1. Introduction
Obesity is a multifactorial disease and a significant public health issue as it is closely linked to higher mortality rates and numerous comorbidities [
1,
2]. Bariatric surgery has emerged as the most effective treatment for severe obesity and is known for its ability to reduce weight and associated diseases [
3]. Surgical management has the highest evidence-based approach to achieve sustained weight loss and improve associated medical conditions. However, it is important to note that bariatric surgery-induced weight loss can also lead to a significant decrease in skeletal muscle mass, eventually increasing the risk of sarcopenia [
4].
Sarcopenia is a clinical condition characterized by a significant loss of muscle mass and strength that is generally studied in elderly patients [
5,
6]. However, it also appears to be present in patients with obesity, conditioned not by age but by metabolic, physical, and lifestyle changes [
7]. Muscle tissue plays a critical role in overall health, and its loss is linked to various adverse outcomes. Recognizing the importance of sarcopenia, several international study groups have recently published consensus statements on its definition and diagnosis [
8].
As suggested in the European Working Group on Sarcopenia in Older People (EWGSOP2), sarcopenia is a muscle disease that may occur at any age. Sarcopenia is common in older age but may also occur earlier in life [
6]. The group identified the need to update its initial definition, and the new EWGSOP2 consensus focuses on low muscle strength as a key for diagnosing sarcopenia, as well as muscle quantity and quality to confirm the diagnosis [
6]. The EWGSOP2 introduces a novel algorithm for identifying sarcopenia. Unlike the traditional method, which relies on a diminished skeletal muscle mass (SMM) alongside a decreased walking speed or muscle strength decline, this algorithm adopts the Find-Assess-Confirm-Severity (F-A-C-S) approach. Muscle strength is evaluated after screening yields positive results or clinical suspicion arises. If muscle weakness is detected, sarcopenia is suspected, and muscle mass is addressed. SMM, appendicular skeletal muscle mass (ASMM), and index (ASMMI) are assessed, and any observed decrease confirms the presence of sarcopenia. Furthermore, severe sarcopenia is identified by decreased physical performance, such as gait speed [
6,
9].
In this context, sarcopenia may have a complex relationship with obesity. Despite the importance of understanding the consequences of substantial weight loss after bariatric surgery and the development of sarcopenia, there is limited documentation and research on this topic. Existing studies also present varying results, emphasizing the need for further investigation.
To answer these limitations, the European Association for the Study of Obesity (EASO) and the European Society for Clinical Nutrition and Metabolism (ESPEN) developed a consensus for evaluating sarcopenia in obese patients [
6]. This document is like the EWGSOP2 but also introduces obesity diagnosis tools, like weight, BMI, and waist circumference.
Sarcopenic obesity is a complex clinical condition that presents a unique challenge due to the combination of obesity and sarcopenia. As a result, individuals with sarcopenic obesity face a higher risk for metabolic diseases, functional impairment, and other adverse clinical outcomes compared to those with either condition alone [
7,
10]. However, if eating disorders and excess fat mass can have negative consequences on muscle mass and its function, patients with obesity may need to develop additional muscle mass to carry out their daily activities, such as simply walking [
11], further complicating the interpretation of the post-surgical data.
Moreover, screening and diagnostic procedures for sarcopenic obesity need to be practical, affordable, and time-efficient, with a focus on assessing altered skeletal muscle functional parameters and body composition. The staging of sarcopenic obesity based on the presence of complications related to altered body composition and muscle function may be essential for guiding treatment and follow-up [
7,
8,
11].
Studies evaluating sarcopenia after bariatric surgery are limited and consider mainly compromised muscle mass. Moreover, the role of the EASO/ESPEN and EWGSOP2 criteria and cut-offs in this setting was not previously studied.
In this study, we prospectively evaluated the impact of bariatric surgery on sarcopenia-related parameters over an 18-month period after surgery in patients undergoing the procedure. Specifically, the study aims to assess changes in muscle strength, muscle mass, and the prevalence of sarcopenic obesity at various time points before and after surgery. We hypothesize that while bariatric surgery will result in significant weight loss, it will also lead to a concomitant reduction in muscle mass and strength, thereby increasing the risk of sarcopenia shortly after surgery as has been defined by both recommendations. Additionally, we aim to determine whether these changes persist or diminish over the follow-up period. The significance of this study lies in its potential to inform clinical practice and improve the management of patients undergoing bariatric surgery, possibly influencing guidelines and recommendations for post-bariatric surgery monitoring and rehabilitation programs.
