Topical Advisory Panel applications are now closed. Please contact the Editorial Office with any queries.
Journal Description
Antibiotics
Antibiotics
is an international, peer-reviewed, open access journal on all aspects of antibiotics, published monthly online by MDPI. The Croatian Pharmacological Society (CPS) is affiliated with Antibiotics and its members receive discounts on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, PMC, Embase, CAPlus / SciFinder, and other databases.
- Journal Rank: JCR - Q1 (Infectious Diseases) / CiteScore - Q1 (General Pharmacology, Toxicology and Pharmaceutics )
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 15 days after submission; acceptance to publication is undertaken in 2.6 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Impact Factor:
4.6 (2024);
5-Year Impact Factor:
4.9 (2024)
Latest Articles
Surveillance of Healthcare-Associated Infections in the WHO African Region: Systematic Review of Literature from 2011 to 2024
Antibiotics 2025, 14(12), 1287; https://doi.org/10.3390/antibiotics14121287 (registering DOI) - 18 Dec 2025
Abstract
►
Show Figures
Background: Evidence on HAIs in Africa is fairly common. Objectives: The main objective was to identify the surveillance tools used for healthcare–associated infections (HAIs) in countries in the WHO African Region. Secondary objectives focused on the organization of surveillance, the pathogens involved, and
[...] Read more.
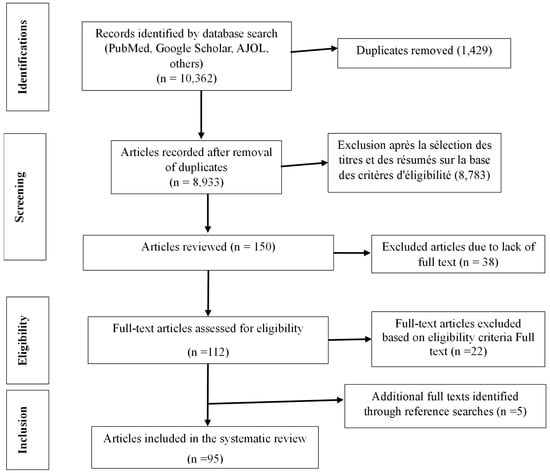
Background: Evidence on HAIs in Africa is fairly common. Objectives: The main objective was to identify the surveillance tools used for healthcare–associated infections (HAIs) in countries in the WHO African Region. Secondary objectives focused on the organization of surveillance, the pathogens involved, and the frequency of multidrug–resistant species. Inclusion and exclusion criteria: Observational or interventional studies on healthcare–associated infections in humans, published between January 2011 and December 2024, in French or English, were included. However, the following publications were not included: animal studies, healthcare–associated infections not related to healthcare, literature reviews, studies outside the period or geographical area, and studies in languages other than French or English. Sources of information and search date: The databases consulted were PubMed, Web of Science, EMBASE, Cochrane, African Index Medicus, Google Scholar, and AJOL. The search was conducted between January and March 2025. Risk of bias assessment: The risk of bias was assessed using a specific grid (eleven criteria), scored from one (low) to three (high). The studies were classified into three levels of methodological quality. The results of the bias assessment showed that the publications were excellent (strong and moderate) with a cumulative rate of 99.9%. Methods of synthesizing results: Data were extracted using a standardized grid and synthesized narratively. No meta–analysis was performed. Number of studies and characteristics: 95 studies were included, mostly cross–sectional studies (82.1%), cohorts (10.4%), and a few case reports. Most were from West Africa (60.0%), particularly Nigeria (16.8%) and South Africa (14.7%). Main results: • Most common pathogens: Staphylococcus aureus (53.7%), Escherichia coli (43.2%), Klebsiella pneumoniae (32.6%). • Resistance profile: ESBL (27.4%), MRSA (21.1%), multidrug resistance (13.7%). • Sources of HAIs: mainly exogenous (83.2%). • Laboratory methods: phenotypic (70.5%), genotypic or genomic rare (3.1%). • Scope of studies: local (96.8%), national (3.2%). Limitations of evidence: Risk of bias due to underreporting of HAIs, methodological heterogeneity, predominance of cross–sectional studies, low use of molecular methods, lack of modeling, and uneven geographical coverage. Overall interpretation and implications: surveillance of HAIs in Africa remains fragmented and poorly standardized. There is a need to strengthen national systems, integrate molecular methods, train professionals, and promote interventional research. The WHO GLASS program can serve as a framework for harmonizing surveillance.
Full article
Open AccessReview
Recent Advances in Endolysin Engineering
by
Mackenzie Aitken, Gayan Abeysekera, Craig Billington and Renwick C. J. Dobson
Antibiotics 2025, 14(12), 1285; https://doi.org/10.3390/antibiotics14121285 (registering DOI) - 18 Dec 2025
Abstract
Antimicrobial resistance threatens a new “dark age” in medical practice. Chronic antibiotic overuse has driven the rise in antimicrobial resistance and promoted the emergence of multidrug-resistant organisms. To address this problem, researchers have developed new approaches. Antimicrobials derived from bacteriophage, which are viruses
[...] Read more.
Antimicrobial resistance threatens a new “dark age” in medical practice. Chronic antibiotic overuse has driven the rise in antimicrobial resistance and promoted the emergence of multidrug-resistant organisms. To address this problem, researchers have developed new approaches. Antimicrobials derived from bacteriophage, which are viruses that target bacteria, are promising candidates. Amongst these candidates, bacteriophage enzymes used in the viral replication cycle are of significant interest. Specifically, endolysins are used by bacteriophage to lyse the bacterial cell wall, leading to structural collapse and cell lysis. Researchers are increasingly applying these proteins externally to multidrug-resistant organisms as a novel antimicrobial treatment. Following this increased interest, many studies have presented protein engineering methods to further enhance the effectiveness of endolysins as antimicrobials. These methods include attachment of membrane-permeabilizing peptides, domain-swapping, and catalytic-site modification. Recent advances in all three fields have seen the implementation of tools like novel in silico design pipelines and library-based screening methods. This review summarizes these recent advances in the rapidly developing field of endolysin engineering and discusses potential future directions in this field.
Full article
(This article belongs to the Special Issue Bacteriophages and Phage-Derived Enzymes as Antibacterial Agents)
►▼
Show Figures
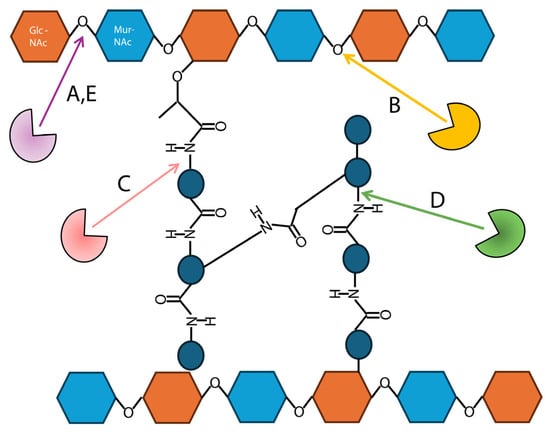
Figure 1
Open AccessReview
Extended-Spectrum β-Lactamase-Producing Escherichia coli and Pediatric UTIs: A Review of the Literature and Selected Experimental Observations
by
Vanessa Tamas, Erlinda R. Ulloa, Monika Kumaraswamy, Samira Dahesh, Raymond Zurich, Victor Nizet and Alison Coady
Antibiotics 2025, 14(12), 1284; https://doi.org/10.3390/antibiotics14121284 (registering DOI) - 18 Dec 2025
Abstract
►▼
Show Figures
Urinary tract infections (UTIs) are common in children and are predominantly caused by uropathogenic Escherichia coli (UPEC). An increasing proportion of these strains produce extended-spectrum β-lactamases (ESBLs), which render β-lactam antibiotics ineffective. Interestingly, some patients with ESBL-producing UTIs improve clinically following treatment with
[...] Read more.
