Journal Description
Gastrointestinal Disorders
Gastrointestinal Disorders
is an international, open access, peer-reviewed journal on gastroenterology, published quarterly online by MDPI. The Robotic Global Surgical Society (TROGSS) is affiliated with Gastrointestinal Disorders and its members receive discounts on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions; authors retain copyright.
- High Visibility: indexed within Scopus, ESCI (Web of Science), FSTA, and other databases.
- Journal Rank: CiteScore - Q2 (Immunology and Microbiology (miscellaneous))
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 19.2 days after submission; acceptance to publication is undertaken in 3.9 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
- Reliable service: rigorous peer review and professional production.
Impact Factor:
0.8 (2024)
Latest Articles
Beyond the Gut: Inflammatory Bowel Disease as a Driver of Cardiovascular and Thromboembolic Risk—A Systematic Review and Meta-Analysis of 1.4 Million Patients
Gastrointest. Disord. 2025, 7(4), 78; https://doi.org/10.3390/gidisord7040078 - 11 Dec 2025
Abstract
►
Show Figures
Background: Inflammatory bowel disease (IBD) is associated with systemic inflammation and potential cardiovascular complications. This meta-analysis evaluates long-term cardiovascular risks in IBD. Methods: Electronic databases were searched for studies examining cardiovascular, cerebrovascular, and thromboembolic risks in IBD. Adjusted hazard ratios (aHRs)
[...] Read more.
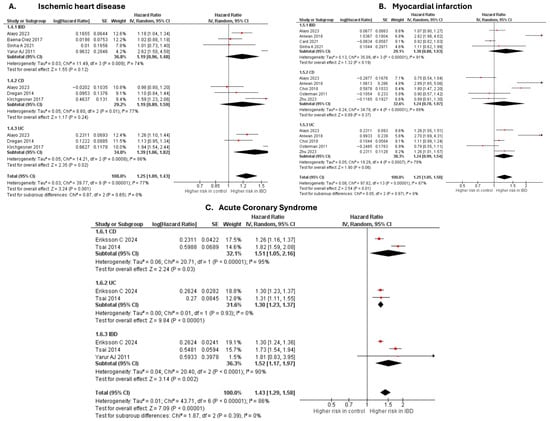
Background: Inflammatory bowel disease (IBD) is associated with systemic inflammation and potential cardiovascular complications. This meta-analysis evaluates long-term cardiovascular risks in IBD. Methods: Electronic databases were searched for studies examining cardiovascular, cerebrovascular, and thromboembolic risks in IBD. Adjusted hazard ratios (aHRs) with 95% confidence intervals (CIs) were pooled using a random-effects model. Results: Fifty-three studies comprising 1,406,773 patients were analyzed. IBD was linked to increased risk of ischemic heart disease (aHR 1.25; p = 0.001) myocardial infarction (aHR 1.25; p = 0.01), acute coronary syndrome (aHR 1.43; p < 0.00001), heart failure (aHR 1.24; p < 0.00001), atrial fibrillation (aHR 1.20; p < 0.00001), and stroke (aHR 1.13; p < 0.00001). Elevated risks were also observed for peripheral arterial disease (aHR 1.41; p < 0.00001), diabetes mellitus (aHR 1.40; p < 0.00001), venous thromboembolism (aHR 1.98; p < 0.00001), deep vein thrombosis (aHR 2.85; p = 0.0004), and pulmonary embolism (aHR 1.98; p = 0.03). Importantly, IBD was associated with increased cardiovascular (aHR 1.14; p = 0.03) and all-cause mortality (aHR 1.53; p < 0.00001). Conclusions: IBD patients face higher risk for adverse cardiovascular outcomes, thromboembolic disease, and mortality, necessitating early cardiovascular risk assessment and targeted interventions in this population.
Full article
Open AccessReview
Beyond Digestion: The Gut Microbiota as an Immune–Metabolic Interface in Disease Modulation
by
Imran Mohammad, Md. Rizwan Ansari, Mohammed Sarosh Khan, Md. Nadeem Bari, Mohammad Azhar Kamal and Muhammad Musthafa Poyil
Gastrointest. Disord. 2025, 7(4), 77; https://doi.org/10.3390/gidisord7040077 - 3 Dec 2025
Abstract
The gut microbiota has emerged as a critical immune–metabolic interface, orchestrating a complex network of interactions that extend well beyond digestion. This highly diverse community of bacteria, viruses, archaea, and eukaryotic microbes modulates host immunometabolism, metabolic reprogramming, and systemic inflammatory responses, thereby shaping
[...] Read more.
The gut microbiota has emerged as a critical immune–metabolic interface, orchestrating a complex network of interactions that extend well beyond digestion. This highly diverse community of bacteria, viruses, archaea, and eukaryotic microbes modulates host immunometabolism, metabolic reprogramming, and systemic inflammatory responses, thereby shaping human health and disease trajectories. Dysbiosis, or disruption of microbial homeostasis, has been implicated in inflammatory bowel disease, cardiometabolic disorders, neurodegeneration, dermatological conditions, and tumorigenesis. Through the biosynthesis of short-chain fatty acids (SCFAs), bile acid derivatives, tryptophan metabolites, and microbial-derived indoles, the gut microbiota regulates epigenetic programming, barrier integrity, and host–microbe cross-talk, thereby influencing disease onset and progression. In oncology, specific microbial taxa and oncomicrobiotics (cancer-modulating microbes) are increasingly recognized as key determinants of immune checkpoint inhibitor (ICI) responsiveness, chemotherapeutic efficacy, and resistance mechanisms. Microbiota-targeted strategies such as fecal microbiota transplantation (FMT), precision probiotics, prebiotics, synbiotics, and engineered microbial consortia are being explored to recalibrate microbial networks and enhance therapeutic outcomes. At the systems level, the integration of multi-omics platforms (metagenomics, transcriptomics, proteomics, and metabolomics) combined with network analysis and machine learning-based predictive modeling is advancing personalized medicine by linking microbial signatures to clinical phenotypes. Despite remarkable progress, challenges remain, including the standardization of microbiome therapeutics, longitudinal monitoring of host–microbe interactions, and the establishment of robust ethical and regulatory frameworks for clinical translation. Future directions should prioritize understanding the causal mechanisms of microbial metabolites in immunometabolic regulation, exploring microbial niche engineering, and developing precision microbiome editing technologies (CRISPR, synthetic biology).
Full article
(This article belongs to the Special Issue Feature Papers in Gastrointestinal Disorders in 2025–2026)
►▼
Show Figures

