-
 Burden of Infected Diabetic Foot Ulcers on Hospital Admissions and Costs in a Third-Level Center
Burden of Infected Diabetic Foot Ulcers on Hospital Admissions and Costs in a Third-Level Center -
 Exploration of Foundational Models for Blood Glucose Forecasting in Type-1 Diabetes Pediatric Patients
Exploration of Foundational Models for Blood Glucose Forecasting in Type-1 Diabetes Pediatric Patients -
 Lifestyle Medicine Case Manager Nurses for Type Two Diabetes Patients: An Overview of a Job Description Framework—A Narrative Review
Lifestyle Medicine Case Manager Nurses for Type Two Diabetes Patients: An Overview of a Job Description Framework—A Narrative Review -
 The Main Risk Factors in Type 2 Diabetes for Cognitive Dysfunction, Depression, and Psychosocial Problems: A Systematic Review
The Main Risk Factors in Type 2 Diabetes for Cognitive Dysfunction, Depression, and Psychosocial Problems: A Systematic Review -
 Exosome-Derived microRNAs: Bridging the Gap Between Obesity and Type 2 Diabetes in Diagnosis and Treatment
Exosome-Derived microRNAs: Bridging the Gap Between Obesity and Type 2 Diabetes in Diagnosis and Treatment
Journal Description
Diabetology
Diabetology
is an international, peer-reviewed, open access journal on diabetes research published monthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, EBSCO, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 26.3 days after submission; acceptance to publication is undertaken in 5.8 days (median values for papers published in this journal in the first half of 2025).
- Journal Rank: CiteScore - Q2 (Medicine (miscellaneous))
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
2.2 (2024);
5-Year Impact Factor:
2.5 (2024)
Latest Articles
Effect of Menstrual Cycle on Glycemic Outcomes and Insulin Requirements in Women with Type 1 Diabetes Who Are Users of Advanced Hybrid Closed-Loop Systems
Diabetology 2025, 6(11), 139; https://doi.org/10.3390/diabetology6110139 - 4 Nov 2025
Abstract
►
Show Figures
Purpose: It has been previously described that some women with type 1 diabetes (T1D) may experience changes in glucose levels in relation to their menstrual cycle. However, whether an advanced hybrid closed-loop system (AHCL) can mitigate these cycle-dependent changes is yet to be
[...] Read more.
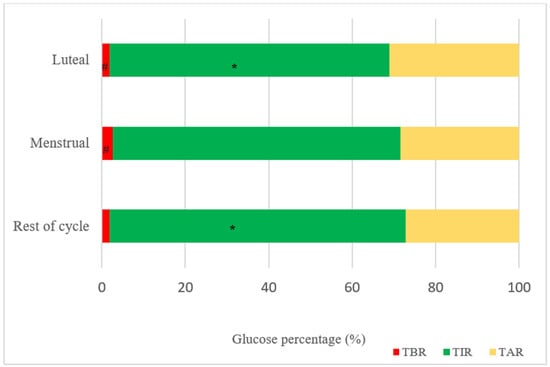
Purpose: It has been previously described that some women with type 1 diabetes (T1D) may experience changes in glucose levels in relation to their menstrual cycle. However, whether an advanced hybrid closed-loop system (AHCL) can mitigate these cycle-dependent changes is yet to be determined. Methods: This study is a prospective analysis of a cohort of premenopausal women with T1D with spontaneous menstrual cycles who are users of an AHCL system 780G Medtronic®. Three consecutive cycles were analyzed for each patient, and each cycle was divided into three phases (menstrual, luteal, and rest of cycle phase). Results: Fifteen subjects were included. Mean age was 38 ± 7.6 years, HbA1c was 7.12 ± 0.7%, and diabetes duration was 21 ± 13.7 years. Mean glucose was higher in the luteal phase compared to the menstrual period (p = 0.029 luteal vs. menstrual) and the rest of the cycle (p = 0.018 luteal vs. rest of cycle). The time in range (TIR) was lower in the luteal phase compared to the rest of cycle phase (p = 0.015 luteal vs. rest of cycle). The time below range (TBR) was significantly higher in the menstrual compared to the luteal phase (p = 0.007 luteal vs. menstrual). Daily insulin requirements were higher in luteal phase compared to rest of cycle (p = 0.017 luteal vs. rest of cycle). Conclusions: A higher mean glucose and lower TIR, despite a higher total insulin dose, was observed in the luteal phase. A higher TBR was observed in the menstrual phase. However, AHCL with 780G Medtronic® achieves a TIR of almost 70% in all cycle phases.
Full article
Open AccessArticle
Circulating Anti-Insulin Antibodies Protect Against Nocturnal Hypoglycemia in Patients with Type 2 Diabetes Treated with Long-Acting Insulin Analogues
by
Tokio Sanke, Yuko Matsuoka, Yoshiki Kadoya, Shoichi Yamada, Eri Tamagawa and Atsuyo Fujita
Diabetology 2025, 6(11), 138; https://doi.org/10.3390/diabetology6110138 - 4 Nov 2025
Abstract
►▼
Show Figures
Background: Long-acting insulin analogues have been widely used in patients with type 2 diabetes with reduced insulin secretion. In these patients, hypoglycemia may occur during the night when they do not consume food. We have already reported that anti-insulin antibodies developed at a
[...] Read more.
Background: Long-acting insulin analogues have been widely used in patients with type 2 diabetes with reduced insulin secretion. In these patients, hypoglycemia may occur during the night when they do not consume food. We have already reported that anti-insulin antibodies developed at a fairly high frequency in patients with type 2 diabetes treated with insulin analogues. Therefore, clinical factors associated with nocturnal hypoglycemia, including anti-insulin antibodies, were searched in patients with type 2 diabetes treated with insulin analogues. Methods: The subjects consisted of 55 patients with type 2 diabetes with relatively stable glucose control treated with long-acting insulin analogues and 15 non-diabetic subjects. Using a continuous glucose monitoring, glucose fluctuation was observed for 10 days. Hypoglycemia was defined as a glucose monitoring level of less than 54 mg/dL for more than 15 min. Results: Nocturnal (duration 6 h, from midnight to 6 a.m.) hypoglycemia was observed in 13 patients (23.6%). All of the cases were unrecognized. Daytime (duration 18 h, from 6 a.m. to midnight) hypoglycemia was also observed in 14 patients (25.5%). Stratified analysis and logistic regression analysis disclosed that anti-insulin antibodies were significantly associated with nocturnal hypoglycemia in contrast to daytime hypoglycemia, which was not associated with anti-insulin antibodies but associated with lower HbA1c. That is, the frequency of nocturnal hypoglycemia was significantly higher in the negative group and lower in the positive group of the anti-insulin antibodies. Conclusions: These results suggest that circulating anti-insulin antibodies protect against nocturnal hypoglycemia.
