Circulating Anti-Insulin Antibodies Protect Against Nocturnal Hypoglycemia in Patients with Type 2 Diabetes Treated with Long-Acting Insulin Analogues
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Glucose Monitoring
2.3. Anti-Insulin Antibodies
2.4. Statistical Analysis
2.5. Approval of This Study
3. Results
3.3. Nocturnal Hypoglycemia in Diabetic Patients
3.4. Daytime Hypoglycemia
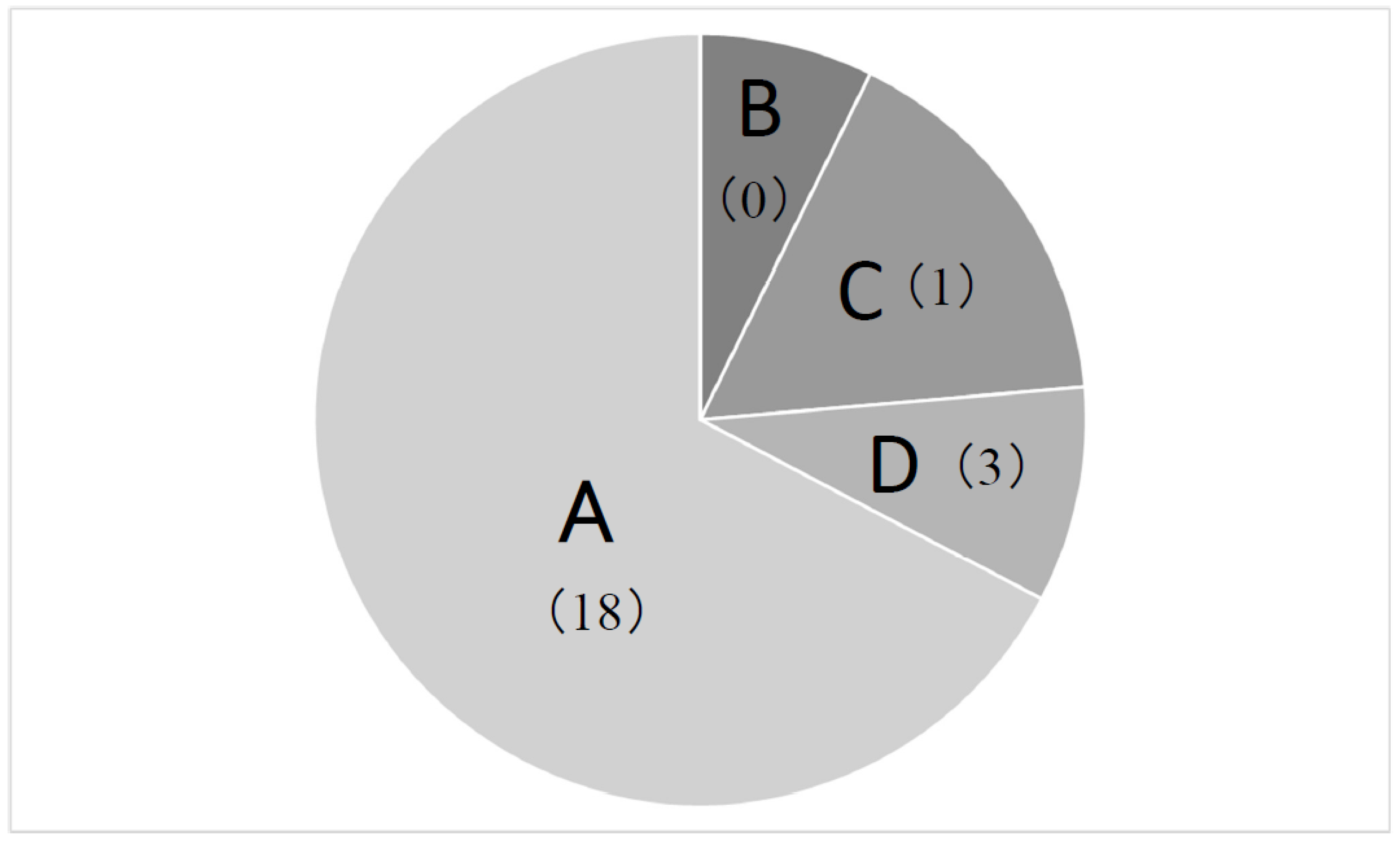
3.5. Positivity of AIA in Hypoglycemia
3.6. Types of Insulin Preparations and Nocturnal Hypoglycemia
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nathan, D.M.; Buse, J.B.; Davidson, M.B.; Ferrannini, E.; Holman, R.R.; Sherwin, R.; Zinman, B.; American Diabetes Association; European Association for Study of Diabetes. Medical management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: A consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009, 32, 193–203. [Google Scholar] [CrossRef]
- Owens, D.R.; Traylor, L.; Mullins, P.; Landgraf, W. Patient-level meta-analysis of efficacy and hypoglycemia in people with type 2 diabetes initiating insulin glargine 100 U/mL or neutral protamine Hagedorn insulin analyzed according to concomitant oral antidiabetes therapy. Diabetes Res. Clin. Pract. 2017, 124, 57–65. [Google Scholar] [CrossRef]
- Goldman, J.; Kapitza, C.; Pettus, J.; Heise, T. Understanding how pharmacokinetic and pharmacodynamic differences of basal analog insulins influence clinical practice. Curr. Med. Res. Opin. 2017, 33, 1821–1831. [Google Scholar] [CrossRef]
- Freemantle, N.; Chou, E.; Frois, C.; Zhuo, D.; Lehmacher, W.; Vlajnic, A.; Wang, H.; Chung, H.W.; Zhang, Q.; Wu, E.; et al. Safety and efficacy of insulin glargine 300 u/mL compared with other basal insulin therapies in patients with type 2 diabetes mellitus: A network meta-analysis. BMJ Open 2016, 6, e009421. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.; Bernjak, A.; Williams, S.; Fawdry, R.A.; Hibbert, S.; Freeman, J.; Sheridan, P.J.; Heller, S.R. Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Diabetes 2014, 63, 1738–1747. [Google Scholar] [CrossRef]
- Frier, B.M. Hypoglycemia in diabetes mellitus: Epidemiology and clinical implications. Nat. Rev. Endocrinol 2014, 10, 711–7228. [Google Scholar] [CrossRef] [PubMed]
- Graveling, A.J.; Frier, B.M. The risk of nocturnal hypoglycaemia in insulin–treated diabetes. Diabetes Res. Clin. Pract. 2017, 133, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Crane, P.K.; Walker, R.; Hubbard, R.A.; Li, G.; Nathan, D.M.; Zheng, H.; Haneuse, S.; Zheng, H.; Haneuse, S.; Craft, S.; et al. Glucose levels and risk of dementia. N. Engl. J. Med. 2013, 369, 540–546. [Google Scholar] [CrossRef]
