The Impact of Intraoperative Traffic and Door Openings on Surgical Site Infections: An Umbrella Review
Abstract
1. Introduction
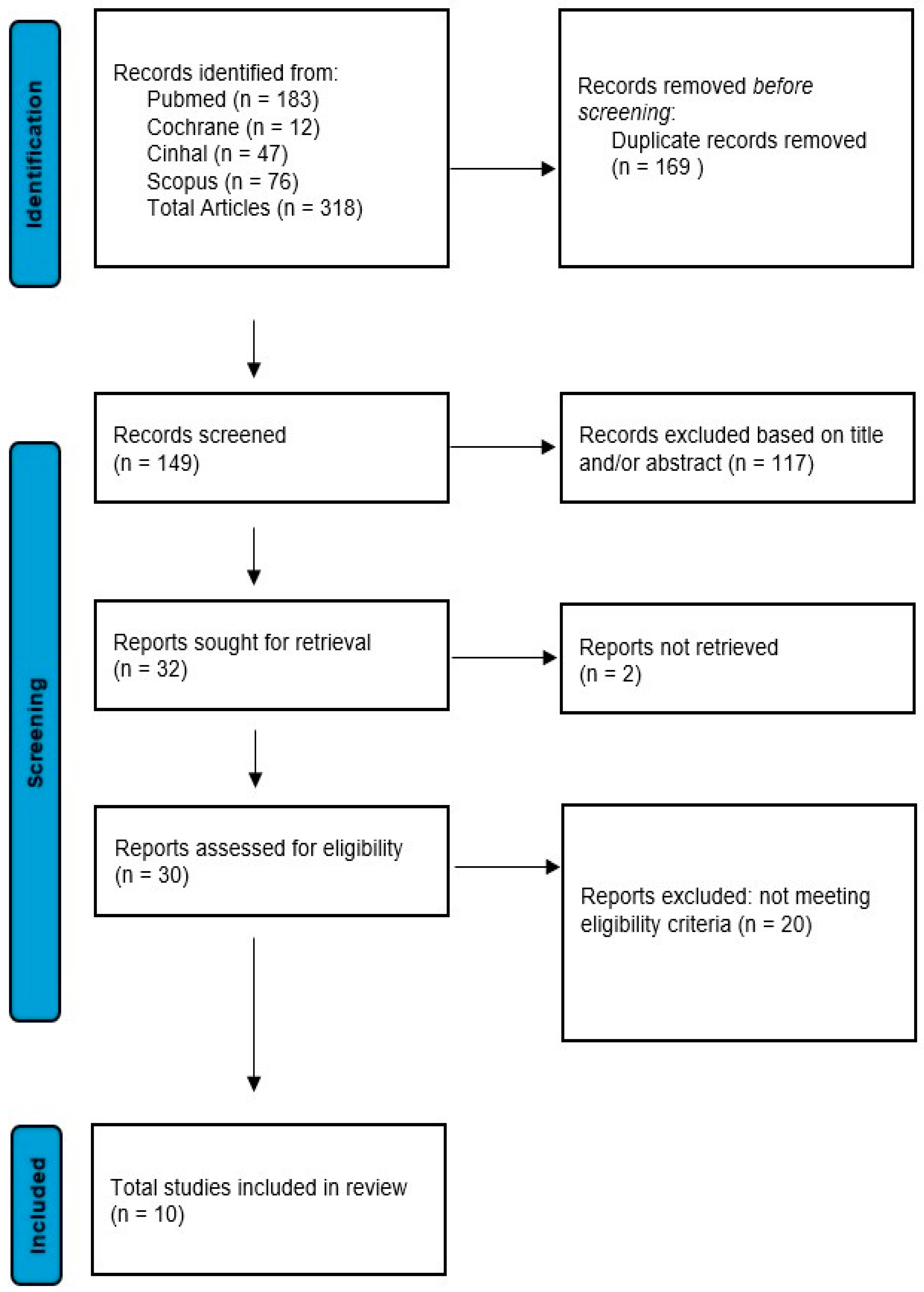
2. Materials and Methods
2.1. Study Design
2.2. Problem Identification
2.3. Inclusion and Exclusion Criteria
2.4. Literature Search
2.5. Data Extraction and Synthesis
3. Results
| Author (Year) Country | Study Design | Objective | Population | Main Results | Quantitative Data |
|---|---|---|---|---|---|
| Lynch et al. [20] (2009). USA | Quantitative–Descriptive Study | Determines the number of door openings in the OR and the role of nursing staff | 28 surgical procedures observed | Nursing staff responsible for 37–52% of door openings | Door openings: 52% nurses, 24% surgeons, 18% anesthesiologists |
| Parikh et al. [19] (2010), USA | Quantitative–Descriptive Study | Determines the number of door openings in the OR and the role of nursing staff | 30 pediatric procedures | High number of door openings correlated with infection risk | Average door openings per procedure: 79, Infection risk >100 openings: 2.49× |
| Bohl et al. [24] (2010), USA | Randomized Controlled Trial | Evaluates the impact of intraoperative traffic on surgical site infection rates | 1116 neurosurgical cases | Infection rate paradoxically higher in the reduced traffic group | Infection rate in reduced traffic group: 3.8%, normal group: 2.1% |
| Kurmann et al. [27] (2011), Switzerland | Observational Study | Evaluates the impact of noise in the OR on the risk of surgical site infections | Patients undergoing surgery | Significant increase in infections with high intraoperative noise levels | Increased infection risk: +20%, Noise level: >80 dB |
| Andersson et al. [21] (2012), Sweden | Descriptive Observational Study | Analyzes air quality and the number of people present in the OR | 30 orthopedic surgical procedures | Strong correlation between microbial air contamination and the number of people present | OR traffic: 18 door openings/hour, Air contamination: +15% |
| Mathijssen et al. [23] (2016), Netherlands | Quantitative–Descriptive Study | Examines the correlation between door openings and microbial air contamination | Hip revision surgery | Door openings associated with a significant increase in microbial contamination | CFU increase after >100 door openings: +26.6% |
