Pericapsular Nerve Group Block Versus Lumbar Epidural Block for Pain Management After Hip Surgeries with a Focus on Pediatric Patients: A Narrative Review
Abstract
1. Introduction
1.1. Overview of Pediatric Hip Surgeries
1.2. Postoperative Pain Issues
1.3. Introduction to Lumbar Epidural Block vs. Pericapsular Nerve Group Block
2. Methods
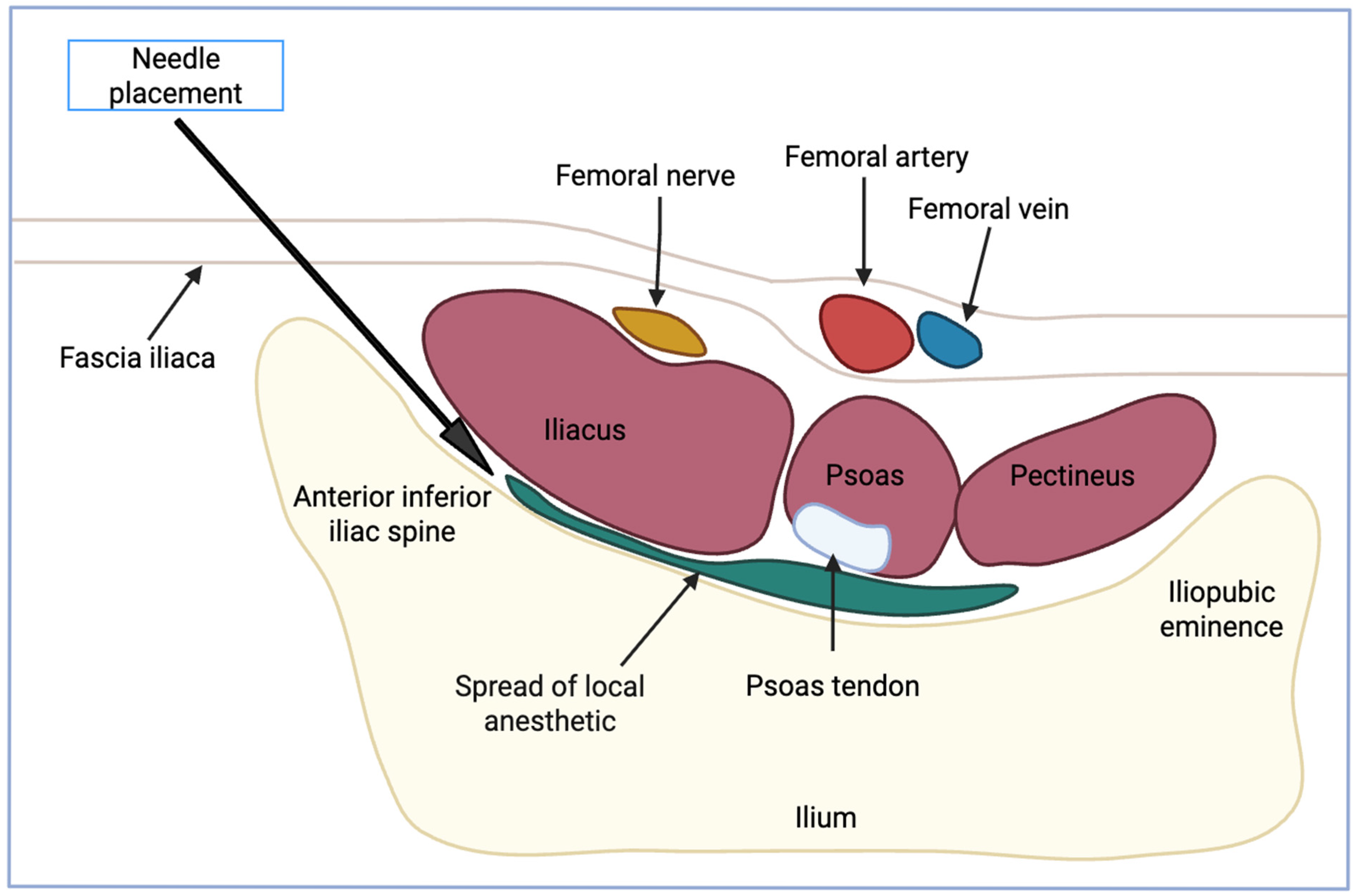
3. Pericapsular Nerve Group (PENG) Block
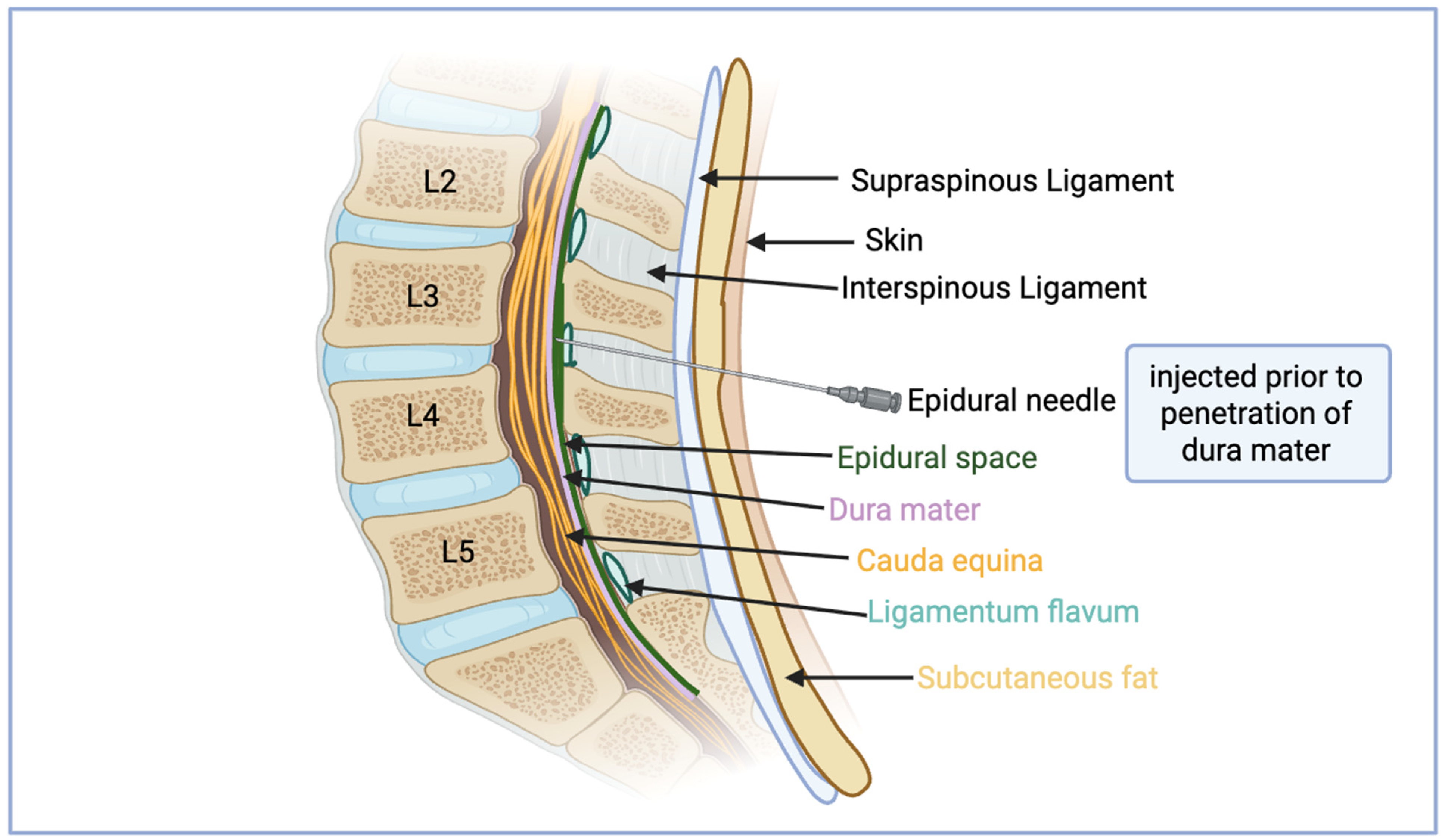
4. Lumbar Epidural Block
5. Comparison of the Efficacy Between Blocks
6. Discussion and Conclusions
7. Limitation of Current Evidence
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Fan, Z.; Yan, L.; Liu, H.; Li, X.; Fan, K.; Liu, Q.; Li, J.J.; Wang, B. The Prevalence of Hip Osteoarthritis: A Systematic Review and Meta-Analysis. Arthritis Res. Ther. 2023, 25, 51. Available online: https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-023-03033-7 (accessed on 24 May 2025). [CrossRef]
- Azevedo, D.C.; Hoff, L.S.; Kowalski, S.C.; de Andrade, C.A.F.; Trevisani, V.F.M.; de Melo, A.K.G. Risk Factors for Osteoporotic Hip Fracture Among Community-Dwelling Older Adults: A Real-World Evidence Study. Adv. Rheumatol. 2024, 64, 8. Available online: https://advancesinrheumatology.biomedcentral.com/articles/10.1186/s42358-024-00350-6 (accessed on 24 May 2025). [CrossRef]
- Crofts, H.; McConkey, M.; Lodhia, P. Pediatric Hip Arthroscopy: A Review of Indications and Treatment Outcomes. Curr. Rev. Musculoskelet. Med. 2023, 16, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Lopata, L.; Roh, A.; Huang, M.; Monteleone, M.A.; Wang, S.; Sun, L.S. Factors influencing postoperative pain following discharge in pediatric ambulatory surgery patients. J. Clin. Anesth. 