- Murata, Y.; Kadoya, Y.; Yamada, S.; Sanke, T. Cognitive impairment in elderly patients with type 2 diabetes mellitus: Prevalence and related clinical factors. Diabetol. Int. 2016, 8, 193–198. [Google Scholar] [CrossRef]
- Tamagawa, E.; Matsuoka, Y.; Kadoya, Y.; Yamada, S.; Fujita, A.; Sanke, T. Prevalence of serum anti-insulin antibodies and clinical features in patients with type 2 diabetes treated with insulin analogues. J. Jpn. Diabetes Soc. 2023, 66, 247–253. [Google Scholar]
- International Hypoglycaemia Study Group. Glucose Concentrations of Less Than 3.0 mmol/L (54 mg/dL) Should Be Reported in Clinical Trials: A Joint Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2017, 40, 155–157. [Google Scholar] [CrossRef]
- Morita, S.; Shimajiri, Y.; Matsuoka, Y.; Kadoya, Y.; Yamada, S.; Matsuoka, T.; Sanke, T. Exploring genetic risk factors for β-cell deterioration in type 2 diabetes mellitus: Insights from longitudinal C-peptide analysis. Diabetes Res. Clin. Pract. 2025, e222, 112049. [Google Scholar] [CrossRef]
- Bailey, T.; Bode, B.W.; Christiansen, M.P.; Klaff, L.J.; Alva, S. The performance and usability of a factory calibrated Flash Glucose Monitoring System. Diabetes Technol. Ther. 2015, 17, 787–794. [Google Scholar] [CrossRef]
- Battelino, T.; Danne, T.; Bergenstal, R.M.; Amiel, S.A.; Beck, R.; Biester, T.; Bosi, E.; Buckingham, B.A.; Cefalu, W.T.; Close, K.L.; et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations from the International Consensus on Time in Range. Diabetes Care 2019, 42, 1593–1603. [Google Scholar] [CrossRef]
- Chehregosha, H.; Khamseh, M.E.; Malek, M.; Hosseinpanah, F.; Ismail-Beigi, F. A view beyond HbA1c: Role of continuous glucose monitoring. Diabetes Ther. 2019, 10, 853–863. [Google Scholar] [CrossRef]
- Service, F.J.; Molnar, G.D.; Rosevear, J.W.; Ackerman, E.; Gatewood, L.C.; Taylor, W.F. Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes 1970, 19, 644–655. [Google Scholar] [CrossRef]
- Unger, J.; Parkin, C. Hypoglycemia in insulin-treated diabetes: A case for increased vigilance. Postgrad. Med. 2011, 123, 81–91. [Google Scholar] [CrossRef]
- Matsuda, M.; DeFronzo, R.A. Insulin sensitivity induces obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care 1999, 22, 1462–1470. [Google Scholar] [CrossRef] [PubMed]