| Wanta et al. [22] (2016), USA | Case–Control Study | Evaluates the impact of intraoperative traffic on the risk of superficial surgical site infections | Adult patients (>18 years) undergoing clean surgical procedures | No significant correlation after risk adjustment analysis | Average traffic: 35 events, no significant association |
| Stauning et al. [26] (2018), Ghana/Denmark | Observational Study | Evaluates microbial air contamination in relation to intraoperative traffic | 124 general surgery patients | 2.5% increase in microbial contamination for each additional person in the room | Contamination increase per person in the room: +2.5% |
| Roth et al. [25] (2019), Switzerland | Prospective Observational Study | Determines the effect of door openings in cardiac surgery on surgical site infections | 688 patients undergoing cardiac surgery | Internal door openings were significantly correlated with infection risk | Door openings in cardiac surgery: 68% correlated with infections |
| Bediako-Bowan et al. [18] (2020), Ghana | Prospective Cohort Study | Analyzes risk factors associated with surgical site infections in abdominal surgery | 358 patients undergoing abdominal surgery | Tripled risk of infections when more than 10 people are in the room | Infection risk: +3.1×, People in the room: >10 |
| Macro-Area | Analyzed Variables | Reference Articles | Main Results |
|---|---|---|---|
| Intraoperative Traffic | Effect of Traffic Reduction on SSI | Wanta et al. [22], Bohl et al. [24], Roth et al. [25] | Traffic reduction showed a variable effect on SSI: not statistically significant (p = 0.06, p = 0.75, p = 0.83) |
| Operating Room Traffic Monitoring | Parikh et al. [19] | High number of door openings and traffic significantly correlated with infections (statistically significant, p < 0.05) | |
| Intraoperative Traffic as a Modifiable Risk Factor | Wanta et al. [22] | Intraoperative traffic identified as a modifiable risk factor for SSI (statistically significant, p = 0.006) | |
| Total Number of Traffic Events and SSI | Wanta et al. [22] | Total number of traffic events was significantly higher in SSI cases compared to non-SSI cases (statistically significant, p = 0.006) | |