Figure 1
Open AccessArticle
Preoperative Injection of Indocyanine Green Fluorescence at the Anorectal Junction Safely Identifies the Inferior Mesenteric Artery in a Prospective Case-Series Analysis of Colorectal Cancer Patients
by
Franco Roviello, Eleonora Andreucci, Ludovico Carbone, Natale Calomino, Stefania Piccioni, Lucia Bobbio, Riccardo Piagnerelli, Andrea Fontani and Daniele Marrelli
Gastrointest. Disord. 2025, 7(4), 76; https://doi.org/10.3390/gidisord7040076 - 28 Nov 2025
Abstract
►▼
Show Figures
Background: Indocyanine green (ICG)-guided surgery is an emerging technique to enhance intraoperative visualization of nodes and tumor location. However, there is no uniform protocol regarding the optimal timing, dosage, or injection site for ICG in colorectal cancer surgery. We assess the feasibility
[...] Read more.
Background: Indocyanine green (ICG)-guided surgery is an emerging technique to enhance intraoperative visualization of nodes and tumor location. However, there is no uniform protocol regarding the optimal timing, dosage, or injection site for ICG in colorectal cancer surgery. We assess the feasibility of ICG injection at the anorectal junction immediately before surgery to safely identify the inferior mesenteric artery (IMA). Methods: This was a prospective study involving robotic left hemicolectomy or anterior resection of the rectum for primary colorectal cancer in 2024 in a single center. A total of 10–20 mg was injected into the anorectal submucosa at four quadrants circumferentially using an anoscope immediately before robot docking. Results: In this first study, ICG allowed us to identify the IMA in 84.6% of 26 patients (mean age 66.5 years; BMI 26.7 kg/m2), without intraoperative medical and surgical complications. Elevated BMI correlated with failure of IMA detection (r = −0.77, p < 0.001), despite high ICG doses trending toward improved vascular visualization (p = 0.097). A mean of 22 lymph nodes was harvested after ICG injection, with yields unaffected by the quality of IMA visualization. Conclusions: Submucosal injection of ICG is a feasible and easily adoptable option for early identification of the IMA, thereby preventing major vascular injuries, particularly in patients with challenging anatomy. A standardized protocol was implemented to improve reliability.
Full article

Figure 1
Open AccessReview
Endobiliary Radiofrequency Ablation: Principles, Technique, and Evidence in Cholangiocarcinoma
by
Michele Montori, Daniele Balducci, Francesco Martini, Marco Valvano, Andrea Sorge, Maria Eva Argenziano, Enrico Palmeri, Giuseppe Tarantino, Marco Marzioni, Antonio Benedetti and Luca Maroni
Gastrointest. Disord. 2025, 7(4), 75; https://doi.org/10.3390/gidisord7040075 - 26 Nov 2025
Abstract
Unresectable extrahepatic cholangiocarcinoma remains a challenging malignancy with limited therapeutic options and poor prognosis. In this setting, effective and durable biliary drainage is crucial to prevent cholangitis, allow timely initiation and maintenance of systemic therapy, and ultimately improve survival. Endobiliary radiofrequency ablation (RFA)
[...] Read more.
Unresectable extrahepatic cholangiocarcinoma remains a challenging malignancy with limited therapeutic options and poor prognosis. In this setting, effective and durable biliary drainage is crucial to prevent cholangitis, allow timely initiation and maintenance of systemic therapy, and ultimately improve survival. Endobiliary radiofrequency ablation (RFA) has emerged as a promising adjunct to biliary stenting, aimed at delaying tumor ingrowth and prolonging stent patency through localized thermal ablation of malignant tissue. Several studies have reported longer stent patency and, in some cases, improved survival with RFA plus stenting compared with stenting alone. However, the literature remains heterogeneous, and recent high-quality trials have yielded conflicting results, highlighting the need for further standardization of technique and patient selection. This narrative review summarizes the current evidence on the role of endobiliary RFA in unresectable cholangiocarcinoma, with particular emphasis on mechanism of action, endoscopic technique and oncologic outcomes.
Full article
(This article belongs to the Special Issue Feature Papers in Gastrointestinal Disorders in 2025–2026)
►▼
Show Figures
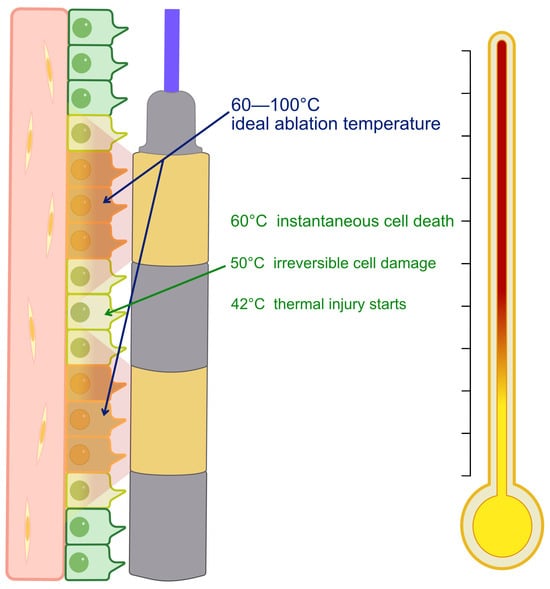
Figure 1
Open AccessCase Report
Paraneoplastic Hypereosinophilia Revealing Disseminated Colorectal Signet Ring Cell Carcinoma
by
Saša Rink, Sabina Škrgat, Matevž Harlander and Polona Mlakar
Gastrointest. Disord. 2025, 7(4), 74; https://doi.org/10.3390/gidisord7040074 - 24 Nov 2025
Abstract
►▼
Show Figures
Background: Hypereosinophilia, defined as a peripheral blood eosinophil count greater than 1.5 × 109/L, can arise from allergic, infectious, autoimmune, or malignant conditions. In solid tumors, it is rare and most often linked to mucin-secreting carcinomas, while on extremely rare
[...] Read more.
Background: Hypereosinophilia, defined as a peripheral blood eosinophil count greater than 1.5 × 109/L, can arise from allergic, infectious, autoimmune, or malignant conditions. In solid tumors, it is rare and most often linked to mucin-secreting carcinomas, while on extremely rare occasions, it accompanies signet ring cell carcinoma, a highly aggressive form of adenocarcinoma. Case Presentation: A 64-year-old woman presented with dyspnea and hypereosinophilia (2.9 × 109/L). She was admitted with suspected eosinophilic pneumonia, but extensive testing was inconclusive. After bone marrow biopsy, her condition deteriorated; histology revealed metastatic signet ring cell carcinoma. PET/CT showed skeletal metastases without apparent local recurrence, although colonoscopy could not be performed to definitively rule it out. Retrospective review uncovered a 2 mm rectal polyp with signet ring cell carcinoma (SRCC) removed two years earlier. Peripheral eosinophilia progressively increased from 0.16 × 109/L ten months earlier to a peak of 4.29 × 109/L one month prior to admission. She died four weeks after discharge. Conclusions: To the best of our knowledge, this case represents one of the smallest reported primary colorectal SRCC lesions (2 mm) presenting with disseminated disease and paraneoplastic hypereosinophilia as the first diagnostic clue. Monitoring peripheral blood eosinophil counts may provide additional insight into disease activity and prognosis in solid tumors.
Full article