- Clamp, L.D.; Hume, D.J.; Lambert, E.V.; Kroff, J. Enhanced insulin sensitivity in successful, long-term weight loss maintainers compared with matched controls with no weight loss history. Nutr. Diabetes 2017, 7, e282. [Google Scholar] [CrossRef] [PubMed]
- Scatchard, G. The attraction of proteins for small molecules and ions. Ann. N. Y. Acad. Sci. 1949, 51, 600–665. [Google Scholar] [CrossRef]
- Hu, X.; Chen, F. Exogenous insulin antibody syndrome (EIAS): A clinical syndrome associated with insulin antibodies induced by exogenous insulin in diabetic patients. Endocr. Connect. 2018, 7, R47–R55. [Google Scholar] [CrossRef]
- Hirata, Y.; Uchigata, Y. Insulin autoimmune syndrome in Japan. Diabetes Res. Clin. Pract. 1994, 24, S153–S157. [Google Scholar] [CrossRef]
- Dong, Z.Y.; Feng, J.H.; Zhang, J.F. Efficacy and Tolerability of Insulin Degludec Versus Other Long-acting Basal Insulin Analogues in the Treatment of Type 1 and Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis. Clin. Ther. 2022, 44, 1520–1533. [Google Scholar] [CrossRef]
- Pedersen-Bjergaard, U.; Agesen, R.M.; Brøsen, J.M.B.; Alibegovic, A.C.; Andersen, H.U.; Beck-Nielsen, H.; Gustenhoff, P.; Hansen, T.K.; Hedetoft, C.; Jensen, T.J.; et al. Comparison of treatment with insulin degludec and glargine U100 in patients with type 1 diabetes prone to nocturnal severe hypoglycaemia: The HypoDeg randomized, controlled, open-label, crossover trial. Diabetes Obes. Metab. 2022, 24, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Alhmoud, E.N.; Saad, M.O.; Omar, N.E. Efficacy and safety of insulin glargine 300 units/mL vs insulin degludec in patients with type 1 and type 2 diabetes: A systematic review and meta-analysis. Front. Endocrinol. 2024, 14, 1285147. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.; Bajaj, H.S.; Lingvay, I.; Heller, S.R. Clinical perspectives on the frequency of hypoglycemia in treat-to-target randomized controlled trials comparing basal insulin analogs in type 2 diabetes: A narrative review. BMJ Open Diabetes Res. Care 2024, 12, e003930. [Google Scholar] [CrossRef] [PubMed]
| N | 55 |
|---|---|
| Gender (% of male) | 63.6 |
| Age (years old) | 68.1 ± 11.5 |
| Body mass index (kg/m2) | 23.7 ± 3.9 |
| Years after diagnosis (years) | 23.0 ± 10.2 |
| HbA1c (%) | 8.0 ± 1.0 |
| Fasting serum C-peptide (ng/mL) $ (N = 42) | 0.93 ± 0.85 |
| eGFR (mL/min/1.73 m2) | 62.6 ± 19.8 |
| Dose of basal insulin (Unit/kg/day) | 0.20 ± 0.07 |
| Injection time of basal insulin (N) | |
| At breakfast | 16 |
| At bedtime | 39 |
| Nocturnal Hypoglycemia | (+) | (−) | p |