| Effect of Operating Room Traffic on Infections | Bohl et al. [24] | BRITE trial: association between traffic and infections, but not statistically significant (p > 0.05) | |
| Door Openings | Number of Door Openings per Procedure and SSI | Parikh et al. [19] | More than 100 door openings per procedure were associated with an SSI incidence of 26.6% (95% CI: 19.1–35.3), with an RR of 2.49 (95% CI: 1.48–4.18) |
| Number of Door Openings and SSI Risk | Mathijssen et al. [23] | >100 door openings per procedure significantly increased microbial contamination (statistically significant, p < 0.001) | |
| Impact of Door Openings on Microbial Contamination | Mathijssen et al. [23] | Every 100 door openings increased microbial contamination by 26.6% (statistically significant, p < 0.001) | |
| Impact of Door Openings in Abdominal Surgeries | Bediako-Bowan et al. [18] | Door openings during abdominal surgery tripled SSI risk (statistically significant, p < 0.01) | |
| Frequent Door Openings and SSI Risk in Cardiac Surgery | Roth et al. [25] | Frequent door openings in cardiac surgery increased SSI risk by 68% (statistically significant, p < 0.05) | |
| Microbial Contamination | Traffic Flow and Air Contamination | Andersson et al. [21] | High traffic in orthopedic surgery correlated with increased air contamination in the OR (statistically significant, p = 0.001) |
| Number of People in the Operating Room and Microbial Contamination | Stauning et al. [26] | Each additional person in the OR increased microbial contamination by 2.5% (statistically significant, p < 0.001) | |
| Intraoperative Factors and Microbial Contamination | Stauning et al. [26] | Intraoperative factors like general anesthesia and incision time significantly influenced microbial contamination (statistically significant, p < 0.001) | |
| Operating Room Traffic Flow and Air Quality | Stauning et al. [26] | High traffic flow in surgical wards in Ghana correlated with airborne contamination (statistically significant, p = 0.001 for number of persons and CFU/m3) | |
| Microbial Contamination and Intraoperative Noise | Kurmann et al. [27] | High intraoperative noise levels were significantly associated with increased SSI risk (statistically significant, p < 0.05) | |