2017, 39, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Genel, F.; Harris, I.A.; Patanwala, A.E.; Adie, S.; Stevens, J.; Hassett, G.; Luckie, K.; Penm, J.; Naylor, J. Effectiveness of Pharmacological-Based Interventions, Including Education and Prescribing Strategies, to Reduce Subacute Pain After Total Hip or Knee Arthroplasty: A Systematic Review of Randomized Controlled Trials. Pain Med. 2022, 23, 1476–1488. [Google Scholar] [CrossRef] [PubMed]
- Carlton, E.F.; Moniz, M.H.; Scott, J.W.; Prescott, H.C.; Becker, N.V. Financial Outcomes After Pediatric Critical Illness Among Commercially Insured Families. Crit. Care 2023, 27, 227. Available online: https://ccforum.biomedcentral.com/articles/10.1186/s13054-023-04493-8 (accessed on 24 May 2025). [CrossRef]
- Daughtrey, H.R.; Ruiz, M.O.; Felix, N.; Saynina, O.; Sanders, L.M.; Anand, K.J.S. Incidence of mental health conditions following pediatric hospital admissions: Analysis of a national database. Front. Pediatr. 2024, 12, 1344870. [Google Scholar] [CrossRef]
- Odegard, M.; Kelley-Quon, L.I. Postoperative Opioid Prescribing, Use, and Disposal in Children. Adv. Pediatr. 2022, 69, 259–271. [Google Scholar] [CrossRef]
- Kil, H.K. Caudal and epidural blocks in infants and small children: Historical perspective and ultrasound-guided approaches. Korean J. Anesthesiol. 2018, 71, 430–439. [Google Scholar] [CrossRef]
- Girón-Arango, L.; Peng, P.W.H.; Chin, K.J.; Brull, R.; Perlas, A. Pericapsular Nerve Group (PENG) Block for Hip Fracture. Reg. Anesth. Pain Med. 2018, 43, 859. [Google Scholar] [CrossRef]
- Bunnell, A.M.; Smith, J.V. Pericapsular Nerve Group (PENG) Block for Pediatric Hip Surgery: A Report of Three Cases. Cureus 2025, 17, e78996. [Google Scholar] [CrossRef] [PubMed]
- Elhamrawy, A.; Kerbage, J.; Veneziano, G.; Martin, D.P.; Tobias, J.D. Pericapsular Nerve Group (PENG) Block in Pediatric Patients Undergoing Hip and Pelvic Surgical Procedures: An Educational Focused Review. J. Pain Res. 2024, 17, 3697–3705. [Google Scholar] [CrossRef] [PubMed]