Figure 1
Open AccessCorrection
Correction: Rivero-Moreno et al. Single Anastomosis Duodenoileostomy with Sleeve Gastrectomy Versus Sleeve Gastrectomy Alone: A Systematic Review and Meta-Analysis on Behalf of TROGSS—The Robotic Global Surgical Society. Gastrointest. Disord. 2025, 7, 27
by
Yeisson Rivero-Moreno, Alba Zevallos, Samantha Redden-Chirinos, Víctor Bolivar-Marín, Dayanna Silva-Martinez, Aman Goyal, Arturo Estrada, Rebeca Domínguez-Profeta, Diego Camacho, Sjaak Pouwels, Wah Yang, Luigi Marano, Adel Abou-Mrad and Rodolfo J. Oviedo
Gastrointest. Disord. 2025, 7(4), 73; https://doi.org/10.3390/gidisord7040073 - 10 Nov 2025
Abstract
In the original publication [...]
Full article
Open AccessReview
Akkermansia muciniphila in Cardiometabolic Medicine: Mechanisms, Clinical Studies, and Therapeutic Outlook
by
Alireza FakhriRavari and Minh Hien Chau Nguyen
Gastrointest. Disord. 2025, 7(4), 72; https://doi.org/10.3390/gidisord7040072 - 9 Nov 2025
Abstract
Akkermansia muciniphila—a mucus-resident commensal—has emerged as a promising target at the interface of metabolism, barrier function, and immunity. Observational human studies link higher intestinal abundance of A. muciniphila with healthier adiposity and glycemic profiles, while preclinical experiments demonstrate causal benefits on adiposity,
[...] Read more.
Akkermansia muciniphila—a mucus-resident commensal—has emerged as a promising target at the interface of metabolism, barrier function, and immunity. Observational human studies link higher intestinal abundance of A. muciniphila with healthier adiposity and glycemic profiles, while preclinical experiments demonstrate causal benefits on adiposity, insulin resistance, gut-barrier integrity, and inflammatory tone. These effects are attributed to mucus-layer reinforcement, reduced intestinal permeability and endotoxemia, production of short-chain fatty acids, and host signaling by defined bacterial components. In a randomized proof-of-concept trial in overweight/obese insulin-resistant adults, pasteurized A. muciniphila was safe and well-tolerated and improved insulin sensitivity and total cholesterol versus placebo; live cells showed directionally favorable but non-significant trends. A separate multicenter randomized trial of a five-strain consortium that included A. muciniphila improved post-prandial glucose and HbA1c in type 2 diabetes, supporting translational potential while underscoring the need for strain-resolved studies. Evidence for liver and cardiovascular benefits is strong in animals (e.g., MASLD and atherosclerosis models) but remains preliminary in humans. Inter-individual response heterogeneity—potentially influenced by baseline Akkermansia levels and gut-barrier status—highlights the value of personalized, microbiome-guided approaches. Larger, longer clinical studies are now warranted to define optimal dosing and formulation (live vs. pasteurized), durability, safety across populations, and impacts on hard outcomes (clinically meaningful weight change, glycemic endpoints, and cardiometabolic events). Overall, A. muciniphila represents a promising microbial adjunct for metabolic health with a plausible path from postbiotic concepts to clinical application, pending confirmatory trials.
Full article
Open AccessArticle
Facilitating and Hindering Factors in the Implementation of a Care Transition Strategy: Mixed Methods Study
by
Marcia Baiocchi Amaral Danielle, Elisiane Lorenzini, Ana Letícia Missio de Oliveira, Anthony John Onwuegbuzie, Letícia Flores Trindade, Michelle Mariah Malkiewiez, Darlisom Sousa Ferreira, Luana Amaral Alpirez and Adriane Cristina Bernat Kolankiewicz
Gastrointest. Disord. 2025, 7(4), 71; https://doi.org/10.3390/gidisord7040071 - 5 Nov 2025
Abstract
►▼
Show Figures
Objective: To identify facilitating and hindering factors for implementing a care transition strategy for adult patients undergoing elective colorectal cancer surgery, within a primary health care (PHC) context, addressing gaps in the literature on implementation challenges and contextual factors influencing such strategies.
[...] Read more.
Objective: To identify facilitating and hindering factors for implementing a care transition strategy for adult patients undergoing elective colorectal cancer surgery, within a primary health care (PHC) context, addressing gaps in the literature on implementation challenges and contextual factors influencing such strategies. Methods: This complex mixed methods study combined a randomized clinical trial (RCT) and a qualitative component within an Implementation Research framework. The RCT enrolled adult patients with colorectal cancer, while the qualitative phase included a multilevel sample of participants. Iterative data integration occurred throughout the planning, implementation, and evaluation phases. The intervention was assessed using the RE-AIM (Reach, Efficacy, Adoption, Implementation, Maintenance) framework. Statistical analyses were conducted using IBM SPSS Statistics 22.0, applying descriptive and inferential methods. Results: Our findings revealed that the adoption of the intervention was satisfactory; however, Reach, Efficacy, and Implementation were not achieved. Facilitating factors included recognition of the potential of the care transition strategy to improve patient outcomes, and the intervention’s feasibility, replicability, and low cost. The main hindering factors identified included poor communication between care levels, inadequate material resources, and high workload. Integration of qualitative insights helped explain the limited quantitative impact, highlighting contextual challenges during the COVID-19 pandemic. Conclusions: The care transition strategy was well accepted by participants and health care providers, demonstrating potential to strengthen continuity of care between hospital and PHC services. Nonetheless, significant organizational and resource-related barriers hindered its effectiveness. Future studies are required to adapt transitional care models to overcome communication gaps, optimize resource allocation, and enhance implementation in similar settings.
Full article

