-
 Ground-Glass Opacities and Highly Perfused Lung Areas as Risk Factors for Pulmonary Hemorrhage in CT-Guided Lung Biopsy
Ground-Glass Opacities and Highly Perfused Lung Areas as Risk Factors for Pulmonary Hemorrhage in CT-Guided Lung Biopsy -
 Impact of Deep Learning 3D CT Super-Resolution on AI-Based Pulmonary Nodule Characterization
Impact of Deep Learning 3D CT Super-Resolution on AI-Based Pulmonary Nodule Characterization -
![Metabolic Differences in Neuroimaging with [<sup>18</sup>F]FDG in Rats Under Isoflurane and Hypnorm–Dormicum](https://pub.mdpi-res.com/title_story/title_story_17473672685397.jpg?1750315394) Metabolic Differences in Neuroimaging with [18F]FDG in Rats Under Isoflurane and Hypnorm–Dormicum
Metabolic Differences in Neuroimaging with [18F]FDG in Rats Under Isoflurane and Hypnorm–Dormicum -
 Fast Hadamard-Encoded 7T Spectroscopic Imaging of Human Brain
Fast Hadamard-Encoded 7T Spectroscopic Imaging of Human Brain
Journal Description
Tomography
Tomography
is an international, peer-reviewed open access journal on imaging technologies published monthly online by MDPI (from Volume 7 Issue 1-2021).
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, MEDLINE, PMC, and other databases.
- Journal Rank: JCR - Q2 (Radiology, Nuclear Medicine and Medical Imaging)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 23.8 days after submission; acceptance to publication is undertaken in 3.3 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
2.2 (2024);
5-Year Impact Factor:
2.2 (2024)
Latest Articles
Longitudinal Overlap and Metabolite Analysis in Spectroscopic MRI-Guided Proton Beam Therapy in Pediatric High-Grade Glioma
Tomography 2025, 11(6), 71; https://doi.org/10.3390/tomography11060071 - 19 Jun 2025
Abstract
Background: Pediatric high-grade glioma (pHGG) is a highly aggressive cancer with unique biology distinct from adult high-grade glioma, limiting the effectiveness of standard treatment protocols derived from adult research. Objective: The purpose of this report is to present preliminary results from an ongoing
[...] Read more.
Background: Pediatric high-grade glioma (pHGG) is a highly aggressive cancer with unique biology distinct from adult high-grade glioma, limiting the effectiveness of standard treatment protocols derived from adult research. Objective: The purpose of this report is to present preliminary results from an ongoing pilot study integrating spectroscopic magnetic resonance imaging (sMRI) to guide proton beam therapy and longitudinal imaging analysis in pediatric patients with high-grade glioma (pHGG). Methods: Thirteen pediatric patients under 21 years old with supratentorial WHO grade III-IV glioma underwent baseline and serial whole-brain spectroscopic MRI alongside standard structural MRIs. Radiation targets were defined using T1-weighted contrast enhanced, T2-FLAIR, and Cho/NAA ≥ 2X maps. Longitudinal analyses included voxel-level metabolic change maps and spatial overlap metrics comparing pre-proton therapy and post-. Results: Six patients had sufficient longitudinal data; five received sMRI-guided PBT. Significant positive correlation (R2 = 0.89, p < 0.0001) was observed between T2-FLAIR and Cho/NAA ≥ 2X volumes. Voxel-level difference maps of Cho/NAA and Choline revealed dynamic metabolic changes across follow-up scans. Analyzing Cho/NAA and Cho changes over time allowed differentiation between true progression and pseudoprogression, which conventional MRI alone struggles to achieve. Conclusions: Longitudinal sMRI enhanced metabolic tracking in pHGG, detects early tumor changes, and refines RT targeting beyond structural imaging. This first in-kind study highlights the potential of sMRI biomarkers in tracking treatment effects and emphasizes the complementary roles of metabolic and radiographic metrics in evaluating therapy response in pHGG.
Full article
(This article belongs to the Section Cancer Imaging)
►
Show Figures
Open AccessArticle
Assessment of Mandibular Bone Architecture in Patients with Endocrine Disorders Using Fractal Dimension and Histogram Analysis
by
Elif Yıldızer, Saliha Kubra Sari, Fatih Peker, Ali Riza Erdogan, Kevser Sancak and Sinan Yasin Ertem
Tomography 2025, 11(6), 70; https://doi.org/10.3390/tomography11060070 - 18 Jun 2025
Abstract
►▼
Show Figures
Objective: Endocrine disorders, including diabetes mellitus and thyroid dysfunctions, can significantly impact bone metabolism and structure. This study aimed to assess mandibular trabecular architecture in patients with type 1 diabetes mellitus (T1DM), type 2 diabetes mellitus (T2DM), hyperthyroidism, and hypothyroidism using fractal dimension
[...] Read more.
Objective: Endocrine disorders, including diabetes mellitus and thyroid dysfunctions, can significantly impact bone metabolism and structure. This study aimed to assess mandibular trabecular architecture in patients with type 1 diabetes mellitus (T1DM), type 2 diabetes mellitus (T2DM), hyperthyroidism, and hypothyroidism using fractal dimension (FD) and histogram analyses (HA), comparing the findings with a healthy control group. Methods: This retrospective study analyzed panoramic radiographs from 200 individuals, comprising 40 patients in each of the four endocrine disorder groups and 40 healthy controls. Fractal dimension and histogram-based pixel intensity analyses were conducted using ImageJ™ (version 1.53) software. Four standardized regions of interest (ROI) were evaluated on the right mandible, and statistical comparisons were conducted across groups using one-way analysis of variance (ANOVA), t-test, Mann–Whitney U, and Spearman correlation analyses. Results: Age and gender distributions did not differ significantly between groups. FD analysis revealed a significant reduction at ROI1 in the hyperthyroidism group compared to controls (p = 0.018); however, no other significant FD differences were observed among the remaining groups or ROIs. A significant positive correlation was found between FD and histogram values at ROI1 and ROI2 (p < 0.001), while pixel intensity values did not differ significantly across groups in any ROI. Conclusion: Although no significant differences were found in diabetic groups, the decreased FD in hyperthyroid patients suggests that FD analysis may be a useful non-invasive method to detect subtle bone alterations. Further research with larger sample sizes and comprehensive biochemical analyses are needed to confirm these findings.