| Pedestrian Traffic Measurement and Infection Control Implications | Lynch et al. [20] | Greater pedestrian traffic in the OR linked to increased SSI risk (statistical significance not reported) |
3.1. Intraoperative Traffic
3.2. Door Openings
3.3. Microbial Air Contamination
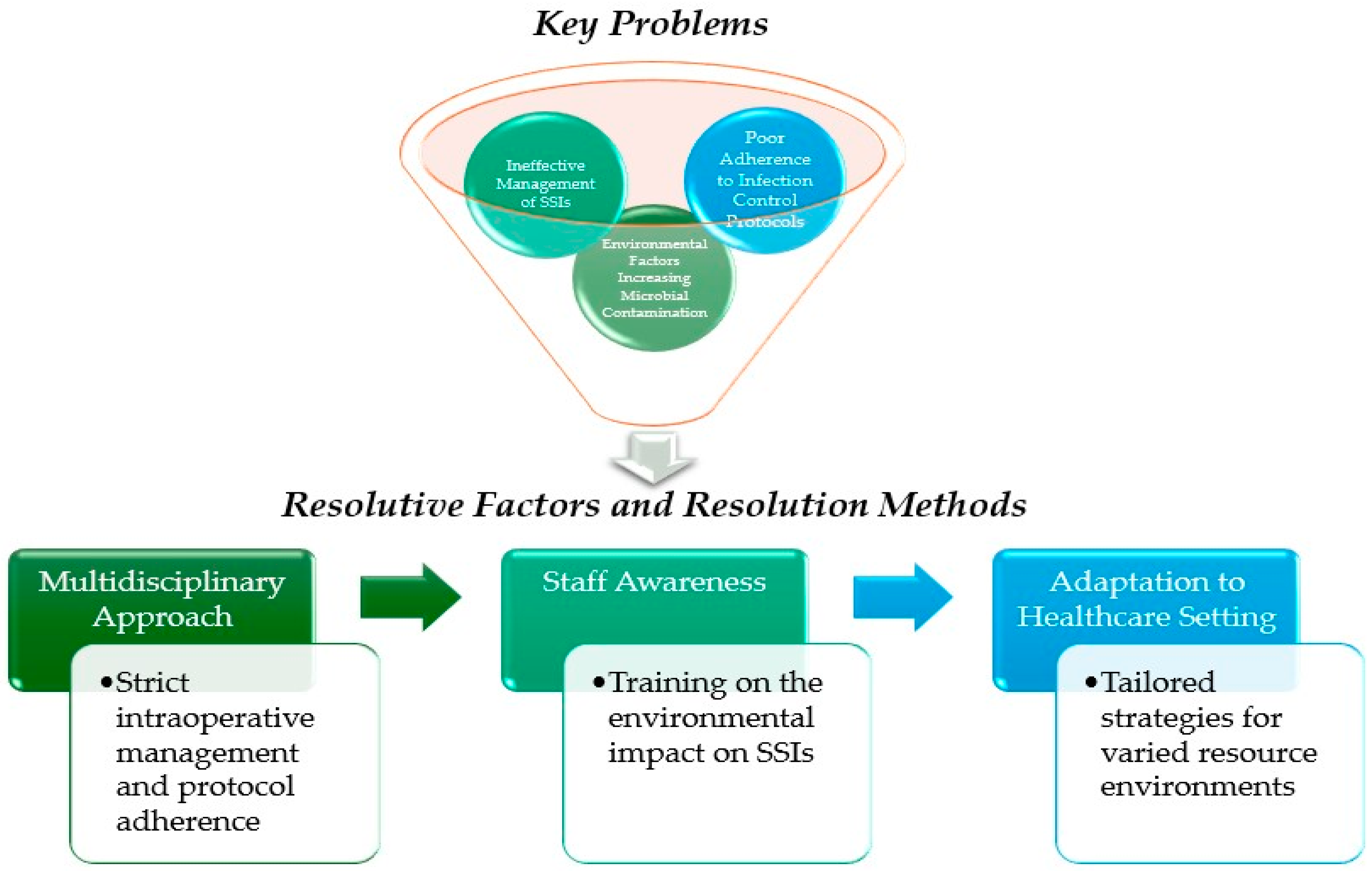
4. Discussion
4.1. Limitations
4.2. Implications for Clinical Practice
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A. Search Strategy
| Database | Search Queries |
| Cinahl | (“Surgical Wound Infection*” OR “surgical site infection*”) AND (“operating room traffic” OR “door openings”) |
| Cochrane | (“Surgical Wound infection (MeSH)” OR “Surgical Site Infection” OR “Surgical Site Infections” OR “Surgical Wound Infection” OR “Surgical Wound Infections”) AND (“Operating room traffic” OR “door openings”) (“Surgical Wound Infection” OR “surgical site infections”) AND (“operating room traffic” OR “door openings”) “Surgical Wound Infection” AND “operating room traffic” “surgical site infections” AND “operating room traffic” “Surgical Wound Infection”[Mesh]) AND “door openings” “surgical site infections” AND “door openings” |
| PubMed | “surgical site infections” AND “operating room foot traffic” (“Surgical Wound Infection”[Mesh]) AND “operating room foot traffic” (“Surgical Wound Infection”[Mesh] OR “surgical site infections”) AND (“operating room traffic” OR “door openings”) “Surgical Wound Infection”[Mesh]) AND “operating room traffic” “surgical site infections” AND “operating room traffic” “Surgical Wound Infection”[Mesh]) AND “door openings” “surgical site infections” AND “door openings” (“Surgical Wound Infection”[Mesh] OR “surgical site infection*”) AND (“operating room traffic” OR “door openings”) |
| Scopus | (“Surgical Wound Infection*” OR “surgical site infection*”) AND (“operating room traffic” OR “door openings”) |
References
- Borchardt, R.A.; Tzizik, D. Update on surgical site infections: The new CDC guidelines. JAAPA 2018, 31, 52–54. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità. Protocollo per la Sorveglianza delle Infezioni del Sito Chirurgico. EpiCentro. 2022. Available online: https://www.epicentro.iss.it/sorveglianza-ica/pdf/Protocollo%20Sito%20chirurgico%20VERS%20definitiva%2012%2010%2022-1.pdf (accessed on 28 March 2025).