2. Methods
2.1. Study Design
This prospective study of patients undergoing bariatric surgery was conducted at a single surgical center, the Center for Integrated Responsibility for Bariatric Surgery and Metabolic Diseases (CRI.COM) at a Portuguese Hospital (ULSAC). The entire protocol has been previously described [
12].
The invitation to participate was made in the context of an outpatient appointment, and participants who agreed to participate in the study were delivered the free and informed consent form previously approved by the University and Hospital Ethics Committee (HESE_CE_1917/21).
As inclusion criteria, patients should be enrolled for bariatric surgery at the hospital, both men and women, aged between 18 and 65, with a body mass index (BMI) of more than 35 kg/m2, with medical-associated morbidities, who agree to participate in the study. Patients with previous bariatric surgery were excluded. Participants were recruited during outpatient appointments, where the study was explained, and they were invited to participate. Screening included a detailed medical history and physical examination to ensure eligibility. All patients underwent bariatric and metabolic surgery between December 2021 and December 2022.
During the study period, all patients were followed using standard follow-up by bariatric surgeons, nutritionists, psychologists, and nurses.
2.2. Peri-Operative Management
The multidisciplinary group evaluated and performed the surgery in all patients according to a standard protocol. The surgical procedure was a Roux-en-Y gastric bypass (RYGB). After surgery, the participants received similar support from the different team specialists from the team, with standard follow-up appointments and consultations.
2.3. Outcomes Definition and Data Collection
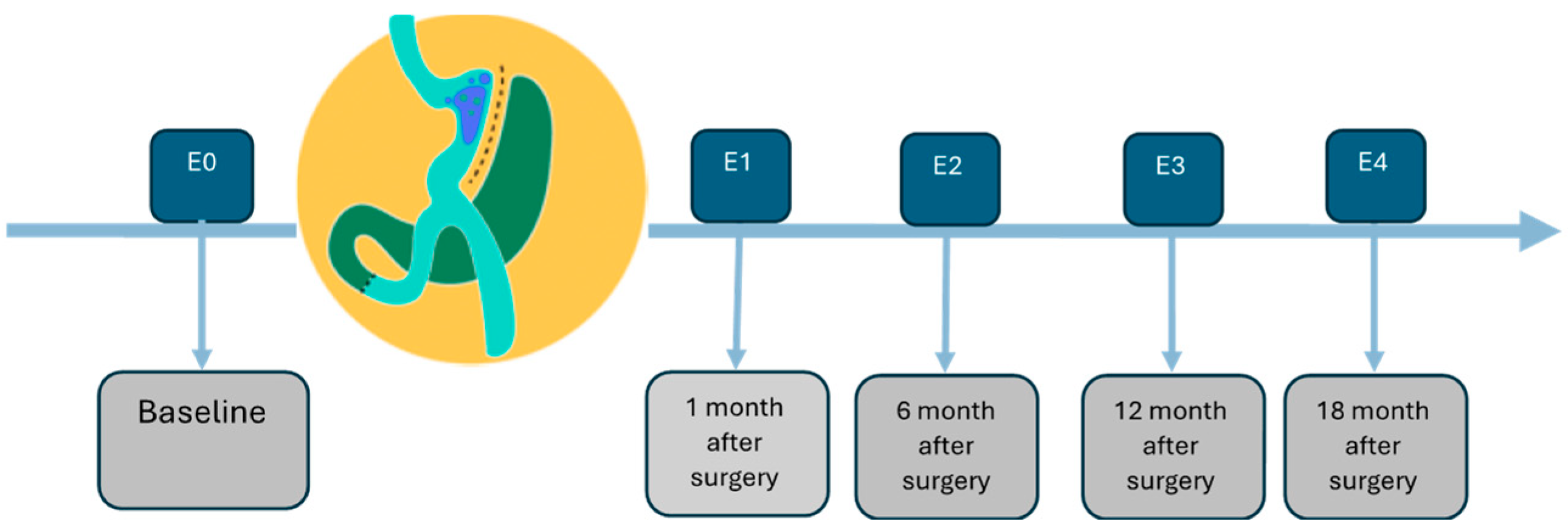
According to the study plan, all parameters were evaluated at the five time points— before surgery and at 1, 6, 12, and 18 months after surgery (
Figure 1).