Full article

Figure 1
Open AccessArticle
Structured Transformation of Unstructured Prostate MRI Reports Using Large Language Models
by
Luca Di Palma, Fatemeh Darvizeh, Marco Alì and Deborah Fazzini
Tomography 2025, 11(6), 69; https://doi.org/10.3390/tomography11060069 - 17 Jun 2025
Abstract
Objectives: to assess the ability of high-performing open-weight large language models (LLMs) in extracting key radiological features from prostate MRI reports. Methods: Five LLMs (Llama3.3, DeepSeek-R1-Llama3.3, Phi4, Gemma-2, and Qwen2.5-14B) were used to analyze free-text MRI reports retrieved from clinical practice. Each LLM
[...] Read more.
Objectives: to assess the ability of high-performing open-weight large language models (LLMs) in extracting key radiological features from prostate MRI reports. Methods: Five LLMs (Llama3.3, DeepSeek-R1-Llama3.3, Phi4, Gemma-2, and Qwen2.5-14B) were used to analyze free-text MRI reports retrieved from clinical practice. Each LLM processed reports three times using specialized prompts to extract (1) dimensions, (2) volume and PSA density, and (3) lesion characteristics. An experienced radiologist manually annotated the dataset, defining entities (Exam) and sub-entities (Lesion, Dimension). Feature- and physician-level performance were then assessed. Results: 250 MRI exams reported by 7 radiologists were analyzed by the LLMs. Feature-level performances showed that DeepSeek-R1-Llama3.3 exhibited the highest average score (98.6% ± 2.1%), followed by Phi4 (98.1% ± 2.2%), Llama3.3 (98.0% ± 3.0%), Qwen2.5 (97.5% ± 3.9%), and Gemma2 (96.0% ± 3.4%). All models excelled in extracting PSA density (100%) and volume (≥98.4%), while lesions’ extraction showed greater variability (88.4–94.0%). LLMs’ performance varied among radiologists: Physician B’s reports yielded the highest mean score (99.9% ± 0.2%), while Physician C’s resulted in the lowest (94.4% ± 2.3%). Conclusions: LLMs showed promising results in automated feature-extraction from radiology reports, with DeepSeek-R1-Llama3.3 achieving the highest overall score. These models can improve clinical workflows by structuring unstructured medical text. However, a preliminary analysis of reporting styles is necessary to identify potential challenges and optimize prompt design to better align with individual physician reporting styles. This approach can further enhance the robustness and adaptability of LLM-driven clinical data extraction.
Full article
(This article belongs to the Special Issue Cutting-Edge Applications: Artificial Intelligence and Deep Learning Revolutionizing CT and MRI)
►▼
Show Figures
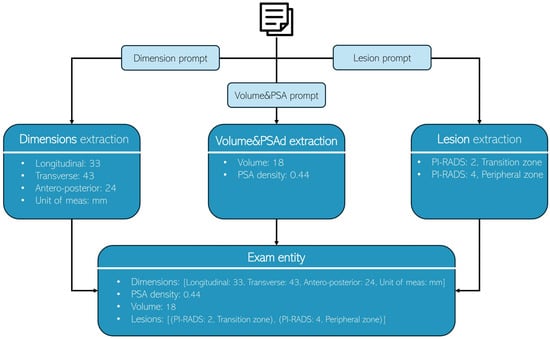
Figure 1
Open AccessReview
Applications of Advanced Imaging for Radiotherapy Planning and Response Assessment in the Central Nervous System
by
Liam S. P. Lawrence, Rachel W. Chan, Amit Singnurkar, Jay Detsky, Chris Heyn, Pejman J. Maralani, Hany Soliman, Greg J. Stanisz, Arjun Sahgal and Angus Z. Lau
Tomography 2025, 11(6), 68; https://doi.org/10.3390/tomography11060068 - 12 Jun 2025
Abstract
Background/Objectives: Radiotherapy for tumors of the central nervous system (CNS) could be improved by incorporating advanced imaging techniques into treatment planning and response assessment. The objective of this narrative review is to highlight the recent developments in magnetic resonance imaging (MRI) and positron
[...] Read more.
Background/Objectives: Radiotherapy for tumors of the central nervous system (CNS) could be improved by incorporating advanced imaging techniques into treatment planning and response assessment. The objective of this narrative review is to highlight the recent developments in magnetic resonance imaging (MRI) and positron emission tomography (PET) for applications in CNS radiotherapy. Methods: Recent articles were selected for discussion, covering the following topics: advanced imaging on MRI-linear accelerators for early response assessment in glioma; PET for guiding treatment planning and response assessment in glioma; and contrast-enhanced imaging and metabolic imaging for differentiating tumor progression and radiation necrosis for brain metastasis treatment. Where necessary, searches of scholarly databases (e.g., Google Scholar, PubMed) were used to find papers for each topic. The topics were chosen based on the perception of promise in advancing specific applications of CNS radiotherapy and not covered in detail elsewhere. This review is not intended to be comprehensive. Results: Advanced MRI sequences and PET could have a substantial impact on CNS radiotherapy. For gliomas, the tumor response to therapy could be assessed much earlier than using the conventional technique of measuring changes in tumor size. Using advanced imaging on combined imaging/therapy devices like MR-Linacs would enable response monitoring throughout radiotherapy. For brain metastases, radiation necrosis and tumor progression might be reliably differentiated with imaging techniques sensitive to perfusion or metabolism. However, the lack of level 1 evidence supporting specific uses for each imaging technique is an impediment to widespread use. Conclusions: Advanced MRI and PET have great promise to change the standard of care for CNS radiotherapy, but clinical trials validating specific applications are needed.
Full article
(This article belongs to the Special Issue Progress in the Use of Advanced Imaging for Radiation Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Determination of the Most Suitable Cut-Off Point of the Cervical Foraminal Cross-Sectional Area at the C5/6 Level to Predict Cervical Foraminal Bony Stenosis
by
Joohyun Lee, Jee Young Lee, Keum Nae Kang, Jae Ni Jang, Sukhee Park and Young Uk Kim
Tomography 2025, 11(6), 67; https://doi.org/10.3390/tomography11060067 - 10 Jun 2025
Abstract
►▼
Show Figures
Background: Cervical foraminal bony stenosis (CFBS) is a common degenerative spinal condition that causes radicular pain and functional impairment in the upper extremities. Accurate and objective diagnosis of CFBS remains challenging due to the absence of standardized morphometric criteria. This study aimed
[...] Read more.