- Turgut, M.; Protas, M.; Gardner, B.; Oskouian, R.J.; Loukas, M.; Tubbs, R.S. The accessory obturator nerve: An anatomical study with literature analysis. Anatomy 2017, 11, 121–127. [Google Scholar] [CrossRef]
- Gupta, N.; Das, S.; Chatterjee, N.; Munjal, M. A Retrospective Study of Ultrasound-Guided Pericapsular Nerve Group Block with Dexamethasone: An Excellent Option for Early Mobility Following Total Hip Replacement Surgery. Cureus 2025, 14, e32515. [Google Scholar] [CrossRef]
- Margenfeld, F.; Zendehdel, A.; Poilliot, A.; Tamborrini, G.; Beck, M.; Müller-Gerbl, M. Pericapsular Nerve Group (PENG) Block on Cadavers: A Scoping Review. J. Diagn. Med. Sonogr. 2024, 41, 356–363. Available online: https://journals.sagepub.com/doi/full/10.1177/87564793241303167 (accessed on 24 May 2025). [CrossRef]
- Merella, F.; Mossetti, V. Ultrasound-guided upper and lower extremity nerve blocks in children. BJA Educ. 2020, 20, 42–50. [Google Scholar] [CrossRef]
- Jung, Y.; Choi, S.; Lee, S.; Kim, N.; Kim, E. Effective protocol for continuous pericapsular nerve group block in femur fracture patients undergoing hip surgery: Two case reports. Kosin Med. J. 2024, 39, 214–219. [Google Scholar] [CrossRef]
- Domagalska, M.; Wieczorowska-Tobis, K.; Reysner, T.; Geisler-Wojciechowska, A.; Grochowicka, M.; Kowalski, G. Pericapsular Nerves Group (PENG) Block in Children under Five Years of Age for Analgesia in Surgery for Hip Dysplasia: Case Report. J. Pers. Med. 2023, 13, 454. [Google Scholar] [CrossRef]
- Mostafa, T.A.H.; Omara, A.F.; Khalil, N.K. Comparison of ultrasound-guided erector spinae plane block with ultrasound-guided pericapsular nerve group block for paediatric hip surgery: A randomised, double-blinded study. Indian J. Anaesth. 2024, 68, 616–622. [Google Scholar] [CrossRef]