Figure 1
Open AccessReview
Venous Manifestations of Gastric Cancer: Bilateral Varicose Veins as a Rare Initial Presentation—A Narrative Review
by
Anna Laura Maiozzi, Filomena Botta, Silvia Maccioni, Livia Stanga, Lucretia Marin-Bancila, Ciprian Ilie Rosca, Anca Dinu, Abhinav Sharma and Nilima Rajpal Kundnani
Gastrointest. Disord. 2025, 7(4), 70; https://doi.org/10.3390/gidisord7040070 - 31 Oct 2025
Abstract
►▼
Show Figures
Background: Varicose veins (VVs) are an overlying manifestation of chronic venous disease, commonly occurring in the lower extremities. While typically linked to primary venous insufficiency, they can occasionally be secondary to systemic disease, e.g., malignancies, by various mechanisms such as tumor compression, hypercoagulability,
[...] Read more.
Background: Varicose veins (VVs) are an overlying manifestation of chronic venous disease, commonly occurring in the lower extremities. While typically linked to primary venous insufficiency, they can occasionally be secondary to systemic disease, e.g., malignancies, by various mechanisms such as tumor compression, hypercoagulability, and paraneoplastic syndromes. Bilateral varicose veins, as a presenting symptom of gastric cancer, are extremely rare and poorly documented. Materials and Methods: A comprehensive literature search was conducted to identify reports and studies linking varicose veins and malignancies, with particular focus on gastric cancer. The search was performed using the PubMed, Scopus, and Web of Science databases covering the last 13 years. Results: Literature Review: A review of the literature in the past decade identified publications, mostly case reports, describing associations between varicose-like venous changes and malignancies such as gastric, pancreatic, hepatic, and small-bowel tumors. The predominant mechanisms reported were inferior vena cava obstruction, tumor-related thrombosis, and paraneoplastic migratory superficial thrombophlebitis (Trousseau’s syndrome). Only a few cases involved gastric cancer as the primary site, with venous changes often being the first clinical sign. There is limited experience with gastric cancer that presents alongside bilateral collateral or varicose veins initially. Apart from the various reports having malignancies and varicose veins we also describe the case of a 50-year-old man who had extended history of bilateral lower-limb varicose veins. Severe, unexplained anaemia without obvious bleeding was discovered during examination. A biopsy verified a gastric adenocarcinoma, while upper gastrointestinal endoscopy revealed an ulcerated mass on the stomach’s greater curvature. Peritoneal dissemination was discovered with additional staging. A palliative subtotal gastrectomy was carried out because of the patient’s ongoing anaemia and suspected chronic bleeding caused by the tumour. The venous symptoms preceded any gastrointestinal issues. Conclusions: Although uncommon, malignancy should be considered in the differential diagnosis for atypical or rapidly progressing bilateral varicose veins, especially when accompanied by systemic symptoms or lab results such as unexplained anemia. Increased suspicion may lead to earlier cancer detection in some patients.
Full article

Figure 1
Open AccessReview
Global Dynamics of Research on Antibiotic Resistance in Helicobacter pylori: A Bibliometric Analysis
by
Sergiu Dorin Matei, Ramona Nicoleta Suciu, Tiberia Ilias, Cristian Hocopan and Ovidiu Frățilă
Gastrointest. Disord. 2025, 7(4), 69; https://doi.org/10.3390/gidisord7040069 - 30 Oct 2025
Abstract
►▼
Show Figures
This review conducts a bibliometric analysis of scientific literature on antibiotic resistance in Helicobacter pylori (H. Pylori), aiming to map scientific production, identify trends and key themes, analyze collaboration models, and highlight research gaps to inform research priorities and guide public
[...] Read more.
This review conducts a bibliometric analysis of scientific literature on antibiotic resistance in Helicobacter pylori (H. Pylori), aiming to map scientific production, identify trends and key themes, analyze collaboration models, and highlight research gaps to inform research priorities and guide public health policies, amidst the growing challenge of multidrug resistance affecting treatment success. Background/Objectives: H. Pylori infection is usually contracted during childhood and often becomes chronic and asymptomatic in 80–90% of cases. Eradication requires complex treatments involving proton pump inhibitors and multiple antibiotics, but success rates have declined due to increased antibiotic resistance caused by genetic mutations, efflux mechanisms, altered membrane permeability, and biofilm formation. Reports indicate an alarming increase in multidrug resistance, affecting the effectiveness of treatments. Methods: The bibliometric analysis was performed using the Web of Science Core Collection (WoS) database, which provides comprehensive bibliographic data. Filters were applied for articles in English, reducing the set to 39,879 papers. The analysis was performed using the VOSviewer program (v1.6.20) to visualize co-author networks, citations, and keyword co-occurrence, and Microsoft Excel for processing and organization. Results: Editorial Trends: Over the last decade (2016–2025), interest in this topic has increased, with over 4000 publications annually in 2020, although a slight decline was observed in 2023. Leading Contributors: China is the most prolific author, followed by the USA and Japan. Cited Articles and Key Publications: Articles by prominent authors are frequently cited in 2022 and 2023, indicating their high relevance. Bibliographic Coupling Analysis: This revealed three main thematic clusters centered around research by specific authors. Keyword Analysis: A total of 57,462 terms were identified, of which 5292 appeared at least five times; “Helicobacter pylori” was the most frequent, followed by “infection” and “eradication.” Visualized terms highlight central areas of interest, such as “risk,” “cancer,” and “resistance”. Conclusions: This bibliometric analysis underscores a rising research focus on H. pylori antibiotic resistance, with recent publications providing essential clinical guidelines and epidemiological insights into the infection’s global impact. China leads in contributions, followed by the US and Japan. Significant articles by notable authors received many citations, emphasizing their significance.
Full article