Background: Cervical foraminal bony stenosis (CFBS) is a common degenerative spinal condition that causes radicular pain and functional impairment in the upper extremities. Accurate and objective diagnosis of CFBS remains challenging due to the absence of standardized morphometric criteria. This study aimed to determine an optimal cut-off value for the cervical foraminal cross-sectional area (CFCSA) at the C5/6 level as a diagnostic indicator of CFBS. Methods: We conducted a retrospective case-control study including 154 patients aged 50 years or older with clinically and radiologically confirmed CFBS and 150 age-matched asymptomatic controls. Cervical spine magnetic resonance imaging (MRI) was performed in all subjects and CFCSA measurements were obtained from sagittal T2-weighted images using a standardized protocol. Group differences were analyzed using t-tests and diagnostic performance was assessed using receiver operating characteristic (ROC) curve analysis. Results: The mean CFCSA was significantly lower in the CFBS group (25.65 ± 7.19 mm2) compared to the control group (43.00 ± 8.38 mm2; p < 0.001). ROC analysis identified a CFCSA threshold of 33.02 mm2 as the optimal cut-off point for predicting CFBS, yielding a sensitivity of 86.4%, a specificity of 86.7%, and an area under the curve (AUC) of 0.94 (95% CI: 0.91–0.96). Conclusions: These findings suggest that CFCSA is a robust and reproducible morphological parameter for evaluating foraminal stenosis. The proposed cut-off may enhance diagnostic accuracy and aid in clinical decision-making for patients presenting with C6 radiculopathy. However, given this study’s retrospective, single-center design, further validation through multicenter, prospective studies across multiple cervical levels is warranted.
Full article

Figure 1
Open AccessArticle
Image Quality and Lesion Detectability with Low-Monoenergetic Imaging: A Study of Low-Concentration Iodine Contrast in Hepatic Multiphase CT for Chronic Liver Disease
by
Jae En Kim, Yewon Lim, Jin Sil Kim, Hyo Jeong Lee, Jeong Kyong Lee and Hye Ah Lee
Tomography 2025, 11(6), 66; https://doi.org/10.3390/tomography11060066 - 4 Jun 2025
Abstract
►▼
Show Figures
Background: This study aimed to evaluate whether low-concentration iodine contrast-enhanced multiphase low-monoenergetic computed tomography (LCLM CT; 270 mg I/mL, 40 keV) is non-inferior to standard-dose computed tomography (SDCT; 350 mg I/mL) in image quality and lesion detectability for chronic liver disease patients. Methods:
[...] Read more.
Background: This study aimed to evaluate whether low-concentration iodine contrast-enhanced multiphase low-monoenergetic computed tomography (LCLM CT; 270 mg I/mL, 40 keV) is non-inferior to standard-dose computed tomography (SDCT; 350 mg I/mL) in image quality and lesion detectability for chronic liver disease patients. Methods: Sixty-seven patients underwent both protocols. Image quality was assessed using a 5-point scale with a non-inferiority margin of −0.5. Quantitative metrics included signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR). Lesion detectability was evaluated using jackknife free-response receiver operating characteristic (JAFROC) analysis with a −0.1 margin. Results: LCLM CT reduced iodine dose per kilogram by 21.9%. Despite higher image noise, it achieved higher CNR for the aorta and hepatic lesions, as well as superior hepatic artery clarity. Image quality was non-inferior (difference: −0.119; 95% CI: −0.192 to −0.047), and lesion detectability (FOM: 0.744 vs. 0.721; difference: 0.023; 95% CI: −0.170 to 0.218) also showed non-inferiority. Conclusions: LCLM CT maintains diagnostic performance and improves vascular contrast while reducing iodine burden, supporting its clinical utility in longitudinal HCC surveillance.
Full article

Figure 1
Open AccessArticle
Optimizing Radiation Risk Assessment in CT Imaging: Establishing Institutional Diagnostic Reference Levels and Personalized Dose Strategies for Chest, Abdomen, and Pelvis Scans
by
Zuhal Y. Hamd, Huda I. Almohammed, Elbagir Mansour, Abdoelrahman Hassan A. B. and Awadia Gareeballah
Tomography 2025, 11(6), 65; https://doi.org/10.3390/tomography11060065 - 3 Jun 2025
Abstract
Background: As a diagnostic radiology procedure, computed tomography (CT) contributes to patient radiation exposure; hence, it deserves special consideration. The use of diagnostic reference levels (DRLs) is an efficient way to optimize patient radiation dosage. The computed tomography dose index volume (CTDIv) and
[...] Read more.
Background: As a diagnostic radiology procedure, computed tomography (CT) contributes to patient radiation exposure; hence, it deserves special consideration. The use of diagnostic reference levels (DRLs) is an efficient way to optimize patient radiation dosage. The computed tomography dose index volume (CTDIv) and the dose-length product (DLP) help to measure DRLs. Methods: A retrospective analysis was conducted on 106 patients (43.9% male, 56.1% female; mean age of 48.18 years) who underwent computed tomography chest, abdomen, and pelvis (CT CAP) scans using a Toshiba Aquilion Prime 160-slice CT scanner. Data included patient demographics, CT parameters (mA, tube rotation time, pitch, slice thickness, and slice count), and dose indices: dose length product (DLP), computed tomography dose index volume (CTDIvol), and effective dose. Cancer risks were calculated based on effective dose, patient demographics, and scan parameters. Results: This study demonstrated that the mean values for DLP, CTDIvol, and effective dose were 1719.64 ± 488.45 mGy·cm, 25.97 ± 6.96 mGy, and 27.5 ± 7.82 mSv, respectively. Cancer risk estimates ranged from 0.048% to 1.58%, with higher risks observed for females, younger patients. Significant correlations were found between dose indices and technical parameters, including pitch, kVp, tube rotation time, and slice thickness (p < 0.005). Conclusions: The mean values for DLP, CTDIvol, and effective dose for abdominopelvic scans were higher than those found in previous studies, with significant correlation of weight on these values. Optimizing CT protocols and establishing DRLs tailored to clinical indications are critical for minimizing radiation exposure and enhancing patient safety.
Full article
(This article belongs to the Special Issue Progress in the Use of Advanced Imaging for Radiation Oncology)
►▼
Show Figures

Figure 1
Open AccessArticle
Role of Amide Proton Transfer Weighted MRI in Predicting MGMTp Methylation Status, p53-Status, Ki-67 Index, IDH-Status, and ATRX Expression in WHO Grade 4 High Grade Glioma
by
Faris Durmo, Jimmy Lätt, Anna Rydelius, Elisabet Englund, Tim Salomonsson, Patrick Liebig, Johan Bengzon, Peter C. M. van Zijl, Linda Knutsson and Pia C. Sundgren
Tomography 2025, 11(6), 64; https://doi.org/10.3390/tomography11060064 - 31 May 2025
Abstract
►▼
Show Figures
Objectives: To assess amide proton transfer weighted (APTw) MR imaging capabilities in differentiating high-grade glial tumors across alpha-thalassemia/mental retardation X-linked (ATRX) expression, tumor-suppressor protein p53 expression (p53), O6-methylguanine-DNA methyltransferase promoter (MGMTp) methylation, isocitrate dehydrogenase (IDH) status, and proliferation marker Ki-67 (Ki-67 index) as
[...] Read more.