- Jadon, A.; Srivastawa, S.; Bakshi, A.; Sahoo, R.K.; Singh, B.K.; Sinha, N. Does adding lateral femoral cutaneous nerve block improves the analgesia of pericapsular nerve group block in the fractured hip surgeries? Braz. J. Anesthesiol. 2022, 72, 836–838. [Google Scholar] [CrossRef]
- Balasubramaniam, A.; Kumar Naggaih, S.; Tarigonda, S.; Madhusudhana, R. Ultrasound-Guided Pericapsular Nerve Group Block for Hip Surgery: A Randomized Controlled Trial Study Comparing Ropivacaine and Ropivacaine with Dexamethasone. Cureus 2023, 15, e34261. [Google Scholar] [CrossRef] [PubMed]
- Kalanjiyam, G.P.; Kanna, R.M.; Rajasekaran, S. Pediatric spinal injuries—Current concepts. J. Clin. Orthop. Trauma 2023, 38, 102122. [Google Scholar] [CrossRef] [PubMed]
- Kao, S.C.; Lin, C.S. Caudal Epidural Block: An Updated Review of Anatomy and Techniques. BioMed Res. Int. 2017, 2017, 9217145. [Google Scholar] [CrossRef]
- Jain, D.; Hussain, S.Y.; Ayub, A. Comparative evaluation of landmark technique and ultrasound-guided caudal epidural injection in pediatric population: A systematic review and meta-analysis. Paediatr. Anesth. 2022, 32, 35–42. [Google Scholar] [CrossRef]
- Xu, W.; Wei, H.; Zhang, T. Methods of prolonging the effect of caudal block in children. Front. Pediatr. 2024, 12, 1406263. [Google Scholar] [CrossRef]
- Goyal, V.; Kubre, J.; Radhakrishnan, K. Dexmedetomidine as an adjuvant to bupivacaine in caudal analgesia in children. Anesth. Essays Res. 2016, 10, 227–232. [Google Scholar] [CrossRef]
- Rezayi Soufiani, A.; Joulani, M.; Jolani, M.S.; Parish, M. Accessing the efficacy and peri-operative adverse effects of three different hyperbaric bupivacaine 0.5% dosages for spinal anesthesia induction in lower limb orthopedic surgeries: A randomized clinical trial. BMC Anesthesiol. 2024, 24, 285. [Google Scholar] [CrossRef]
- Avila Hernandez, A.N.; Hendrix, J.M. Epidural Anesthesia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK542219/ (accessed on 6 May 2025).