Weight evaluation was measured using a scale. The patients were without shoes or heavy clothing. Height was determined by a manual stadiometer. BMI was calculated (weight/height
2), and the abdominal circumference was determined by a measuring tape [
13,
14]. To evaluate body composition, the dual-energy X-ray absorptiometry—DEXA (DXA, Hologic QDR, Hologic, Inc., Bedford, MA, USA) was used [
15].
For screening, both the EWGSOP2 and the ESPEN/EASO consensuses recommend the use of the SARC-F questionnaire (FIND) in clinical practice [
6,
9].
The SARC-F is a self-reported questionnaire with five questions: Strength (S), Assistance walking (A), Rising from a chair (R), Climbing stairs (C), and Falls (F). Each answer is rated on a scale of 0 to 2, ranging from “not at all” to “very difficult”. A total score is calculated out of 10. The recommended cut-off value for positive screening for sarcopenia is ≥4 points [
16,
17,
18].
All participants completed the SARC-F scale at each of the five time points.
In both consensuses, the first diagnostic criterion (ASSESS) for sarcopenia is low muscle strength. In our study, muscle strength was determined by the handgrip strength test and the five-times-to-stand test.
The handgrip strength test was conducted using manual pressure dynamometry for measuring grip strength (Jamar
®) to evaluate the muscle strength of the upper limbs. Participants were instructed to stand with their elbows fully relaxed and straight. Each hand was tested twice, and the maximum grip strength value obtained was recorded as the muscle strength test value [
19,
20]. The dynamometer was calibrated before each testing session to ensure accuracy, and all tests were administered by trained personnel to minimize inter-rater variability.
The sit-to-stand test evaluated the muscle strength of the lower limbs, in which participants were instructed to stand and sit for 30 s as many times as possible. The timed chair stand test is a variation that counts how many times a patient can rise and sit on the chair over a 30 s interval [
21,
22]. Because the chair stand test evaluates both strength and endurance, it offers a reliable yet practical measure of strength, and this is the test used in this investigation.
The cut-off used for handgrip strength was set at <27 kg for males and <16 kg for females [
23], and >15 s for five rises on the chair rise test (5 times sit-to-stand) [
22].
Confirmation of sarcopenia (
CONFIRM) based on muscle quantity or mass can be reported by appendicular skeletal muscle mass (ASMM) using dual-energy X-ray absorptiometry—DEXA. DEXA has been chosen because it is a common method for measuring skeletal muscle mass [
9]. SMM refers to the amount of muscle attached to the skeleton and helps in systemic movement and posture maintenance, whereas ASMM is the sum of the muscle mass of the four limbs [
24].
To estimate ASMMI, the sum of the muscle mass of the upper and lower extremities (muscle mass of arms [kg] + muscle mass of legs [kg]) was divided by height squared (m
2) (ASMMI = ASMM/height
2) [
25]. The ASMMI value has been used to assess sarcopenia in different populations, but there is still an ongoing debate about the preferred parameter to represent muscle mass [
6]. As suggested by the ESPEN/EASO consensus, in this study, we also considered the values of ASMM/weight for male (cut-off < 28.27%) and female patients (cut-off <23.47%) [
7].
The severity (SEVERITY) of sarcopenia was evaluated using the 400 m walk test to assess walking ability and endurance, and the staging level by the presence of at least one complication attributable to sarcopenic obesity. Participants were asked to complete 20 laps of 20 m each as fast as possible and were allowed up to two rest stops during the test [
26,
27]. Physical performance was considered low when the test was incomplete or took more than 6 min to complete C6].
2.4. Algorithm to Diagnose Sarcopenia and Sarcopenic Obesity—F-A-C-S
According to the EWGSOP2, sarcopenia diagnosis is based on low muscle strength combined with decreased muscle mass (male grip strength < 27 kg, ASMM < 20 kg, ASMMI < 7.0 kg/m
2; female grip strength < 16 kg, ASMM < 15 kg, ASMMI < 5.7 kg/m
2,) [
6]. Sarcopenia is considered severe when low physical performance is identified (400 m walk test ≥ 6 min) [
6]. For sarcopenic obesity (ESPEN/EASO) all previous cut-off values were considered, adding the ESPEN/EASO consensus parameters: BMI (BMI > 30 kg/m
2), waist circumference (WC) (WC ≥ 102 cm for male and ≥ 88 cm for female patients), and ASMM/weight (ASMM/weight < 28.27% for male and < 23.47% for female patients) [
7].