Urinary tract infections (UTIs) are common in children and are predominantly caused by uropathogenic Escherichia coli (UPEC). An increasing proportion of these strains produce extended-spectrum β-lactamases (ESBLs), which render β-lactam antibiotics ineffective. Interestingly, some patients with ESBL-producing UTIs improve clinically following treatment with antibiotics like cephalexin, despite demonstrated in vitro resistance. Working alongside and at times synergistically with antibiotics, host immune factors, such as the antimicrobial peptide cathelicidin (LL-37), contribute to bacterial clearance through direct killing and inhibition of biofilm formation. In this review, we summarize the current understanding of pediatric ESBL-producing UPEC infections and present selected in vitro and in vivo experimental data evaluating the combined effects of LL-37 and cephalexin on clinical isolates. Although no synergy was observed, ESBL-producing isolates demonstrated reduced bacterial burden in vivo compared to a non-ESBL UPEC strain. These findings suggest that host immune factors and environmental conditions may influence the fitness and virulence of drug-resistant UTI pathogens, warranting further investigation.
Full article
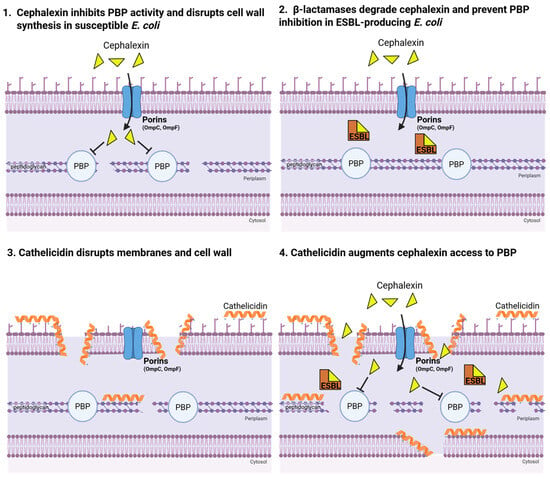
Figure 1
Open AccessArticle
Pathogen-Specific Actinium-225 and Lutetium-177 Labeled Antibodies for Treatment of Biofilm-Associated Implant Infections: Initial In Vivo Proof-of-Concept
by
F. Ruben H. A. Nurmohamed, Kevin J. H. Allen, Mackenzie E. Malo, Connor Frank, J. Fred F. Hooning van Duvenbode, Berend van der Wildt, Alex J. Poot, Marnix G. E. H. Lam, Jos A. G. van Strijp, Peter G. J. Nikkels, H. Charles Vogely, Harrie Weinans, Ekaterina Dadachova and Bart C. H. van der Wal
Antibiotics 2025, 14(12), 1283; https://doi.org/10.3390/antibiotics14121283 (registering DOI) - 18 Dec 2025
Abstract
Background: the primary challenge with implant infections is the formation of biofilm, which harbors dormant bacteria that reduce the effectiveness of antibiotics and amplify antibiotic resistance, exacerbating the global antimicrobial resistance crisis. A potential novel treatment strategy is radioimmunotherapy, which uses antibodies linked
[...] Read more.
Background: the primary challenge with implant infections is the formation of biofilm, which harbors dormant bacteria that reduce the effectiveness of antibiotics and amplify antibiotic resistance, exacerbating the global antimicrobial resistance crisis. A potential novel treatment strategy is radioimmunotherapy, which uses antibodies linked to radioisotopes to deliver targeted radiation to the bacteria and biofilm. We describe the first in vivo use of targeted radiation therapy, employing Actinium-225 (α-radiation) and Lutetium-177 (β-radiation) labeled antibodies to treat a Staphylococcus aureus biofilm-associated intramedullary implant infection. Untargeted radiation in the form of unbound radionuclide treatment was also evaluated. Methods: to assess therapeutic efficacy, bacterial counts were performed on implant and surrounding bone after seven days of follow-up. Biodistribution was evaluated using SPECT/CT and ex vivo gamma counting. Results: radioimmunotherapy using an antibody against wall teichoic acid which was labeled with Actinium-225 and Lutetium-177 achieved bacterial reductions between 45% and 93% on the implant and surrounding bone. Surprisingly, a similar antimicrobial effect was observed with unbound Actinium-225 treatment reducing the bacterial load by 80% on the implant and 98% in the surrounding bone. Indications of maximum tolerated dose (MTD) with Lutetium-177 labeled antibodies were observed through hepatic and renal function evaluations. Conclusions: These results should be interpreted in the context of the study’s constraints, particularly the limited animal sample size. Nonetheless, the results suggest that in vivo applied radiation may help reduce a biofilm-associated infection at the implant site as well as in the surrounding bone. These findings encourage further investigation into the use of targeted and non-targeted radiation, potentially combined with antibiotics, to develop effective strategies for eradicating biofilm-associated implant infections.
Full article
(This article belongs to the Special Issue Challenges of Antibiotic Resistance: Biofilms and Anti-Biofilm Agents)
►▼
Show Figures
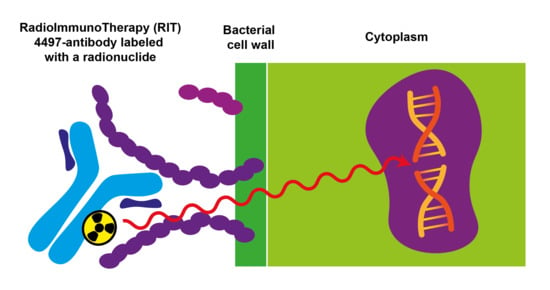
Graphical abstract
Open AccessArticle
Prevalence and Patterns of Antibiotic Prescribing Among Children Aged 1–7 Years in Primary Health Care Centers in Prishtina and Ferizaj, Kosovo (2022–2025): A Retrospective Observational Study
by
Fitim Bexhet Alidema, Arieta Hasani Alidema, Lirim Shefki Mustafa, Mirlinda Havolli and Fellenza Abazi
Antibiotics 2025, 14(12), 1282; https://doi.org/10.3390/antibiotics14121282 - 18 Dec 2025
Abstract
Background: The inappropriate and empirical use of antibiotics in early childhood remains a major global public health concern, contributing significantly to the rise of antimicrobial resistance (AMR). In Kosovo, the COVID-19 pandemic further influenced prescribing behaviors in primary care, increasing the reliance on
[...] Read more.
Background: The inappropriate and empirical use of antibiotics in early childhood remains a major global public health concern, contributing significantly to the rise of antimicrobial resistance (AMR). In Kosovo, the COVID-19 pandemic further influenced prescribing behaviors in primary care, increasing the reliance on symptom-based treatment in the absence of laboratory confirmation and age-appropriate formulations. Aim: This study aimed to assess the prevalence and patterns of antibiotic prescribing among children aged 1–7 years in primary health care centers in Prishtina and Ferizaj from January 2022 to December 2025, and to compare regional differences in prescribing practices and guideline adherence. Methods: A retrospective observational study was conducted using data from the national electronic health record system and protocol books. All pediatric visits for children aged 1–7 years with infectious diagnoses were included. Descriptive statistics, Chi-square tests, and multivariable logistic regression were used to evaluate prescribing prevalence, demographic and seasonal variations, and independent predictors of antibiotic use, including assessment of appropriateness based on international pediatric guidelines. Results: Of 4320 pediatric visits, 1328 (30.7%) resulted in an antibiotic prescription. Prescribing prevalence was higher in Ferizaj (34.2%) than in Prishtina (28.5%, p < 0.01). Amoxicillin–clavulanic acid (42.9%) and amoxicillin (21.5%) were the most frequently prescribed agents, while macrolides (11.7% vs. 6.2%) and cephalosporins (7.9% vs. 3.4%) were more common in Ferizaj. Only 61.4% of prescriptions were fully guideline-concordant. Younger age (1–3 years), winter season, and residence in Ferizaj were independently associated with higher odds of receiving an antibiotic. Conclusions: Pediatric antibiotic prescribing in Kosovo remains high and predominantly empirical, reflecting real-world limitations in diagnostic capacity and formulation availability. Significant proportions of partially appropriate and inappropriate prescriptions highlight the need for standardized pediatric guidelines, improved diagnostic support, and strengthened stewardship initiatives within primary care.