- Wani, T.M.; Dabaliz, A.; Kadah, K.; Veneziano, G.; Tumin, D.; Tobias, J.D. Comparison of the skin-to-epidural space distance at the thoracic and lumbar levels in children using magnetic resonance imaging. Saudi J. Anesth. 2020, 14, 493–497. [Google Scholar] [CrossRef]
- Silva, M.; Halpern, S.H. Epidural analgesia for labor: Current techniques. Local Reg. Anesth. 2010, 3, 143–153. [Google Scholar] [CrossRef]
- Macpherson, D.; Quondamatteo, F.; Broom, M. Update on applied epidural anatomy. BJA Educ. 2022, 22, 182–189. [Google Scholar] [CrossRef]
- Swezey, E.; Bordoni, B. Anatomy, Bony Pelvis and Lower Limb: Lateral Femoral Cutaneous Nerve. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK532301/ (accessed on 13 August 2025).
- Tomlinson, J.; Ondruschka, B.; Prietzel, T.; Zwirner, J.; Hammer, N. A systematic review and meta-analysis of the hip capsule innervation and its clinical implications. Sci. Rep. 2021, 11, 5299. [Google Scholar] [CrossRef]
- Refai, N.A.; Black, A.C.; Tadi, P. Anatomy, Bony Pelvis and Lower Limb: Thigh Femoral Nerve. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK556065/ (accessed on 13 August 2025).
- Casati, A.; Santorsola, R.; Aldegheri, G.; Ravasi, F.; Fanelli, G.; Berti, M.; Fraschini, G.; Torri, G. Intraoperative epidural anesthesia and postoperative analgesia with levobupivacaine for major orthopedic surgery: A double-blind, randomized comparison of racemic bupivacaine and ropivacaine. J. Clin. Anesth. 2003, 15, 126–131. [Google Scholar] [CrossRef]
- Del Buono, R.; Padua, E.; Pascarella, G.; Costa, F.; Tognù, A.; Terranova, G.; Greco, F.; Perez, M.F.; Barbara, E. Pericapsular nerve group block: An overview. Minerva Anestesiol. 2021, 87, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Chenyang, D.; Xu, B.; Lao, Y.; Sheng, H.; Zhang, S.; Huang, Y.; Chen, R.J. Pericapsular nerve group block reduces opioid use and pain after hip surgery: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2024, 19, e0310008. [Google Scholar] [CrossRef] [PubMed]
- Yeoh, S.R.; Chou, Y.; Chan, S.M.; Hou, J.D.; Lin, J.A. Pericapsular Nerve Group Block and Iliopsoas Plane Block: A Scoping Review of Quadriceps Weakness after Two Proclaimed Motor-Sparing Hip Blocks. Healthcare 2022, 10, 1565. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.; Bhasulamani, S.P.; James, D.; Yadav, B.; Rai, E. A cross-sectional observation study to evaluate the efficacy and complications of epidural analgesia in paediatric population. J. Anaesthesiol. Clin. Pharmacol. 2023, 39, 189–194. [Google Scholar] [CrossRef]
- Pearson, A.C.S.; Dodd, S.E.; Kraus, M.B.; Ligda, K.M.O.; Hertzberg, L.B.; Patel, P.V.; Chandrabose, R.K. Pilot Survey of Female Anesthesiologists’ Childbearing and Parental Leave Experiences. Anesth. Analg. 2019, 128, e109. [Google Scholar] [CrossRef]
- Kasanavesi, R.C.; Gazula, S.; Pula, R.; Thakur, N. Safety of post-operative epidural analgesia in the paediatric population: A retrospective analysis. Indian J. Anaesth. 2015, 59, 636–640. [Google Scholar] [CrossRef]
- Bryant, J.; Joselyn, A.; Tobias, J. The Complicated Uncomplicated Epidural Placed Under General Anesthesia: A Complete Spinal in the Post-Anesthesia Recovery Unit. J. Med. Cases 2014, 5, 564–566. [Google Scholar] [CrossRef]