2.5. Statistical Methods
Statistical analysis was performed with the SPSS version 27.0 (IBM SPSS Inc., Chicago, IL, USA) to determine the parameters and outcomes. Categorical variables are expressed as frequencies and percentages, and continuous variables are expressed as mean and standard deviation. Data normality was assessed using the Shapiro–Wilk test. Repeated measures ANOVA was used to evaluate changes over time within the same group, with post hoc tests conducted using Bonferroni correction to adjust for multiple comparisons.
For categorical variables, chi-square tests were used to compare proportions between groups, with Fisher’s exact test applied when expected frequencies were low. Statistically significant results were considered for p-values ≤ 0.05.
3. Results
3.1. Weight
A total of 17 participants (88.2% female) were enrolled in this study with a mean age of 46.9 (± 11.4) years, a mean BMI of 42.9 (± 5.14) kg/m
2, a mean weight of 105.9 (± 17.5) kg, and a mean waist circumference of 123 (± 12) cm (
Table 1).
After surgery and throughout the study period, the mean weight decreased and was always significantly lower than the baseline, namely 91.8 kg at 1 month post-surgery (p < 0.001), 75.4 kg at 6 months (p < 0.001), 69.9 kg at 12 months (p < 0.001), and 70.8 kg at 18 months (p < 0.001). The comparison between the weight observed at each assessment point and the preoperative weight (baseline) was always statistically significant.
When the assessments were compared sequentially, the differences between the baseline weight and the weight at 1 month, the weight at 1 month and the weight at 6 months, and the difference between 6 and 12 months all showed a decrease with statistical significance (
p < 0.001). On the other hand, between 12 months and 18 months, weight remained practically stable, with no statistically significant difference (
Table 2). BMI and waist circumference assessments showed similar evolutions.
3.2. Screening
The application of the SARC-F questionnaire before and after surgery showed an increase in the SARC-F result between the preoperative and postoperative assessments. This increase may reflect an increase in the risk of developing sarcopenia during the peri-operative period and may be a result of the surgical intervention.
Applying the EWGSOP2 sarcopenia screening criteria (SARC-F), 70.6% of patients had a positive screening at the preoperative assessment. During the postoperative period, the number of positive screenings was 88.2%, 70.6%, 58.8% and 0% at 1 month, 6, 12, and 18 months, respectively. Only the result at 18 months showed a statistically significant difference compared to the baseline (
Table 3).
Using the ESPEN/EASO screening criteria for sarcopenic obesity (also assessed using BMI, waist circumference, and the SARC-F questionnaire), the result was positive at the preoperative assessment in 70.6% of patients. This percentage was 88.2% in the first month after surgery, but the difference was not statistically significant. After the first month, the screening was considered positive in a decreasing percentage of patients (35.3% at 6 and 12 months, and 0% at 18 months), and these differences were considered significant (
Table 4).
3.3. Muscle Strength
The handgrip assessments at 1 month, 6 months, 12 months, and 18 months were 18.1 kg, 16.8 kg, 17.7 kg, and 17.3 kg, respectively. All these results were lower than the handgrip assessed before surgery (20.4 kg), showing a statistically significant difference. When comparing handgrip strength between consecutive assessment points, there was a reduction between the baseline value and the first postoperative month (20.4 kg versus 17.8 kg) with a statistically significant difference. Subsequent comparisons—between 1 month and 6 months (17.8 kg versus 16.8 kg), between 6 months and 12 months (16.8 kg versus 17.7 kg), and between 12 months and 18 months (17.7 kg versus 17.3 kg)—showed only slight variations without statistical significance.
The sit-to-stand test at 1 month, 6 months, 12 months, and 18 months showed results of 12.8 n, 13.2 n, 13.1 n, and 12.8 n, respectively. None of these evaluations showed a statistically significant difference when compared to the preoperative (baseline) value of 12.6.
The cut-offs to classify the results of the handgrip strength as normal or abnormal are the same in both the EWGSOP2 and the ESPEN/EASO consensus. When we applied these criteria for the handgrip test evolution before and after surgery, 35.3% of the patients already met the criterion for compromised muscle strength before surgery. At 1 month post-surgery, 70.6% met the criterion, and at 6 months 64.7%. These differences from the baseline were statistically significant. At 12 and 18 months, 52.9% of patients were positive, and these differences from the baseline were not significant.