|---|---|---|---|
| N | 13 | 42 | |
| Clinical factors | |||
| Gender (% of male) | 53.8 | 66.7 | 0.536 |
| Age (years old) | 72.4 ± 11.0 | 66.8 ± 11.4 | 0.129 |
| Years after diagnosis (years) | 24.1 ± 8.0 | 22.7 ± 10.9 | 0.636 |
| Body mass index (kg/m2) | 21.5 ± 2.9 | 24.4 ± 3.9 | 0.015 |
| HbA1c (%) | 7.7 ± 1.0 | 8.1 ± 1.0 | 0.203 |
| Fasting serum C-peptide (ng/mL) $ | 0.68 ± 0.62 | 0.99 ± 0.84 | 0.265 |
| (N = 8) | (N = 34) | ||
| eGFR (mL/min/1.73 m2) | 60.6 ± 14.6 | 63.3 ± 21.2 | 0.377 |
| Dose of basal insulin (Unit/kg/day) | 0.21 ± 0.05 | 0.20 ± 0.07 | 0.620 |
| Positivity of anti-insulin antibodies (%) | 7.7 (1/13) | 50.0 (21/42) | 0.009 |
| Injection time of long-acting insulin | 61.5 (5:8) | 73.8 (11:31) | 0.489 |
| % of bedtime (at morning:at bedtime) | |||
| CGM metrics | |||
| For whole day monitoring glucose | |||
| Average glucose (mg/dL) | 167 ± 35 | 198 ± 47 | 0.033 |
| CV (%) | 46.3 ± 10.8 | 31.9 ± 6.2 | <0.001 # |
| MAGE (mg/dL) | 131 ± 31 | 116 ± 38 | 0.192 |
| For Daytime monitoring glucose | |||
| Average glucose (mg/dL) | 181 ± 38 | 207 ± 53 | 0.101 |
| TAR (%) | 42.3 ± 18.8 | 59.1 ± 25.6 | 0.034 |
| TIR (%) | 50.8 ± 17.1 | 39.8 ± 25.1 | 0.146 |
| TBR (%) [TIL + TIVL] | 6.9 ± 10.0 | 1.2 ± 2.4 | 0.002 # |
| TIL (%) | 3.2 ± 3.7 | 1.0 ± 1.9 | 0.005 # |
| TIVL (%) | 3.7 ± 7.6 | 0.2 ± 0.6 | 0.001 # |
| For Nocturnal monitoring glucose | |||
| Average glucose (mg/dL) | 124 ± 38 | 174 ± 46 | 0.017 |
| TAR (%) | 18.9 ± 15.7 | 42.0 ± 29.2 | 0.009 |
| TIR (%) | 58.9 ± 28.6 | 57.1 ± 28.6 | 0.905 |
| TBR (%) [TIL + TIVL] | 22.2 ± 24.1 | 1.0 ± 2.2 | <0.001 # |
| TIL (%) | 9.8 ± 8.4 | 1.0 ± 2.2 | <0.001 # |
| TIVL (%) | 12.4 ± 20.7 | 0 | <0.001 # |
| Explanatory Variable | Standard Partial Regression Coefficient | Odds Ratio (95% CI) | p |
|---|---|---|---|
| Daytime hypoglycemia (0: negative, 1: positive) | 1.379 | 23.694 (2.431 to 230.865) | 0.006 |
| Body mass index (%) | −0.733 | 0.825 (0.610 to 1.116) | 0.213 |
| HbA1c (%) | 0.382 | 1.492 (0.420 to 5.294) | 0.536 |
| Anti-insulin antibodies (0: negative, 1: positive) | −1.263 | 0.076 (0.007 to 0.879) | 0.039 |
| Basal insulin dose (10× Unit/kg/day) | −0.177 | 0.974 (0.834 to 1.139) | 0.742 |
| Daytime Hypoglycemia | (+) | (−) | p |
|---|---|---|---|
| N | 14 | 41 | |
| Clinical factor | |||
| Gender (% of male) | 50.0 | 68.3 | 0.335 |
| Age (years old) | 71.6 ± 12.0 | 67.0 ± 11.2 | 0.189 |
| Years after diagnosis (years) | 24.6 ± 7.6 | 22.5 ± 11.0 | 0.520 |
| Body mass index (kg/m2) | 21.9 ± 2.8 | 24.3 ± 4.0 | 0.038 |