Full article

Graphical abstract
Open AccessArticle
Prevalence of Elevated Insulin Resistance Risk in a Large Office Worker Population: Sex-Stratified Analyses and Lifestyle Correlates
by
Alberto Ramírez Gallegos, Pedro Juan Tárraga López, Ángel Arturo López-González, Carla Busquets-Cortés, Irene Coll Campayo, Miguel García Samuelsson and José Ignacio Ramírez Manent
Diabetology 2025, 6(11), 137; https://doi.org/10.3390/diabetology6110137 - 4 Nov 2025
Abstract
►▼
Show Figures
Background: Insulin resistance (IR) is a key pathophysiological mechanism linking obesity, type 2 diabetes, and cardiovascular disease. Office workers, due to prolonged sedentary behavior and suboptimal lifestyle patterns, may be particularly susceptible to IR. However, large-scale studies in this occupational group remain scarce.
[...] Read more.
Background: Insulin resistance (IR) is a key pathophysiological mechanism linking obesity, type 2 diabetes, and cardiovascular disease. Office workers, due to prolonged sedentary behavior and suboptimal lifestyle patterns, may be particularly susceptible to IR. However, large-scale studies in this occupational group remain scarce. Objective: To evaluate the prevalence of elevated IR risk using non–insulin-based indices—TyG, METS-IR, and SPISE—and their associations with sociodemographic and lifestyle factors in a large sample of Spanish office workers. Methods: This cross-sectional study included 82,020 office workers from Spain (2021–2022). IR risk was assessed using the TyG index, METS-IR, and SPISE, all derived from fasting biochemical and anthropometric data. Sociodemographic and lifestyle variables were self-reported using validated questionnaires. Sex-stratified analyses and multivariate logistic regression models were performed. Results: Men showed significantly higher odds of elevated IR risk compared to women across all indices: TyG (OR = 2.48, 95% CI: 2.37–2.60), METS-IR (OR = 1.47, 95% CI: 1.38–1.57), and SPISE (OR = 1.88, 95% CI: 1.78–1.99). Smoking, physical inactivity, and low adherence to the Mediterranean diet were independently associated with elevated IR scores, regardless of sex or age. Conclusions: A substantial proportion of office workers exhibit elevated insulin resistance risk, particularly among men and those with unhealthy lifestyles. TyG, METS-IR, and SPISE are valuable, low-cost tools for early IR detection in occupational health settings. These findings support the implementation of preventive strategies targeting modifiable behaviors in sedentary working populations.
Full article
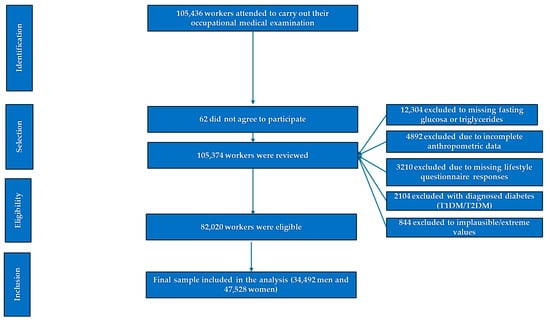
Figure 1
Open AccessArticle
Utilisation of Group-Based Diabetes Education Programmes: Perspectives of Healthcare Practitioners
by
Muili Olugbenga Lawal, Anthony Woodman, Farouk Ayodeji Lawal and Hameedat Olajumoke Omobayo
Diabetology 2025, 6(11), 136; https://doi.org/10.3390/diabetology6110136 - 3 Nov 2025
Abstract
►▼
Show Figures
Background: Structured patient education (SPE) is a critical component of diabetes management, with the potential to reduce its physical, social, and economic burden. National and international guidelines emphasise the importance of raising awareness and equipping individuals with the knowledge and skills necessary
[...] Read more.
Background: Structured patient education (SPE) is a critical component of diabetes management, with the potential to reduce its physical, social, and economic burden. National and international guidelines emphasise the importance of raising awareness and equipping individuals with the knowledge and skills necessary for effective self-management. In the UK, practice nurses are central to this effort, playing a key role in identifying at-risk individuals and facilitating referrals to diabetes education programmes. However, non-attendance at these programmes remains a persistent challenge, undermining the impact of policy initiatives and service provision. Aim of the study: This study aimed to explore practice nurses’ perspectives on the factors contributing to non-attendance at diabetes education centres and to identify potential strategies to improve uptake. Methods: A qualitative approach was employed, involving semi-structured face-to-face interviews with eight practice nurses across six general practice (GP) surgeries in Southeast England. Data were analysed thematically to uncover key patterns and insights. Results: Findings reveal that barriers to attendance are multifaceted, encompassing personal, social, and systemic factors. These include limited patient understanding of the benefits of education, cultural and language differences, scheduling conflicts, and perceived relevance of the programmes. Conclusions: The results highlight the need for a coordinated, patient-centred approach that addresses these challenges through improved communication, flexibility in programme delivery, and enhanced interprofessional collaboration.
Full article

Graphical abstract
Open AccessArticle
The Dutch HbA1c Lifestyle Study (DAF-Study): Seasonal Variation of HbA1c in the Dutch Diabetes Population—Associations with Macronutrient Intake and Physical Activity
by
Erwin Kemna, Henk Bilo, Martine Deckers, Christiaan Slim, Annemarieke Loot, Linda M. Henricks, Jacoline Brinkman, Jody van den Ouweland, Steef Kurstjens, Madeleen Bosma, Iris van Vlodrop, Pauline Verschuure, Jurgen Kooren, Stefan Coolen, Karin Mohrmann, Martin Schuijt, Johannes Krabbe, Robert Wever, Marlies Oostendorp, Ivon van der Linden, Margriet van Kogelenberg, Margo Molhoek, Mieke Koenders, Silvia Endenburg, Roseri de Beer and Cas Weykampadd
Show full author list
remove
Hide full author list
Diabetology 2025, 6(11), 135; https://doi.org/10.3390/diabetology6110135 - 3 Nov 2025
Abstract
►▼
Show Figures
Background/Objectives: Seasonal variation in hemoglobin A1c (HbA1c) values has been previously documented, with physical activity (PA) and macronutrient intake (MNI) suggested as potential drivers. This study combines seasonal mean HbA1c values from the Dutch (pre)diabetes population with national survey data on PA
[...] Read more.