Figure 1
Open AccessReview
Gut Microbiota: An Ally in the Mechanisms and Interventions of Healthy Aging
by
Samia Chatterjee, Ananda Vardhan Hebbani and Khajamohiddin Syed
Gastrointest. Disord. 2025, 7(4), 68; https://doi.org/10.3390/gidisord7040068 - 26 Oct 2025
Abstract
►▼
Show Figures
The gut microbiota greatly influences host physiology, including immune regulation, metabolic balance, and brain health. Aging is associated with alterations in the gut microbiome, including reduced microbial diversity and increased pro-inflammatory bacteria, which are linked to age-related decline and chronic diseases. This review
[...] Read more.
The gut microbiota greatly influences host physiology, including immune regulation, metabolic balance, and brain health. Aging is associated with alterations in the gut microbiome, including reduced microbial diversity and increased pro-inflammatory bacteria, which are linked to age-related decline and chronic diseases. This review examines the impact of the gut microbiota on key indicators of aging, including cellular senescence, mitochondrial dysfunction, alterations in gene expression, and immune system modifications. It also examines microbiome-related diseases associated with aging, including neurodegeneration, cardiovascular issues, metabolic syndrome, and frailty. Additionally, it highlights evidence-based methods to restore a youthful microbial profile. New findings suggest that certain microbial substances, including short-chain fatty acids, urolithins, and bile acids, play a role in regulating inflammation, maintaining barrier integrity, and influencing metabolism. Age-related diseases are often associated with molecular pathways driven by an imbalance in the gut microbiome. Various intervention strategies, from dietary changes and probiotics to personalized nutrition and fecal microbiota transplantation, have shown promise in reversing signs of microbial aging and improving health outcomes in both lab and human studies. Overall, the gut microbiome serves as both a marker and a regulator of healthy aging. Treatments that restore microbial balance offer hopeful ways to extend healthy living. Future studies should focus on developing long-term, multifaceted, and personalized methods to identify causal pathways and enhance microbiota-based strategies for various aging populations.
Full article

Figure 1
Open AccessReview
Genetic Predisposition and Nutritional Interactions in Gastroenterology: A Review of European Clinical Recommendations
by
Vaios Svolos, Anastasia Triantafyllou, Georgios Charmantzis, Maria Delliou, Maria-Nikoletta Nanti, Melina Moustaka, Eleni Bakasieta, Evanthia Balafa, Dimitra Eleftheria Strongylou and Odysseas Androutsos
Gastrointest. Disord. 2025, 7(4), 67; https://doi.org/10.3390/gidisord7040067 - 17 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Despite the growing understanding of the relationship between the genome and nutrition, clearly defined and evidence-based clinical guidelines remain insufficient. The objective of this review was to identify and compile all available European guidelines related to the impact of genetic predisposition
[...] Read more.
Background/Objectives: Despite the growing understanding of the relationship between the genome and nutrition, clearly defined and evidence-based clinical guidelines remain insufficient. The objective of this review was to identify and compile all available European guidelines related to the impact of genetic predisposition on nutritional recommendations in the field of gastroenterology. Methods: A review of guidelines and position papers issued by four European organisations [the European Crohn’s and Colitis Organisation (ECCO), the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN), the European Society for Clinical Nutrition and Metabolism (ESPEN), and United European Gastroenterology (UEG)] was conducted for the past ten years. Results: Out of 5196 recommendations and statements extracted from 124 manuscripts, only 13 highlighted a link between genetic predisposition and dietary factors in clinical gastroenterology. From the available guidelines, there is no clear trend indicating an increased focus on genetic background and its association with nutrition in recent years. Conclusions: There is a critical opportunity for European organisations to develop an evidence-based information framework, guided by clinical protocols, in order to integrate the large volume of genetic data into clinical practice and personalised care of individuals with gastrointestinal disorders.
Full article

Graphical abstract
Open AccessReview
Toward Earlier Detection: Revisiting Colorectal Cancer Screening Age in the U.S. and Europe
by
Vlad Buică, Ancuța Năstac, Gina Gheorghe, Teodor Florin Georgescu, Camelia Cristina Diaconu and Vlad Alexandru Ionescu
Gastrointest. Disord. 2025, 7(4), 66; https://doi.org/10.3390/gidisord7040066 - 16 Oct 2025
Abstract
►▼
Show Figures
Background: Colorectal cancer (CRC) represents one of the leading causes of cancer-related morbidity and mortality globally. Although national screening programs in Europe and the United States have demonstrated success in reducing incidence and death rates among populations aged 50 and above, a
[...] Read more.
Background: Colorectal cancer (CRC) represents one of the leading causes of cancer-related morbidity and mortality globally. Although national screening programs in Europe and the United States have demonstrated success in reducing incidence and death rates among populations aged 50 and above, a concerning increase in early-onset colorectal cancer (EOCRC), defined as diagnosis before age 50, has emerged. Methods: This paper is a narrative literature review comparing American and European CRC screening guidelines. A comprehensive search was conducted using the PubMed database with emphasis on publications from the past ten years. Results: The United States has adapted more swiftly to EOCRC trends by lowering the recommended screening age to 45, supported by modeling studies showing life-years gained and improved cost-effectiveness. In contrast, European programs remain largely organized and cost-efficient but predominantly initiate screening at age 50, potentially missing high-risk younger adults. EOCRC appears to demonstrate unique molecular and pathological features compared to late-onset CRC. Participation and adherence to screening also vary significantly between regions and modalities, with colonoscopy remaining the gold standard but less scalable than fecal immunochemical tests. Conclusions: The rising incidence of EOCRC calls for a reassessment of CRC screening policies. While the European model emphasizes equity and structure, its slower responsiveness to epidemiological changes may lead to late detection in younger cohorts. The American model’s earlier screening age addresses emerging trends but faces challenges in implementation equity. A hybrid approach may provide the optimal management, balancing public health benefit with system sustainability.
Full article

