabetes mellitus (DM). It is currently unknown whether DM causes a decrease in pVHL expression. In this study, we determined the level of pVHL expression in the pancreas of mice with type 2 DM (T2DM) induced by a high-calorie diet (HCD). Methods: Mice of the C57BL/6 and BALB/c strains were fed with a HCD for 10 weeks, and another group of mice of both strains were fed a standard diet (SD). The mice were monitored for body weight and glucose levels until the end of the treatment. Immunodetection for pVHL, HIF-1α, Insulin and GLUT-1 was performed. Results: A significant increase in body weight in C57BL/6 mice fed HCD at week 10 compared to mice fed a SD (p < 0.05), with similar results for the BALB/c strain. The glucose level was significantly higher in the C57BL/6 strain and the BALB/c strain fed with HCD compared to mice on a SD (p < 0.05). There was lower pVHL and insulin expression in the pancreatic islets of both strains fed HCD. In contrast, there was higher pVHL expression in the pancreatic islets of both strains of mice fed a SD. HIF-1α and GLUT-1 expression was higher in mice fed HCD than in mice fed a SD. Conclusions: HCD-induced T2DM causes low pVHL expression in the pancreatic islets of C57BL/6 and BALB/c mice, suggesting that low pVHL expression is related to the development of T2DM in mice.
Full article
(This article belongs to the Special Issue Regulatory Networks of Pancreatic Beta-Cell Function and Insulin Secretion: Intrinsic Mechanisms and Extrinsic Modulators)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Semaglutide Therapy and Cardiorenal Risk Management in Type 2 Diabetes: hsCRP as a Biomarker of Risk
by
Nikolay Krasimirov Kostadinov, Tcvetelina Totomirova and Boyan Ivanov Nonchev
Diabetology 2025, 6(12), 142; https://doi.org/10.3390/diabetology6120142 - 25 Nov 2025
Abstract
►▼
Show Figures
Background: Inflammation plays a key role in the pathogenesis of type 2 diabetes (T2D) and the associated cardiovascular complications. High-sensitivity C-reactive protein (hsCRP) is a widely used marker of systemic inflammation as well as a predictor of cardiovascular risk. Objective: There is increasing
[...] Read more.
Background: Inflammation plays a key role in the pathogenesis of type 2 diabetes (T2D) and the associated cardiovascular complications. High-sensitivity C-reactive protein (hsCRP) is a widely used marker of systemic inflammation as well as a predictor of cardiovascular risk. Objective: There is increasing evidence that glucagon-like peptide-1 receptor agonists (GLP-1RAs), including semaglutide, may have effects on hsCRP levels, independent of their effects on glycemic control and body weight loss. This purpose of our study is to explore the effect of semaglutide on hsCRP levels in patients with type 2 diabetes. Additionally, we aimed to determine whether the observed effect of semaglutide on hsCRP is fully mediated by changes in HbA1c and body weight, or whether there is a direct effect suggesting the presence of an independent anti-inflammatory mechanism. Methods: The study included 70 outpatients with diagnosed type 2 diabetes undergoing therapy with metformin and/or a sulfonylurea. Semaglutide was added to the existing therapeutic regimen. All participants were followed up after a 6-month a period. At the beginning and at the end of the study, the hsCRP values, some selected indicators of glycemic control, and the anthropometric measurements were recorded. Results: The mean hsCRP value at baseline was 4.90 ± 1.21 mg/L, while after six-month therapy, it dropped to 2.23 ± 2.21 mg/L. Conclusions: The results of the analysis have a good potential to contribute to a better understanding of the pleiotropic effects of GLP-1 RAs and support the hypothesis of a direct anti-inflammatory role of semaglutide, which could have clinical significance in the context of cardiometabolic risk management in patients with type 2 diabetes.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Diabetology
Current Understanding of Gender Differences in Diabetes and Rheumatological Diseases
Guest Editors: Giancarlo Tonolo, Daniela MarottoDeadline: 15 December 2025
Special Issue in
Diabetology
Feature Papers in Diabetology 2025
Guest Editor: Peter CliftonDeadline: 31 December 2025
Special Issue in
Diabetology
Healthy Habits of Diabetes: Prevention, Intervention and Management Strategies
Guest Editors: Jie Hu, Eileen R. FauldsDeadline: 10 January 2026
Special Issue in
Diabetology
Regulatory Networks of Pancreatic Beta-Cell Function and Insulin Secretion: Intrinsic Mechanisms and Extrinsic Modulators
Guest Editors: Chiara Saponaro, Mara SuleimanDeadline: 15 January 2026