- World Health Organization. Global Guidelines for the Prevention of Surgical Site Infection, 2nd ed.; World Health Organization: Geneva, Switzerland, 2018; Available online: https://iris.who.int/handle/10665/277399 (accessed on 19 February 2024).
- Seidelman, J.L.; Mantyh, C.R.; Anderson, D.J. Surgical site infection prevention: A review. JAMA 2023, 329, 244–252. [Google Scholar] [CrossRef]
- Chauveaux, D. Preventing surgical-site infections: Measures other than antibiotics. Orthop. Traumatol. Surg. Res. 2015, 101 (Suppl. S1), S77–S83. [Google Scholar] [CrossRef]
- Avsar, P.; Patton, D.; Ousey, K.; Blackburn, J.; O’Connor, T.; Moore, Z. The impact of surgical site infection on health-related quality of life: A systematic review. Wound Manag. Prev. 2021, 67, 10–19. [Google Scholar] [CrossRef]
- Han, C.; Chen, W.; Ye, X.L.; Cheng, F.; Wang, X.Y.; Liu, A.B.; Mu, Z.H.; Jin, X.J.; Weng, Y.H. Risk factors analysis of surgical site infections in postoperative colorectal cancer: A nine-year retrospective study. BMC Surg. 2023, 23, 320. [Google Scholar] [CrossRef] [PubMed]
- Shambhu, S.; Gordon, A.S.; Liu, Y.; Pany, M.; Padula, W.V.; Pronovost, P.J.; Hsu, E. The burden of health care utilization, cost, and mortality associated with select surgical site infections. Jt. Comm. J. Qual. Patient Saf. 2024, 50, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Podgorny, K.; Berríos-Torres, S.I.; Bratzler, D.W.; Dellinger, E.P.; Greene, L.; Nyquist, A.C.; Saiman, L.; Yokoe, D.S.; Maragakis, L.L.; et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect. Control Hosp. Epidemiol. 2014, 35, 605–627. [Google Scholar] [CrossRef] [PubMed]
- Neumayer, L.; Hosokawa, P.; Itani, K.; El-Tamer, M.; Henderson, W.G.; Khuri, S.F. Multivariable predictors of postoperative surgical site infection after general and vascular surgery: Results from the Patient Safety in Surgery Study. J. Am. Coll. Surg. 2007, 204, 1178–1187. [Google Scholar] [CrossRef]
- Kanamori, H.; Rutala, W.A.; Gergen, M.F.; Weber, D.J. Perioperative bacterial contamination from patients on contact precaution in operating room environment. Open Forum Infect. Dis. 2020, 7, ofaa508. [Google Scholar] [CrossRef]
- Healthcare Infection Society (HIS). Guidelines to reduce ritualistic behavior in operating theatres without increasing surgical site infection risk. J. Hosp. Infect. 2023, 140, 165.e1–165.e28. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Guidelines for Indoor Air Quality: Selected Pollutants; WHO Regional Office for Europe: Geneva, Switzerland, 2010; Available online: https://www.who.int/publications/i/item/9789289002134 (accessed on 28 March 2025).