Full article
(This article belongs to the Special Issue Antibiotics for Primary Care Practice)
Open AccessArticle
Navigating Antimicrobial Resistance Insights: An In-Depth Analysis of Healthcare Providers’ Knowledge, Attitudes, and Practices, with an Emphasis on Precision Medicine in Pakistan
by
Sidra Shahid, Aiman Athar, Shahzeen Farooq, Madena Yahya, Muhammad Saad Ashraf, Shafaq Mahmood and Abdul Momin Rizwan Ahmad
Antibiotics 2025, 14(12), 1281; https://doi.org/10.3390/antibiotics14121281 - 18 Dec 2025
Abstract
Antibiotics play a crucial role in the treatment of many complicated problems in clinical medicine, but antimicrobial resistance (AMR) has emerged as a serious concern threatening to undermine its effectiveness. Precision medicine (PM) which tailors treatment to individual and genetic and lifestyle factors,
[...] Read more.
Antibiotics play a crucial role in the treatment of many complicated problems in clinical medicine, but antimicrobial resistance (AMR) has emerged as a serious concern threatening to undermine its effectiveness. Precision medicine (PM) which tailors treatment to individual and genetic and lifestyle factors, may offer a novel approach to combat AMR. Yet, little is known about how healthcare providers in Pakistan understand and integrate the concept of precision medicine within their knowledge, attitudes, and practices (KAP) towards AMR. This study aims to investigate the knowledge, attitude, and practices of healthcare professionals towards AMR and to explore their perception about precision medicine as a strategy to reduce AMR. A mixed method approach was employed for the study. The knowledge, attitude, and practices (KAP) of healthcare professionals (N = 326) were assessed through a validated questionnaire. SPSS version 26 (Statistical Package for the Social Sciences) was employed for descriptive and bivariate analyses to determine KAP score and its association with demographics. Qualitative data were gathered through a focus group discussion and thematic analysis was performed to explore the perception about PM. Results showed that healthcare professionals demonstrate poor knowledge (55.5%), relatively positive attitudes (54.6%), and that nearly half had unfavorable practices (48.3%). Significant associations (p < 0.05) were found between KAP scores and factors such as location, healthcare setting, educational level, professional designation, and prior infectious disease training. During focus group discussion (FGD), HCPs emphasized the cautious use of PM, particularly in the management of resistant infections. However, limitations in resources, poor governance, poverty, and access to data and testing facilities were highlighted as barriers in the implementation of PM into practice. This study highlights critical gaps in knowledge and practices towards AMR among HCPs. While PM is viewed as a potential tool against AMR, systemic support, resource allocation, and targeted awareness programs are essential to integrate PM into clinical practice.
Full article
(This article belongs to the Special Issue Antibiotic Resistance: From the Bench to Patients, 2nd Edition)
►▼
Show Figures
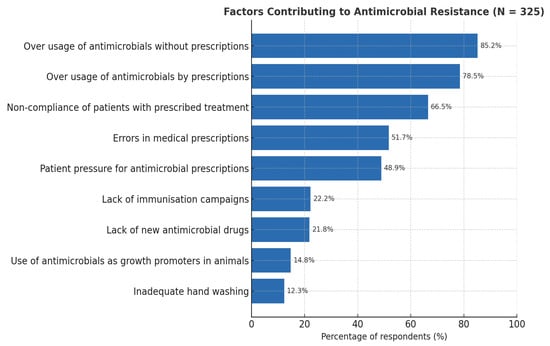
Figure 1
Open AccessArticle
Efficacy of Dual-Antibiotic-Loaded Bone Cement Against Multi-Drug-Resistant Staphylococcus aureus and Enterococcus faecalis in a Galleria mellonella Model of Periprosthetic Joint Infection
by
You Zhao, Gopala Krishna Mannala, Raphaëlle Youf, Martina Humez, Ruth Schewior, Klaus-Dieter Kühn, Volker Alt and Martijn Riool
Antibiotics 2025, 14(12), 1280; https://doi.org/10.3390/antibiotics14121280 - 17 Dec 2025
Abstract
Background: Antibiotic-loaded bone cement (ALBC) is widely used for local antibiotic delivery in joint arthroplasty to prevent and treat prosthetic joint infections (PJIs). In this study, we evaluated the efficacy of cemented Kirschner (K)-wires coated with various ALBC formulations using a Galleria mellonella
[...] Read more.
Background: Antibiotic-loaded bone cement (ALBC) is widely used for local antibiotic delivery in joint arthroplasty to prevent and treat prosthetic joint infections (PJIs). In this study, we evaluated the efficacy of cemented Kirschner (K)-wires coated with various ALBC formulations using a Galleria mellonella infection model against multidrug-resistant (MDR) Staphylococcus aureus and Enterococcus faecalis. Methods: We tested commercially available bone cements, including gentamicin-only formulations (PALACOS R+G) and dual-antibiotic formulations, combining gentamicin with either clindamycin (COPAL G+C) or vancomycin (COPAL G+V), alongside an antibiotic-free control (PALACOS R). In vitro assays—including minimum inhibitory/bactericidal concentration (MIC/MBC) determination, antibiotic release kinetics, agar diffusion, and antibiofilm evaluations—demonstrated effective antibiotic release and significant antimicrobial activity against both planktonic and biofilm-associated bacteria. Results: In vivo, ALBC-coated K-wires were well tolerated in G. mellonella and significantly protected the larvae from S. aureus infection compared to controls. Notably, dual-antibiotic formulations provided superior protection, correlating with substantial reductions in bacterial colonisation on implant surfaces and in surrounding tissues. Conclusions: These findings support the utility of the G. mellonella model as a high-throughput, cost-effective platform for the preclinical evaluation of antimicrobial strategies to prevent and treat PJIs and further demonstrate the effectiveness of dual-loaded ALBC against multidrug-resistant bacteria.
Full article
(This article belongs to the Special Issue Experimental Models and Novel Therapies for Difficult-to-Treat Biofilm-Associated Infections)
►▼
Show Figures
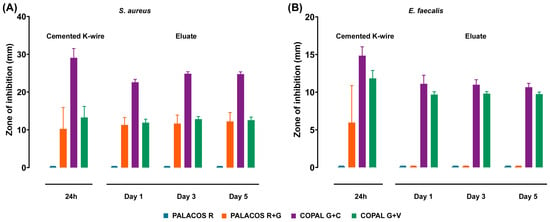
Figure 1
Open AccessReview
Antibiotic Prophylaxis and Postoperative Therapy in Tooth Extractions for Patients at Risk of Medication-Related Osteonecrosis of the Jaw (MRONJ): A Scoping Review
by
Selene Barone, Alessandro Antonelli, Antonio Madonna, Amerigo Giudice, Massimo Borelli and Francesco Bennardo
Antibiotics 2025, 14(12), 1279; https://doi.org/10.3390/antibiotics14121279 - 17 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Although several studies have reported antibiotic protocols for the prevention of medication-related osteonecrosis of the jaw (MRONJ) in patients receiving antiresorptive and/or antiangiogenic therapy following tooth extraction, it remains unclear which protocol is the most effective. Accordingly, this scoping review analyzed
[...] Read more.
