Abstract
Background and Clinical Significance: Angioleiomyoma (ALM) is a benign tumor that generally presents as a single lesion and, according to the updated WHO classification, includes the following three histological subtypes: solid (or capillary), cavernous, and venous. Typically, ALMs are described as well-defined nodules in the lower extremities but are unusually located in the acral locations and toes. We summarize two cases of ALM and perform a systematic review to provide foot surgeons with the most up-to-date and useful information on the epidemiological aspects, anatomical distribution, and specific histological subtypes of ALM in the foot. Materials and Methods: A systematic review was carried out according to the criteria of a PICO framework, and a systematic search and data processing were carried out according to the PRISMA guidelines. We analyzed patient demographics, clinical characteristics, diagnostic workup, treatment, and clinical outcomes. Each one of the included articles was independently assessed for methodological quality and risk of bias by an independent evaluator. The risk of bias of the included studies was assessed based on their characteristics. Results: This systematic review included 14 case series with 172 reported cases of ALM. One hundred and seventy-two (18.57%) were cases of ALM located on foot, excluding the ankle region. The female-to-male ratio was 1.48. The most common location was the hindfoot (41.5%), followed by the forefoot (20.2%) and the midfoot (8.9%). In 29.4% of cases, the location of the lesions could not be determined. The most frequent location of the lesions was subcutaneous (69%), followed by subaponeurotic (16.5%) and skin (14.5%) locations. The most frequent histological presentation was the solid histologic subtype (65%), followed by the venous subtype (21%) and the cavernous subtype (14%), respectively. Of the total reported cases of ALM located in foot, 63.1% presented as solid painful lesions. Calcified presentations occurred in 7% of cases, with more than half of the cases located in the hindfoot. Surgical excision was the treatment of choice in the two herein reported cases of solid ALM located in the hindfoot, one of them with a calcified presentation. No recurrence was observed in either case after two and five years of follow-up, respectively. All cases reviewed after surgical excision showed a low recurrence rate with a favorable prognosis regardless of the histological subtype and a very rare tendency toward malignancy. Conclusions: ALMs of the foot present as well-defined, painful nodules in the subcutaneous tissue of middle-aged women. Solid histological subtypes are the most prevalent. Histopathological analysis is usually essential for confirmation. Treatment consists primarily of direct excision, with remarkably low recurrence rates.
1. Introduction and Clinical Significance
Angioleiomyomas (ALMs), or vascular leiomyomas, are benign neoplasms originating from non-striated arterial or venous smooth muscle cells, particularly in the tunica media. It is estimated that ALM has a prevalence of around 5% among all benign soft tissue neoplasms. It is commonly found in subcutaneous or subaponeurotic tissues of the lower extremities. Minor traumas, venous stasis, and hormonal changes have been proposed as etiologic features; however, its exact histogenesis is still debated. ALM usually presents primarily in middle-aged women as a solitary, painful, slow-growing subcutaneous nodule [1,2].
From a histopathological point of view, ALM is a distinct variant of leiomyoma that includes the following three histological subtypes depending on the size, thickness, and shape of the vascular channels: capillary or solid, venous, and cavernous subtypes [3]. Solid and venous ALMs represent approximately 90% of cases, with the solid subtype being the most common, with approximately 66% of the cases described [2,4]. ALM and myopericytoma are closely related tumors with a common concentric growth pattern of myoid cells, particularly in the venous or cavernous subtypes, and similar immunohistochemical findings for smooth muscle markers [5].
The presence of calcifications in ALM has been reported more often in acral locations, probably related to repetitive minor trauma. This dystrophic calcification can masquerade as the real nature of ALM and has been interpreted as degenerative in nature [6,7].
Despite the low incidence of acral ALM, in the last two decades, the number of reported cases has increased markedly, probably related to the increase in medical research. However, the demographics of acral ALMs have been poorly described in the literature. The low reported incidence could be due to previous studies that have produced limited data due to a lack of interdisciplinary approaches or restricted patient populations.
We present two case reports describing the clinical management of solid ALMs located in the hindfoot, one of them with a calcified presentation. At the same time, and due to the low reported incidence of acral ALM of the foot, we consider it appropriate to conduct a systematic review to provide surgeons with the most up-to-date and useful information related to the demographic aspects, anatomical distribution, and specific histological subtypes of ALMs on the foot.