| HbA1c (%) | 7.4 ± 0.8 | 8.2 ± 1.0 | 0.013 |
| Fasting serum C-peptide (ng/mL) $ | 0.75 ± 0.76 | 0.98 ± 0.82 | 0.396 |
| (N = 10) | (N = 32) | ||
| eGFR (mL/min/1.73 m2) | 60.0 ± 15.3 | 63.5 ± 21.2 | 0.568 |
| Dose of basal insulin (Unit/kg/day) | 0.22 ± 0.06 | 0.19 ± 0.07 | 0.148 |
| Positivity of anti-insulin antibodies (%) | 28.6 (4/14) | 43.9 (18/41) | 0.361 |
| Injection time of long-acting-insulin % of bedtime (at morning:at bedtime) | 64.3 (5:9) | 73.2 (11:30) | 0.519 |
| CGM metrics | |||
| For whole day monitoring glucose | |||
| Average glucose (mg/dL) | 153 ± 33 | 204 ± 43 | <0.001 |
| CV (%) | 43.1 ± 10.0 | 32.6 ± 8.1 | <0.001 |
| MAGE (mg/dL) | 116 ± 37 | 120 ± 37 | 0.737 |
| For Nocturnal monitoring glucose | |||
| Average glucose (mg/dL) | 126 ± 39 | 175 ± 46 | 0.001 # |
| TAR (%) | 19.7 ± 18.3 | 42.3 ± 29.0 | 0.009 |
| TIR (%) | 63.5 ± 24.4 | 55.5 ± 27.6 | 0.337 |
| TBR (%) [TIL + TIVL] | 16.8 ± 24.5 | 2.3 ± 6.3 | <0.001 # |
| TIL (%) | 6.7 ± 7.2 | 1.8 ± 4.7 | <0.001 # |
| TIVL (%) | 10.1 ± 20.7 | 0.5 ± 1.9 | <0.001 # |
| For Daytime monitoring glucose | |||
| Average glucose (mg/dL) | 160 ± 35 | 216 ± 47 | <0.001 |
| TAR (%) | 30.9 ± 16.4 | 57.2 ± 22.0 | <0.001 |
| TIR (%) | 51.7 ± 22.5 | 39.2 ± 23.7 | 0.014 |
| TBR (%) [TIL + TIVL] | 8.6 ± 9.0 | 0.4 ± 0.5 | <0.001 # |
| TIL (%) | 4.7 ± 3.5 | 0.4 ± 0.5 | <0.001 # |
| TIVL (%) | 3.9 ± 7.2 | 0 | <0.001 # |
| Explanatory Variable | Standard Partial Regression Coefficient | Odds Ratio (95% CI) | p |
|---|---|---|---|
| Nocturnal hypoglycemia (0: negative, 1: positive) | 1.377 | 25.600 (2.858 to 228.555) | 0.004 |
| Body mass index (kg/m2) | −0.119 | 0.969 (0.731 to 1.285) | 0.828 |
| HbA1c (%) | −1.341 | 0.246 (0.075 to 0.803) | 0.020 |
| Anti-insulin antibodies (0: negative, 1: positive) | 0.223 | 1.577 (0.193 to 12.904) | 0.671 |
| Basal insulin dose (10× Unit/kg/day) | 0.885 | 1.140 (0.994 to 1.308) | 0.062 |
| Anti-Insulin Antibodies | (+) | (−) | p |
|---|---|---|---|
| N | 22 | 33 | |
| Clinical factor | |||
| Gender (% of male) | 63.6 | 63.6 | 1.000 |
| Age (years old) | 65.5 ± 10.4 | 69.9 ± 11.9 | 0.172 |
| Years after diagnosis (years) | 22.9 ± 11.3 | 23.1 ± 9.6 | 0.941 |
| Body mass index (kg/m2) | 24.2 ± 3.3 | 23.4 ± 4.2 | 0.448 |
| HbA1c (%) | 8.1 ± 1.0 | 7.9 ± 1.0 | 0.426 |
| Fasting serum C-peptide (ng/mL) $ | 0.91 ± 0.76 | 0.81 ± 0.65 | 0.685 |
| (N = 15) | (N = 25) | ||
| eGFR (mL/min/1.73 m2) | 59.5 ± 19.5 | 64.7 ± 19.9 | 0.341 |
| Dose of basal insulin (Unit/kg/day) | 0.20 ± 0.08 | 0.20 ± 0.06 | 0.864 |