Background/Objectives: Although several studies have reported antibiotic protocols for the prevention of medication-related osteonecrosis of the jaw (MRONJ) in patients receiving antiresorptive and/or antiangiogenic therapy following tooth extraction, it remains unclear which protocol is the most effective. Accordingly, this scoping review analyzed antibiotic use in dental extractions in these patients, focusing on whether antibiotic duration influences MRONJ occurrence. Methods: Two authors independently searched PubMed, Scopus, and Web of Science (2003–2025). Out of the 770 studies screened, 36 were included. Descriptive statistics, a meta-analysis comparing MRONJ incidence in patients treated with high-dose (HD) and low-dose (LD) antiresorptive treatment according to the therapeutic indication and generalized linear mixed models on antibiotic duration were obtained (α = 0.05). Results: Amoxicillin, alone or with clavulanic acid, was the most used antibiotic, and in 8 studies it was combined with metronidazole. Seven studies reported parenteral antibiotic administration. Median antibiotic duration was 1.5 days pre-extraction, 5.5 days post-extraction, and 7 days overall. MRONJ risk was significantly higher in HD than LD patients (95% CI: 1.46–5.43; p = 0.002), and antibiotic duration was positively associated with reduced MRONJ risk in HD patients (β = –0.15, p = 0.026; OR = 0.86, 95% CI: 0.75–0.98). Conclusions: The literature shows heterogeneous antibiotic protocols for MRONJ prevention. The increased MRONJ risk and greater protective effect of antibiotics in HD patients suggest that patient risk profile may be more relevant than the antibiotic regimen.
Full article
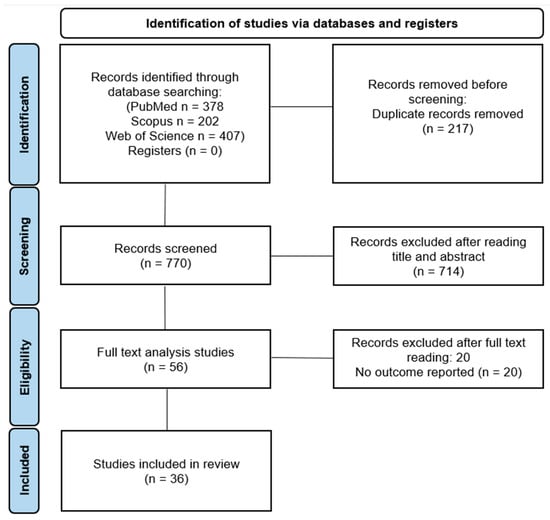
Figure 1
Open AccessArticle
Occurrence of Virulence and Antibiotic Resistance in Pseudomonas aeruginosa Isolated from the Environmental Water from Tamaulipas, Mexico
by
Jessica I. Licea-Herrera, Abraham Guerrero, Paulina Guel, Virgilio Bocanegra-García, Gildardo Rivera and Ana Verónica Martínez-Vázquez
Antibiotics 2025, 14(12), 1278; https://doi.org/10.3390/antibiotics14121278 - 17 Dec 2025
Abstract
Background/Objectives: Antibiotic-resistant strains have been reported in aquatic ecosystems, with varying prevalence and resistance patterns by region. In Tamaulipas, Mexico, little information has been generated on this topic, making it difficult to estimate their potential risk to environmental and human health. Therefore, the
[...] Read more.
Background/Objectives: Antibiotic-resistant strains have been reported in aquatic ecosystems, with varying prevalence and resistance patterns by region. In Tamaulipas, Mexico, little information has been generated on this topic, making it difficult to estimate their potential risk to environmental and human health. Therefore, the objective of this study was to evaluate the presence and virulence of antibiotic-resistant strains of Pseudomonas aeruginosa in environmental water from Tamaulipas, Mexico. Methods: One hundred water samples were collected from different water bodies in Tamaulipas to identify P. aeruginosa by PCR and MALDI-TOF, virulence gene detection, antimicrobial susceptibility testing, and detection class 1 integrons. Results: In this study, 109 P. aeruginosa strains were isolated. Eight virulence genes were identified in 47.7% to 80.7% of the strains, with the rhlAB gene being the most frequent. The strains showed resistance or intermedia resistance to 10 of the 16 antibiotics tested, in a range of resistance values 0.9–66.2%. In total, 100% (109/109) were susceptible to ceftazidime (CAZ), gentamicin (GM), amikacin (AN), netilmicin (NET), tobramycin (NN) and norfloxacin (NOR), and 65.7% were resistant to ticarcillin/clavulanic acid and 53.5% to ticarcillin; the resistance to the remaining antibiotics was between 19.4% and 0.9%. The class 1 integron was not identified in any of the strains analyzed. Conclusions:P. aeruginosa in environmental waters of Tamaulipas showed potential to cause infections and low rates of resistance to most of the antibiotics tested. However, 20% were resistant to one of the most common treatments, which could pose a risk to public health.
Full article
(This article belongs to the Special Issue Drivers of Virulence and Antimicrobial Resistance in Emerging and Re-Emerging Pathogens)
►▼
Show Figures
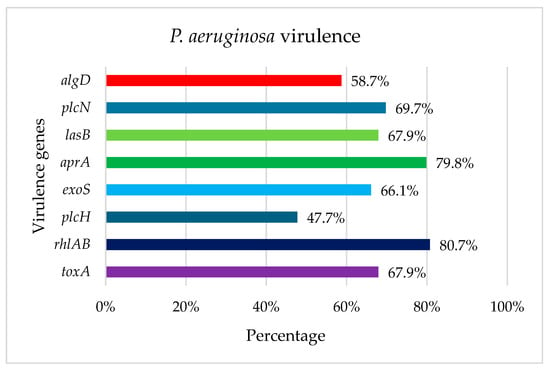
Figure 1
Open AccessArticle
Exploring the Value of Paired Microbiology and Histology in Chronic Osteomyelitis and Fracture-Related Infections
by
Anton A. N. Peterlin, Martin McNally, Nicole L. Henriksen, Sophie A. Blirup-Plum, Ann Jørgensen, Andreas Ibrahim Jørgensen, Inger Brock, Hans Gottlieb and Louise K. Jensen
Antibiotics 2025, 14(12), 1277; https://doi.org/10.3390/antibiotics14121277 - 16 Dec 2025
Abstract
Background: Microbiological culture and histology are gold standards for diagnosing chronic osteomyelitis (cOM) and fracture-related infection (FRI). This study investigated whether combining these modalities within a single tissue sample provides additional insight into disease severity. We hypothesized that high neutrophil and osteoclast
[...] Read more.