3.4. Muscle Mass
The ASMM parameter showed decreasing postoperative results: 19.72 kg, 17.53 kg, 15.90 kg, and 14.40 kg, respectively. When compared with the preoperative baseline result (21.92 kg), the difference was always statistically significant (p < 0.001). The sequential comparison between the assessment time points throughout the postoperative period—between 1 month and 6 months (19.73 kg versus 17.53 kg), between 6 and 12 months (17.53 kg versus 15.90 kg), and between 12 and 18 months (15.90 kg versus 14.40 kg)—always showed a statistically significant decrease.
The ASMMI (kg/m2) also showed a constant decrease from the baseline result (8.79) to 7.91, 7.03, 6.39, and 5.79 at 1, 6, 12 and 18 months after surgery, respectively. All differences were statistically significant (p < 0.001).
ASSM/weight (kg/kg) increased significantly between the preoperative assessment (20.6%) and the assessments carried out at 1 month (p = 0.039) and 6 months (p < 0.001) after surgery (21.4% and 23.3%). On the other hand, the assessments carried out at 12 and 18 months (21.1% and 20.5%) showed no significant difference when compared to the baseline assessment. In terms of progress, there was a significant difference between the preoperative assessment and the first month (20.6% versus 21.4%) and between the first and sixth month (21.4% versus 23.3%). Between 6 and 12 months there was also a significant difference, but in the opposite direction (23.3 kg/kg versus 21.1%). There was no difference between 12 and 18 months (21.1% versus 20.5%).
Applying the EWGSOP2 suggested cut-off for ASSMI (kg/m2), all patients had a normal index at baseline and one month after surgery. After that evaluation, 11.8%, 29.4%, and 52.9% of patients had an abnormal index at 6, 12, and 18 months, respectively, and this difference was statistically significant.
When the ESPEN/EASO recommended cut-off for ASMM/weight (kg/kg) was applied at the different evaluations, we found out that 94.1% of patients already had an abnormal result at baseline. This number was 88.2%, 70.6%, 88.2%, and 94.1% at 1, 6, 12, and 18 months, respectively.
3.5. Severity
The results of the 400 m walk test showed an increase in test time in all assessments 8.79 min, 8.74 min, 9.58 min, and 10.1 min at 1 month, 6 months, 12 months, and 18 months, respectively, when compared to the baseline value (7.61 min).
Over time, there was a significant increase (p = 0.016) in the test value between the preoperative assessment and the first month (7.61 min versus 8.79 min) and stability between 1 and 6 months (8.79 min versus 8.74 min). Again, there was a significant difference between 6 and 12 months (p = 0.019) (8.74 min versus 9.58 min) and a stable value between 12 and 18 months (9.58 min versus 10.1 min).
3.6. Sarcopenia Diagnosis
Applying the two cumulative EWGSOP2 criteria for diagnosing sarcopenia (criteria 1: reduced strength assessed by handgrip test and criteria 2: reduced muscle mass measured by decreased ASMM/height2) and its proposed cut-offs, it was found that at baseline 35% of the patients had probable sarcopenia, but no patients met both criteria for achieving a diagnosis. At one month after surgery the result was the same. Beyond that moment, 11.8%, 29.4%, and 52.9% of the patients met both criteria to obtain a diagnosis of sarcopenia.
When we applied the two ESPEN/EASO cut-offs for diagnosing sarcopenia associated with obesity, both muscle function (handgrip) and body composition (ASSM/weight), a cumulative result showed that of 35.3% of patients had sarcopenia at baseline. After surgery, the patients that met the same criteria for sarcopenia was 70.6%, 41.2%, 52.9%, and 52.9% at 1 month, 6, 12, and 18 months, respectively. This increase, when compared to the baseline, was statistically significant only up to 6 months (p < 0.05).
4. Discussion
This study provides valuable insights into the impact of bariatric surgery on sarcopenia and sarcopenic obesity over an 18-month period, utilizing EWGSOP2 and ESPEN/EASO consensus criteria. The findings indicate significant weight loss post-surgery, accompanied by reductions in muscle mass and strength, particularly evident in the early postoperative period. Notably, handgrip strength declined significantly one month after surgery, while other muscle function tests, such as the sit-to-stand test, did not show significant deterioration. The prevalence of sarcopenic obesity increased immediately post-surgery, peaking at one month and returning to pre-surgery levels by six months.