2. Case Presentation
The present two case reports followed the CARE (CAse REport) statement and checklist guidelines [8].
2.1. Case 1
A 57-year-old male with a history of hypertension and hyperthyroidism presented with a lump in his left heel for over 2 years. This was causing pain when wearing closed shoes due to friction.
The clinical examination of the patient revealed a single mass mimicking a soft-tissue tumor on the posterior aspect of the heel (insertion of the Achilles tendon area), which was palpable. On ultrasound examination, we observed a well-defined nodule with a size of 11.2 mm × 3.6 mm with a hypoechogenic aspect, superficial to the insertion of the Achilles tendon, with a negative Doppler color. We explained to the patient that surgery was the only option to remove the mass, which he agreed to. The surgery was performed under local anesthesia. A transverse incision was made in the skin, and the white glistening subcutaneous nodule was identified, exposed, and removed. The subcutaneous cellular tissue and skin were closed with 4/0 absorbable and 4/0 nylon suture, respectively. Histological and immunohistochemical findings confirmed the diagnosis of ALM. Histopathological exam at low magnification showed a well-defined and homogeneous nodular lesion surrounded by a fibrous pseudo capsule. At high magnification, eosinophilic, fusiform, atypical cells were observed, arranged in fascicles. Blood vessels with thick muscular (venous) and thin (cavernous) walls, interspersed with fascicles, were also identified. No images of mitosis were isolated. The cellular component showed strong and diffuse immunostaining for smooth muscle actin (SMA) and desmin, consistent with smooth muscle differentiation (Figure 1). Twenty-two months after surgery, the patient had no recurrence of the mass.
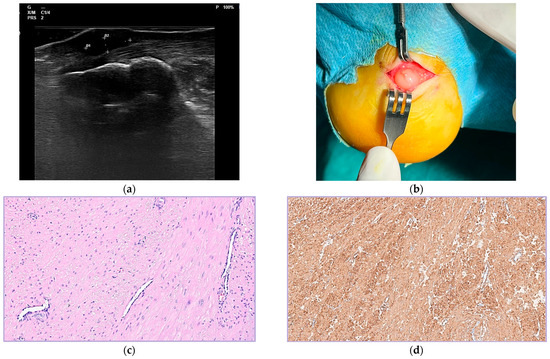
Figure 1.
Ultrasound image. A well-defined, hypoechoic, ovoid subcutaneous nodule without internal blood flow signals can be observed in contact with the Achilles tendon (a). Intraoperative appearance of tumor prior to resection. White glistening subcutaneous nodule can be observed (b). At high magnification, eosinophilic, spindle-shaped, and bland cells are observed, arranged in fascicles. Blood vessels with thick (venous) and thin (cavernous) muscular walls are also seen interspersed with the fascicles. Images of mitoses are not isolated. (H/E, 20×). Immunohistochemical study shows spindle cells (c) with strong and diffuse immunostaining for α-smooth muscle actin (d).
2.2. Case 2
A 53-year-old woman with no relevant medical history consulted for a painful lump on the medial edge of the heel of her left foot that had been developing for 6 months with progressive growth. Ultrasound examination revealed a well-defined nodule with a maximum diameter of 7 mm, a hypoechoic appearance located in the subcutaneous tissue, and a negative Doppler color signal. Radiological examination revealed the presence of a lesion with irregular edges and a bone density that did not adhere to calcaneus. The proposed surgical procedure was an excisional biopsy, which the patient accepted. The surgery was performed under local anesthesia. A longitudinal incision was made in the skin, and a well-encapsulated subcutaneous lesion was located and completely excised. The subcutaneous tissue and skin were properly sutured, and the patient was discharged.
At low magnification, the histopathological characteristics showed a well-defined and encapsulated neoformation, most of which was calcified, and only in certain areas was the presence of a proliferation of spindle cells whose characteristics were compatible with smooth muscle cells detected (Figure 2). At high magnification, smooth muscle cell proliferation was observed with a single elliptical-shaped nucleus, fine chromatin, and eosinophilic cytoplasm. No atypia or mitoses were observed. Histological findings confirmed the diagnosis of calcified angioleiomyoma. Five years after surgery, the patient had no recurrence of the mass.