Background: Microbiological culture and histology are gold standards for diagnosing chronic osteomyelitis (cOM) and fracture-related infection (FRI). This study investigated whether combining these modalities within a single tissue sample provides additional insight into disease severity. We hypothesized that high neutrophil and osteoclast numbers correlate with culture-positive microbiology and that double-positive samples may indicate more severe disease. Methods: In this prospective single-centre study, adults undergoing surgery for confirmed FRI or cOM were included. Clinical and disease classification data (FRI and BACH) were recorded. Five deep-tissue samples were collected intraoperatively and divided for paired microbiological culture and histological assessment of neutrophil infiltration, according to international diagnostic guidelines. Results: Forty-one patients were included (11 cOM, 30 FRI) of whom 68% received preoperative antibiotics. Nineteen patients (46%) were identified as culture-positive, while 32 patients (78%) were histologically positive according to international diagnostic guidelines, respectively. Among the 205 samples, 31% were culture-positive, 56% histology-positive, and 26% double-positive. Histological scores were significantly higher in culture-positive samples (p < 0.001). Treatment failure occurred in seven patients (18%), all with FRI. Paired positive samples were associated with increased odds of clinical failure and earlier revision, with odds increasing 1.68-fold for each additional paired positive sample (95% CI, 1.10–2.77). Conclusions: The paired analysis demonstrated a strong concordance between culture-positivity and suppurative inflammation within the same sample. Combining microbiology and histology may help identify patients at increased risk of revision and enhance diagnostic certainty, particularly in patients identified as culture-negative.
Full article
(This article belongs to the Special Issue Diagnostics and Antibiotic Therapy in Bone and Joint Infections)
►▼
Show Figures
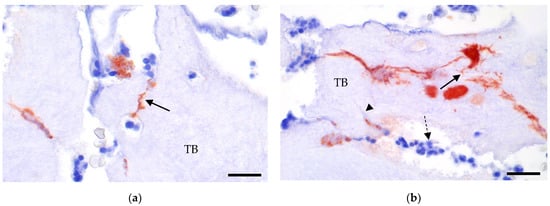
Figure 1
Open AccessArticle
Multidrug Resistance in Bacterial Isolates from Clinical Samples Submitted to a National Veterinary Diagnostic Facility in Uganda (2014–2020): A Retrospective Analysis
by
Steven Kakooza, Michael Mahero, Damien F. N. Munyiirwa, Wilfred Eneku, Esther Nabatta, Paul Ssajjakambwe, Grace Athieno, Dorcus Namuyinda, Edrine B. Kayaga, Howard Onyuth, Edward M. Wampande, Francis Mutebi and John B. Kaneene
Antibiotics 2025, 14(12), 1276; https://doi.org/10.3390/antibiotics14121276 - 16 Dec 2025
Abstract
Background/Objectives: Antimicrobial Resistance (AMR) is a pressing global animal and public health challenge. There is limited data on AMR prevalence, trends, and drivers in bacterial pathogens from animal sources in Uganda. Thus, this study investigated the occurrence and factors associated with multidrug resistance
[...] Read more.
Background/Objectives: Antimicrobial Resistance (AMR) is a pressing global animal and public health challenge. There is limited data on AMR prevalence, trends, and drivers in bacterial pathogens from animal sources in Uganda. Thus, this study investigated the occurrence and factors associated with multidrug resistance (MDR) in bacterial isolates recovered from clinical samples of animals submitted to the national veterinary diagnostic laboratory in Uganda. Methods: A retrospective study analyzed antibiogram data of bacteria from animal samples submitted to the Central Diagnostic Laboratory, Makerere University in Uganda between 2014 and 2020. The cleaned dataset comprised 590 cases with antibiogram data. Statistical analyses were conducted using R software version 4.5.2. Results: Gram-negative bacteria were predominant (74.4%) among the samples from clinical cases. The overall MDR proportion in the general bacteria population was 41.7% over the seven-year period. Among the clinically relevant bacteria, MDR was highest in Escherichia coli (57.2%), followed by Staphylococcus aureus (35.8%) and Salmonella (15.5%). Univariable screening of predictors hypothesized that MDR was influenced by year of case submission, animal host type, and bacterial group (p < 0.05). Multivariable logistic regression showed that isolates submitted in 2019 (vs. 2015) had significantly higher odds of MDR (aOR = 4.21; 95% CI: 1.62–13.14), indicating a marked temporal increase in resistance. Gram-negative bacteria (vs. Gram-positives) were also more likely to exhibit MDR (aOR = 1.62; 95% CI: 1.07–2.48). Conclusions: The high occurrence of MDR in bacterial pathogens from animal clinical submissions revealed the need for improved antimicrobial stewardship and integrated AMR surveillance in Uganda, particularly within the central region from which most diagnostic samples originated.
Full article
(This article belongs to the Special Issue Antimicrobial Resistance and Infections in Animals)
►▼
Show Figures

Figure 1
Open AccessArticle
Analysis of the Concordance Between the Use of Phenotypic Screening Tests with the β-Lactamase Gene Profile in Selected Gram-Negative Bacteria
by
Patrycja Głowacka, Izabela Marczuk, Patrycja Wójcicka, Monika Ogórkiewicz, Marta Ciesielska, Dorota Żakowska, Paweł Rutyna, Anna Koszczyńska, Marta Łączyńska, Natalia Podsiadły, Emilia Paziewska and Beata Cieśluk-Olchowska
Antibiotics 2025, 14(12), 1275; https://doi.org/10.3390/antibiotics14121275 - 16 Dec 2025
Abstract
Background: There are many methods of identifying microbial resistance to therapeutic agents; however, they can generally be classified into two main categories: phenotypic and genotypic. The study aims to determine drug sensitivity and to analyze the correlation between the results obtained from
[...] Read more.
Background: There are many methods of identifying microbial resistance to therapeutic agents; however, they can generally be classified into two main categories: phenotypic and genotypic. The study aims to determine drug sensitivity and to analyze the correlation between the results obtained from cultures on commercial chromogenic media BrillianceTM CRE (OXOID) and BrillianceTM ESBL (OXOID) and the occurrence of specific resistance genes carbapenemase (IMP, NDM, VIM, KPC, OXA), ESBL β-lactamase (TEM, SHV, CTX-M), and AmpC (CMY, DHA), which will be used in drug sensitivity tests. Methods: The present study used bacteria, including Klebsiella pneumoniae, Acinetobacter baumannii, and Escherichia coli, obtained from patients hospitalized in military hospitals in Poland. All strains were plated on the commercial chromogenic media and subjected to antimicrobial susceptibility testing. Additionally, molecular assays detecting three main classes according to the mechanism of action, enzyme type carbapenemase (IMP, NDM, VIM, KPC, OXA), ESBL β-lactamase (TEM, SHV, CTX-M), and AmpC (CMY, DHA) were performed using the real-time PCR method. Results: The results of the studies indicate the presence of carbapenemases and ESBL genes. Among K. pneumoniae strains, the dominant gene was CTX-M-15 (88.89%), followed by the SHV (84.12%), NDM (46.03%), TEM (41.26%), KPC (34.92%), and OXA-48 (19.04%). In contrast, A. baumanii was dominated by carbapenemases from the OXA family (OXA-51 in 96.00% and OXA-24/40 in 84.00%). E. coli exhibits a high prevalence of CTX-M-15 (53.85%), TEM (46.15%), NDM (38.46%), and CMY-2 (30.77%). It was observed that the CTX-M-15 gene was commonly co-identified with SHV (n = 43). All tested strains grew on chromogenic BrillianceTM CRE medium. In the case of BrillianceTM ESBL medium, the genes determining the resistance mechanism were detected in 41.7% for A. baumannii, 53.8% for E. coli, and 100% for K. pneumoniae. Chromogenic media perfectly differentiate strains to species. A moderate positive correlation of the occurrence of the antibiotic resistance genes was observed for OXA-51 and OXA-24/40 genes, which were resistant to meropenem (rho = 0.45, p < 0.001). K-means cluster analysis performed on integrated genotype–phenotype data allowed for the identification of three distinct clusters characterized by distinct resistance gene profiles. These results demonstrate that selective agar media enable faster identification compared to other conventional techniques; however, the obtained results should be confirmed by other validated phenotypic methods, and, if possible, by a molecular assay.
