- Review
Anaesthesia in Microsurgical Flap Reconstruction: A Review
- Arturi Federica,
- Serra Letizia and
- Barbieri Alberto
- + 5 authors
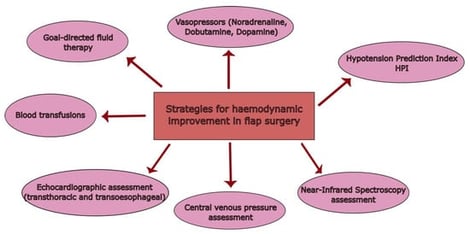
Background: In head and neck reconstructive surgery, flap loss remains a major complication and continues to represent a significant challenge in perioperative management. Although free tissue transfer is widely used, unsatisfactory outcomes are still reported across different flap procedures. Anaesthetic management plays an important role in influencing flap perfusion through its effects on systemic haemodynamics, regional blood flow, and microcirculation. However, there is currently no consensus on universally acceptable haemodynamic targets, and the impact of intraoperative strategies appears to be highly application-specific. Materials and Methods: This narrative review was conducted in accordance with the 2019 SANRA guidelines. PubMed® was used as the primary database for literature selection. Relevant studies addressing anaesthetic management in head and neck free flap surgery were reviewed, with a particular focus on intraoperative haemodynamic control, ischemia–reperfusion injury, fluid and transfusion management, vasoactive agents, and advanced monitoring techniques. Results: Ischemia–reperfusion injury represents a major mechanism of vascular compromise in free flap surgery and has a significant impact on microcirculatory perfusion. The literature suggests that several anaesthetic strategies—including goal-directed fluid therapy, cautious use of vasopressors, and advanced haemodynamic monitoring—may support intraoperative haemodynamic stability and improve flap perfusion. Nevertheless, the magnitude of haemodynamic improvement achievable with these strategies and their effect on graft survival vary according to patient characteristics, surgical factors, and flap type. Conclusions: Current evidence indicates that anaesthetic management has the potential to contribute to improved intraoperative haemodynamic control in head and neck free flap reconstruction, thereby supporting graft viability. However, haemodynamic targets and management strategies cannot be generalised and should be interpreted within specific clinical contexts. Rather than aiming for optimisation, future research should focus on defining acceptable clinical outcomes for individual applications and on evaluating whether achievable haemodynamic improvements are sufficient to reduce flap-related complications to clinically acceptable levels.
9 February 2026






![PRISMA flow diagram illustrating the study selection process [16]. * Databases searched include MEDLINE (via PubMed), Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL). ** Records were excluded by human reviewers during the title and abstract screening phase based on the predefined eligibility criteria; no automation tools were utilized for this process.](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/surgeries/surgeries-07-00020/article_deploy/html/images/surgeries-07-00020-g001-550.jpg)