Bariatric surgery is currently the most effective type of treatment for moderate and severe obesity. On the other hand, the weight loss caused by bariatric surgery represents not only fat mass loss, but is often accompanied by muscle mass loss. Addressing this subject is not an easy task due to the different muscle function and body composition study methods, as well as the absence of a clear consensus on the preferred tools and cut-offs to be used to establish a diagnosis of sarcopenic obesity. Also, different surgical procedures and other variables may impact on muscle mass and function differently.
In this study, we used the assessment tools recommended by both the EWGSOP2 group and the EASO/ESPEN consensus, including muscle function and mass assessments, with a focus on the handgrip test as a surrogate for muscle function and ASMM, ASMM/weight, ASMMI and ASMM/height2 to represent muscle mass. This data allowed us to evaluate the patients according to the algorithms proposed by both consensuses. The decision to perform multiple assessments, before and after surgery, was made to better elucidate this complex relationship between weight, adiposity, muscle mass, and muscle function after bariatric surgery.
Considering the specific bariatric surgery results on weight management, there was, as expected, a reduction in the patient’s median weight, BMI, and waist circumference up to the first year of follow-up, with no relevant change at 18 months. Besides reducing weight and adiposity, the eventual loss of muscle mass and muscle function is a concern in bariatric surgery. This effect may be an undesired side-effect of surgery.
4.1. Screening
Using the cut-offs for positive results, screening for sarcopenic obesity was already positive in most patients before surgery. When the EWGSOP2 criteria were used, the number of patients at risk for this condition decreased only 18 months after surgery, but when the ESPEN/EASO criteria was applied, the decrease was already present 6 months after surgery. This result shows that patients who are candidates for bariatric surgery already have a significant risk for sarcopenic obesity before surgery, and that bariatric surgery may take some time to decrease that risk as evaluated by the screening tool.
4.2. Muscle Strength
Muscle strength, one of the key aspects of sarcopenia, was assessed by different tests, but with a special focus on handgrip strength. This test is recommended both by the EWGSOP2 [
6] and the ESPEN/EASO consensus [
7]. Previously, the FNIH recommendations also stated that grip strength was the preferred method to assess muscle strength (using a cut-off of 26 kg for males and 16 kg for females) [
24].
The sit-to-stand test did not show identical results. There was no difference when the results before or after surgery were compared, or even during follow-up. It is interesting to note that the test in which muscle strength is analyzed without interference from the patient’s weight, the handgrip test, was the one that showed a clear and significant change, while the test that is dependent on weight did not. It can be argued that, in the specific context of patients with obesity who have undergone surgery and whose weight has decreased significantly between each two assessments, this reduction in weight could have interfered with the results of the 5 times sit-to-stand test, since decreasing body weight also decreases the muscular effort assessed in this test. On the other hand, weight loss is not expected to interfere with the handgrip muscle strength test, so the best test to show sarcopenia in this context is the handgrip.
The impact of bariatric surgery on the handgrip test has been debated. A recent meta-analysis by Jung et al. [
28] concerning muscle strength after bariatric surgery could not show muscle strength loss when all the data was pooled. Nevertheless, the aggregated number of subjects was not very large (n = 301), and the authors stated that their analysis had several limitations, namely that the studies were heterogeneous and represented only specific populations. Also, the timing of the assessments after surgery was heterogeneous, with most studies being performed only 6 months after the surgical procedure. In none of those studies, strength was assessed one month after surgery as in this study. Other variables that are probably relevant are gender and the surgical procedure chosen for each patient, as these factors may also impact weight and muscle loss.
Nevertheless, even if the global pooled data did not indicate that, some of the studies included in the meta-analysis showed a clear absolute decrease in muscle strength. Alba et al. showed a significant decrease from preoperative values (
p = 0.001). The mean 12-month change in absolute strength showed a decline of 2.6 kg, all of which occurred in the first six postoperative months [
29]. Oppert et al. also showed a 21 kg muscle strength decrease [
30], and Cole et al. showed a 2.8 kg decline [
31]. It is worth mentioning that these three studies were the only ones included in the meta-analysis where the only surgical procedure used was the RYGB.
Stegen et al., in 2010, already showed a 7% or 18% reduction in handgrip strength in RYGP patients [
32]. Another study, not included in the meta-analysis, by Crispim Carvalho et al., where the great majority of patients were RYGP patients (16/21), also showed a significant decrease in handgrip strength at one-year follow-up [
33]. Another study published in 2019 also showed a reduction from 34.18 kg to 31.91 kg in handgrip strength 6 months after surgery [
34], even though it is unclear what surgical procedure was performed.
