- Review
Prehabilitation in Plastic Surgery: Optimizing Patients for Superior Surgical Outcomes
- Jelena Nikolić,
- Marija Marinković and
- Ivana Mijatov
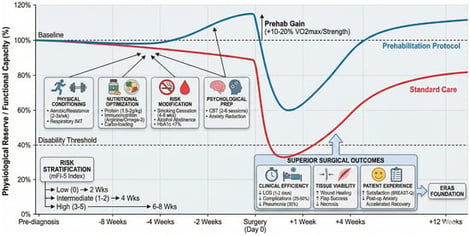
Prehabilitation represents a proactive, multimodal strategy to enhance patient resilience prior to plastic and reconstructive surgery, building on the success of Enhanced Recovery After Surgery (ERAS) pathways. This narrative review synthesizes the conceptual framework of prehabilitation—encompassing exercise training, nutritional optimization, risk factor modification, and psychological preparation—and examines its current application within plastic surgery. While evidence from selected randomized trials and systematic reviews in orthopedic and colorectal surgery suggests potential reductions in complications (often in the range of 20–40% in higher-risk populations), the results remain heterogeneous and context-dependent. To date, there have been no randomized controlled trials on plastic surgery, despite unique patient populations facing modifiable risks, including smoking, obesity, and malnutrition. This review proposes a risk-stratified prehabilitation framework tailored to key plastic surgery domains: breast reconstruction, head-and-neck microsurgery, post-bariatric body contouring, and major esthetic procedures. Practical implementation strategies address timelines, multidisciplinary teams, and digital delivery tools. By positioning prehabilitation as a structured preoperative component within ERAS pathways, plastic surgeons may support better perioperative readiness, potentially influencing complications, recovery, and patient experience. This review proposes conceptual frameworks intended to guide structured evaluation and future clinical research in plastic surgery.
12 March 2026