Full article
(This article belongs to the Special Issue Genetics and Antimicrobial Resistance in Pathogens of Hospital Importance)
►▼
Show Figures

Figure 1
Open AccessArticle
No Evidence of Temperature-Driven Antimicrobial Resistance in Salmonella Bacteraemia in Queensland, Australia
by
Naveen Manchal, Megan K. Young, Maria Eugenia Castellanos and Oyelola A. Adegboye
Antibiotics 2025, 14(12), 1274; https://doi.org/10.3390/antibiotics14121274 - 16 Dec 2025
Abstract
Background: Antimicrobial resistance (AMR) has been predicted to worsen with rising ambient temperatures and climate change, though the causal association between temperature and antimicrobial resistance in Salmonella species remains unconfirmed. This study investigates the association between rising ambient temperatures and resistance to antimicrobials
[...] Read more.
Background: Antimicrobial resistance (AMR) has been predicted to worsen with rising ambient temperatures and climate change, though the causal association between temperature and antimicrobial resistance in Salmonella species remains unconfirmed. This study investigates the association between rising ambient temperatures and resistance to antimicrobials used to treat Salmonella bacteraemia in Queensland, Australia. Methods: Time-series analysis with distributed lag non-linear models was used to test associations between deseasonalised temperature and resistance to ampicillin, ciprofloxacin, gentamicin, and third-generation cephalosporins, adjusting for precipitation, seasonality, and temporal trends. Results: A total of 1012 Salmonella bacteraemia cases were analysed in this study. Resistance to any antibiotic occurred in 25.5% of cases (95% CI: 22.8–28.3), resistance to gentamicin in 15.4% (95% CI: 13.2–17.8), and resistance to cephalosporins in 15% (95% CI: 12.9–17.4), with variation among Salmonella serotypes. After adjustment, no antimicrobial resistance was significantly associated with temperature: gentamicin (RR = 1.23 per 1 °C, 95% CI: 0.57–2.65, p = 0.59), cephalosporins (RR = 1.19, 95% CI: 0.52–2.72, p = 0.68), ciprofloxacin (RR = 1.88, 95% CI: 0.29–12.03, p = 0.50), and ampicillin (RR = 1.93, 95% CI: 0.28–13.17, p = 0.50). A marginal temperature–precipitation interaction for cephalosporins, identified using GAM (p = 0.048), did not remain significant after multiple testing correction, nor was it robust across model specifications (GLM p = 0.058) or cross-validation. Conclusions: The findings demonstrate that climate–AMR relationships are not universal, highlighting the importance of geographic, epidemiologic, and organism contexts in these associations.
Full article
(This article belongs to the Special Issue Antimicrobial Resistance in the Era of Climate Change)
►▼
Show Figures
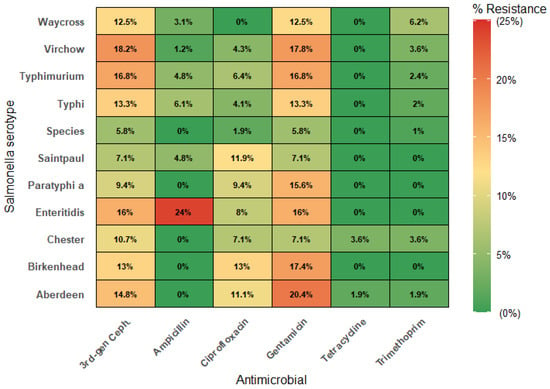
Figure 1
Open AccessArticle
Prevalence and Associated Factors for Purchasing Antibiotics Without a Prescription Among Patients in Rural South Africa: Implications for Addressing Antimicrobial Resistance
by
Tiyani Milta Maluleke, Morgan Tiyiselani Maluleke, Nishana Ramdas, Ana Golić Jelić, Amanj Kurdi, Audrey Chigome, Stephen M. Campbell, Vanda Marković-Peković, Natalie Schellack, Brian Godman and Johanna C. Meyer
Antibiotics 2025, 14(12), 1273; https://doi.org/10.3390/antibiotics14121273 - 16 Dec 2025
Abstract
Background: Antimicrobial resistance (AMR) is now a critical issue in South Africa, enhanced by considerable inappropriate prescribing of antibiotics. There is currently variable dispensing of antibiotics without a prescription. Where this occurs, it is principally for urinary tract infections (UTIs) and sexually transmitted
[...] Read more.
Background: Antimicrobial resistance (AMR) is now a critical issue in South Africa, enhanced by considerable inappropriate prescribing of antibiotics. There is currently variable dispensing of antibiotics without a prescription. Where this occurs, it is principally for urinary tract infections (UTIs) and sexually transmitted infections (STIs). Consequently, there is a need to comprehensively evaluate antibiotic dispensing patterns and factors influencing this to reduce AMR. Methods: A previously piloted questionnaire was administered to patients exiting three different categories of community pharmacies in a rural province. The questionnaire included data on the prevalence of antibiotics dispensed, whether without a prescription, and the rationale for this. Results: A total of 465 patients leaving community pharmacies with a medicine were interviewed. 54.4% of interviewed patients were dispensed at least one antibiotic, with 78.7% dispensed these without a prescription from either independent or franchise pharmacies. Metronidazole (36.1%) and azithromycin (32.7%) were the most dispensed antibiotics. STIs were the most common infectious disease for which an antibiotic was dispensed (60.1%), with 99.6% dispensed without a prescription. Upper respiratory tract infections (URTIs) were the most common infection where antibiotics were dispensed with a prescription (60.0%), with little dispensing without a prescription (7.1%). The most frequently cited reasons for obtaining antibiotics without a prescription were prior use (56.8%), long waiting times at PHC clinics (15.6%), and financial constraints (6.0%). Conclusions: There is an urgent need to review community pharmacists’ scope of practice, including allowing them to prescribe antibiotics for infectious diseases such as UTIs, similar to other countries. Concomitantly, utilise trained community pharmacists to engage with prescribers to improve future antibiotic use, especially for URTIs.
Full article
(This article belongs to the Special Issue Therapy of Infectious Diseases Among Children and Adults: The Role of Antibiotics in Daily Practice)
Open AccessCorrection
Correction: Khan et al. Adherence to Antibacterial Therapy and Associated Factors in Lower Respiratory Infections in War-Affected Areas: A Randomized Controlled Trial. Antibiotics 2025, 14, 977
by
Faiz Ullah Khan, Farman Ullah Khan, Haishaerjiang Wushouer, Luwen Shi and Yu Fang
Antibiotics 2025, 14(12), 1272; https://doi.org/10.3390/antibiotics14121272 - 16 Dec 2025
Abstract
There was an error in the original publication [...]
Full article
(This article belongs to the Section Antibiotics Use and Antimicrobial Stewardship)
Open AccessArticle
Proteomic Analysis of the Differential Response of Pseudomonas aeruginosa and Staphylococcus aureus to Lacticaseibacillus rhamnosus Cell-Free Supernatant and Lactic Acid
by
Marta Bianchi, Giuseppantonio Maisetta, Semih Esin, Giovanna Batoni and Kevin Kavanagh
Antibiotics 2025, 14(12), 1271; https://doi.org/10.3390/antibiotics14121271 - 15 Dec 2025
Abstract
Background/Objectives: Postbiotics derived from lactic acid bacteria are emerging as promising antimicrobial agents due to their antibacterial, antibiofilm, and immunomodulatory properties. Among their metabolites, lactic acid (LA) is thought to play a major role in antimicrobial activity. This study investigated the proteomic response
[...] Read more.