In this study, contrary to the overall result of the meta-analysis, the handgrip test did show a clear decrease in strength as early as one month after surgery, with no further changes or deterioration afterward and up to eighteen months.
If we look closely at the data of the meta-analysis by Jung et al. [
28], only three papers, like this study, included exclusively RYGP patients. These three papers [
29,
31,
35,
36] all showed the same result—a decrease in handgrip strength—that was also found in other papers [
32,
33,
34] considering RYGP patients, showing the same results as ours.
Gender also seems to be a factor in muscle strength loss. Jung et al. performed a sub-group analysis of the pooled data in their meta-analysis based on the percentage of men below or above 30%. They concluded that in the studies with over 70% of women, handgrip strength was reduced by 1.5 kg. This is in accordance with the current results, where 80% of the patients were women, and a reduction in muscle strength was found [
33].
The results show that the decline in muscle function in RYGP patients after surgery is clear. It also appears very early in the postoperative period, at the one-month evaluation. It can be speculated that the first assessments performed in other studies, after 6 months, may not capture this early effect.
The relationship between post-bariatric surgery status and the strength assessed by the handgrip test is not yet clear. The differences in results of several studies may be due to differences in patient selection and methodology. Attention must be given to the type of surgical procedure, gender, and the time elicited after surgery.
4.3. Muscle Mass
Muscle mass loss is one of the critical components of sarcopenia and of sarcopenic obesity. Bariatric surgery causes significant weight loss. This is mainly due to fat mass loss, but muscle mass loss is also present. In this setting, muscle mass loss can be present before surgery and be caused or aggravated by surgery, resulting in a new onset sarcopenic obesity or worsening of a previous condition.
Nujten et al. performed a meta-analysis studying lean body mass, skeletal muscle mass, and fat-free mass losses after bariatric surgery. They concluded that there is a clear loss of muscle mass—8.13 kg LBM—one year after surgery [
37]. They also studied the impact of different procedures and found that the gastric band had a lesser impact, but the other procedures (RYGP, Sleeve, BPD) all had similar outcomes.
Jung et al. performed a systematic review and meta-analysis of muscle strength and muscle mass after bariatric surgery. They found a decrease in lean mass in all studies except two. The pooled data showed a reduction of 7.4 kg in this parameter. Rodrigues studied skeletal muscle mass in three groups of bariatric patients, divided according to BMI levels. In all groups, there was a loss of SMM of between 5.8 and 6.8 kg one year after surgery [
38].
There is debate about which parameter should be used to define sarcopenic obesity. In this study, ASMM, ASMMI, and ASMM/weight over 18 months were studied. These parameters were chosen because they are recommended by the EWGSOP2 consensus [
6] or by the ESPEN/EASO consensus [
7]. Another option would have been to assess ALM/BMI, previously proposed by the FNIH Sarcopenia Project [
24].
In the current study, the loss of muscle mass was somewhat more profound than in other investigations. This decrease was in line with the decrease in total body weight. Nevertheless, ASMM/weight, a parameter less dependent on weight and recommended by ESPEN/EASO guidelines as a representation of muscle mass in bariatric patients, did not show any decrease.
Other authors found similar results. Alba et al. observed a decline of 14% in lean mass and of 16% on ALM 12 months after surgery [
29]. Pekar et al. [
15] found a decrease in ALMI from 9.7 to 7.7 kg/m
2 18 months after surgery.
Vassilev et al. found a decrease in lean body mass from 63.38 to 58.87 kg 24 weeks after surgery. With MRI, those authors observed a decrease in skeletal muscle index from 52.65 to 42.48 cm
2/m
2 within the same time span [
39]. Using BIA, Martinez el al. found a decrease in fat-free mass from 66.47 kg to 55.48 kg 24 months after surgery [
11].
4.4. Severity
The test used to determine severity, the 400 m walk test, showed contradictory results in patients of this study. However, we must remember that this context corresponds to bariatric surgery patients. In this treatment, there is a significant weight loss between the time of the preoperative assessment and the time of the postoperative assessment. This marked weight loss achieved with bariatric surgery could compromise the reliability of the 400 m walk test physical performance test since performance in this test depends not only on the quantity and quality of skeletal muscle, but also on the physical effort required for walking. This effort in these patients after surgery may be facilitated due to the weight loss achieved.