Background/Objectives: Seasonal variation in hemoglobin A1c (HbA1c) values has been previously documented, with physical activity (PA) and macronutrient intake (MNI) suggested as potential drivers. This study combines seasonal mean HbA1c values from the Dutch (pre)diabetes population with national survey data on PA and MNI from 2018 to 2021 to identify key associations. Methods: HbA1c data were collected from 24 laboratory organizations in the Netherlands and Dutch Caribbean. MNI and total energy intake data were extracted from the Dutch National Food Consumption Survey, while PA data came from the Dutch National Sports Participation Index Survey. Weighting factors were applied to align PA and MNI data with HbA1c data. Seasonal averages were analyzed for significant differences, and a prediction model compared PA and MNI with actual HbA1c values. Results: Among 5,635,920 HbA1c results, the average HbA1c increased by 0.71 mmol/mol (NGSP 0.06%) over four years, with an overall mean of 52.4 mmol/mol (NGSP 7.0%). Seasonal HbA1c variation showed a dip in summer–autumn and a peak in winter–spring (1.2 mmol/mol; NGSP 0.11%; p < 0.0001). MNI, except for total energy intake (which peaked in summer; p < 0.001), showed no significant trends or association with HbA1c (p = 0.157). PA decreased by 7.2% over the study period, with seasonal peaks in summer–autumn, showing an inverse relationship with HbA1c (p < 0.0001). During the COVID-19 lockdowns, PA significantly decreased, and mean HbA1c values increased more markedly than in previous years. The prediction model confirmed PA as a significant driver of seasonal HbA1c variation (p = 0.004). Conclusions: These findings suggest that PA is the strongest driver of seasonal variation in HbA1c. Public health initiatives and support programs promoting physical activity are essential for improving HbA1c regulation.
Full article

Graphical abstract
Open AccessArticle
A Qualitative Analysis of First-Year Dental Students’ Opinions on Diabetes Screening in the Dental Setting
by
André Priede, Rodrigo Mariño, Ivan Darby and Phyllis Lau
Diabetology 2025, 6(11), 134; https://doi.org/10.3390/diabetology6110134 - 3 Nov 2025
Abstract
Background: As the global incidence of diabetes continues to rise, expanding the scope of practice for primary healthcare professionals is essential in addressing the type 2 diabetes (T2D) epidemic. Oral health is bidirectionally linked to systemic health, and dentists are in a unique
[...] Read more.
Background: As the global incidence of diabetes continues to rise, expanding the scope of practice for primary healthcare professionals is essential in addressing the type 2 diabetes (T2D) epidemic. Oral health is bidirectionally linked to systemic health, and dentists are in a unique position to engage in preventative activities, such as disease screening. The aim of this study was to investigate first-year dental students’ perceptions of screening for diabetes, and to explore their intentions to implement screening on graduation. Methods: First-year dental students (n = 98) were asked to write an essay about their views and attitudes to diabetes screening in the dental setting. Consent was provided by 51 students for their essays to be thematically analysed. Results: The study found that students’ intentions to perform screening after graduation are shaped by their diabetes knowledge, views on screening protocols, awareness of professional roles, and experience with interprofessional collaboration. Conclusions: The dental setting is an ideal location for increasing opportunistic diabetes screening in primary care. Most first-year dental students viewed diabetes screening favourably and intended to implement after graduation. However, the study indicates changes in dental education and practice are required to equip students with the skills and knowledge needed for diabetes screening. The dental students that participated in this study represent the future dental professionals whose knowledge and attitudes to diabetes and disease screening will determine the future uptake of this initiative.
Full article
Open AccessSystematic Review
Efficacy of Hyperbaric Oxygen Therapy in Diabetic Retinopathy and Macular Edema: A Systematic Review and Meta-Analysis
by
Enrico Moccia, Vincenzo Rizzuto, Pasquale Longobardi, Anita Ferrone, Marco Laurino, Artūrs Zemītis and Giuseppe Covello
Diabetology 2025, 6(11), 133; https://doi.org/10.3390/diabetology6110133 - 1 Nov 2025
Abstract
►▼
Show Figures
Background: Diabetic retinopathy (DR) and diabetic macular edema (DME) are major causes of vision loss in diabetes. Hyperbaric oxygen therapy (HBOT) has been explored as an adjunctive treatment due to its potential to enhance oxygenation, reduce inflammation, and lower oxidative stress in
[...] Read more.
Background: Diabetic retinopathy (DR) and diabetic macular edema (DME) are major causes of vision loss in diabetes. Hyperbaric oxygen therapy (HBOT) has been explored as an adjunctive treatment due to its potential to enhance oxygenation, reduce inflammation, and lower oxidative stress in retinal tissues. This systematic review and meta-analysis assessed HBOT’s efficacy in improving best-corrected visual acuity (BCVA) and central macular thickness (CMT). Methods: A comprehensive search across major databases up to May 2025 identified five eligible studies involving 463 eyes. Results: Pooled data showed HBOT significantly improved BCVA (mean difference—0.05 LogMAR; 95% CI: −0.09 to −0.01; p < 0.05) with no heterogeneity (I2 = 0%), suggesting consistent functional benefit. However, sensitivity analysis revealed this effect was fragile, losing significance when the largest study was excluded. For CMT, HBOT was associated with a significant reduction (−75.21 (95% CI −90.04 to −60.38; p < 0.05), though heterogeneity was high (I2 = 62%), likely due to differences in patient profiles and treatment combinations. Conclusions: While HBOT shows potential in managing DR and DME, further robust randomized trials are needed to validate its clinical utility and define optimal treatment protocols
Full article
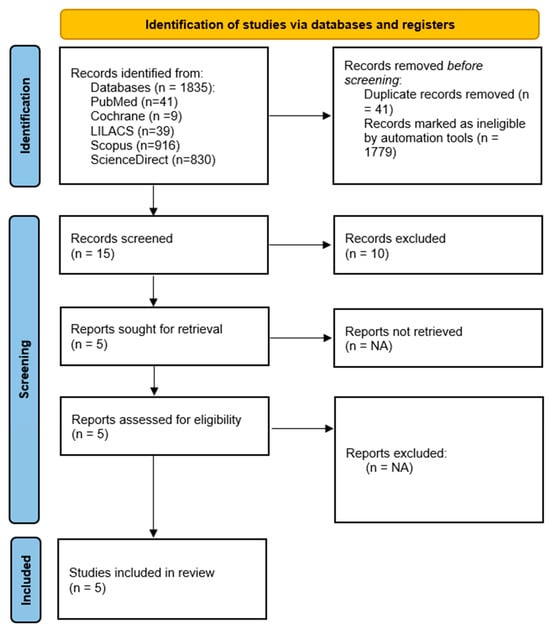
Figure 1
Open AccessArticle
Peripheral Blood Gene Expression Profiling in Proliferative Diabetic Retinopathy Using NanoString Technology
by
Alon Zahavi, Shirel Weiss, Jawad Abu Dbai, Talal Salti and Nitza Goldenberg-Cohen
Diabetology 2025, 6(11), 132; https://doi.org/10.3390/diabetology6110132 - 1 Nov 2025
Abstract
►▼
Show Figures
Background: Proliferative diabetic retinopathy (PDR) is a vision-threatening complication of diabetes characterized by retinal neovascularization. Predicting which diabetic patients will develop PDR remains challenging. Measuring mRNA expression levels may help elucidate the molecular pathways involved in PDR pathogenesis. This study investigated the expression
[...] Read more.
