- Perspective
WALANT vs. Axillary Block for Dual Mobility Trapeziometacarpal Prosthesis: A Prospective Comparative Study
- Edoardo Biondi,
- Guido Koverech and
- Matteo Guzzini
- + 2 authors
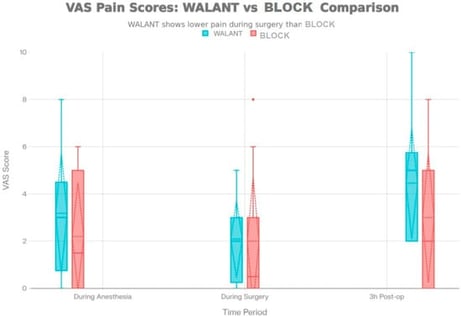
Background/Objectives: Thumb basal joint arthritis is a common degenerative condition often requiring surgery when conservative treatment fails. Dual mobility trapeziometacarpal prostheses are increasingly used, but the optimal anesthetic strategy remains debatable. This study aimed to explore whether WALANT provides intraoperative analgesia and short-term safety comparable to axillary block in dual mobility trapeziometacarpal arthroplasty. Methods: A prospective observational comparative study was carried out on 21 patients (11 WALANT, 10 axillary block) undergoing dual mobility trapeziometacarpal prosthesis for stage II–III in thumb basal joint arthritis according to Eaton–Littler classification at two hospital facilities of ASL Roma 5, from February–December 2025. Patients treated with the WALANT technique were assigned to Group A, whereas those undergoing an axillary block were assigned to Group B. Pain intensity was recorded on a 0–10 visual analogue scale at three stages: during anesthetic administration, during surgery, and 3 h after the procedure. Group A received a field infiltration with 1% mepivacaine combined with epinephrine 1:100,000 and sodium bicarbonate, while Group B underwent an ultrasound-guided brachial plexus block using 0.5–0.7% ropivacaine and a pneumatic tourniquet inflated to 250 mmHg. Results: Pain during anesthesia induction was similar between groups (Group A 3.18 ± 2.89 vs. Group B 2.20 ± 2.37, p = 0.393). Intraoperative pain did not differ significantly (Group A 2.27 ± 1.79 vs. Group B 2.00 ± 2.71, p = 0.898). At 3 h postoperative, Group B showed a trend toward lower pain levels (Group A 4.36 ± 2.54 vs. Group B 3.00 ± 3.08, p = 0.244). No anesthetic failures, no conversion to general anesthesia, and no neurological or ischemic complications occurred in either group. Conclusions: In this prospective observational comparative cohort, WALANT and axillary block provide comparable intraoperative analgesia for dual mobility trapeziometacarpal prosthesis, with comparable safety profiles. WALANT offers advantages in ease of administration, absence of tourniquet-related risks, and potential for intraoperative functional testing. Axillary block provides more prolonged postoperative analgesia in the first 3 h. The choice between techniques should be individualized based on patient-specific factors, anxiety profile, and local expertise. These results should be interpreted as preliminary and hypothesis-generating, given the exploratory design, the small sample size, and the limited statistical power of the study.
26 February 2026