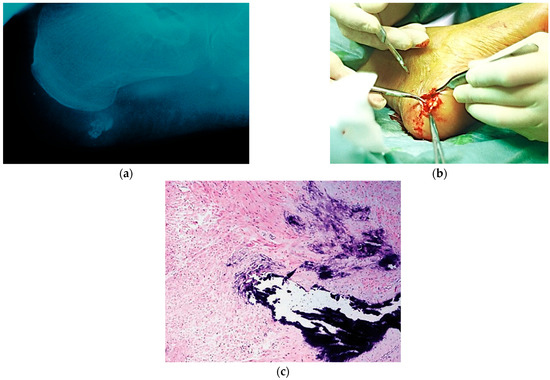
Figure 2.
Lateral X-ray highlighting a 15 mm radiopaque lesion adjacent to the calcaneal (a). Intraoperative images show a firm, white, and glistening mass (b). Histological image showing extensive calcifications. Non-calcified areas showed a fascicular proliferation of bland spindle cells without atypical features (H/E, 10×) (c).
3. Materials and Methods
The search strategy was carried out by the two authors (A.C.-F. and J.M.-G) with a data cutoff of 30 October 2024. The systematic search and data processing were performed in accordance with the “Preferred Reporting Items for Systematic Reviews and Meta-Analysis” (PRISMA) guidelines. The review was submitted to PROSPERO (registration number CRD420250654176) to prevent the duplication of content, minimize bias, and allow for review comparisons.
A Boolean search was performed in the PubMed, Scopus, EMBASE, Web of Science, and Google Scholar databases and carried out according to the following search strategy: (leiomyoma * OR “angioleiomyoma *” OR “solid angioleiomyoma * OR venous angioleiomyoma * OR cavernous angioleiomyoma) AND (foot). Studies were included based on the following eligibility criteria. The population comprised individuals of all ages with confirmed histological ALM of the foot. All histological subtypes of ALM located in the foot were included, while studies involving cases located in the ankle or other locations of the leg were excluded.
The following criteria were used for the initial selection: human clinical studies, retrospective studies, and case series (two or more cases) with no restrictions on follow-up after surgical removal. Studies prior to July 1984 (the first and largest published series of cases on ALM), case reports (one case), letters to the editor, and manuscripts published in a non-English language or without full access to the text were excluded.
Two independent reviewers (A.C.-F. and J.M.-G.) screened titles and abstracts for relevance. Potentially eligible full-text articles were recovered and evaluated against the inclusion criteria. The inter-rater reliability for full-text inclusion was estimated using Cohen’s kappa (κ = 0.92), indicating strong agreement. Data extraction was carried out using a standardized form in Microsoft Excel, gathering information on study design, publication year, and geographic location. Details about sample size and participant demographics, such as age and sex distribution, were recorded. Any discrepancies during data extraction were resolved through consensus or, when necessary, by consulting a third reviewer (C.D.-B.).
Each included article was independently assessed for methodological quality and risk of bias by an independent evaluator. The risk of bias of the included studies was assessed based on their characteristics. To determine the methodological quality of such studies, the Methodological Items Score for Nonrandomized Studies (MINORS) was used. This scale is a valid instrument designed to assess the methodological quality of non-randomized, comparative, or non-comparative surgical studies [9]. The eight items included in the scale are as follows:
- A clearly stated aim: The question addressed should be precise and relevant considering the available literature (D1).
- Inclusion of consecutive patients (D2).
- Prospective data collection (D3).
- Explanation of the criteria used to evaluate the main outcome. Endpoints must be assessed on an intention-to-date basis (D4).
- Blind evaluation of objective endpoints and double-blind evaluation of subjective endpoints (D5).
- The follow-up period is appropriate for the purpose of the study (one year minimum) (D6).
- Loss to follow-up is less than 5% (D7).
- Prospective calculation of study size (D8).
The eight items are scored as 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). The maximum score for non-comparative studies is 16. Each case series study analyzed was classified as having a low risk (10–16 points), moderate risk (6–9 points), or high risk (1–5 points) of bias based on the average domain rating.
