Topic Editors


Advances in Gastrointestinal and Liver Disease: From Physiological Mechanisms to Clinical Practice, 2nd Edition
Topic Information
Dear Colleagues,
The management of gastrointestinal and hepatic diseases is constantly evolving. The progressive understanding of pathogenic mechanisms has improved daily management, representing real translational medicine. For example, understanding the mechanisms underlying HCV virus infection has enabled the development of Direct-Acting Antivirals (DAAs), with a cure rate of 98%. However, patients with advanced liver disease, albeit cured from HCV infection, are still at risk of hepatocellular carcinoma (HCC) development. Therefore, these patients will remain a medical challenge for years to come. New antiviral agents are currently under development for the treatment of chronic delta hepatitis (CHD).
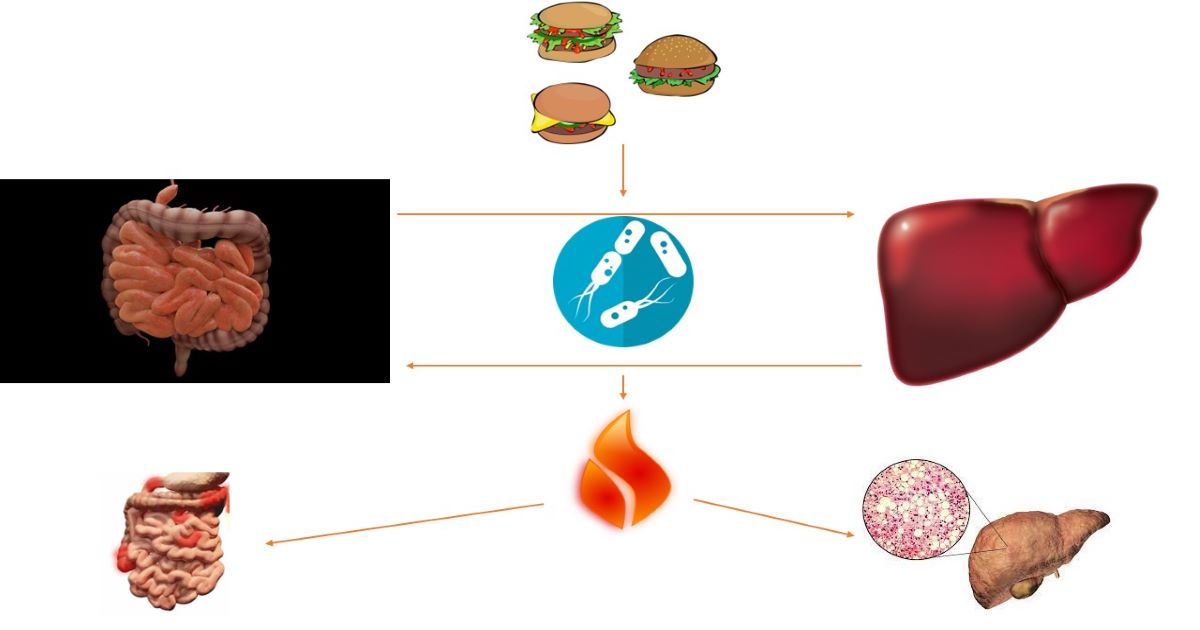
Hopefully, in the near future we will be able to at least control liver disease progression in patients with CHD, the most severe form of chronic viral hepatitis. In the coming decades, NAFLD/NASH will supplant viral hepatitis as the leading cause of chronic liver damage. Efforts are ongoing to identify novel biomarkers and tools for the detection of liver fibrosis and stratify the risk of liver disease progression. Moreover, novel molecules targeting several pathways involved in NAFLD onset and progression are under investigation. The decrease in the prevalence of Helicobacter pylori (H. pylori) infection, the widespread use of proton pump inhibitors, and the relative ease of access to gastroscopies have reduced the incidence of peptic disease and stomach cancer, which was once the main gastrointestinal pathology. In many areas of the world, however, H. pylori infection remains widespread, and there is still room for improvement in eradication strategies. Understanding the inflammatory pathways involved in inflammatory bowel disease has enabled the development of target therapies (anti-TNF, anti-IL12/23, anti-JAK, S1P1 modulators). Increased understanding of the microbiome will lead to applications that will go beyond the confines of the gut, although the COVID-19 pandemic will continue to affect the management of all diseases.
The objective of this Topic is to present the most up-to-date data on the pathogenesis and management of gastrointestinal and hepatological diseases, with a view to an increasingly personalized management of patients.
Dr. Davide Giuseppe Ribaldone
Dr. Gian Paolo Caviglia
Topic Editors
Keywords
- inflammatory bowel diseases
- chronic viral hepatitis
- hepatocellular carcinoma
- digestive endoscopy
- microbiota
- celiac disease
- NALFD
- COVID-19
- Helicobacter pylori
Participating Journals
| Journal Name | Impact Factor | CiteScore | Launched Year | First Decision (median) | APC | |
|---|---|---|---|---|---|---|

Biomedicines
|
3.9 | 6.8 | 2013 | 17 Days | CHF 2600 | Submit |

Current Oncology
|
3.4 | 4.9 | 1994 | 21.5 Days | CHF 2200 | Submit |

Diagnostics
|
3.3 | 5.9 | 2011 | 21 Days | CHF 2600 | Submit |

Journal of Clinical Medicine
|
2.9 | 5.2 | 2012 | 17.7 Days | CHF 2600 | Submit |

Livers
|
2.4 | 3.2 | 2021 | 27.8 Days | CHF 1200 | Submit |

Transplantology
|
- | 1.4 | 2020 | 38.9 Days | CHF 1000 | Submit |

Gastrointestinal Disorders
|
0.8 | 1.2 | 2019 | 19.2 Days | CHF 1400 | Submit |

Preprints.org is a multidisciplinary platform offering a preprint service designed to facilitate the early sharing of your research. It supports and empowers your research journey from the very beginning.
MDPI Topics is collaborating with Preprints.org and has established a direct connection between MDPI journals and the platform. Authors are encouraged to take advantage of this opportunity by posting their preprints at Preprints.org prior to publication:
- Share your research immediately: disseminate your ideas prior to publication and establish priority for your work.
- Safeguard your intellectual contribution: Protect your ideas with a time-stamped preprint that serves as proof of your research timeline.
- Boost visibility and impact: Increase the reach and influence of your research by making it accessible to a global audience.
- Gain early feedback: Receive valuable input and insights from peers before submitting to a journal.
- Ensure broad indexing: Web of Science (Preprint Citation Index), Google Scholar, Crossref, SHARE, PrePubMed, Scilit and Europe PMC.