Objectives: To assess amide proton transfer weighted (APTw) MR imaging capabilities in differentiating high-grade glial tumors across alpha-thalassemia/mental retardation X-linked (ATRX) expression, tumor-suppressor protein p53 expression (p53), O6-methylguanine-DNA methyltransferase promoter (MGMTp) methylation, isocitrate dehydrogenase (IDH) status, and proliferation marker Ki-67 (Ki-67 index) as a preoperative diagnostic aid. Material & Methods: A total of 42 high-grade glioma WHO grade 4 (HGG) patients were evaluated prospectively (30 males and 12 females). All patients were examined using conventional MRI, including the following: T1w-MPRAGE pre- and post-contrast administration, conventional T2w and 3D FLAIR, and APTw imaging with a 3T MR scanner. Receiver operating characteristic (ROC) curves were calculated for the APTw% mean, median, and max signal for the different molecular biomarkers. A logistic regression model was constructed for combined mean and median APTw% signals for p53 expression. Results: The whole-tumor max APTw% signal could significantly differentiate MGMTp from non-MGMTp HGG, p = 0.035. A cutoff of 4.28% max APTw% signal yielded AUC (area under the curve) = 0.702, with 70.6% sensitivity and 66.7% specificity. The mean/median APTw% signals differed significantly in p53 normal versus p53-overexpressed HGG s: 1.81%/1.83% vs. 1.15%/1.18%, p = 0.002/0.006, respectively. Cutoffs of 1.25%/1.33% for the mean/median APTw% signals yielded AUCs of 0.786/0.757, sensitivities of 76.9%/76.9%, and specificities of 50%/66.2%, p = 0.002/0.006, respectively. A logistic regression model with a combined mean and median APTw% signal for p53 status yielded an AUC = 0.788 and 76.9% sensitivity and 66.2% specificity. ATRX-, IDH- wild type (wt) vs. mutation (mut), and the level of Ki-67 did not differ significantly, but trends were found: IDH-wt and low Ki-67 showed higher mean/median/max APTw% signals vs. IDH-mut and high Ki-67, respectively. ATRX-wt vs. mutation showed higher mean and median APTw% signals but lower max APTw% signal. Conclusions: APTw imaging can potentially be a useful marker for the stratification of p53 expression and MGMT status in high-grade glioma in the preoperative setting and potentially aid surgical decision-making.
Full article

Figure 1
Open AccessReview
Current Update on DWI-MRI and Its Radiomics in Liver Fibrosis—A Review of the Literature
by
Ali S. Alyami
Tomography 2025, 11(6), 63; https://doi.org/10.3390/tomography11060063 - 30 May 2025
Abstract
►▼
Show Figures
Introduction: Diffusion-weighted imaging (DWI) is a non-invasive technique for acquiring liver pathology data and characterizing liver lesions. This modality shows promise for applications in the initial diagnosis and monitoring of liver diseases, providing valuable insights for clinical assessment and treatment strategies. Intravoxel incoherent
[...] Read more.
Introduction: Diffusion-weighted imaging (DWI) is a non-invasive technique for acquiring liver pathology data and characterizing liver lesions. This modality shows promise for applications in the initial diagnosis and monitoring of liver diseases, providing valuable insights for clinical assessment and treatment strategies. Intravoxel incoherent motion (IVIM), diffusion kurtosis imaging (DKI), and diffusion tensor imaging (DTI) are advanced forms of DWI. These techniques have proven effective for assessing liver lesions, including liver tumors and fibrosis. However, the results can be inconsistent. Thus, it is essential to summarize the current applications of these methods in liver fibrosis, identify existing limitations, and suggest future directions for development. Methods: This review assessed studies concerning liver DWI and its applications published in the PubMed database over the last nine years. It presents these techniques’ fundamental principles and key factors before discussing their application in liver fibrosis. Results and conclusions: It has been observed that advanced DWI sequences remain unreliable in ensuring the robustness and reproducibility of measurements when assessing liver fibrosis grades, due to inconsistent results and significant overlap among these techniques across different stages of fibrotic conditions.
Full article

Figure 1
Open AccessReview
Development of Cardiac Computed Tomography for Evaluation of Aortic Valve Stenosis
by
Hiroyuki Takaoka, Haruka Sasaki, Joji Ota, Yoshitada Noguchi, Moe Matsumoto, Kazuki Yoshida, Katsuya Suzuki, Shuhei Aoki, Satomi Yashima, Makiko Kinoshita, Noriko Suzuki-Eguchi and Yoshio Kobayashi
Tomography 2025, 11(6), 62; https://doi.org/10.3390/tomography11060062 - 28 May 2025
Abstract
Aortic valve stenosis (AS) is a valvular heart disease that imposes a high afterload on the left ventricle (LV) due to restricted opening of the aortic valve, resulting in LV hypertrophy. Severe AS can lead to syncope, angina pectoris, and heart failure. The
[...] Read more.
Aortic valve stenosis (AS) is a valvular heart disease that imposes a high afterload on the left ventricle (LV) due to restricted opening of the aortic valve, resulting in LV hypertrophy. Severe AS can lead to syncope, angina pectoris, and heart failure. The number of patients with AS has been increasing due to aging populations, the growing prevalence of lifestyle-related diseases, and advances in diagnostic technologies. Therefore, accurate diagnosis and appropriate treatment of AS are essential. In recent years, transcatheter aortic valve implantation (TAVI) has become feasible, and the number of procedures has rapidly increased, particularly among elderly patients. As treatment options for AS expand and diversify, detailed pre-procedural evaluation has become increasingly important. In particular, diagnostic imaging modalities such as computed tomography (CT) have advanced significantly, with notable improvements in image quality. With recent advancements in CT technology—such as increased detector rows, faster gantry rotation speeds, new image reconstruction methods, and the introduction of dual-energy imaging—the scope of cardiac assessment has expanded beyond the coronary arteries to include valves, myocardium, and the entire heart. This includes evaluating restricted AV opening and cardiac function using four-dimensional imaging, assessing AV annulus diameter and AS severity via calcium scoring with a novel motion correction algorithm, and detecting myocardial damage through late-phase contrast imaging using new reconstruction techniques. In cases of pre-TAVI evaluation or congenital bicuspid valves, CT is also valuable for assessing extracardiac structures, such as access routes and associated congenital heart anomalies. In addition, recent advancements in CT technology have made it possible to significantly reduce radiation exposure during cardiac imaging. CT has become an extremely useful tool for comprehensive cardiac evaluation in patients with aortic stenosis, especially those being considered for surgical treatment.