The following information was extracted from the included studies: author(s) and year of publication, number of reported cases, sex, mean age of the patients, location, histological subtype, symptoms (pain or footwear problems), duration, size, presence of calcifications, procedure, follow-up, and recurrence. The foot was divided into 5 zones to analyze the data. The zones of the foot used were adapted as described by Kirby et al., excluding the ankle region [10]. These zones were numbered 1–5, corresponding to the heel (zone 1), the dorsum of the midfoot (zone 2), the plantar surface of the medial or lateral foot arch (zone 3), and the forefoot and toes (zones 4 and 5). The lines correspond to an oblique coronal plane, drawn from the midtarsal joint to the posterior margin of the longitudinal arch; a transverse plane, drawn from the midpoint of the first metatarsal base to the level of insertion of the Achilles tendon into the calcaneus; and two coronal planes, drawn through the first metatarsus–cuneiform joint and metatarso-phalangeal joint. Tumor lesions reported in the lower leg or ankle region were excluded from the analysis (Figure 3).
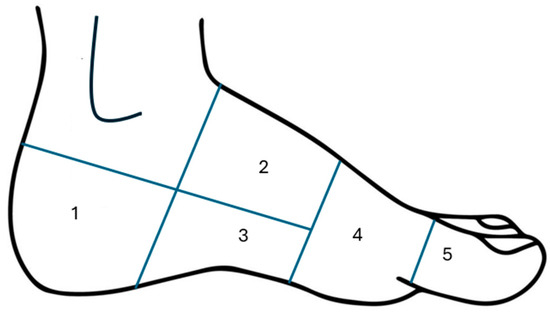
Figure 3.
The zones of the foot used to analyze the data.
The study data was recorded in a special database created using Excel software (Microsoft, Redmond, WA, USA) and classified according to the following characteristics: study design, population characteristics, number of patients, number of cases, location, clinical symptoms, histological subtypes, size, presence of calcifications, follow-up, and outcome.
4. Results
The electronic database search phase (PubMed/Medline, EMBASE, and Google Scholar) produced a total of 86 articles. A total of 67 scientific articles were excluded from the analysis and descriptive summary for the following reasons: out of date (10); one or two ALM case reports of tumors in other anatomical locations (31) or an unspecified foot location (17); research without reported cases (3); noncompliant languages (3); case reports of ALM in animals (2); and the manuscript could not be obtained or the information could not be collected (1). Finally, a total of 14 case series [2,4,6,7], refs. [11,12,13,14,15,16,17,18,19,20] were included in the analysis and descriptive summary (Figure 4).
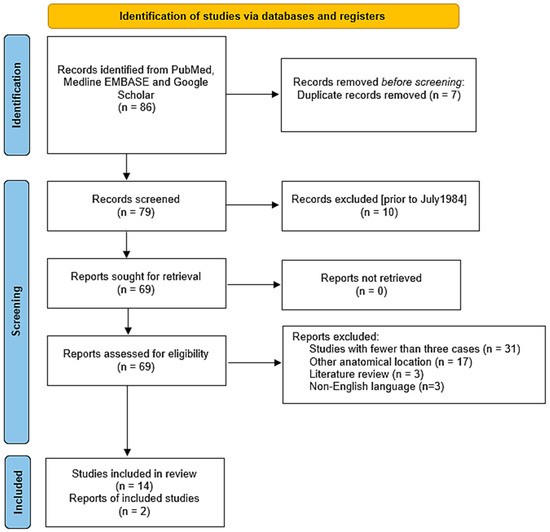
Figure 4.
Summary of the article selection according to PRISMA guidelines.
The results of the risk of bias analysis of the included studies according to the MINORS scale are presented in Table 1.

Table 1.
Quality assessment for non-randomized surgical studies using MINORS score criteria.
A total of 172 cases of foot ALM were described in the 14 included case series. The mean age of the patients was 56.1 ± 10.6 years, with a female to male ratio of 1:48 and 62.5% of the patients being women. The most affected anatomical area of the foot was predominantly the hindfoot (zone 1) in 40.5% of cases, especially the heel, followed by the forefoot (20.2%) and midfoot (8.9%), respectively. Most tumors presented as a single, painful lump with a mean diameter of 21.7 ± 9.0 mm and a mean duration until confirmed diagnosis and surgical excision of 6.1 ± 5.4 years. The mean maximum diameter of tumors in the hindfoot (zone 1) was very similar to that recorded in zones 4 and 5 (9.93 ± 7.15 mm vs. 10.36 ± 9.4 mm), without significant differences. Regarding the deep location of tumors, 69% were in the subcutaneous tissue, 16.5% had a subaponeurotic location, and only an additional 14.5% were cutaneous (Table 2).

Table 2.
Summary of variables from analyzed case series studies of ALMs on the foot.