- Taenzer, A.H.; Walker, B.J.; Bosenberg, A.T.; Martin, L.; Suresh, S.; Polaner, D.M.; Wolf, C.; Krane, E.J. Asleep Versus Awake: Does It Matter? Reg. Anesth. Pain Med. 2014, 39, 279–283. [Google Scholar] [CrossRef]
- Wathen, J.E.; Gao, D.; Merritt, G.; Georgopoulos, G.; Battan, F.K. A randomized controlled trial comparing a fascia iliaca compartment nerve block to a traditional systemic analgesic for femur fractures in a pediatric emergency department. Ann. Emerg. Med. 2007, 50, 162–171.e1. [Google Scholar] [CrossRef]
- Remily, E.A.; Hochstein, S.R.; Wilkie, W.A.; Mohamed, N.S.; Thompson, J.V.; Kluk, M.W.; Nace, J.; Delanois, R.E. The pericapsular nerve group block: A step towards outpatient total hip arthroplasty? Hip Int. 2022, 32, 318–325. [Google Scholar] [CrossRef]
- Wong, G.K.; Arab, A.A.; Chew, S.C.; Naser, B.; Crawford, M.W. Major complications related to epidural analgesia in children: A 15-year audit of 3,152 epidurals. Can. J. Anesth. J. Can. Anesth. 2013, 60, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Orozco, S.; Muñoz, D.; Jaramillo, S.; Herrera, A.M. Pediatric use of Pericapsular Nerve Group (PENG) block for hip surgical procedures. J. Clin. Anesth. 2019, 57, 143–144. [Google Scholar] [CrossRef]
- Domagalska, M.; Ciftci, B.; Reysner, T.; Kolasiński, J.; Wieczorowska-Tobis, K.; Kowalski, G. Pain Management and Functional Recovery after Pericapsular Nerve Group (PENG) Block for Total Hip Arthroplasty: A Prospective, Randomized, Double-Blinded Clinical Trial. J. Clin. Med. 2023, 12, 4931. [Google Scholar] [CrossRef]
- Sharma, H.; Mitra, S.; Singh, J.; Gupta, S.; Garg, S. A Randomized Study Comparing the Efficacy of Ultrasound Guided Lumbar Plexus Block and Epidural Anesthesia for Postoperative Analgesia in Patients Undergoing Total Hip Replacement. Asian J. Anesthesiol. 2020, 58, 131–137. [Google Scholar] [CrossRef]
- Ecoffey, C.; Bosenberg, A.; Lonnqvist, P.A.; Suresh, S.; Delbos, A.; Ivani, G. Practice advisory on the prevention and management of complications of pediatric regional anesthesia. J. Clin. Anesth. 2022, 79, 110725. [Google Scholar] [CrossRef]
| Author (Year) | Groups Studied and Intervention | Results and Findings | Conclusions |
|---|---|---|---|
| Domagalska et al. (2023) [18] | Case report of two children under the age of 5 to determine the analgesic effect of PENG block on hip surgery. | Neither patient required extra opioids during the surgery, or breakthrough opioids or muscle relaxants overnight. Both had numeric pain scores either at or below 3/10. Patients could participate in physical therapy the next day, and there was no proof of block complications. | PENG block provided opioid sparing management and retained motor functioning in these pediatric patients. Observations are encouraging for the efficacy and safety of PENG, but further studies are required. |
| Orozco et al. (2019) [47] | Case report of eight-year-old patient undergoing PENG block for open hip surgery. | Patient did not require intraoperative use of opioids in infusions or boluses. The patient had no pain up to 72 h postoperative recovery, had a pain level of 2/10, and did not require additional analgesia. | PENG block provided opioid sparing management along with decreased pain postoperatively. Observations are encouraging for the efficacy and safety of PENG, but further studies are required. |