Background/Objectives: Postbiotics derived from lactic acid bacteria are emerging as promising antimicrobial agents due to their antibacterial, antibiofilm, and immunomodulatory properties. Among their metabolites, lactic acid (LA) is thought to play a major role in antimicrobial activity. This study investigated the proteomic response of Pseudomonas aeruginosa and Staphylococcus aureus to Lacticaseibacillus rhamnosus cell-free supernatant (CFS) and compared it with that elicited by LA alone. Methods: Overnight bacterial cultures were exposed to sub-MIC LA or CFS (1:10 for P. aeruginosa and 1:8 for S. aureus; ~12.5–15.6 mM LA) for 6 h at 37 °C. Intracellular proteins were harvested and subsequently quantified and purified to be analysed by HPLC–MS/MS, for quantitative label-free proteomics. Results: Proteomic analysis revealed clear separation of treated samples from controls, with largely overlapping responses to CFS and LA. Hallmark acid-stress adaptations were observed, including urease-mediated pH buffering, confirming that part of the response was driven by mild organic acid. In P. aeruginosa, treatments suppressed virulence pathways (phenazines, T3SS), while shifting metabolism toward lactate utilisation and reinforcing the outer membrane (lipid A, polyamine). In S. aureus, decreased abundance of the SaeRS-regulated immune-evasion factor Sbi, together with changes in envelope, ROS and translation-related proteins, suggested a bacteriostatic-like state. S. aureus differences between CFS and LA were more pronounced; CFS uniquely increased cell-wall defences, oxidative stress (SodA, SodM) and chaperone expression (GroS, GrpE), suggesting stress beyond acidification alone. Conclusions: These findings shed light on the molecular mechanisms underlying bacterial adaptation to CFS and highlight their potential as a novel antimicrobial approach.
Full article
(This article belongs to the Special Issue Antibiotics: Fighting Disease and Promoting Health by Embracing the Two Sides of the Same Coin)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Leveraging Communication to Combat Antibiotic Resistance: A Longitudinal Test of a Video-Based Intervention to Improve Providers’ Stewardship Skills
by
Yanmengqian Zhou, Madeline Jupina, Elizabeth Gibbs, Bryan Mesquita and Erina L. Farrell
Antibiotics 2025, 14(12), 1270; https://doi.org/10.3390/antibiotics14121270 - 15 Dec 2025
Abstract
Background: Antibiotic resistance is a pressing public health concern, exacerbated by the prescribing of antibiotics in primary care settings when they are not clinically indicated. Research shows that providers often feel pressured to prescribe antibiotics in response to patients’ expectations. To address this
[...] Read more.
Background: Antibiotic resistance is a pressing public health concern, exacerbated by the prescribing of antibiotics in primary care settings when they are not clinically indicated. Research shows that providers often feel pressured to prescribe antibiotics in response to patients’ expectations. To address this challenge, we developed a theory-informed video intervention to enhance antibiotic stewardship communication skills among current and future primary care providers, with emphasis on college health settings. The intervention consisted of five videos targeting core skills: explaining diagnosis and treatment, discussing antibiotic risks, advising on symptom management, offering patient support, and navigating visits with emerging adults. Program effectiveness was assessed immediately and three months post-intervention. Methods: Providers and medical students (N = 135) completed a three-wave study. At baseline, they reported demographics, perceived importance of the five skill sets, as well as self-efficacy, and completed closed- and open-ended skill assessment. Two weeks later, participants viewed the intervention videos, reassessed their skills, and rated their motivation to improve. Three months after video exposure, they completed the same skill assessments. Results: Participants showed improvements in all communication skills immediately post-intervention, except for supporting patients. While some skills showed sustained improvements at three months, the overall long-term effects were less pronounced. Perceived skill importance, baseline self-efficacy, and post-intervention motivation moderated these effects. Conclusions: A brief video-based intervention effectively enhanced current and future providers’ antibiotic stewardship communication skills. Sustaining these gains, however, requires ongoing reinforcement. Notably, the intervention was especially beneficial for those with low motivation and self-efficacy, key targets for such programs.
Full article
(This article belongs to the Section Antibiotics Use and Antimicrobial Stewardship)
Open AccessArticle
Rule-Breaking and Rulemaking: Governance of the Antibiotic Value Chain in Rural and Peri-Urban India
by
Anne-Sophie Jung, Indranil Samanta, Sanghita Bhattacharyya, Gerald Bloom, Pablo Alarcon and Meenakshi Gautham
Antibiotics 2025, 14(12), 1269; https://doi.org/10.3390/antibiotics14121269 - 15 Dec 2025
Abstract
►▼
Show Figures
Background/Objectives: Antimicrobial resistance (AMR) is a growing global health challenge, driven in part by how antibiotics are accessed, distributed, and used within complex value chains. In peri-urban India, these supply chains involve a range of formal and informal actors and practices, making
[...] Read more.
Background/Objectives: Antimicrobial resistance (AMR) is a growing global health challenge, driven in part by how antibiotics are accessed, distributed, and used within complex value chains. In peri-urban India, these supply chains involve a range of formal and informal actors and practices, making them a critical yet underexamined focus for antimicrobial stewardship efforts. While much research has focused on the manufacturing and regulatory end, less is known about how antibiotics reach consumers in rural and peri-urban settings. This study aimed to map the human antibiotic value chain in West Bengal, India, and to analyse how formal and informal governance structures influence antibiotic use and stewardship. Methods: This qualitative study was conducted in two Gram Panchayats in South 24 Parganas district, West Bengal, India. Semi-structured interviews were carried out with 31 key informants, including informal providers, medical representatives, wholesalers, pharmacists, and regulators. Interviews explored the structure of the antibiotic value chain, actor relationships, and regulatory mechanisms. Data were analysed thematically using a value chain governance framework and NVivo 12 for coding. Results: The antibiotic value chain in rural West Bengal is highly fragmented and governed by overlapping formal and informal rules. Multiple actors—many holding dual or unofficial roles—operate across four to five tiers of distribution. Informal providers play a central role in both prescription and dispensing, often without legal licences but with strong community trust. Informal norms, credit systems, and market incentives shape prescribing behaviour, while formal regulatory enforcement is inconsistent or absent. Conclusions: Efforts to promote antibiotic stewardship must move beyond binary formal–informal distinctions and target governance structures across the entire value chain. Greater attention should be paid to actors higher up the chain, including wholesalers and pharmaceutical marketing networks, to improve stewardship and access simultaneously. This study highlights how fragmented governance structures, overlapping actor roles, and uneven regulation within antibiotic value chains create critical gaps that must be addressed to design effective antimicrobial stewardship strategies.
Full article

Figure 1
Open AccessSystematic Review
Antimicrobial Resistance in Selected Enterobacteriaceae from Broilers and Their Environment: ESBL, AmpC, Carbapenemases, Colistin, and Fluoroquinolone Resistance—A Systematic Review and Meta-Analysis
by
Julia von Kiparski, Nunzio Sarnino, Diana Vargas, Aleksandra Atanasova and Roswitha Merle
Antibiotics 2025, 14(12), 1268; https://doi.org/10.3390/antibiotics14121268 - 15 Dec 2025
Abstract
Background/Objectives: Antimicrobial resistance (AMR) threatens global public health. This systematic review and meta-analysis, as part of the “ENVIRE” project (interventions to control the dynamics of antimicrobial resistance from chickens through the environment), assesses the prevalence of phenotypic and genotypic resistance, including extended-spectrum beta-lactamases
[...] Read more.