Histological examination was performed on all excised tumors, and calcified presentations occurred in 7% of cases, with more than half of cases located in the hindfoot, especially on the heel (7 of 14 cases). Regarding histological subtypes, 65% of ALMs were solid tumors, 21% were venous, and 14% were cavernous or mixed subtypes. In all cases of ALM that underwent immunohistochemical analysis, the spindle cells were positive for α-smooth muscle actin.
Surgical excision was the treatment of choice for all patients, with a mean time to surgery of 6.6 ± 5.41 years from symptom onset. All patients underwent complete surgical excision. Three studies reported a symptom-free period ranging from 12 to 96 months after surgery, with a mean follow-up time of 38 ± 50.3 months. All cases were described as asymptomatic or pain-free at follow-up [6,15,18].
No cases of ALM recurrence localized to the foot were reported. These results are consistent with the cases reported here. In both cases, patients presented with a heel lump, and the time to surgery was two years and six months from the onset of symptoms, respectively. After almost two years (Case 1) and after more than five years (Case 2) of follow-up, neither patient experienced recurrence of the extirped tumors. Of the included studies, only three had appropriate follow-up cases (one year minimum) [6,15,18]. Most cases did not report information on or descriptions of postoperative symptoms. ALMs rarely recur after total surgical excision. Recurrence was observed in three patients (1.7%) [2,4].
5. Discussion
The epidemiology of acral and digital ALMs has been poorly described in the literature. Their low reported incidence could be because previous studies have produced limited data due to a lack of interdisciplinary approaches or restricted patient populations.
Usually, ALM has been reported in patients between the fourth and sixth decades of life. In the present review, the mean age of the patients was 56.1 ± 10.6 years, with a female-to-male ratio of 1:48 and 59.7% of the patients being women. Hachisuga et al., in the largest ALM reported series, observed that lower-extremity tumors occurred in women twice as frequently as in men [2]. This is consistent with the prevalence reported in a systematic review on ALM in the foot and ankle recently published by Matos et al., which included 78 patients, of whom 65.3% were women, with a female-to-male ratio of 1:88 [21]. Available evidence shows that benign soft-tissue tumors of the foot occur more frequently in women [10,11,12,13,14,15,16,17,18,19,20,21,22]. The exact cause of this female preponderance is unknown, but it is suggested that minor and repetitive trauma to the acral areas is more common in women as a result of wearing less physiological footwear, which could contribute to greater tumor development. This circumstance would explain why the prevalence of ALM is significantly higher in the hindfoot and forefoot than in the midfoot, which is less subject to mechanical stress.
In terms of anatomical location, as in the two cases reported here, the data from the present review show that the most affected anatomical area of the foot was the hindfoot (zone 1) in 40% of cases, especially the heel. These results contrast with those reported by Matos et al., which inform that the forefoot is the most frequently affected area, followed by the hindfoot [21]. Unlike the latter, our systematic review is based solely on case series with two or more cases of ALM in the foot, excluding the ankle. However, of the 62 reported cases included in the systematic review by Matos et al., 59 studies were reports with no more than one or two cases of ALMs in the foot and ankle. These differences may also be due, in part, to the fact that in the present review, the location of the lesions was not available in 34% of cases.
The differential diagnosis for ALM should include common benign soft-tissue tumors of the foot and ankle, including tenosynovial giant cell tumor, hemangioma, plantar fibromatosis, schwannoma, and lipoma [22,23]. ALM is typically present as a firm and solid slow-growing nodule that can be asymptomatic or responsible for pain and discomfort. Pain was the single most common complaint, followed by footwear problems, in patients with ALM on the foot. Most tumors presented as a single painful lesion, with pain being the main symptom in many ALMs on the sole, especially on the heel, as in the two cases reported here. The compression of small cutaneous nerve fibers within the ALM and ischemia caused by the reactive force of the ground in the support areas and compressive forces caused by footwear justify why, in our review, 63.1% of injuries presented as painful. However, the presentation of ALM is similar to that of many other acral tumors, and pain is not specific to this tumor. This review showed that there was a wide variation in the duration of symptoms, with a mean duration of 7.4 ± 5.5 years until confirmed diagnosis and surgical excision. The potential paucity of signs and symptoms in some cases of ALM justifies the delay in a correct and accurate diagnosis.