Full article
(This article belongs to the Section Cardiovascular Imaging)
►▼
Show Figures

Figure 1
Open AccessArticle
The Image Clarity Paradox: Higher CZT SPECT Contrast Does Not Always Translate to Diagnostic Accuracy for Alzheimer’s Disease
by
Kiyotaka Nemoto, Bryan J. Mathis, Akemi Iwasaka, Kenjiro Nakayama, Tomohiro Kaneta and Tetsuaki Arai
Tomography 2025, 11(6), 61; https://doi.org/10.3390/tomography11060061 - 25 May 2025
Abstract
Background: Recent advances in single-photon emission computed tomography (SPECT) technology, particularly cadmium–zinc–telluride (CZT) detectors, have improved spatial resolution and contrast in cerebral blood flow imaging. This study aimed to investigate whether these improvements translate to enhanced diagnostic accuracy for Alzheimer’s disease (AD).
[...] Read more.
Background: Recent advances in single-photon emission computed tomography (SPECT) technology, particularly cadmium–zinc–telluride (CZT) detectors, have improved spatial resolution and contrast in cerebral blood flow imaging. This study aimed to investigate whether these improvements translate to enhanced diagnostic accuracy for Alzheimer’s disease (AD). Methods: We compared conventional SPECT (eCAM) with CZT SPECT in 29 patients (mean age 60.9 ± 17.6 years, 69% female) with suspected neurodegenerative diseases. Results: Gray matter/white matter contrast was significantly higher in CZT SPECT compared to eCAM (1.615 ± 0.096 vs. 1.458 ± 0.068, p < 0.001). However, diagnostic accuracy for AD did not improve with CZT SPECT. For the participating psychiatrist, sensitivity decreased from 0.750 (eCAM) to 0.625 (CZT), while for the radiologist, specificity dropped from 0.571 (eCAM) to 0.429 (CZT). Overall accuracy slightly decreased for both readers. Conclusions: These findings suggest that while CZT SPECT offers superior image quality, it may not immediately translate to improved diagnostic accuracy for AD. The study highlights the importance of specialized training for clinicians in interpreting higher-resolution CZT SPECT images to fully leverage their potential in neurodegenerative disease diagnosis. Future research should focus on developing standardized training protocols and larger, multi-center studies to validate these findings.
Full article
(This article belongs to the Section Brain Imaging)
►▼
Show Figures

Figure 1
Open AccessArticle
Early Concepts in CT Image-Guided Robotic Vascular Surgery: The Displacement of Retroperitoneal Structures During Simulated Procedures in a Cadaveric Model
by
Balazs C. Lengyel, Ponraj Chinnadurai, Rebecca G. Barnes, Charudatta S. Bavare and Alan B. Lumsden
Tomography 2025, 11(6), 60; https://doi.org/10.3390/tomography11060060 - 23 May 2025
Abstract
Background: CT image guidance and navigation, although routinely used in complex endovascular procedures, is an unexplored territory in evolving vascular robotic procedures. In robotic surgery, it promises the better localization of vasculature, the optimization of port placement, less inadvertent tissue damage, and increased
[...] Read more.
Background: CT image guidance and navigation, although routinely used in complex endovascular procedures, is an unexplored territory in evolving vascular robotic procedures. In robotic surgery, it promises the better localization of vasculature, the optimization of port placement, less inadvertent tissue damage, and increased patient safety during the dissection of retroperitoneal structures. However, unknown tissue displacement resulting from induced pneumoperitoneum and positional changes compared to the preoperative CT scan can pose significant limitations to the reliability of image guidance. We aimed to study the displacement of retroperitoneal organs and vasculature due to factors such as increased intra-abdominal pressure (IAP) due to CO2 insufflation and patient positioning (PP) using intraoperative CT imaging in a cadaveric model. Methods: A thawed, fresh-frozen human cadaveric model was positioned according to simulated procedural workflows. Intra-arterial, contrast-enhanced CT scans were performed after the insertion of four laparoscopic ports in the abdomen. CT scans were performed with 0–5–15–25 mmHg IAPs in supine, left lateral decubitus, right lateral decubitus, Trendelenburg, and reverse Trendelenburg positions. Euclidean distances between fixed anatomical bony and retroperitoneal vascular landmarks were measured and compared across different CT scans. Results: Comparing the effects of various IAPs to the baseline (zero IAP) in the same PP, an average displacement for retroperitoneal vascular landmarks ranged from 0.6 to 3.0 mm (SD 1.0–2.8 mm). When changing the PPs while maintaining the same IAP, the average displacement of the retroperitoneal vasculature ranged from 2.0 to 15.0 mm (SD 1.7–7.2 mm). Conclusions: Our preliminary imaging findings from a single cadaveric model suggest minimal (~3 mm maximum) target vasculature displacement in the retroperitoneum due to elevated IAP in supine position and higher displacement due to changes in patient positioning. Similar imaging studies are needed to quantify procedural workflow-specific and anatomy-specific deformation, which would be invaluable in developing and validating advanced tissue deformation models, facilitating the routine applicability and usefulness of CT image guidance for target delineation during robotic vascular procedures.
Full article
(This article belongs to the Section Cardiovascular Imaging)
►▼
Show Figures

Figure 1
Open AccessReview
Partial Breast Irradiation for Early-Stage Breast Cancer: Advances, Challenges, and Future Directions—A Narrative Review
by
Ayyaz Qadir, Nabita Singh, Anelyn Chui, Michael Chao, Sergio Uribe and Farshad Foroudi
Tomography 2025, 11(6), 59; https://doi.org/10.3390/tomography11060059 - 22 May 2025
Abstract
Advances in breast cancer treatment have shifted the focus from maximizing local control to balancing oncologic efficacy with treatment de-escalation and toxicity reduction. Whole-breast irradiation (WBI) following breast-conserving surgery remains the standard of care, but with up to 90% of recurrences occurring near
[...] Read more.
Advances in breast cancer treatment have shifted the focus from maximizing local control to balancing oncologic efficacy with treatment de-escalation and toxicity reduction. Whole-breast irradiation (WBI) following breast-conserving surgery remains the standard of care, but with up to 90% of recurrences occurring near the tumor bed, partial breast irradiation (PBI) has emerged as a viable alternative. Large randomized controlled trials (such as IMPORT LOW, Florence, and GEC-ESTRO) have demonstrated comparable ipsilateral breast tumor recurrence (IBTR) rates between PBI and WBI, reinforcing its oncologic safety in well-selected patients. However, challenges remain in optimizing fractionation schedules, refining patient selection, and minimizing late toxicity. Recent innovations, including MRI-guided radiotherapy (MRgRT) and neoadjuvant PBI, offer improved tumor targeting, real-time plan adaptation, and enhanced normal tissue sparing. These advancements hold promise for further reducing radiation-related morbidity and improving cosmetic outcomes. As PBI progresses, integrating novel imaging modalities and hypofractionated regimens will be crucial to refining protocols. This review synthesizes the latest evidence on PBI techniques, clinical outcomes, and emerging technologies to guide future research and clinical decision-making in precision breast radiotherapy.