Background: Proliferative diabetic retinopathy (PDR) is a vision-threatening complication of diabetes characterized by retinal neovascularization. Predicting which diabetic patients will develop PDR remains challenging. Measuring mRNA expression levels may help elucidate the molecular pathways involved in PDR pathogenesis. This study investigated the expression of genes related to inflammatory and proliferative pathways in the peripheral blood of patients with PDR, compared to patients with non-proliferative diabetic retinopathy (NPDR) and healthy controls, using NanoString technology. The findings may aid in identifying potential biomarkers and therapeutic targets for early intervention. Methods: This prospective study was approved by the institutional ethics review board, and written informed consent was obtained from all participants. The study included patients with PDR (n = 9), NPDR (n = 8), and non-diabetic controls (n = 6). Total RNA was extracted from whole blood samples using the MagNA Pure Compact RNA Isolation Kit (Roche Ltd., Basel, Switzerland) and analyzed with the NanoString platform (Agentek Ltd., Yakum, Israel). Results: Expression levels of 578 genes across 15 signaling pathways, including inflammation (e.g., IL-17, TNF, and NF-κB) and cancer-related PI3K-Akt pathways, were evaluated. Sixty-six genes (11.5%) were differentially expressed (p < 0.05) between the PDR group and the NPDR and control groups. The most prominently overexpressed genes in PDR included TGFβ1, TGFβ1R, IL23R, BAX, and CFB, which were primarily involved in inflammatory and proliferative signaling. Conclusions: Gene expression profiling using NanoString technology revealed significant upregulation of genes related to inflammation and proliferation in patients with PDR. These findings suggest that beyond angiogenesis, inflammatory and proliferative pathways may play a central role in PDR development and could serve as targets for novel therapeutic strategies.
Full article

Figure 1
Open AccessSystematic Review
The Diabetes-Pancreatic Cancer Risk Relationship over Time: A Systematic Review and Meta-Analysis
by
Araceli Fuentes, Josep Montserrat-Capdevila, Didac Florensa, Sofia Godoy, Judith Serrano and Pere Godoy
Diabetology 2025, 6(11), 131; https://doi.org/10.3390/diabetology6110131 - 1 Nov 2025
Abstract
►▼
Show Figures
Background/Objectives: The relationship between diabetes and pancreatic cancer (PCa) is controversial. In this meta-analysis and systematic review, we investigated diabetes and time since diagnosis as risk factors for PCa. Methods: Cohort and case-control studies were retrieved through a literature search. RevMan
[...] Read more.
Background/Objectives: The relationship between diabetes and pancreatic cancer (PCa) is controversial. In this meta-analysis and systematic review, we investigated diabetes and time since diagnosis as risk factors for PCa. Methods: Cohort and case-control studies were retrieved through a literature search. RevMan 5.4 software and a random effects model were used to estimate summary risks with their 95% confidence intervals (CIs), and the Newcastle–Ottawa Scale (NOS) was used to assess study quality. Results: Included were 23 studies representing 30,875,355 participants and 86,980 cases of PCa. The summary risk for the 14 case-control studies was 2.30 (95% CI: 2.03–2.62) and for the 9 cohort studies was 2.39 (95% CI: 2.09–2.73). The risk decreased with time after diabetes diagnosis: 3.27, 2.25, 1.55, and 1.12 for <2, 2–5, 5–10, and >10 years, respectively, in the case-control studies. The cohort studies also showed an increased risk of PCa in the first 2 years (4.29) and a decrease over time. Quality scores according to the NOS were 6–9 (good and fair quality), for an overall average of 7.82. Conclusions: Diabetes is a risk factor for PCa and this risk is much higher in the 2 years following diabetes diagnosis. In this period, the subgroup of patients who, through clinical follow-up and/or cancer screening, would have better clinical outcomes should be identified. Bearing in mind the poor survival rate for PCa, diabetes interventions focused on preventing onset and delaying progression via modifiable risk factors to reduce PCa incidence.
Full article

Figure 1
Open AccessArticle
Comparative Accuracy of the ECORE-BF Index Versus Non-Insulin-Based Insulin Resistance Markers in over 400,000 Spanish Adults
by
Marta Marina Arroyo, Joan Obrador de Hevia, Ángel Arturo López-González, Pedro J. Tárraga López, Carla Busquets-Cortés and José Ignacio Ramírez-Manent
Diabetology 2025, 6(11), 130; https://doi.org/10.3390/diabetology6110130 - 1 Nov 2025
Abstract
►▼
Show Figures
Background: The early detection of insulin resistance (IR) is critical for the prevention of type 2 diabetes and cardiometabolic diseases. The ECORE-BF index is a simple anthropometric tool for estimating body fat percentage and overweight. However, its potential utility as a predictor of
[...] Read more.