Figure 1
Open AccessArticle
Assessment of the Accuracy and Clinical Impact of the Preoperative Histopathology of Resected Early Gastric Cancers
by
Pedro Mesquita, Rolando Pinho, João Carlos Silva, Catarina Costa, Pedro Teixeira, Rita Ferreira, Liliana Santos, Ana Ponte and Teresa Freitas
Gastrointest. Disord. 2025, 7(4), 65; https://doi.org/10.3390/gidisord7040065 - 15 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Superficial gastric neoplasms, including dysplasia and early adenocarcinoma, are increasingly managed by endoscopic submucosal dissection (ESD). Preoperative assessment relies on endoscopic forceps biopsy (EFB), despite its limited ability to predict final histology. The diagnostic value of repeat biopsy, the influence of the
[...] Read more.
Background/Objectives: Superficial gastric neoplasms, including dysplasia and early adenocarcinoma, are increasingly managed by endoscopic submucosal dissection (ESD). Preoperative assessment relies on endoscopic forceps biopsy (EFB), despite its limited ability to predict final histology. The diagnostic value of repeat biopsy, the influence of the endoscopy setting where biopsies were taken, and the clinical relevance of histologic discrepancies remain incompletely defined. Methods: We conducted a retrospective, single-center study of 270 superficial gastric lesions resected by ESD between 2015 and 2024. Histologic concordance between EFB and ESD was evaluated, including comparisons between initial and repeated biopsies, and between community- and hospital-based settings. Multivariable models identified predictors of histologic discrepancy and assessed the impact of underestimation on curative resection. The association between biopsy repetition and submucosal fibrosis was also explored. Results: Histologic concordance between EFB and ESD was 54.1%, with underestimation in 41.1% and severe underestimation in 8.9%. Repeat biopsy improved concordance from 39.3% to 60.7% (p = 0.007) and increased adenocarcinoma sensitivity from 12.5% to 56.3%, without increasing submucosal fibrosis. Hospital-based biopsies outperformed community-based ones across all diagnostic metrics. In multivariable analysis, older age and larger lesion size were independent predictors of discrepancy. Histologic underestimation was independently associated with a lower likelihood of curative resection (OR = 0.148; p = 0.003), although only six lesions ultimately exceeded formal ESD criteria due to undetected high-risk features. Conclusions: EFB frequently underestimates histological severity in superficial gastric neoplasia. Repeat biopsy and centralized evaluation significantly improve diagnostic accuracy without increasing procedural risk. However, the role of biopsy lies primarily in excluding high-risk features rather than providing definitive staging. In this context, ESD serves not only as curative therapy but also as a key diagnostic step for accurate staging and treatment planning.
Full article

Figure 1
Open AccessReview
Achalasia and Thyroid Disorders: A Hidden Autoimmune Overlap? Epidemiology, Mechanisms, and Clinical Relevance of an Emerging Association
by
Agostino Fernicola, Armando Calogero, Felice Crocetto, Giacomo Capece, Guido Bocchino and Michele Santangelo
Gastrointest. Disord. 2025, 7(4), 64; https://doi.org/10.3390/gidisord7040064 - 30 Sep 2025
Abstract
Background: Achalasia is a rare primary esophageal motility disorder characterized by impaired lower esophageal sphincter relaxation and progressive loss of peristalsis. Although its pathogenesis remains incompletely understood, autoimmune mechanisms have been repeatedly proposed. Thyroid disorders, particularly autoimmune thyroiditis and Graves’ disease, have been
[...] Read more.
Background: Achalasia is a rare primary esophageal motility disorder characterized by impaired lower esophageal sphincter relaxation and progressive loss of peristalsis. Although its pathogenesis remains incompletely understood, autoimmune mechanisms have been repeatedly proposed. Thyroid disorders, particularly autoimmune thyroiditis and Graves’ disease, have been reported as frequent comorbidities, suggesting a shared autoimmune background. Methods: We conducted a narrative review of PubMed, Scopus, and Web of Science from January 2005 to August 2025. Eligible studies included observational cohorts, case–control analyses, and case reports describing thyroid disease in achalasia. Mechanistic and immunological studies relevant to thyroid autoimmunity were also considered. Data were synthesized narratively and summarized in tables and figures. Results: Despite heterogeneity, evidence consistently indicates an increased prevalence of thyroid disease in achalasia. Early reports described dysfunction in up to one quarter of cases, while Romero-Hernández et al. demonstrated a threefold higher risk of autoimmune thyroid disease. Multicenter data confirmed thyroid autoimmunity in about one fifth of patients. Although thyroid disease did not alter short-term procedural outcomes, unrecognized dysfunction may complicate postoperative evaluation. Immunological findings, including human leukocyte antigen (HLA) susceptibility and lymphocytic infiltration of myenteric plexus, further support a shared autoimmune predisposition. Conclusions: Thyroid disorders, particularly autoimmune hypothyroidism, are more common in achalasia than in the general population. Although the evidence remains limited, the consistent signal suggests a non-random association. Early recognition may improve patient management, while prospective multicenter studies are needed to clarify causality and to determine whether achalasia should be considered part of a broader autoimmune spectrum.
Full article
(This article belongs to the Special Issue Feature Papers in Gastrointestinal Disorders in 2025–2026)
►▼
Show Figures