Full article
Open AccessArticle
Birth-Related Subdural Hemorrhage in Asymptomatic Newborns: Magnetic Resonance Imaging Prevalence and Evolution of Intracranial and Intraspinal Localization
by
Davide Turilli, Leandra Piscopo, Alberto Dessì, Claudia Pinna, Liala Mirella Fattacciu, Emma Solinas, Ilaria Conti, Stefania Tamburrini, Giacomo Sica, Michele Klain, Salvatore Masala and Mariano Scaglione
Tomography 2025, 11(5), 58; https://doi.org/10.3390/tomography11050058 - 20 May 2025
Abstract
►▼
Show Figures
Background: Neonatal birth-related intracranial subdural hemorrhages (SDHs) represent a form of bleeding inside the skull that occurs in newborns. This condition includes the extravasation of blood both in the encephalic parenchyma and in the extra-axial spaces. Recent studies have shown that SDH
[...] Read more.
Background: Neonatal birth-related intracranial subdural hemorrhages (SDHs) represent a form of bleeding inside the skull that occurs in newborns. This condition includes the extravasation of blood both in the encephalic parenchyma and in the extra-axial spaces. Recent studies have shown that SDH and particularly post-traumatic birth-related hemorrhages represent a frequent occurrence, but they are often asymptomatic. The gold standard for the diagnosis and follow-up of patients with SDH is multiparametric Magnetic Resonance Imaging. The aim of this study is to describe our experience by reporting several cases of SDH with different distribution and Central Nervous System involvement by the MRI of this pathology in infants up to 30 days of age. Methods: We analyzed the age and sex of the patients included in this study, the localization of SDH in different CNS areas, and their frequency using distribution plots and pie charts. Results: About the analysis of the SDH locations in the 32 patients, the most common location was the cerebellum (31/32, 96.9%), followed by parietal and occipital lobes (19/32, 59.4%; 18/32, 56.2%, respectively), falx cerebri (11/32, 34.4%), tentorium cerebelli (10/32, 31.2%), temporal lobes (6/32, 18.7%), and finally cervical and dorsal spine in the same patients (4/32, 12.5%). According to SDH locations, the patients were divided into supratentorial, infratentorial, both, and Spinal Canal. Conclusions: Our study confirmed the literature data regarding the neonatal birth-related SDH high frequency, but also allowed us to focus our attention on the rarest spinal SDH localizations with the same benign evolution.
Full article

Figure 1
Open AccessArticle
Time-Intensity Curve Analysis of Contrast-Enhanced Ultrasound for Non-Ossified Thyroid Cartilage Invasion in Laryngeal Squamous Cell Carcinoma
by
Milda Pucėtaitė, Dalia Mitraitė, Rytis Tarasevičius, Davide Farina, Silvija Ryškienė, Saulius Lukoševičius, Evaldas Padervinskis, Valdas Šarauskas and Saulius Vaitkus
Tomography 2025, 11(5), 57; https://doi.org/10.3390/tomography11050057 - 16 May 2025
Abstract
►▼
Show Figures
Objective: This study aimed to assess the diagnostic value of contrast-enhanced ultrasound (CEUS) time–intensity curve (TIC) parameters in detecting non-ossified thyroid cartilage invasion in patients with laryngeal squamous cell carcinoma (SCC). Methods: A CEUS TIC analysis was performed on 32 cases from
[...] Read more.
Objective: This study aimed to assess the diagnostic value of contrast-enhanced ultrasound (CEUS) time–intensity curve (TIC) parameters in detecting non-ossified thyroid cartilage invasion in patients with laryngeal squamous cell carcinoma (SCC). Methods: A CEUS TIC analysis was performed on 32 cases from 27 patients with histologically confirmed laryngeal SCC. The diagnostic performance of time to peak (TTP), peak intensity (PI), wash-in slope (WIS), area under the curve (AUC), and their quantitative differences (∆TTP, ∆PI, ∆WIS, and ∆AUC) to discriminate between the invaded and the non-invaded non-ossified thyroid cartilage was determined using ROC analysis. A logistic regression analysis was employed to identify significant predictors. Results: In an ROC analysis, of all TIC parameters analyzed separately, ∆TTP showed the greatest diagnostic performance (AUC: 0.85). A ∆TTP cut-off of ≤ 8.9 s differentiated between the invaded and the non-invaded non-ossified thyroid cartilage with a sensitivity of 100%, specificity of 76.9%, and accuracy of 81.3%. A combination of ∆TTP and PI increased the AUC to 0.93, specificity to 100%, and accuracy to 96.8%, but reduced the sensitivity to 83.3%. Meanwhile, the visual assessment of enhancement on CEUS to detect cartilage invasion had 83.3% sensitivity and 84.6% specificity. In a univariate logistic regression, only ∆TTP was a significant predictor of non-ossified thyroid cartilage invasion (OR: 0.80; 95% CI: 0.64–1.00). For every second increase in ∆TTP, the probability of thyroid cartilage invasion decreased by 20%. Conclusions: CEUS TIC parameters, particularly a combination of ∆TTP and PI, showed high diagnostic performance in the detection of non-ossified thyroid cartilage invasion in laryngeal SCC.
Full article
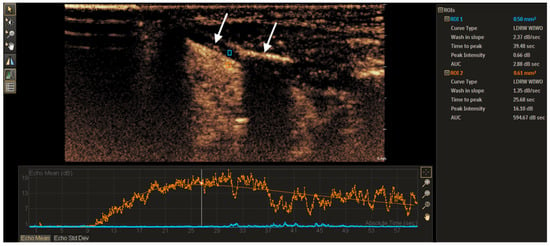
Figure 1
Open AccessArticle
Transforming 3D MRI to 2D Feature Maps Using Pre-Trained Models for Diagnosis of Attention Deficit Hyperactivity Disorder
by
Elahe Hosseini, Seyyed Ali Hosseini, Stijn Servaes, Brandon Hall, Pedro Rosa-Neto, Ali-Reza Moradi, Ajay Kumar, Mir Mohsen Pedram and Sanjeev Chawla
Tomography 2025, 11(5), 56; https://doi.org/10.3390/tomography11050056 - 13 May 2025
Abstract
►▼
Show Figures
Background: According to the World Health Organization (WHO), approximately 5% of children and 2.5% of adults suffer from attention deficit hyperactivity disorder (ADHD). This disorder can have significant negative consequences on people’s lives, particularly children. In recent years, methods based on artificial intelligence
[...] Read more.