| Injection time of long-acting-insulin % of bedtime (at morning:at bedtime) | 77.3 (5:17) | 66.7 (11:22) | 0.547 |
| Frequency of patients with hypoglycemia | |||
| Nocturnal hypoglycemia (%) | 4.5 (1/22) | 36.4 (12/33) | 0.009 |
| Daytime hypoglycemia (%) | 18.2 (4/22) | 27.3 (9/33) | 0.528 |
| CGM metrics | |||
| For whole day monitoring glucose | |||
| Average glucose (mg/dL) | 191 ± 38 | 191 ± 51 | 0.946 |
| CV (%) | 32.3 ± 6.9 | 37.3 ± 10.8 | 0.122 # |
| MAGE (mg/dL) | 109 ± 33 | 126 ± 38 | 0.086 |
| For Nocturnal monitoring glucose | |||
| Average glucose (mg/dL) | 173 ± 38 | 155 ± 54 | 0.173 |
| TAR (%) | 40.2 ± 25.8 | 34.0 ± 30.0 | 0.430 |
| TIR (%) | 58.8 ± 25.2 | 56.6 ± 28.2 | 0.773 |
| TBR (%) [TIL + TIVL] | 0.95 ± 2.53 | 9.34 ± 18.2 | 0.005 # |
| TIL (%) | 0.86 ± 2.21 | 4.54 ± 6.93 | 0.005 # |
| TIVL (%) | 0.09 ± 0.44 | 4.80 ± 14.10 | 0.007 # |
| For Daytime monitoring glucose | |||
| Average glucose (mg/dL) | 199 ± 45 | 203 ± 54 | 0.751 |
| TAR (%) | 53.9 ± 24.9 | 55.9 ± 25.7 | 0.779 |
| TIR (%) | 44.5 ± 23.8 | 41.0 ± 24.1 | 0.596 |
| TBR (%) [TIL + TIVL] | 1.58 ± 2.93 | 3.14 ± 6.94 | 0.641 # |
| TIL (%) | 1.30 ± 2.28 | 1.67 ± 2.79 | 0.738 # |
| TIVL (%) | 0.28 ± 0.77 | 1.47 ± 5.01 | 0.398 # |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanke, T.; Matsuoka, Y.; Kadoya, Y.; Yamada, S.; Tamagawa, E.; Fujita, A. Circulating Anti-Insulin Antibodies Protect Against Nocturnal Hypoglycemia in Patients with Type 2 Diabetes Treated with Long-Acting Insulin Analogues. Diabetology 2025, 6, 138. https://doi.org/10.3390/diabetology6110138
Sanke T, Matsuoka Y, Kadoya Y, Yamada S, Tamagawa E, Fujita A. Circulating Anti-Insulin Antibodies Protect Against Nocturnal Hypoglycemia in Patients with Type 2 Diabetes Treated with Long-Acting Insulin Analogues. Diabetology. 2025; 6(11):138. https://doi.org/10.3390/diabetology6110138
Chicago/Turabian StyleSanke, Tokio, Yuko Matsuoka, Yoshiki Kadoya, Shoichi Yamada, Eri Tamagawa, and Atsuyo Fujita. 2025. "Circulating Anti-Insulin Antibodies Protect Against Nocturnal Hypoglycemia in Patients with Type 2 Diabetes Treated with Long-Acting Insulin Analogues" Diabetology 6, no. 11: 138. https://doi.org/10.3390/diabetology6110138
APA StyleSanke, T., Matsuoka, Y., Kadoya, Y., Yamada, S., Tamagawa, E., & Fujita, A. (2025). Circulating Anti-Insulin Antibodies Protect Against Nocturnal Hypoglycemia in Patients with Type 2 Diabetes Treated with Long-Acting Insulin Analogues. Diabetology, 6(11), 138. https://doi.org/10.3390/diabetology6110138