Background: The early detection of insulin resistance (IR) is critical for the prevention of type 2 diabetes and cardiometabolic diseases. The ECORE-BF index is a simple anthropometric tool for estimating body fat percentage and overweight. However, its potential utility as a predictor of IR risk has not been previously evaluated in large populations using validated IR indices. Methods: This cross-sectional study included 418,343 Spanish workers (172,282 women and 246,061 men) who underwent occupational health evaluations. The ECORE-BF index was calculated for all participants, and its association with four validated surrogate markers of IR was analyzed: the triglyceride–glucose index (TyG), TyG-BMI, METS-IR, and SPISE. Subjects were classified into normal or high-risk IR groups based on established cut-off values. We evaluated the mean ECORE-BF values across groups, the prevalence of ECORE-BF-defined obesity, and the diagnostic performance of ECORE-BF using receiver operating characteristic (ROC) curve analysis. Results: Participants with elevated IR index values had significantly higher mean ECORE-BF scores than those with normal values (p < 0.001). The prevalence of ECORE-BF-defined obesity was substantially higher in all high-risk IR groups, exceeding 99% for METS-IR and SPISE in both sexes. ROC analysis demonstrated the high diagnostic accuracy of ECORE-BF in predicting elevated IR risk, with area under the curve (AUC) values ranging from 0.698 (TyG in men) to 0.992 (METS-IR in women). Sensitivity and specificity were also high, particularly for TyG-BMI, SPISE, and METS-IR, with optimal Youden indices above 0.75. Conclusions: ECORE-BF demonstrated high accuracy as a non-invasive tool for identifying individuals at increased insulin resistance risk; however, due to the cross-sectional design, predictive value for incident disease cannot be inferred. Its simplicity, cost-effectiveness, and high diagnostic accuracy support its potential utility in large-scale screening programs for early detection of metabolic risk.
Full article

Figure 1
Open AccessArticle
Prevalence of Liver Steatosis and Fibrosis Assessed by Transient Elastography in a High Cardiovascular-Risk Outpatient Cohort Including T1DM and T2DM Patients
by
Alina N. Saidi, Willy B. Theel, Diederick E. Grobbee, Aart-Jan van der Lely, Femme Dirksmeier-Harinck, Marco Alings, Ellen van der Zwan-van Beek, Simone P. Rauh, Moniba Rasheed and Manuel Castro Cabezas
Diabetology 2025, 6(11), 129; https://doi.org/10.3390/diabetology6110129 - 1 Nov 2025
Abstract
►▼
Show Figures
Background: Metabolic dysfunction-associated steatotic liver disease (MASLD) is common in T2DM, likely due to insulin resistance and obesity. Although screening is recommended in high-risk patients, its prevalence in outpatient cardiovascular clinical settings remains unclear. Methods: We analyzed data from 475 patients attending a
[...] Read more.
Background: Metabolic dysfunction-associated steatotic liver disease (MASLD) is common in T2DM, likely due to insulin resistance and obesity. Although screening is recommended in high-risk patients, its prevalence in outpatient cardiovascular clinical settings remains unclear. Methods: We analyzed data from 475 patients attending a cardiovascular outpatient clinic: 142 with T2DM, 78 with T1DM, and 255 non-diabetic individuals at elevated cardiovascular risk. Liver steatosis and fibrosis were assessed using vibration-controlled transient elastography (Fibroscan®): steatosis by controlled attenuation parameter (CAP ≥ 275 dB/m), and fibrosis risk by liver stiffness measurement (LSM ≥ 8.1 kPa). Carotid intima-media thickness (cIMT) was also measured. Results: The cohort (47% women, mean age 53 years, BMI 29.8 kg/m2) showed MASLD in 39.2% and fibrosis risk in 18.3%. MASLD was most prevalent in T2DM (57.0%), followed by non-diabetics (35.3%) and T1DM (19.2%) (p < 0.001). Fibrosis risk was also highest in T2DM (22.5%) vs. T1DM (7.7%) and non-diabetics (19.2%) (p = 0.02). CAP values were higher in those with fibrosis risk. T2DM patients with MASLD had higher LSM (7.0 ± 3.0 kPa) compared to those without MASLD (5.1 ± 2.2 kPa; p < 0.001). cIMT was highest in T2DM (0.73 ± 0.12 mm; p = 0.04), but not associated with MASLD or fibrosis. BMI and triglycerides were the strongest predictors of both MASLD and fibrosis. Conclusions: MASLD and risk of significant fibrosis were highest among T2DM patients. Within T2DM, those with MASLD had higher LSM, indicating increased risk of fibrosis. The presence of MASLD and risk of significant fibrosis was not associated with cIMT in this cardiometabolic cohort. BMI and plasma TG were consistent predictors across groups urging for more strict control by body weight reduction and lifestyle interventions.
Full article

Graphical abstract
Open AccessArticle
The Symptom Burden of Autonomic Neuropathy Is Associated with Decreased Quality of Life in 6961 People with Diabetes
by
Sigurd Kassow Morsby, Maria Bitsch Poulsen, Esben Bolvig Mark, Johan Røikjer, Amar Nikontovic, Peter Vestergaard and Christina Brock
Diabetology 2025, 6(11), 128; https://doi.org/10.3390/diabetology6110128 - 1 Nov 2025
Abstract
►▼
Show Figures
Background: Diabetes often causes microvascular complications such as neuropathy. Autonomic neuropathy remains under-recognized, and its impact on quality of life (QoL) is unclear. This study investigated associations between symptoms of autonomic dysfunction, including organ-specific subdomains, and QoL in individuals with type 1 (T1D)
[...] Read more.
Background: Diabetes often causes microvascular complications such as neuropathy. Autonomic neuropathy remains under-recognized, and its impact on quality of life (QoL) is unclear. This study investigated associations between symptoms of autonomic dysfunction, including organ-specific subdomains, and QoL in individuals with type 1 (T1D) and type 2 diabetes (T2D). Methods: A cross-sectional population-based survey was conducted in the North Denmark Region among individuals with T1D and T2D, assessing autonomic symptom burden with the Composite Autonomic Symptom Score-31 (COMPASS-31), general well-being with the Short Form Health Survey (SF-36), and psychological well-being with the Hospital Anxiety and Depression Scale. Multivariate linear regression assessed associations between autonomic symptom scores and QoL outcomes. Results: The COMPASS-31 scores were 8.9 (2.9; 22.8) in T1D and 12.4 (5.3; 26.1) in T2D. SF-36 physical composite scores were 52.1 (43.2; 56.4) in T1D and 49.3 (40.3; 54.8) in T2D, with similar mental composite scores (50.7 (40.3; 56.9) vs. 51.4 (41.2; 57.2)). Signs of moderate to severe anxiety were observed in 9.9% (95% confidence interval (CI): 8.1–11.9) of T1D and 8.9% (95% CI: 8.1–9.6) of T2D, while depression was present in 5.9% (95% CI: 4.5–7.6) and 5.1% (95% CI: 4.5–5.7). Higher autonomic symptom burden, especially pupillary, vasomotor, and bladder domains, was associated with lower SF-36 score and higher anxiety and depression scores. Conclusions: the Autonomic symptom burden is associated with reduced QoL and increased psychological distress in individuals with diabetes. These findings emphasize the importance of assessing and managing autonomic symptoms in diabetes care to support overall well-being.