Background: According to the World Health Organization (WHO), approximately 5% of children and 2.5% of adults suffer from attention deficit hyperactivity disorder (ADHD). This disorder can have significant negative consequences on people’s lives, particularly children. In recent years, methods based on artificial intelligence and neuroimaging techniques, such as MRI, have made significant progress, paving the way for development of more reliable diagnostic tools. In this proof of concept study, our aim was to investigate the potential utility of neuroimaging data and clinical information in combination with a deep learning-based analytical approach, more precisely, a novel feature extraction technique for the diagnosis of ADHD with high accuracy. Methods: Leveraging the ADHD200 dataset, which encompasses demographic information and anatomical MRI scans collected from a diverse ADHD population, our study focused on developing modern deep learning-based diagnostic models. The data preprocessing employed a pre-trained Visual Geometry Group16 (VGG16) network to extract two-dimensional (2D) feature maps from three-dimensional (3D) anatomical MRI data to reduce computational complexity and enhance diagnostic power. The inclusion of personal attributes, such as age, gender, intelligence quotient, and handedness, strengthens the diagnostic models. Four deep-learning architectures—convolutional neural network 2D (CNN2D), CNN1D, long short-term memory (LSTM), and gated recurrent units (GRU)—were employed for analysis of the MRI data, with and without the inclusion of clinical characteristics. Results: A 10-fold cross-validation test revealed that the LSTM model, which incorporated both MRI data and personal attributes, had the best diagnostic performance among all tested models in the diagnosis of ADHD with an accuracy of 0.86 and area under the receiver operating characteristic (ROC) curve (AUC) score of 0.90. Conclusions: Our findings demonstrate that the proposed approach of extracting 2D features from 3D MRI images and integrating these features with clinical characteristics may be useful in the diagnosis of ADHD with high accuracy.
Full article

Figure 1
Open AccessArticle
Preliminary Results of Clinical Experience with Consolidative High-Dose Thoracic Radiotherapy for Patients with Extensive-Stage Small Cell Lung Cancer
by
Hakyoung Kim, Jeongeun Hwang, Sun Myung Kim and Dae Sik Yang
Tomography 2025, 11(5), 55; https://doi.org/10.3390/tomography11050055 - 7 May 2025
Abstract
►▼
Show Figures
Objectives: Extensive-stage small-cell lung cancer (SCLC) has a poor prognosis, but recently, the combination of immunotherapy and chemotherapy has improved treatment outcomes in some patients, and treatment plans may vary depending on the individual’s general condition and tumor response. In addition, intrathoracic tumor
[...] Read more.
Objectives: Extensive-stage small-cell lung cancer (SCLC) has a poor prognosis, but recently, the combination of immunotherapy and chemotherapy has improved treatment outcomes in some patients, and treatment plans may vary depending on the individual’s general condition and tumor response. In addition, intrathoracic tumor control remains a major challenge for this disease. In the current study, we aim to share our clinical experience and demonstrate that consolidative high-dose thoracic radiotherapy effectively reduces intrathoracic tumor recurrence while maintaining acceptable treatment-related toxicities. Materials and Methods: The medical records of 81 SCLC patients treated at Korea University Guro Hospital from January 2019 to December 2023 were reviewed retrospectively. Among them, 22 patients with extensive-stage SCLC who had a favorable tumor response after systemic therapy, including those with oligo-progressive disease limited to the thoracic region and suitable for curative local therapy, received consolidative radiotherapy. A total dose of 52.5 Gy in 25 fractions was administered over 5 weeks to all patients with extensive-stage SCLC. Results and Conclusions: The median follow-up time was 22 months (range: 8–59 months), with the median follow-up period after completing consolidative radiotherapy being 13 months (range: 4–35 months). In-field local recurrence occurred in only one patient after consolidative thoracic radiotherapy. Most importantly, 10 patients with oligo-progressive disease at the thoracic site, at the time of tumor response, remained stable without further intrathoracic in-field recurrence. Additionally, no severe cases of radiation pneumonitis or esophagitis were observed. Based on our institution’s experience, consolidative high-dose thoracic radiotherapy is well-tolerated and associated with fewer intrathoracic recurrences, leading to improved long-term survival in carefully selected patients with extensive-stage SCLC. Given these findings, we believe consolidative radiotherapy should be considered more proactively in clinical practice. Furthermore, these results may help guide the design of future clinical trials.
Full article
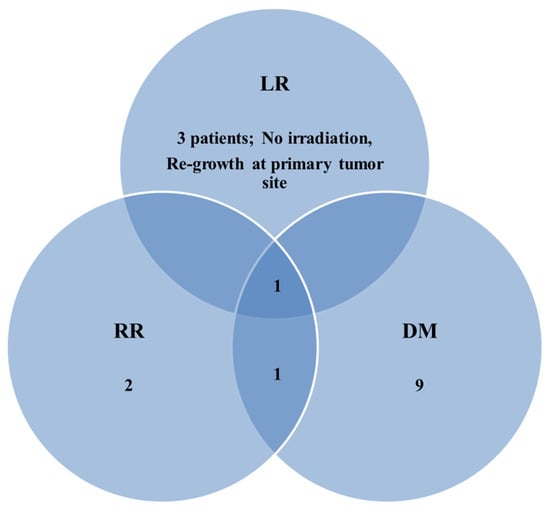
Figure 1
Open AccessArticle
CT Perfusion Imaging in Patients with Acute Ischemic Stroke: The Role of Premorbid Statin Treatment
by
Eliseo Picchi, Francesca Di Giuliano, Noemi Pucci, Fabrizio Sallustio, Silvia Minosse, Alfredo Paolo Mascolo, Federico Marrama, Valentina Ferrazzoli, Valerio Da Ros, Marina Diomedi, Massimo Federici and Francesco Garaci
Tomography 2025, 11(5), 54; https://doi.org/10.3390/tomography11050054 - 6 May 2025
Abstract
Background. Statins appear to be useful in patients with acute ischemic stroke. Our aim was to evaluate the association between premorbid statin treatment and CT perfusion characteristics of acute ischemic stroke. Methods. A retrospective analysis of patients with acute stroke secondary to occlusion
[...] Read more.