- Western Australia Department of Health. Microbiological Air Sampling of Operating Rooms; Western Australia Department of Health: East Perth, WA, Australia, 2021. Available online: https://www.health.wa.gov.au/~/media/Corp/Documents/Health-for/Communicable-Diseases/Guidelines/Guideline-Microbiological-Air-Sampling-of-ORs.pdf (accessed on 19 February 2025).
- Cristina, M.L.; Spagnolo, A.M.; Ottria, G.; Schinca, E.; Dupont, C.; Carbone, A.; Oliva, M.; Sartini, M. Microbial air monitoring in turbulent airflow operating theatres: Is it possible to calculate and hypothesize new benchmarks for microbial air load? Int. J. Environ. Res. Public Health 2021, 18, 10379. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Brown, D. A review of the PubMed PICO tool: Using evidence-based practice in health education. Health Promot. Pract. 2020, 21, 496–498. [Google Scholar] [CrossRef]
- Bediako-Bowan, A.A.A.; Mølbak, K.; Kurtzhals, J.A.L.; Owusu, E.; Debrah, S.; Newman, M.J. Risk factors for surgical site infections in abdominal surgeries in Ghana: Emphasis on the impact of operating room door openings. Epidemiol. Infect. 2020, 148, e147. [Google Scholar] [CrossRef]
- Parikh, S.N.; Grice, S.S.; Schnell, B.M.; Salisbury, S.R. Operating room traffic: Is there any role of monitoring it? J. Pediatr. Orthop. 2010, 30, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Lynch, R.J.; Englesbe, M.J.; Sturm, L.; Bitar, A.; Budhiraj, K.; Kolla, S.; Polyachenko, Y.; Duck, M.G.; Campbell, D.A., Jr. Measurement of foot traffic in the operating room: Implications for infection control. Am. J. Med. Qual. 2009, 24, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Andersson, A.E.; Bergh, I.; Karlsson, J.; Eriksson, B.I.; Nilsson, K. Traffic flow in the operating room: An explorative and descriptive study on air quality during orthopedic trauma implant surgery. Am. J. Infect. Control 2012, 40, 750–755. [Google Scholar] [CrossRef] [PubMed]
- Wanta, B.T.; Glasgow, A.E.; Habermann, E.B.; Kor, D.J.; Cima, R.R.; Berbari, E.F.; Curry, T.B.; Brown, M.J.; Hyder, J.A. Operating room traffic as a modifiable risk factor for surgical site infection. Surg. Infect. 2016, 17, 755–760. [Google Scholar] [CrossRef]
- Mathijssen, N.M.; Hannink, G.; Sturm, P.D.; Pilot, P.; Bloem, R.M.; Buma, P.; Petit, P.L.; Schreurs, B.W. The effect of door openings on numbers of colony forming units in the operating room during hip revision surgery. Surg. Infect. 2016, 17, 535–540. [Google Scholar] [CrossRef]
- Bohl, M.A.; Clark, J.C.; Oppenlander, M.E.; Chapple, K.; Budde, A.; Lei, T.; Meeusen, A.J.; Porter, R.W.; Spetzler, R.F. The Barrow randomized operating room traffic (BRITE) trial: An observational study on the effect of operating room traffic on infection rates. Neurosurgery 2016, 63 (Suppl. S1), 91–95. [Google Scholar] [CrossRef]
- Roth, J.A.; Juchler, F.; Dangel, M.; Eckstein, F.S.; Battegay, M.; Widmer, A.F. Frequent door openings during cardiac surgery are associated with increased risk for surgical site infection: A prospective observational study. Clin. Infect. Dis. 2019, 69, 290–294. [Google Scholar] [CrossRef]
- Stauning, M.T.; Bediako-Bowan, A.; Andersen, L.P.; Opintan, J.A.; Labi, A.K.; Kurtzhals, J.A.L.; Bjerrum, S. Traffic flow and microbial air contamination in operating rooms at a major teaching hospital in Ghana. J. Hosp. Infect. 2018, 99, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Kurmann, A.; Peter, M.; Tschan, F.; Mühlemann, K.; Candinas, D.; Beldi, G. Adverse effect of noise in the operating theatre on surgical-site infection. Br. J. Surg. 2011, 98, 1021–1025. [Google Scholar] [CrossRef]