On the other hand, symptoms can also be conditioned not only by the location, but also by the size and time of the tumor evolution. Many ALMs presented as a slow-growing solitary nodule with an average maximum diameter of less than 20 mm [7,15,18].
The two cases of ALM reported herein were located in the subcutaneous tissue and were of the solid histological subtype. In the present review, 69% of the tumors were located in the subcutaneous tissue, 16.5% had a subaponeurotic location, and only an additional 14.5% were cutaneous. Regarding histological subtypes, 65% of ALMs were solid, 21% were venous, and 14% were of the cavernous or mixed subtype. These data are similar to those reported in other reviews of the literature [21].
Although MRI or US with color Doppler may be beneficial in some cases of ALM and may suggest a preliminary diagnosis, final confirmation by histopathological analysis is mandatory, and ALMs are rarely diagnosed before surgery. Typical sonographic features of ALM include a small hypoechoic mass with a superficial location, well-defined margins, complete solid components, and a low or moderate vascular density. Most cases show no blood flow signals, and only some show small or moderate blood flow signals on color Doppler flow imaging [13,24]. Although certain imaging signs on US may suggest a specific subtype, histological examination is still required for accurate classification and appropriate treatment. US examination did not show signals of internal blood flow on color Doppler sonography in any of the cases reported here.
Most surgeons find that conventional radiography is sufficient to proceed with surgical excision. As in one of our reported cases, radiography may be helpful in revealing the presence of calcifications in some ALMs. Calcifications are rare in ALM (1.9–3.3% of cases), with only 31 cases previously reported in the literature [7]. Calcification ranged from minor deposits to complete calcification, potentially leading to misdiagnosis. Calcification is often present in the three histological variants of ALM and is usually restricted to small foci, being more frequent in acral locations, which is probably related to repetitive minor trauma [6,7]. Of the 172 cases of ALM of the foot analyzed in this review, only 12 cases (7%) presented macroscopic calcifications, of which just over half were located in the heel. However, Matos et al. reported a very high percentage of calcified ALM (27.8%). We believe that this high incidence was due to the fact that 20 of the 31 cases of calcified ALM reported in the literature were included in the systematic review, which could have led to selection bias, with atypical or more striking cases being overrepresented [21]. The present review is based solely on case series with two or more cases of ALM in the foot, excluding the ankle. Of the 62 cases of ALM reported in the systematic review by Matos et al., 59 studies were reports with no more than one or two cases of ALM in the foot and ankle, and only six studies included in this review are coincident.
Histologically, ALM presents two-layered circumferentially arranged vascular channels, with bundles of mature smooth muscles oriented around blood vessels. The immunohistochemical examination of ALM showed positive SMA in all cases, while desmin was positive in a slightly lower proportion [4]. The histological findings in both cases reported here confirmed the diagnosis of ALM. In Case 2, actin was consistently present in the tumor and immunohistochemistry showed strong and diffuse immunostaining for SMA and desmin, highlighting its smooth muscle nature.
Although only 3 of the 14 series of cases included in this systematic review had adequate follow-up (minimum of one year), reported recurrence after surgical excision was very low (only three cases) [2,4]. Malignant progression to grade 1 angioleiomyosarcoma is extremely rare, with only three cases of malignant transformation of ALM in an extremity and no evidence of metastatic disease [25,26,27]. ALM of the foot, typically associated with significant pain, may result in a shorter time to surgery, reducing the risk of malignant transformation.
This systematic review has several limitations that should be acknowledged. First, the results of this systematic review are based on data from only fourteen case series. More than half of the studies were small case series, given the rarity of ALM of the foot. This limited sample size may have introduced publication bias. Second, although only two of the included case series were found to have a high risk of bias, their retrospective nature introduces potential biases that may have influenced the obtained results. Despite these limitations, the present review provides detailed information about the epidemiological and clinical aspects of ALMs specifically located on the foot. Moreover, it highlights the clinical and histological characteristics of these tumors to improve diagnostic accuracy and ensure appropriate management, assisting clinicians in improving patient outcomes.
