- Systematic Review
Effectiveness of Pulsed Electromagnetic Field Therapy on Neuropathic Pain: A Systematic Review and Meta-Analysis
- Jesus Antonio Lara-Reyes,
- Cristofer Zarate-Calderon and
- Fausto Rojas-Durán
- + 2 authors
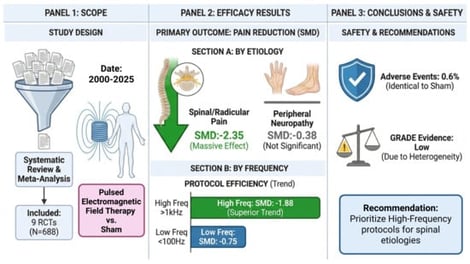
Background: Neuropathic pain represents a substantial global burden with limited effective therapeutic options. Pulsed Electromagnetic Field (PEMF) therapy has emerged as a potential non-invasive adjuvant, though clinical evidence remains inconsistent. This systematic review and meta-analysis evaluated PEMF efficacy and safety, specifically analyzing the influence of etiology and stimulation parameters. Methods: Following PRISMA 2020 guidelines (PROSPERO: CRD420251184151), five databases (Cochrane, PubMed, Scopus, Web of Science, and LILACS) were searched for Randomized Controlled Trials (RCTs) comparing PEMF versus sham. Risk of bias was assessed via Cochrane RoB 2, and heterogeneity was explored through detailed subgroup analyses. Results: Thirteen RCTs met the inclusion criteria (N = 688). While global analysis indicated a statistically significant pain reduction (SMD: −1.01; p = 0.03), it exhibited extreme statistical heterogeneity (I2 = 92.8%) and instability. After adjusting for missing studies using the Trim-and-Fill method, global significance disappeared. However, subgroup analysis resolved this inconsistency, revealing a massive, clinically meaningful effect in Spinal/Radicular pain (SMD: −2.35; 95% CI: −4.42 to −0.29), whereas Peripheral Neuropathy showed no significant reduction (SMD: −0.38; 95% CI: −0.86 to 0.10). Conclusions: The PEMF evidence base for neuropathic pain is currently highly fragmented. Extreme heterogeneity and publication bias render “one-size-fits-all” efficacy estimates invalid and potentially misleading. Instead, our data reveals a critical etiological divergence: PEMF appears highly effective for spinal/radicular pathology, likely due to the mechanical nature of the lesion, but demonstrates limited efficacy for diffuse peripheral neuropathy. Future research must abandon generic protocols in favor of etiology-specific trials, prioritizing high-frequency parameters and rigorous bias control.
6 February 2026