- Lansing, S.S.; Moley, J.P.; McGrath, M.S.; Stoodley, P.; Chaudhari, A.M.W.; Quatman, C.E. High number of door openings increases the bacterial load of the operating room. Surg. Infect. 2021, 22, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Schafer, M.; Dixon, H.; Palladino, K.; Baumann, S.; Martinson, J.; Bolland, M.; Lakdawala, M.; Yassin, M. Automated traffic monitoring of neurosurgical operating room. Am. J. Infect. Control 2024, 52, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.L.; Lipps, J.A.; Pritchard, C.L.; Venkatachalam, A.M.; Olson, D.M. An operating room audit to examine for patterns of staff entry/exit: Pattern sequencing as a method of traffic reduction. J. Infect. Prev. 2021, 22, 69–74. [Google Scholar] [CrossRef]
- Parent, M. OR traffic and surgical site infections: A quality improvement project. AORN J. 2021, 113, 379–388. [Google Scholar] [CrossRef]
- Crolla, R.M.P.H.; van der Laan, L.; Veen, E.J.; Hendriks, Y.; van Schendel, C.; Kluytmans, J. Reduction of surgical site infections after implementation of a bundle of care. PLoS ONE 2012, 7, e44599. [Google Scholar] [CrossRef]
- van der Slegt, J.; van der Laan, L.; Veen, E.J.; Hendriks, Y.; Romme, J.; Kluytmans, J. Implementation of a bundle of care to reduce surgical site infections in patients undergoing vascular surgery. PLoS ONE 2013, 8, e71566. [Google Scholar] [CrossRef]
- Qvistgaard, M.; Lovebo, J.; Almerud-Österberg, S. Intraoperative prevention of surgical site infections as experienced by operating room nurses. Int. J. Qual. Stud. Health Well-Being 2019, 14, 1632109. [Google Scholar] [CrossRef]
- Wistrand, C.; Falk-Brynhildsen, K.; Nilsson, U. National Survey of Operating Room Nurses’ Aseptic Techniques and Interventions for Patient Preparation to Reduce Surgical Site Infections. Surg. Infect. 2018, 19, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Borer, A.; Gilad, J.; Meydan, N.; Riesenberg, K.; Schlaeffer, F.; Alkan, M.; Schlaeffer, P. Impact of active monitoring of infection control practices on deep sternal infection after open-heart surgery. Ann. Thorac. Surg. 2001, 72, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Esser, J.; Shrinski, K.; Cady, R.; Belew, J. Reducing OR traffic using education, policy development, and communication technology. AORN J. 2016, 103, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Aktaş, F.; Damar, H.T. Determining operating room nurses’ knowledge and use of evidence-based recommendations on preventing surgical site infections. J. PeriAnesthesia Nurs. 2022, 37, 404–410. [Google Scholar] [CrossRef]
- Ferrara, G.; Cangelosi, G.; Morales Palomares, S.; Mancin, S.; Melina, M.; Diamanti, O.; Sguanci, M.; Amendola, A.; Petrelli, F. Optimizing Ultrasound Probe Disinfection for Healthcare-Associated Infection Control: A Comparative Analysis of Disinfectant Efficacy. Microorganisms 2024, 12, 2394. [Google Scholar] [CrossRef]
- Perez, P.; Holloway, J.; Ehrenfeld, L.; Cohen, S.; Cunningham, L.; Miley, G.B.; Hollenbeck, B.L. Door openings in the operating room are associated with increased environmental contamination. Am. J. Infect. Control 2018, 46, 954–956. [Google Scholar] [CrossRef]