| Domagalska et al. (2023) [48] | A Prospective, Randomized, Double-Blinded Clinical Trial with 468 patients to determine the effect of PENG block on pain management and recovery after total hip arthroplasty. | Compared to sham groups, PENG block had decreased overall opioid consumption, increased quadriceps strength, increased time to first opioid, and decreased NRS pain scores at rest and with movement. | The PENG block shows that it is an effective analgesic option in total hip arthroplasty in adults, which shows promise for the applicability in pediatrics as well. |
| Hu et al. (2024) [37] | Systemic review and meta-analysis of randomized control trials to determine effectiveness of PENG block in relation to opioid use. | Significantly lower opioid consumption in adults 24 h after hip fracture surgery among those who received spinal anesthesia. Significantly lower dynamic pain scores, but no significant difference in static pain scores. PENG block also showed significantly lower risks of unsatisfactory events. | These early trials have evidence that supports PENG blocks can significantly reduce opioid consumption after hip surgery and improve early functional recovery. Still more studies need to be completed in pediatric-specific populations to allow for more solid conclusions. |
| Patient/Surgical Factor | Favors PENG Block | Favors Lumbar Epidural | Favors Caudal Epidural |
|---|---|---|---|
| Expected post-op pain severity | Mild–moderate | Moderate–severe | Mild–moderate |
| Surgical invasiveness | Less invasive procedures | Extensive bilateral or complex surgery | Moderate invasiveness |
| Need for motor sparing/early mobilization | High priority | Lower priority | Lower priority |
| Coagulopathy or anticoagulant use | Considered when neuraxial techniques are relatively contraindicated; superficial, extra-neuraxial injection [50] | Contraindicated | Contraindicated |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmadzadeh, S.; Schwab, H.M.; O’Dell Duplechin, M.; Broocks, K.M.; Hirsch, J.D.; Drinkard, J.; Shekoohi, S. Pericapsular Nerve Group Block Versus Lumbar Epidural Block for Pain Management After Hip Surgeries with a Focus on Pediatric Patients: A Narrative Review. Neurol. Int. 2025, 17, 142. https://doi.org/10.3390/neurolint17090142
Ahmadzadeh S, Schwab HM, O’Dell Duplechin M, Broocks KM, Hirsch JD, Drinkard J, Shekoohi S. Pericapsular Nerve Group Block Versus Lumbar Epidural Block for Pain Management After Hip Surgeries with a Focus on Pediatric Patients: A Narrative Review. Neurology International. 2025; 17(9):142. https://doi.org/10.3390/neurolint17090142
Chicago/Turabian StyleAhmadzadeh, Shahab, Hunter M. Schwab, Mary O’Dell Duplechin, Kalob M. Broocks, Jon D. Hirsch, Joseph Drinkard, and Sahar Shekoohi. 2025. "Pericapsular Nerve Group Block Versus Lumbar Epidural Block for Pain Management After Hip Surgeries with a Focus on Pediatric Patients: A Narrative Review" Neurology International 17, no. 9: 142. https://doi.org/10.3390/neurolint17090142
APA StyleAhmadzadeh, S., Schwab, H. M., O’Dell Duplechin, M., Broocks, K. M., Hirsch, J. D., Drinkard, J., & Shekoohi, S. (2025). Pericapsular Nerve Group Block Versus Lumbar Epidural Block for Pain Management After Hip Surgeries with a Focus on Pediatric Patients: A Narrative Review. Neurology International, 17(9), 142. https://doi.org/10.3390/neurolint17090142