6. Conclusions
This review provides complete and detailed information on the demographics and clinical aspects of ALMs specifically located in the foot and highlights the clinical and histological characteristics of these tumors. ALMs typically appear as well-defined painful nodules and particularly occur in the hindfoot of middle-aged women. They commonly arise in the subcutaneous tissue, and solid histological subtypes are highly prevalent. Smooth muscle actin was present in all cases included here. Histopathological analysis is generally essential for confirmation. Treatment primarily involves straightforward excision, with notablly low complication and recurrence rates. Despite the low recurrence rate reported in the literature, based on our cases and the cases reviewed in the literature, we recommend that clinicians treating patients with ALM perform annual follow-up for at least three years, supported using US.
Author Contributions
Conceptualization A.C.-F.; methodology, M.B.-M.; software, M.B.-M. and A.C.-M.; formal analysis A.C.-F. and J.M.-G.; resources, C.D.-B.; writing—original draft preparation, A.C.-F.; writing—review and editing, A.C.-F. and J.M.-G.; visualization C.D.-B. and V.E.C.-J.; supervision, A.C.-F.; data curation A.C.-F. and J.M.-G.; project administration A.C.-F.; supervision A.C.-F.; validation A.C.-F., J.M.-G., C.D.-B., V.E.C.-J. and A.C.-M.; Writing-original draft A.C.-F. and V.E.C.-J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The case report was conducted in accordance with the Declaration of Helsinki, and the Institutional Review Board of the Universidad de Sevilla determined that it meets the exemption criteria to be evaluated by an ethics committee because this is not required for the publication of two cases. In case reports, only the informed consent document signed by the patients is required.
Informed Consent Statement
Written informed consent was obtained from the two patients.
Data Availability Statement
All data generated during this study is included in this article. The data for this study were obtained using the EMR to obtain the details needed to complete two case reports.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ALM | Angioleiomyoma (singular or plural depending on context) |
| CARE | CAse REport (guidelines for case reports) |
| CC BY | Creative Commons Attribution |
| EMBASE | Excerpta Medica Database |
| H/E | Hematoxylin and Eosin (histological stain) |
| MINORS | Methodological Index for Nonrandomized Studies |
| MRI | Magnetic Resonance Imaging |
| N/A | Not Available |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| SMA | Smooth Muscle Actin |
| US | Ultrasound |
References
- Matos, M.; Soares, S.; Agaoua, M. Current Concepts of Foot and Ankle Angioleiomyoma. J. Foot Ankle Surg. 2023, 62, 746–749. [Google Scholar] [CrossRef]
- Hachisuga, T.; Hashimoto, H.; Enjoji, M. Angioleiomyoma. A Clinicopathologic Reappraisal of 562 Cases. Cancer 1984, 54, 126–130. [Google Scholar] [CrossRef]
- Morimoto, N. Angiomyoma (vascular leiomyoma).: A Clinicopathologic Study. Med. J. Kagoshima Univ. 1973, 24, 663–687. [Google Scholar]
- Bernard, M.; Le Nail, L.R.; de Pinieux, G.; Samargandi, R. Angioleiomyoma: An Update with a 142-Case Series. Life 2024, 14, 338. [Google Scholar] [CrossRef]
- Matsuyama, A.; Hisaoka, M.; Hashimoto, H. Angioleiomyoma: A clinicopathologic and immunohistochemical reappraisal with special reference to the correlation with myopericytoma. Hum. Pathol. 2007, 38, 645–651. [Google Scholar] [CrossRef]
- Maheshwari, A.V.; Temple, H.T.; Murocacho, C.A. Calcified angiomyomas of the foot: A case report. Foot Ankle Int. 2008, 29, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Peñaranda, J.M.; Pita da Veiga, G.; Pérez-Muñoz, N.; Fernández-Figueras, M.T. Acral Calcified Vascular Leiomyoma: Report of 3 Cases and Literature Review. Am. J. Dermatopathol. 2021, 43, 732–735. [Google Scholar] [CrossRef] [PubMed]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE Guidelines for Case Reports: Explanation and Elaboration Document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Kirby, E.J.; Shereff, M.J.; Lewis, M.M. Soft-tissue tumors and tumor-like lesions of the foot. An analysis of eighty-three cases. J. Bone Jt. Surg. Am. 1989, 71, 621–626. [Google Scholar] [CrossRef]