Figure 1
Open AccessReview
The Role of Artificial Intelligence and Information Technology in Enhancing and Optimizing Stapling Efficiency in Metabolic and Bariatric Surgery: A Comprehensive Narrative Review
by
Sjaak Pouwels, Alex Mwangi, Michail Koutentakis, Moises Mendoza, Sanskruti Rathod, Santosh Parajuli, Saurabh Singhal, Uresha Lakshani, Wah Yang, Kahei Au and Safwan Taha
Gastrointest. Disord. 2025, 7(4), 63; https://doi.org/10.3390/gidisord7040063 - 30 Sep 2025
Cited by 1
Abstract
Background: Over the years, surgical techniques have evolved, resulting in an abundance of available procedures in the armamentarium of metabolic and bariatric surgeons, and the technology has also advanced in a similar way. Significant steps have been made in stapling technology especially,
[...] Read more.
Background: Over the years, surgical techniques have evolved, resulting in an abundance of available procedures in the armamentarium of metabolic and bariatric surgeons, and the technology has also advanced in a similar way. Significant steps have been made in stapling technology especially, introducing artificial intelligence (AI) in optimizing this technology for better treatment outcomes. The introduction of AI in stapling technology showed a decrease in potential stapling complications not only in MBS, but also in other (surgical) specialties. Areas Covered: This review will cover the general principles of stapling in surgery, but with an emphasis on both the technical and anatomical considerations. We will also discuss the mechanisms of staplers and potential safety hazards. Finally, we will focus on how AI is integrated in stapling technology, potential pros and cons, and areas for future development of stapling technology and the integration of AI. Conclusions: In metabolic and bariatric surgery, stapling is a technical procedure that requires a comprehensive understanding of the anatomical and physiological characteristics of the target tissue. Variability in tissue thickness, vascularity, elasticity, and mechanical load, compounded by patient-specific factors and intraoperative dynamics, demands constant vigilance and adaptability from the surgeon. The integration of AI and digital technologies offers potential improvements in refining this process. By providing real-time feedback on tissue properties and supporting intraoperative decision-making, these tools can assist surgeons in optimizing staple-line integrity and minimizing complications. The ongoing combination of surgical expertise with intelligent technology may contribute to advancing precision stapling in metabolic and bariatric surgery.
Full article
(This article belongs to the Special Issue GastrointestinaI & Bariatric Surgery)
Open AccessReview
Keystone Species Restoration: Therapeutic Effects of Bifidobacterium infantis and Lactobacillus reuteri on Metabolic Regulation and Gut–Brain Axis Signaling—A Qualitative Systematic Review (QualSR)
by
Michael Enwere, Edward Irobi, Adamu Onu, Emmanuel Davies, Gbadebo Ogungbade, Omowunmi Omoniwa, Charles Omale, Mercy Neufeld, Victoria Chime, Ada Ezeogu, Dung-Gwom Pam Stephen, Terkaa Atim and Laurens Holmes, Jr.
Gastrointest. Disord. 2025, 7(4), 62; https://doi.org/10.3390/gidisord7040062 - 28 Sep 2025
Abstract
Background: The human gut microbiome—a diverse ecosystem of trillions of microorganisms—plays an essential role in metabolic, immune, and neurological regulation. However, modern lifestyle factors such as antibiotic overuse, cesarean delivery, reduced breastfeeding, processed and high-sodium diets, alcohol intake, smoking, and exposure to
[...] Read more.
Background: The human gut microbiome—a diverse ecosystem of trillions of microorganisms—plays an essential role in metabolic, immune, and neurological regulation. However, modern lifestyle factors such as antibiotic overuse, cesarean delivery, reduced breastfeeding, processed and high-sodium diets, alcohol intake, smoking, and exposure to environmental toxins (e.g., glyphosate) significantly reduce microbial diversity. Loss of keystone species like Bifidobacterium infantis (B. infantis) and Lactobacillus reuteri (L. reuteri) contributes to gut dysbiosis, which has been implicated in chronic metabolic, autoimmune, cardiovascular, and neurodegenerative conditions. Materials and Methods: This Qualitative Systematic Review (QualSR) synthesized data from over 547 studies involving human participants and standardized microbiome analysis techniques, including 16S rRNA sequencing and metagenomics. Studies were reviewed for microbial composition, immune and metabolic biomarkers, and clinical outcomes related to microbiome restoration strategies. Results: Multiple cohort studies have consistently reported a 40–60% reduction in microbial diversity among Western populations compared to traditional societies, particularly affecting short-chain fatty acid (SCFA)-producing bacteria. Supplementation with B. infantis is associated with a significant reduction in systemic inflammation—including a 50% decrease in C-reactive protein (CRP) and reduced tumor necrosis factor-alpha (TNF-α) levels—alongside increases in regulatory T cells and anti-inflammatory cytokines interleukin-10 (IL-10) and transforming growth factor-beta 1 (TGF-β1). L. reuteri demonstrates immunomodulatory and neurobehavioral benefits in preclinical models, while both probiotics enhance epithelial barrier integrity in a strain- and context-specific manner. In murine colitis, B. infantis increases ZO-1 expression by ~35%, and L. reuteri improves occludin and claudin-1 localization, suggesting that keystone restoration strengthens barrier function through tight-junction modulation. Conclusions: Together, these findings support keystone species restoration with B. infantis and L. reuteri as a promising adjunctive strategy to reduce systemic inflammation, reinforce gut barrier integrity, and modulate gut–brain axis (GBA) signaling, indicating translational potential in metabolic and neuroimmune disorders. Future research should emphasize personalized microbiome profiling, long-term outcomes, and transgenerational effects of early-life microbial disruption.
Full article
(This article belongs to the Special Issue Feature Papers in Gastrointestinal Disorders in 2025–2026)
►▼
Show Figures

Figure 1
Open AccessArticle
Impact of a Failsafe Reminder Letter and Associated Factors on Correct Follow-Up After a Positive FIT in the Flemish Colorectal Cancer Screening Program
by
Sarah Hoeck and Thuy Ngan Tran
Gastrointest. Disord. 2025, 7(4), 61; https://doi.org/10.3390/gidisord7040061 - 26 Sep 2025
Abstract
►▼
Show Figures
Background: Timely diagnostic colonoscopy (DC) after a positive fecal immunochemical test (FIT+) is essential for effective colorectal cancer (CRC) screening. In Flanders, 16% of FIT+ participants in 2022 had no DC in the 24 months following the FIT+ result. This study evaluated the
[...] Read more.
Background: Timely diagnostic colonoscopy (DC) after a positive fecal immunochemical test (FIT+) is essential for effective colorectal cancer (CRC) screening. In Flanders, 16% of FIT+ participants in 2022 had no DC in the 24 months following the FIT+ result. This study evaluated the impact of a failsafe reminder letter—sent 24 months after a FIT+ result without registered correct follow-up—on DC completion and identified factors associated with correct follow-up. Methods: We included all individuals in the Flemish CRC screening program who had a FIT+ result between 2017 and 2019 and later received a failsafe letter due to lacking correct follow-up within 24 months. Correct follow-up was defined as a complete colonoscopy, virtual colonoscopy, or cancer diagnosis. We calculated the proportion of individuals completing correct follow-up within 24 months of the letter. Multivariable logistic regression examined associations between odds of correct follow-up and individual and area-level characteristics. Results: Of the 7175 individuals who received a failsafe letter, 16.1% completed correct follow-up within 24 months. Individuals aged 70–74 had significantly lower odds of correct follow-up than those aged 60–64 (odd ratio (OR) = 0.59; 95% confidence interval (CI): 0.48–0.72). Living in areas with a higher proportion of young adults in higher education was associated with higher odds of correct follow-up (OR = 1.041; 95% CI: 1.002–1.080). Conclusions: The failsafe letter modestly improved follow-up among a hard-to-reach group. Older age and lower area-level educational attainment were linked to reduced odds of correct follow-up. Targeted efforts are needed to improve DC completion in these subgroups.
Full article