Full article

Graphical abstract
Open AccessArticle
Experience with Oral Semaglutide in Clinical Practice: Efficacy and Safety Data from the Multicentric Croatian Study
by
Klara Ormanac, Tomislav Bozek, Klara Žuljević, Josip Grbavac, Matea Petrinovic, Sanja Klobucar, Silvija Canecki Varzic, Maja Cigrovski Berkovic and Ines Bilic-Curcic
Diabetology 2025, 6(11), 127; https://doi.org/10.3390/diabetology6110127 - 1 Nov 2025
Abstract
►▼
Show Figures
Background: Oral semaglutide is the first oral GLP-1 receptor agonist approved for treating patients with type 2 diabetes mellitus (T2DM). This real-world retrospective study evaluated its effectiveness and tolerability in patients requiring a third-line antidiabetic agent due to poor glucoregulation. Methods: Adult patients
[...] Read more.
Background: Oral semaglutide is the first oral GLP-1 receptor agonist approved for treating patients with type 2 diabetes mellitus (T2DM). This real-world retrospective study evaluated its effectiveness and tolerability in patients requiring a third-line antidiabetic agent due to poor glucoregulation. Methods: Adult patients with T2DM who were taking oral semaglutide and were monitored at tertiary diabetes centers in Croatia were identified through electronic medical records between October 2022 and December 2024. Patients’ data were included in the analysis if they had been on oral semaglutide for at least six months. Results: A total of 163 patients (72 females and 91 males) were recruited, with 96.9% classified as overweight or obese. Among them, 145 had a BMI greater than 30 (mean BMI: 34.18 ± 4.60). The addition of oral semaglutide to their treatment regimen resulted in significant reductions in BMI, HbA1c, and both postprandial and fasting blood glucose levels, as well as in AST and ALT levels (all p < 0.05). There was also an increase in HDL levels (p = 0.007). The side effects observed were consistent with those previously recognized. Conclusions: This study demonstrates that oral semaglutide is safe and effective for glycemic and extraglycemic management in a real-world setting when used as a third-line agent. The best outcomes in terms of weight and HbA1c reduction can be expected when it is introduced early, ideally within the first five years of diabetes duration, and particularly in patients who are insulin naive.
Full article

Graphical abstract
Open AccessSystematic Review
Negative-Pressure Wound Therapy in Diabetic Foot Management: Synthesis of International Randomized Evidence over Two Decades
by
George Theodorakopoulos and David G. Armstrong
Diabetology 2025, 6(11), 126; https://doi.org/10.3390/diabetology6110126 - 1 Nov 2025
Abstract
Background: Diabetic foot ulcers (DFUs) carry high risks of infection, amputation, and mortality. We systematically reviewed randomized controlled trials (RCTs) of negative-pressure wound therapy (NPWT), including single-use systems, for clinically uninfected DFUs (with sensitivity analyses for mixed/infected cohorts). Methods: We searched PubMed and
[...] Read more.
Background: Diabetic foot ulcers (DFUs) carry high risks of infection, amputation, and mortality. We systematically reviewed randomized controlled trials (RCTs) of negative-pressure wound therapy (NPWT), including single-use systems, for clinically uninfected DFUs (with sensitivity analyses for mixed/infected cohorts). Methods: We searched PubMed and Scopus (1 January 2004–30 June 2024). Dual reviewers performed screening and extraction; risk of bias was assessed with Cochrane Risk of Bias 2 (RoB 2) and certainty of evidence with GRADE. When ≥2 trials reported comparable outcomes, we used random-effects meta-analysis. The DiaFu cohort reported in two publications was counted once across analyses. Results: Eleven RCT publications (n = 1699; 10 unique cohorts) met criteria; eight trials (n = 1456) informed the primary endpoint. Trials largely excluded severe ischemia; findings therefore apply mainly to neuropathic or mixed-etiology DFUs with adequate perfusion. NPWT increased complete healing at 12–16 weeks (risk ratio [RR] 1.46, 95% CI 1.21–1.76; I2 = 48%) and shortened time to healing (mean difference –18 days, 95% CI −28 to −8). Effects were similar for conventional and single-use NPWT. Outcomes did not vary systematically within commonly used pressure ranges (approximately −80 to −125 mmHg). Only two RCTs reported direct cost data (exploratory). Moderate heterogeneity (Higgins’ I2 48–68%) reflected variation in ulcer severity, device type/settings, dressing-change frequency, and off-loading protocols. Conclusions: NPWT probably improves short-term healing of clinically uninfected DFUs compared with standard care and may reduce minor amputations, without increasing adverse events. Certainty is moderate for healing and low for most secondary outcomes. Benefits appear consistent across device classes and may support earlier discharge and community-based care. Evidence gaps include ischemia-dominated ulcers, long-term outcomes (recurrence and limb preservation), adherence mechanisms, and contemporary cost-effectiveness.
Full article
(This article belongs to the Special Issue Prevention and Care of Diabetic Foot Ulcers)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Knowledge and Practices in Diabetic Foot Ulcer Prevention Among Patients with Diabetes Mellitus in Gauteng, South Africa
by
Tshifhiwa Mukheli, Tshepo P. Mokoena, Shingirai B. Kagodora and Thifhelimbilu E. Luvhengo
Diabetology 2025, 6(11), 125; https://doi.org/10.3390/diabetology6110125 - 1 Nov 2025
Abstract
Background: Patients with diabetes mellitus are at increased risk of foot ulcerations. Prevention and timeous treatment of diabetic foot ulcer requires a multidisciplinary team, including patients and healthcare workers. The study investigated levels of knowledge regarding foot care and prevention of diabetic foot
[...] Read more.