Background/Objectives: Antimicrobial resistance (AMR) threatens global public health. This systematic review and meta-analysis, as part of the “ENVIRE” project (interventions to control the dynamics of antimicrobial resistance from chickens through the environment), assesses the prevalence of phenotypic and genotypic resistance, including extended-spectrum beta-lactamases (ESBLs), AmpC beta-lactamases, carbapenemases, colistin, and fluoroquinolone resistance, in broiler chickens and their environment. Methods: The analysis covers the years 2002–2022, focusing on Escherichia (E.) coli, Klebsiella spp., Enterobacter spp., and Citrobacter spp. in fecal, meat, environmental, and other-than-feces samples from observational studies published in PubMed and Web of Science. Quality assessment was performed using the Alberta Heritage Foundation criteria. Results: Data from 170 studies, conducted in Europe, North Africa, and North America, were included. The most frequently studied resistance was to beta-lactam, with focus on ESBL-producing and AmpC beta-lactamase isolates. The pooled prevalence of ESBL-resistant E. coli observed in meat samples at 41% and in fecal samples at 38% demonstrated significant heterogeneity between the studies. The negative binomial regression analysis of prevalence data revealed significantly higher ESBL-producing E. coli rates in European meat samples compared to North African samples. Conclusions: This systematic review revealed substantial variation in prevalence and emphasizes the need for standardized surveillance systems and robust study designs.
Full article
(This article belongs to the Special Issue Antimicrobial Resistance and Epidemiological Study of Clinically Relevant Pathogens)
►▼
Show Figures

Figure 1
Open AccessReview
Silver Nanoparticles Used in Medical–Dental Plastics for Therapeutic Purposes: A Comprehensive Review
by
José Luis Maruri-Casas, Edith Lara-Carrillo, Víctor Hugo Toral-Rizo, Raúl Alberto Morales-Luckie, Gloria Elena Guzmán-Celaya, Norma Guadalupe Ibañez-Mancera, Francisco Javier Tejeda-Nava, Saraí Carmina Guadarrama-Reyes, Elías Nahúm Salmerón-Valdés and Ana Miriam Santillán-Reyes
Antibiotics 2025, 14(12), 1267; https://doi.org/10.3390/antibiotics14121267 - 15 Dec 2025
Abstract
Background/Objectives: The integration of silver nanoparticles (AgNPs) into plastic materials has emerged as a promising strategy to provide biomedical and dental devices with an active antimicrobial barrier. In this review, we aimed to synthesize the scientific evidence published between 2013 and 2024 regarding
[...] Read more.
Background/Objectives: The integration of silver nanoparticles (AgNPs) into plastic materials has emerged as a promising strategy to provide biomedical and dental devices with an active antimicrobial barrier. In this review, we aimed to synthesize the scientific evidence published between 2013 and 2024 regarding the therapeutic efficacy, biocompatibility, and safety of AgNP-functionalized plastics by following the 2020 PRISMA guidelines. Methods: Searches were conducted in PubMed, Scopus, Web of Science, SciELO, and ScienceDirect. A total of 634 records were identified, of which 21 studies met the inclusion criteria after full-text evaluation. Results: Plastics containing AgNPs show a significant reduction in microbial load (Escherichia coli, Stafilococcus aureus, and Candida albicans) and exhibit controlled release of Ag+ ions, with generally low cytotoxicity levels. The most frequent applications included catheters, dental prostheses, dressings, and orthodontic resins. However, methodological heterogeneity and the scarcity of clinical trials limit the extrapolation of findings. Conclusions: AgNPs confer relevant therapeutic advantages to polymers, but long-term clinical studies are needed to confirm their safety and effectiveness.
Full article
(This article belongs to the Special Issue Antimicrobial Biomaterials for Dentistry)
►▼
Show Figures
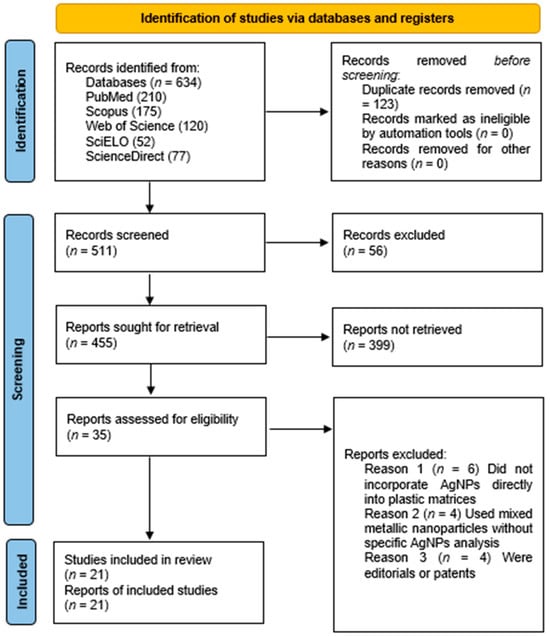
Figure 1

Journal Menu
► ▼ Journal Menu-
- Antibiotics Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Agriculture, Animals, Veterinary Sciences, Antibiotics, Zoonotic Diseases
Animal Diseases in Agricultural Production Systems: Their Veterinary, Zoonotic, and One Health Importance, 2nd Edition
Topic Editors: Ewa Tomaszewska, Beata Łebkowska-Wieruszewska, Tomasz Szponder, Joanna Wessely-SzponderDeadline: 31 March 2026
Topic in
Antibiotics, IJMS, Microbiology Research, Pharmaceuticals, Pharmaceutics, Nanomaterials, Microorganisms
Challenges and Future Prospects of Antibacterial Therapy, 2nd Edition
Topic Editors: Kwang-Sun Kim, Zehra EdisDeadline: 30 November 2026
Topic in
Agriculture, Animals, Antibiotics, Microorganisms, Poultry, Pathogens, Veterinary Sciences, Biologics
Advances in Infectious and Parasitic Diseases of Animals
Topic Editors: Felipe M. Salvarani, Sheyla Farhayldes Souza Domingues, Júlia Angélica Gonçalves Da SilveiraDeadline: 31 December 2026
Topic in
Antioxidants, Biology, Biomedicines, Microorganisms, JoF, IJMS, Stresses, Antibiotics
Microbial Redox Biology: From Stress Response to Biotechnology
Topic Editors: Michal Letek, Volker BehrendsDeadline: 1 March 2027

Conferences
Special Issues
Special Issue in
Antibiotics
Environmental Risk and Antibiotic Resistance in Hospital-Acquired Infections
Guest Editor: Catherine NeuwirthDeadline: 20 December 2025
Special Issue in
Antibiotics
Antibiotic Surveillance and Rational Use in Special Populations: Enhancing Stewardship for Vulnerable Groups
Guest Editors: Phumzile P Skosana, Filippo MarianoDeadline: 20 December 2025
Special Issue in
Antibiotics
Antibiotics and Antimicrobial Resistance in Aquaculture: Alternative and Complementary Treatment Methods
Guest Editor: Jaime RomeroDeadline: 30 December 2025
Special Issue in
Antibiotics
Biofilms and Urinary Tract Infections
Guest Editors: Dino Sgarabotto, Anabela BorgesDeadline: 31 December 2025
Topical Collections
Topical Collection in
Antibiotics
Antimicrobial Prescribing and Antimicrobial Use in Healthcare Settings
Collection Editors: Masayuki Maeda, Yuichi Muraki
Topical Collection in
Antibiotics
Staphylococcus— Molecular Pathogenesis, Virulence Regulation and Antibiotics Resistance
Collection Editor: Ewa Szczuka
Topical Collection in
Antibiotics
Editorial Board Members' Collection Series: Structural Aspects of AMPs and Antimicrobials
Collection Editors: J. Michael Conlon, Marc Maresca, Bong-Jin Lee, Aurélie Tasiemski
Topical Collection in
Antibiotics
Synthetic and Natural Products-Based Antimicrobial and Antiparasitic Agents
Collection Editor: Antonio Eduardo Miller Crotti