Figure 1
Open AccessArticle
General Practitioners and Gut Microbiota: Surveying Knowledge and Awareness in Italy
by
Cesare Tosetti, Alessandra Belvedere, Massimo Berardino, Luciano Bertolusso, Rosanna Cantarini, Francesco Carofiglio, Floriana Di Bella, Daniele Franchi, Andrea Furnari, Alessandro Marturano, Tecla Mastronuzzi, Roberto Barone, Giuseppe Disclafani, Silvia Dubini, Marco Prastaro, Riccardo Scoglio, Alessandro Rossi and Ignazio Grattagliano
Gastrointest. Disord. 2025, 7(4), 60; https://doi.org/10.3390/gidisord7040060 - 25 Sep 2025
Abstract
Background/Objectives: The role of the intestinal microbiota in gastroenterological diseases has gained increasing relevance in general medicine. The study aimed to evaluate the knowledge and awareness of Italian general practitioners regarding gut microbiota, as well as the clinical applications of probiotics and prebiotics.
[...] Read more.
Background/Objectives: The role of the intestinal microbiota in gastroenterological diseases has gained increasing relevance in general medicine. The study aimed to evaluate the knowledge and awareness of Italian general practitioners regarding gut microbiota, as well as the clinical applications of probiotics and prebiotics. Methods: The survey research involved 457 Italian general practitioners, who anonymously filled an online structured questionnaire. Results: Most respondents identified antibiotics, diet, gastrointestinal infections, and stress as factors that can modulate the gut microbiota, while a smaller proportion recognized the role of physical activity. A comparable number acknowledged the influence of obesity, smoking, and immunosuppressant drugs. Although most participants correctly defined probiotics, the concept of prebiotics was less widely understood. Probiotics were primarily prescribed for irritable bowel syndrome, suspected dysbiosis, or during antibiotic therapy, and only a portion of physicians reported routinely combining them with prebiotics. The selection of probiotic strains was mainly based on personal experience, while fecal microbiota analysis was seldom used in clinical practice. Conclusions: These findings provide an updated snapshot of current knowledge and practices regarding the microbiota in Italian general medicine and highlight critical gaps, particularly in the understanding of prebiotics and less recognized modulatory factors.
Full article
(This article belongs to the Special Issue Feature Papers in Gastrointestinal Disorders in 2025–2026)
►▼
Show Figures

Figure 1
Open AccessArticle
Cardiovascular Risk Assessments and Ultrasound-Assisted Re-Stratification in Patients with Inflammatory Bowel Disease (IBD)
by
Giuseppe Blando, Arianna Toscano, Anna Viola, Laura Patanè, Sabrina Verachtert, Carmela Morace, Giovanni Squadrito, Giuseppe Mandraffino, Angela Alibrandi, Walter Fries and Giuseppe Costantino
Gastrointest. Disord. 2025, 7(4), 59; https://doi.org/10.3390/gidisord7040059 - 24 Sep 2025
Abstract
Background: Patients with ulcerative colitis (UC) and Crohn’s disease (CD) have an increased cardiovascular risk (CVR). The aim of the present study was to stratify the CVR of patients with UC and CD according to the most recent guidelines via carotid ultrasound
[...] Read more.
Background: Patients with ulcerative colitis (UC) and Crohn’s disease (CD) have an increased cardiovascular risk (CVR). The aim of the present study was to stratify the CVR of patients with UC and CD according to the most recent guidelines via carotid ultrasound (US) to detect subclinical atherosclerotic disease. Methods: Demographic and disease-related data of consecutive patients with IBD were prospectively collected along with information on blood pressure, body mass index, lipid profile, and concomitant medications. CVR was stratified at inclusion according to the most recent version of Systematic Coronary Risk Evaluation 2 (SCORE2) and re-stratified after carotid US when subclinical atherosclerotic disease was detected. Results: A total of 166 patients aged ≥ 40 years with IBD were included. Before carotid US evaluation, 43.4% of patients with IBD were at moderate risk, 40.3% at high risk, and 16.3% at very high risk. With carotid US, subclinical atherosclerosis was diagnosed in 48% of patients, leading to CVR re-stratification from moderate to high in 18% of patients and from high to very high in 4% of patients. The only predictive factor for re-stratification was failure with more than two biologics (p = 0.047; OR 2.187, 95% CI: 1.004–4.741). Conclusions: CVR is considerably prevalent in patients with IBD. Carotid US may help to re-classify CVR and should be considered as a risk modifier in patients at intermediate risk. Screening for CVD risk factors should be recommended in IBD.
Full article
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Diagnostics, Gastrointestinal Disorders, IJMS, JCM, Nutrients, Medicina
Advances in Comprehensive Management Strategies for Inflammatory Bowel Disease
Topic Editors: Vito Annese, Vincenzo Villanacci, Fabiana Castiglione, Ferdinando D'Amico, Flavio CaprioliDeadline: 30 June 2026
Topic in
Cancers, Diagnostics, Gastrointestinal Disorders, JCM, Current Oncology
Metastatic Colorectal Cancer: From Laboratory to Clinical Studies, 2nd Edition
Topic Editors: Ioannis Ntanasis-Stathopoulos, Diamantis I. TsilimigrasDeadline: 20 August 2026
Topic in
Cancers, Diagnostics, Gastrointestinal Disorders, JCM, Children
Evolving Role of Endoscopy in Adult and Pediatric Gastrointestinal Disorders
Topic Editors: Valerio Balassone, Dominique Schluckebier, Matteo Tacelli, Luigi Dall'OglioDeadline: 30 November 2026
Topic in
Biomedicines, Current Oncology, Diagnostics, JCM, Livers, Transplantology, Gastrointestinal Disorders
Advances in Gastrointestinal and Liver Disease: From Physiological Mechanisms to Clinical Practice, 2nd Edition
Topic Editors: Davide Giuseppe Ribaldone, Gian Paolo CavigliaDeadline: 20 December 2026

Special Issues
Special Issue in
Gastrointestinal Disorders
Pediatric Gastrointestinal Endoscopy and Surgery: Current Challenges and Future Directions
Guest Editors: Mario Lima, Marco Di MitriDeadline: 25 January 2026
Special Issue in
Gastrointestinal Disorders
GastrointestinaI & Bariatric Surgery
Guest Editors: Rodolfo Oviedo, Aman Goyal, Luigi MaranoDeadline: 25 February 2026
Special Issue in
Gastrointestinal Disorders
The Interactions of Diet, Genes, Gut Microbiota and Immune System in Health and Disease
Guest Editors: Vaios Svolos, Athina A. SamaraDeadline: 20 May 2026
Special Issue in
Gastrointestinal Disorders
Novel Therapies for the Treatment of Inflammatory Bowel Disease
Guest Editors: Angharad Vernon-Roberts, Andrew DayDeadline: 25 June 2026