Background: Patients with diabetes mellitus are at increased risk of foot ulcerations. Prevention and timeous treatment of diabetic foot ulcer requires a multidisciplinary team, including patients and healthcare workers. The study investigated levels of knowledge regarding foot care and prevention of diabetic foot ulcer in patients with diabetes mellitus. Methods: We conducted a cross-sectional descriptive study using structured face-to-face interviews of patients seen at the outpatient department. Interviews covered socio-demographic and clinical characteristics, and foot care practices. Statistical analysis was performed using STATA 15. Results: The study involved 245 participants with a mean age of participants was 53.7 (SD) years, and 69% were female. The majority, 77.6%, had Type 2 diabetic mellitus (DM). Mean score of appropriate knowledge on diabetic foot ulcer (DFU) was 73.5%, lower scores were 44.9% and 45.7% for moisturizing between toes and wearing slippers outdoors, respectively. Knowledge of foot care was significantly influenced by age (p = 0.0033), duration of DM (p = 0.047), treatment type (p = 0.002), prior education on foot care (p < 0.0001), and existence of foot complications (p = 0.030). Conclusions: Younger patients and those with Type 1 diabetes mellitus had less knowledge of appropriate foot care and prevention of DFU. We recommend the implementation of structured and targeted educational interventions.
Full article
(This article belongs to the Special Issue Innovations in the Identification, Prevention and Management of Diabetes-Related Foot Complications)
Open AccessReview
How the Salutogenic Pattern of Health Reflects in Type 2 Diabetes Mellitus: A Narrative Review
by
Sandra Mijač, Ksenija Vitale, Karmen Lončarek and Goran Slivšek
Diabetology 2025, 6(11), 124; https://doi.org/10.3390/diabetology6110124 - 1 Nov 2025
Abstract
By 2045, approximately 783.2 million people are projected to be diagnosed with type 2 diabetes mellitus (T2DM). In addition, obesity is expected to affect up to 22% of the world’s population or one in four people. The diabesity epidemic, a worrying trend in
[...] Read more.
By 2045, approximately 783.2 million people are projected to be diagnosed with type 2 diabetes mellitus (T2DM). In addition, obesity is expected to affect up to 22% of the world’s population or one in four people. The diabesity epidemic, a worrying trend in which T2DM and obesity co-occur, is becoming increasingly evident and could be the most significant epidemic of non-communicable chronic diseases in human history. The salutogenic pattern of health, which emphasises well-being and resistance resources, could be a promising solution to address this alarming worldwide problem. The salutogenic pattern of health has numerous positive effects on the health of persons with T2DM. These include reducing the risk of it, lowering some biomarkers and laboratory parameters related to its control, and promoting a better lifestyle, ultimately improving the overall quality of life. The salutogenic pattern of health offers an effective and evidence-based approach to address the growing global problem of chronic non-communicable diseases such as T2DM. Integrating this theory into standard modern medical practice has the potential to significantly improve health outcomes and overall patient well-being, making it an important direction for modern medicine. Accordingly, the aim is to explore and analyse the salutogenic pattern of health associated with T2DM in order to prevent it, but also the better management of it.
Full article
(This article belongs to the Special Issue Lifestyle Behavior Intervention for Diabetes Prevention and Management: 2nd Edition)
►▼
Show Figures

Figure 1
Open AccessArticle
A Mathematical Modeling Approach to Estimate Blood Glucose Behavior in Individuals with Prediabetes
by
Alexis Alonso-Bastida, Dolores Azucena Salazar-Piña, Manuel Adam-Medina, Lourdes Gutiérrez-Xicotencatl, Christian Ríos-Enríquez, Margarita Ramos-García and Daniel Villanueva-Vásquez
Diabetology 2025, 6(11), 123; https://doi.org/10.3390/diabetology6110123 - 29 Oct 2025
Abstract
►▼
Show Figures
Background: Glucose homeostasis is a crucial physiological process, and its disruption is closely linked to the onset of Type 2 Diabetes Mellitus (T2DM), a major global health issue. Objective: This study presents a novel mathematical model to describe glucose dynamics in
[...] Read more.
Background: Glucose homeostasis is a crucial physiological process, and its disruption is closely linked to the onset of Type 2 Diabetes Mellitus (T2DM), a major global health issue. Objective: This study presents a novel mathematical model to describe glucose dynamics in both healthy individuals and those with prediabetic risk factors. Methods: We analyzed 311 days of continuous glucose monitoring data from 43 participants (14 healthy and 29 at risk, aged 25–55), using a Dual Extended Kalman Filter to estimate parameters and unmeasurable variables, while accounting for parametric variability. We applied the Levenberg–Marquardt algorithm to minimize estimation error. Results: Based on average parameter values and standardized inputs, 311 simulations were conducted, showing strong agreement with experimental data (r = 0.98, p < 0.01). Conclusions: The model provides an accurate representation of glucose regulation and serves as a valuable in-silico tool for advancing preventive strategies against T2DM, marking one of the first models specifically tailored to individuals with prediabetes.
Full article

Graphical abstract
Open AccessArticle
Machine Learning for Causal Inference in Hospital Diabetes Care: TMLE Analysis of Selection Bias in Diabetic Foot Infection Treatment—A Cautionary Tale
by
Rim Hur and Robert Rushakoff
Diabetology 2025, 6(11), 122; https://doi.org/10.3390/diabetology6110122 - 28 Oct 2025
Abstract
Background/Objectives: Diabetic foot infections (DFIs) are a leading cause of hospitalization, amputation, and costs among patients with diabetes. Although early treatment is assumed to reduce complications, its real-world effects remain uncertain. We applied a causal machine-learning (ML) approach to investigate whether early DFI
[...] Read more.
Background/Objectives: Diabetic foot infections (DFIs) are a leading cause of hospitalization, amputation, and costs among patients with diabetes. Although early treatment is assumed to reduce complications, its real-world effects remain uncertain. We applied a causal machine-learning (ML) approach to investigate whether early DFI treatment improves hospitalization and clinical outcomes. Methods: We conducted an observational study using de-identified UCSF electronic health record (EHR) data from 1434 adults with DFI (2015–2024). Early treatment (<3 days after diagnosis) was compared to delayed/no treatment (≥3 days or none). Outcomes included DFI-related hospitalization and lower-extremity amputation (LEA). Confounders included demographics, comorbidities, antidiabetic medication use, and laboratory values. We applied Targeted Maximum Likelihood Estimation (TMLE) with SuperLearner, a machine-learning ensemble. Results: Early treatment was associated with higher hospitalization risk (TMLE risk difference [RD]: 0.293; 95% CI: 0.220–0.367), reflecting the triage of clinically sicker patients. In contrast, early treatment showed a protective trend against amputation (TMLE RD: −0.040; 95% CI: −0.098 to 0.066). Results were consistent across estimation methods and robust to bootstrap validation. A major limitation is that many patients likely received treatment outside UCSF, introducing uncertainty around exposure classification. Conclusions: Early treatment of DFIs increased hospitalization but reduced amputation risk, a paradox reflecting appropriate clinical triage and systematic exposure misclassification from fragmented healthcare records. Providers prioritize the sickest patients for early intervention, leading to greater short-term utilization but potentially preventing irreversible complications. These findings highlight a cautionary tale; even with causal ML, single-institution analyses may misrepresent treatment effects, underscoring the need for causally informed decision support and unified EHR data.