- Gupte, C.; Butt, S.H.; Tirabosco, R.; Saifuddin, A. Angioleiomyoma: Magnetic resonance imaging features in ten cases. Skelet. Radiol. 2008, 37, 1003–1009. [Google Scholar] [CrossRef]
- Hammond, M.I.; Miner, A.G.; Piliang, M.P. Acral and digital angioleiomyomata: 14-year experience at the Cleveland Clinic and review of the literature. J. Cutan. Pathol. 2017, 44, 342–345. [Google Scholar] [CrossRef]
- Zhang, J.Z.; Zhou, J.; Zhang, Z.C. Subcutaneous Angioleiomyoma: Clinical and Sonographic Features with Histopathologic Correlation. J. Ultrasound Med. 2016, 35, 1669–1673. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Sudo, Y.; Tsunoda, R.; Nanno, M.; Arai, S.; Takai, S. Association of Magnetic Resonance Imaging Features with Angioleiomyoma Histologic Subtype. J. Nippon. Med. Sch. 2021, 87, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Ipponi, E.; Bechini, E.; Ruinato, A.D.; Franco, S.; D’Arienzo, A.; Andreani, L. Angioleiomyoma of the Foot: Clinical and Functional Outcomes of Surgical Treatment in a Case Series. J. Am. Podiatr. Med. Assoc. 2024, 114, 23–25. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.H.; Izumi, M.; Nakatani, Y.; Ohara, K. Calcified angioleiomyoma—Histopathologic and ultrasonographic analysis of the calcification process. Dermatol. Sin. 2021, 39, 202–205. [Google Scholar] [CrossRef]
- Szolomayer, L.K.; Talusan, P.G.; Chan, W.F.; Lindskog, D.M. Leiomyoma of the Foot and Ankle: A Case Series. Foot Ankle Spec. 2017, 10, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Yates, B.J. Angioleiomyoma: Clinical presentation and surgical management. Foot Ankle Int. 2001, 22, 670–674. [Google Scholar] [CrossRef]
- Kacerovsca, D.; Michal, M.; Kreuzberg, B.; Mukensnabl, P.; Kazacov, D. Acral calcified vascular leiomyoma of the skin:A rare clinicopathological variant of cutaneous vascular leiomyoma. J. Am. Acad. Dermatol. 2008, 59, 1000–1004. [Google Scholar] [CrossRef]
- Bodapati, V.S.; Sunderamoorthy, D. Angioleiomyoma—Rare soft tissue tumor of the foot and ankle, review of two patients and review of the literature. J. Surg. Case Rep. 2021, 2021, rjab535. [Google Scholar] [CrossRef]
- Matos, M.J.; Soares, S.; Schwab, J.M.; Tannast, M.; Seidel, A. Foot and ankle angioleiomyoma: A systematic review. BMC Musculoskelet. Disord. 2025, 26, 246. [Google Scholar] [CrossRef]
- Scheele, C.; Toepfer, A.; Beischl, S.; Dammerer, D.; Harrasser, N.; von Eisenhart-Rothe, R.; Lenze, F. Insights into the Distribution Patterns of Foot and Ankle Tumours: Update on the Perspective of a University Tumour Institute. J. Clin. Med. 2024, 13, 350. [Google Scholar] [CrossRef]
- Córdoba-Fernández, A.; Sánchez-Robles, L.J.; Lobo-Martín, A. Tenosynovial Giant Cell Tumor in the Forefoot: Two Case Reports and Literature Review. J. Am. Podiatr. Med. Assoc. 2021, 111, 25. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Kim, S.S.; Lee, S.Y.; Choi, Y.J.; Chung, E.C.; Rho, M.H. Sonographic appearances of soft tissue angioleiomyomas: Differences from other circumscribed soft tissue hypervascular tumors. J. Ultrasound Med. 2012, 31, 1589–1595. [Google Scholar] [CrossRef]
- Ward, T.R.W.; Eastley, N.C.; Sheikh, N.; Ashford, R.U. Intralesional leiomyosarcoma malignant transformation from a biopsied benign angioleiomyoma of the proximal anterior tibia. BMJ Case Rep. 2024, 17, e259887. [Google Scholar] [CrossRef] [PubMed]
- Herren, D.B.; Zimmermann, A.; Büchler, U. Vascular leiomyoma in an index finger undergoing malignant transformation. J. Hand Surg. Br. 1995, 20, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Trojani, M.; Contesso, G.; Coindre, J.M.; Rouesse, J.; Bui, N.B.; de Mascarel, A.; Goussot, J.F.; David, M.; Bonichon, F.; Lagarde, C. Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system. Int. J. Cancer 1984, 33, 37–42. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).