- Assolari, F.; Mancin, S.; Lopane, D.; Dacomi, A.; Coldani, C.; Tomaiuolo, G.; Cattani, D.; Palomares, S.M.; Cangelosi, G.; Mazzoleni, B. Advanced practice nursing in surgery: A scoping review of roles, responsibilities, and educational programs. Int. Nurs. Rev. 2024. [Google Scholar] [CrossRef]
- Sguanci, M.; Mancin, S.; Gazzelloni, A.; Diamanti, O.; Ferrara, G.; Morales Palomares, S.; Parozzi, M.; Petrelli, F.; Cangelosi, G. The Internet of Things in the Nutritional Management of Patients with Chronic Neurological Cognitive Impairment: A Scoping Review. Healthcare 2024, 13, 23. [Google Scholar] [CrossRef]
- Mieronkoski, R.; Azimi, I.; Rahmani, A.M.; Aantaa, R.; Terävä, V.; Liljeberg, P.; Salanterä, S. The Internet of Things for basic nursing care-A scoping review. Int. J. Nurs. Stud. 2017, 69, 78–90. [Google Scholar] [CrossRef]
- Sguanci, M.; Palomares, S.M.; Cangelosi, G.; Petrelli, F.; Sandri, E.; Ferrara, G.; Mancin, S. Artificial Intelligence in the Management of Malnutrition in Cancer Patients: A Systematic Review. Adv. Nutr. 2025, 16, 100438. [Google Scholar] [CrossRef]
- Cangelosi, G.; Mancin, S.; Morales Palomares, S.; Pantanetti, P.; Quinzi, E.; Debernardi, G.; Petrelli, F. Impact of School Nurse on Managing Pediatric Type 1 Diabetes with Technological Devices Support: A Systematic Review. Diseases 2024, 12, 173. [Google Scholar] [CrossRef]
- Pantanetti, P.; Cangelosi, G.; Morales Palomares, S.; Ferrara, G.; Biondini, F.; Mancin, S.; Caggianelli, G.; Parozzi, M.; Sguanci, M.; Petrelli, F. Real-World Life Analysis of a Continuous Glucose Monitoring and Smart Insulin Pen System in Type 1 Diabetes: A Cohort Study. Diabetology 2025, 6, 7. [Google Scholar] [CrossRef]
- Mezzalira, E.; Orsini, L.P.; Leardini, C.; Veronesi, G. Towards zero emissions in healthcare. The Italian experience. In Routledge Handbook of Climate Change and Health System Sustainability; Routledge: London, UK, 2024. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drago, J.; Scollo, S.; Cosmai, S.; Cattani, D.; Modena, G.; Mancin, S.; Morales Palomares, S.; Petrelli, F.; Marfella, F.; Cangelosi, G.; et al. The Impact of Intraoperative Traffic and Door Openings on Surgical Site Infections: An Umbrella Review. Surgeries 2025, 6, 61. https://doi.org/10.3390/surgeries6030061
Drago J, Scollo S, Cosmai S, Cattani D, Modena G, Mancin S, Morales Palomares S, Petrelli F, Marfella F, Cangelosi G, et al. The Impact of Intraoperative Traffic and Door Openings on Surgical Site Infections: An Umbrella Review. Surgeries. 2025; 6(3):61. https://doi.org/10.3390/surgeries6030061
Chicago/Turabian StyleDrago, Jessica, Sarah Scollo, Simone Cosmai, Daniela Cattani, Gloria Modena, Stefano Mancin, Sara Morales Palomares, Fabio Petrelli, Francesca Marfella, Giovanni Cangelosi, and et al. 2025. "The Impact of Intraoperative Traffic and Door Openings on Surgical Site Infections: An Umbrella Review" Surgeries 6, no. 3: 61. https://doi.org/10.3390/surgeries6030061
APA StyleDrago, J., Scollo, S., Cosmai, S., Cattani, D., Modena, G., Mancin, S., Morales Palomares, S., Petrelli, F., Marfella, F., Cangelosi, G., Lopane, D., & Mazzoleni, B. (2025). The Impact of Intraoperative Traffic and Door Openings on Surgical Site Infections: An Umbrella Review. Surgeries, 6(3), 61. https://doi.org/10.3390/surgeries6030061