Full article
(This article belongs to the Special Issue Diabetes Management in the Hospital: Applications of Artificial Intelligence)
►▼
Show Figures
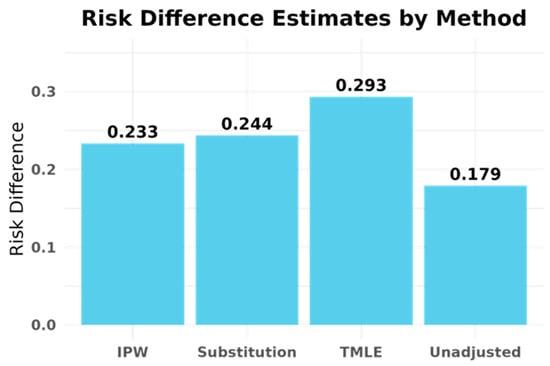
Figure 1
Open AccessArticle
Prevalence of Alcohol Use Disorder Among Hospital Admissions with Type 2 Diabetes in Spain: Trends from 2016 to 2023 and Predictors of Hospitalization and In-Hospital Mortality
by
Lucia Jiménez-Sierra, Ana López-de-Andres, Valentín Hernández-Barrera, Rodrigo Jiménez-Garcia, David Carabantes-Alarcon, Andrés Bodas-Pinedo, Hikaru Kobayashi-García and José J. Zamorano-León
Diabetology 2025, 6(10), 121; https://doi.org/10.3390/diabetology6100121 - 20 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Alcohol consumption is a major public health concern, particularly among individuals with type 2 diabetes (T2D), due to its impact on morbidity and mortality. However, alcohol use disorder (AUD) among hospitalized T2D patients in Spain remains understudied. This study analyzed trends
[...] Read more.
Background/Objectives: Alcohol consumption is a major public health concern, particularly among individuals with type 2 diabetes (T2D), due to its impact on morbidity and mortality. However, alcohol use disorder (AUD) among hospitalized T2D patients in Spain remains understudied. This study analyzed trends in AUD prevalence in adults hospitalized with T2D (2016–2023), identified associated factors, and assessed predictors of in-hospital mortality (IHM). Methods: We conducted a retrospective observational study using the Spanish National Hospital Discharge Database. Adults (≥18 years) with T2D were included. Joinpoint regression and multivariable logistic regression were applied. Results: Among 5,192,189 hospital admissions with T2D, 326,433 (6.29%) had AUD. Prevalence increased from 5.05% in 2016 to 7.52% in 2023 (annual percent change 5.95%; p < 0.05). AUD was more frequent in men (9.99%) than women (1.12%). Rising trends were observed for smoking (67.9% to 70.6%), cocaine use (2.0% to 3.15%), and cannabinoid use (1.08% to 1.78%) (all p < 0.001). Factors strongly associated with AUD included male sex (aOR 5.67; 95% CI 5.60–5.75), age 50–64 years, smoking (aOR 3.68 in men; 5.61 in women), cocaine use (aOR 4.55 in men; 7.68 in women), and mental disorders. IHM was 7.0% in T2D with AUD, peaking at 7.85% in 2020. Higher IHM was associated with age ≥ 80 years, hypoglycemia, and COVID-19, while obesity and mental disorders were linked to lower IHM. Conclusions: AUD prevalence in hospital admission with T2D in Spain is high and rising, particularly among women, with concomitant substance use also increasing. Comprehensive, sex-sensitive strategies are urgently needed in both hospital and outpatient care.
Full article

Figure 1
Open AccessReview
The Cardiovascular and Macrovascular Benefits of Achieving Early Type 2 Diabetes Remission
by
Lianna Khachikyan and Jay H. Shubrook
Diabetology 2025, 6(10), 120; https://doi.org/10.3390/diabetology6100120 - 17 Oct 2025
Abstract
Type 2 diabetes is a chronic non-communicable disease that has reached epidemic levels. While there is ample evidence that type 2 diabetes can, for many, be prevented or at least well managed, this disease progresses in most people with type 2 diabetes who
[...] Read more.
Type 2 diabetes is a chronic non-communicable disease that has reached epidemic levels. While there is ample evidence that type 2 diabetes can, for many, be prevented or at least well managed, this disease progresses in most people with type 2 diabetes who are not achieving glucose targets. Those who do not achieve glucose targets have higher rates of microvascular and macrovascular complications. Further, the economic burden of diabetes, its treatment and its complications is substantial. Diabetes management goals should include prevention in those at risk and early intensive control to induce benefits through the legacy effect. However, what is seen more often is therapeutic inertia with delays in the diagnosis and each step of care. This results in reactive diabetes management in which the disease progresses faster than the management. While the use of newer potent glucose-lowering agents continues to expand, the durability of these agents when treatment is stopped is unknown. In this narrative review, the authors explore the impact of achieving diabetes remission on the reduction in cardiovascular complications.
Full article
(This article belongs to the Special Issue Early Intervention and Treatment Strategies for Diabetes)
►▼
Show Figures

Graphical abstract
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Diabetology
Obesity and Diabetes: Healthy Lifestyle Choices
Guest Editors: Elena Gangitano, Maria Irene BelliniDeadline: 15 November 2025
Special Issue in
Diabetology
New Perspectives and Future Challenges in Diabetic Retinopathy
Guest Editor: Akifumi KushiyamaDeadline: 30 November 2025
Special Issue in
Diabetology
Current Understanding of Gender Differences in Diabetes and Rheumatological Diseases
Guest Editors: Giancarlo Tonolo, Daniela MarottoDeadline: 15 December 2025
Special Issue in
Diabetology
Feature Papers in Diabetology 2025
Guest Editor: Peter CliftonDeadline: 31 December 2025