4.5. Sarcopenia Diagnosis
The consensus criteria from EWGSOP2 and ESPEN/EASO aim to define sarcopenia and sarcopenic obesity [
7]. They advance a set of tests that can be chosen to determine the presence of this condition and suggest cut-offs to obtain a clear diagnosis. This is essential for facilitating research on the predisposing factors, consequences, prevention, and treatment of this condition.
However, few studies have been published to date that report the use of both these consensus criteria, as in this research, where handgrip strength was used to assess muscle function, and ASMM, ASMMI, and ASMM/weight were used to assess body composition. The cut-offs chosen were 27 kg for males and 16 kg for females for handgrip strength; <7.0 kg/m2 for males and <5.7 kg/m2 for females for ASMMI; and 28.27% for males, and 23.47% for females for ASMM/weight.
According to these results, one-third of the patients already presented sarcopenic obesity before surgery when the complete ESPEN/EASO criteria was used, but the result was 0% when the EWGSOP2 criteria was applied.
After surgery, there were clear differences in the results of the function and muscle mass tests over time. However, when applying the cut-offs for the diagnosis pathway only one month after surgery, there was also a clear difference in diagnosis when using the different consensuses. In fact, using EWGSOP2, the percentage of patients that met diagnostic criteria increased from 6 months onwards, affecting half the patients 18 months after surgery. However, when the ESPEN/EASO criteria were used, the percentage of patients classified as sarcopenic obesity increased one month after surgery (from 35.3% to 70.6%) whith one-third of the patients developing new-onset OS. Afterwards, from 6 to 18 months, this percentage was not different from baseline.
Future research should focus on larger, multicenter studies to confirm these findings and examine the long-term effects of bariatric surgery on sarcopenia and sarcopenic obesity. Investigating the efficacy of targeted interventions, such as resistance training programs and nutritional support [
40], or plant-derived natural products [
41], in preventing muscle loss post-surgery is also essential. Moreover, studies exploring the underlying mechanisms of muscle loss and recovery in bariatric patients will help develop more effective strategies for maintaining muscle health. Understanding the role of different bariatric procedures and patient characteristics in influencing these outcomes will further refine postoperative care protocols.
5. Conclusions
A short-term consequence of obesity surgery, specifically in the postoperative period, may be an increase in sarcopenia. This is shown by a clear decrease in muscle function when assessed by the handgrip test. On the other hand, this effect does not appear in tests whose performance is influenced by the patient’s weight: the 5 times sit-to-stand and the 400 m walk tests results did not suffer any deterioration. One possible interpretation is that, in these tests, the effects of the reduction in muscle mass and strength are masked by the reduction in the degree of physical demand of these three tests caused by the reduction in body weight after surgery.
Also, muscle quantity, as measured by ASMM or ASMMI, decreased continuously after surgery. However, when ASMM is adjusted by weight or BMI, the results are equivocal. This could probably be a result of a lack of clear understanding of the relative influence of surgery and weight loss itself on muscle mass.
When both muscle strength and muscle mass criteria and cut-offs are used in a cumulative way, and according to both consensuses, antagonistic results were observed. This may be a consequence of the present lack of a clear-cut definition of sarcopenia, despite the different studies, reviews and other papers that have been published on this subject. Nevertheless, the present results seem to indicate a significant deleterious impact of bariatric surgery on muscle strength and mass, the most important indicators of sarcopenia. This is very clear in the handgrip test, ASMM, and ASSMI. Considering the relevance of muscle strength and muscle mass for health and well-being, it could be considered that these indicators should be preferred for sarcopenic obesity diagnosis. Also, the impact seems to occur very early after surgery, which may indicate that the appropriate timeframe to try to prevent this effect may be the prehabilitation period followed by the post-surgery timeframe.
Limitations
One limitation of this study is its small sample size of 17 patients, which may affect the generalizability and statistical power of the findings. The limited sample size might have restricted our ability to detect smaller yet clinically significant differences. Additionally, most participants were female, which may not fully represent the broader bariatric surgery population. The absence of a non-surgical group may limit the conclusions. However, we believe that a control group with non-surgical patients with the same level of weight loss that bariatric surgery provides would be impossible to recruit, considering the low efficacy of non-surgical approaches. Only bypass patients were recruited to limit the variability of results. Future studies with larger, more diverse samples are needed to validate these findings and explore potential gender differences in the impact of bariatric surgery on muscle mass and strength. Despite these limitations, our study provides important preliminary insights into the changes in muscle function and mass post-surgery.