Background. Statins appear to be useful in patients with acute ischemic stroke. Our aim was to evaluate the association between premorbid statin treatment and CT perfusion characteristics of acute ischemic stroke. Methods. A retrospective analysis of patients with acute stroke secondary to occlusion of large vessels in the anterior circulation was performed to assess collateral flow, ischemic core volume, and ischemic penumbra using CT angiography and CT perfusion maps. Fisher’s exact test was used to compare baseline characteristics of patients in the two groups. The Wilcoxon rank-sum test for independent groups was used to compare all variables obtained for the two different groups with and without statin use. Results. We identified 61 patients, including 29 treated with statins and 32 not treated with statins before stroke onset matched by age, gender, and vascular risk factors except for hypercholesterolemia. The statin group showed lower National Institutes of health Stroke Scale scores at onset (14 ± 6.1 vs. 16 ± 4.5; p = 0.04) and lower volumes of brain tissue characterized by impaired cerebral blood flow (CBF), cerebral blood volume (CBV), and
(This article belongs to the Section Neuroimaging)
►▼
Show Figures
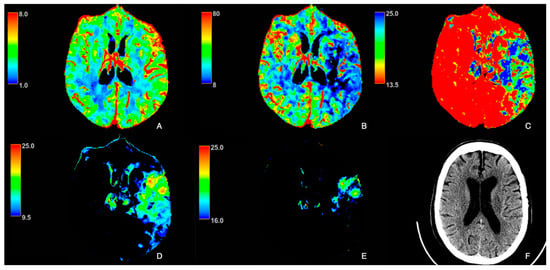
Figure 1
Open AccessArticle
Shoulder Injury Related to Vaccine Administration (SIRVA) Following COVID-19 Vaccination: Correlating MRI Findings with Patient Demographics
by
Naser Obeidat, Ruba Khasawneh, Ahmad Alrawashdeh, Ali M. Abdel Kareem, Mohammad K. Al-na’asan, Mohammad Alkhatatba and Suhaib Bani Essa
Tomography 2025, 11(5), 53; https://doi.org/10.3390/tomography11050053 - 2 May 2025
Abstract
►▼
Show Figures
Objectives: Shoulder injury related to vaccine administration (SIRVA), previously observed with influenza vaccines, has gained clinical significance with widespread COVID-19 vaccination. However, few studies correlate vaccine types and demographic factors with the MRI findings of SIRVA. This study aimed to evaluate MRI findings
[...] Read more.
Objectives: Shoulder injury related to vaccine administration (SIRVA), previously observed with influenza vaccines, has gained clinical significance with widespread COVID-19 vaccination. However, few studies correlate vaccine types and demographic factors with the MRI findings of SIRVA. This study aimed to evaluate MRI findings of SIRVA following COVID-19 vaccination and assess associations with vaccine type and patient characteristics. Methods: A retrospective cohort study was conducted on 35 patients with new-onset shoulder complaints within six weeks of COVID-19 vaccination between May 2021 and May 2022. MRI findings suggestive of SIRVA were reviewed, including subacromial bursitis, rotator cuff tears, and adhesive capsulitis. Demographic data, vaccine type, clinical symptoms, and treatments were collected. Follow-up interviews (1–30 September 2024) assessed symptom persistence and vaccine hesitancy. Descriptive statistics and Chi-square tests were used to explore associations. Results: Of the 35 patients (mean age 53.6 ± 9.0 years; 54.3% female), subacromial bursitis was the most common MRI finding (89.5%), followed by tendonitis (47.4%) and adhesive capsulitis (36.8%). Tendonitis correlated with older age (p = 0.024) and AstraZeneca vaccination (p = 0.033). Subacromial bursitis was linked to female sex (p = 0.013) and higher BMI (p = 0.023). Adhesive capsulitis was associated with receiving the Sinopharm vaccine (p = 0.029). Persistent symptoms (22.9%) were more common in younger patients, women, and those with right-sided injections. Conclusions: SIRVA following COVID-19 vaccination showed different MRI patterns associated with female sex, higher BMI, and vaccine type. Awareness of these patterns may expedite recognition of COVID-19-associated SIRVA in routine practice.
Full article

Figure 1
Open AccessReview
Medical Image Segmentation: A Comprehensive Review of Deep Learning-Based Methods
by
Yuxiao Gao, Yang Jiang, Yanhong Peng, Fujiang Yuan, Xinyue Zhang and Jianfeng Wang
Tomography 2025, 11(5), 52; https://doi.org/10.3390/tomography11050052 - 30 Apr 2025
Cited by 4
Abstract
Medical image segmentation is a critical application of computer vision in the analysis of medical images. Its primary objective is to isolate regions of interest in medical images from the background, thereby assisting clinicians in accurately identifying lesions, their sizes, locations, and their
[...] Read more.
Medical image segmentation is a critical application of computer vision in the analysis of medical images. Its primary objective is to isolate regions of interest in medical images from the background, thereby assisting clinicians in accurately identifying lesions, their sizes, locations, and their relationships with surrounding tissues. However, compared to natural images, medical images present unique challenges, such as low resolution, poor contrast, inconsistency, and scattered target regions. Furthermore, the accuracy and stability of segmentation results are subject to more stringent requirements. In recent years, with the widespread application of Convolutional Neural Networks (CNNs) in computer vision, deep learning-based methods for medical image segmentation have become a focal point of research. This paper categorizes, reviews, and summarizes the current representative methods and research status in the field of medical image segmentation. A comparative analysis of relevant experiments is presented, along with an introduction to commonly used public datasets, performance evaluation metrics, and loss functions in medical image segmentation. Finally, potential future research directions and development trends in this field are predicted and analyzed.
Full article
(This article belongs to the Section Artificial Intelligence in Medical Imaging)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- Tomography Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Editorial Office
- 10th Anniversary
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Anatomia, Biomedicines, IJMS, Medicina, Tomography
Human Anatomy and Pathophysiology, 3rd Edition
Topic Editors: Francesco Cappello, Mugurel Constantin RusuDeadline: 31 May 2026

Conferences
Special Issues
Special Issue in
Tomography
Functional and Molecular Imaging of the Abdomen
Guest Editor: Michael T. McMahonDeadline: 30 June 2025
Special Issue in
Tomography
Clinical and Molecular Analytic in Neuro-Oncology
Guest Editors: Alessandro Pesce, Angelo Pompucci, Maurizio Salvati, Alessandro FratiDeadline: 30 November 2025
Special Issue in
Tomography
Emergent Perspectives in Oncology Imaging
Guest Editors: Mariano Scaglione, Leandra PiscopoDeadline: 30 December 2025
Special Issue in
Tomography
Orthopaedic Radiology: Clinical Diagnosis and Application
Guest Editor: Olumide A. DanisaDeadline: 31 December 2025








