Journal Description
Obesities
Obesities
is an international, peer-reviewed, open access journal on all aspects of obesity published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 13.4 days after submission; acceptance to publication is undertaken in 2.9 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Cluster of Food, Nutrition, and Health Science: Beverages, Dietetics, Foods, Nutraceuticals, Nutrients and Obesities.
Impact Factor:
1.3 (2024);
5-Year Impact Factor:
1.2 (2024)
Latest Articles
The Relationship of Education Level, Lifestyle, and Personality to BMI and Obesity Differs Between Men and Women
Obesities 2025, 5(4), 69; https://doi.org/10.3390/obesities5040069 - 26 Sep 2025
Abstract
►
Show Figures
Obesity has become a major global health concern, but few studies have examined the determinants of body mass index (BMI, kg/m2) and overweight/obesity (BMI ≥ 25) specifically in women. This study investigated the roles of education, lifestyle, and personality using data
[...] Read more.
Obesity has become a major global health concern, but few studies have examined the determinants of body mass index (BMI, kg/m2) and overweight/obesity (BMI ≥ 25) specifically in women. This study investigated the roles of education, lifestyle, and personality using data from a questionnaire survey of 4276 Japanese adults (2215 women and 2061 men) aged 30–79 years. Multiple regression and logistic regression analyses were conducted to identify factors associated with BMI (continuous) and obesity (BMI ≥ 25) in women. The multiple regression results indicated that educational attainment, rest, diet, and conscientiousness were negatively associated with BMI, whereas extraversion and openness were positively associated with BMI. Logistic regression further showed that higher education, regular exercise, sufficient rest, and conscientiousness were associated with non-obesity (BMI < 25), while openness was associated with obesity (BMI ≥ 25). To our knowledge, this is the first study to identify determinants of BMI and obesity in women with a simultaneous focus on education, lifestyle, and personality traits.
Full article
Open AccessSystematic Review
The Combined Effect of the Mediterranean Diet and Physical Activity on the Components of Metabolic Syndrome in Adults: A Systematic Review of Randomised Controlled Trials
by
Luiza Teixeira, Diogo Monteiro, Rui Matos, Raúl Antunes and Miguel Jacinto
Obesities 2025, 5(4), 68; https://doi.org/10.3390/obesities5040068 - 25 Sep 2025
Abstract
►▼
Show Figures
Metabolic syndrome (MetS) is a global public health challenge, characterized by the coexistence of cardiometabolic risk factors such as abdominal obesity, dyslipidaemia, hypertension, and insulin resistance. Non-pharmacological strategies, including the Mediterranean diet (MD) and physical activity (PA), have been widely studied for their
[...] Read more.
Metabolic syndrome (MetS) is a global public health challenge, characterized by the coexistence of cardiometabolic risk factors such as abdominal obesity, dyslipidaemia, hypertension, and insulin resistance. Non-pharmacological strategies, including the Mediterranean diet (MD) and physical activity (PA), have been widely studied for their potential to prevent and manage MetS. This systematic review aimed to synthesize the evidence on the combined effect of MD and PA on MetS components in adults, based on randomized controlled trials (RCTs). Twenty-two RCTs published between 2018 and 2024 were included, involving 11,478 participants. The interventions ranged from 8 weeks to 3 years and combined adapted or hypocaloric MDs with moderate-to-high-intensity PA, typically including walking, aerobic exercise, or high-intensity interval training (HIIT), performed 3 to 7 times per week. The combined interventions resulted in reductions in body weight (−2.5 to −7.2 kg), body mass index (−0.7 to −2.2 kg/m2), waist circumference (−5.1 to −7.8 cm), and blood pressure (up to −9.0 mmHg systolic and −6.7 mmHg diastolic). Improvements in HDL cholesterol, triglyceride levels, and insulin sensitivity were also observed. These findings suggest that integrated interventions based on the Mediterranean lifestyle are effective in reducing MetS components and may support future public health strategies.
Full article

Figure 1
Open AccessArticle
Supplementation Effects of Hibiscus sabdariffa L. Flower Aqueous Extract on Body Composition and Metabolism in Eutrophic and Obese Rats
by
João Fernando Bernardo da Costa, Alana Louzada Millions Monteiro, Bruna Almeida Nascimento, Clarice Maia Vinagre de Oliveira, Karen Pereira Coutinho, Anderson Junger Teodoro, Barbara Elisabeth Teixeira-Costa and Mariana Sarto Figueiredo
Obesities 2025, 5(4), 67; https://doi.org/10.3390/obesities5040067 - 25 Sep 2025
Abstract
Obesity is a chronic, multifactorial disease characterized by excess body fat and is a major risk factor for various metabolic disorders. Bioactive compounds from the diet have been recognized for their role in preventing chronic non-communicable diseases and as adjuvants in managing endocrine–metabolic
[...] Read more.
Obesity is a chronic, multifactorial disease characterized by excess body fat and is a major risk factor for various metabolic disorders. Bioactive compounds from the diet have been recognized for their role in preventing chronic non-communicable diseases and as adjuvants in managing endocrine–metabolic dysfunctions. Hibiscus sabdariffa L. (HSL) is rich in bioactive compounds with antioxidant, antihypertensive, and antihyperlipidemic properties. This study evaluated the effects of HSL flower extract supplementation on body composition, lipid profile, and biochemical parameters in both eutrophic and high-fat diet-induced obese rats. Thirty-two Wistar rats were assigned to four groups: control, control plus HSL extract, high-fat diet, and high-fat diet plus HSL extract. The extract was administered orally at 150 mg kg−1 for thirty days. Dual-energy X-ray absorptiometry revealed that HSL supplementation significantly attenuated fat mass gain (from 98 g to 75 g) and adiposity indices (10.23 to 8.86) in obese rats without altering total body mass. Moreover, the HSL extract improved lipid profiles by reducing LDL cholesterol from 23 to 13 mg dL−1 and exhibited potential hepatoprotective effects linked with decreased ALT (40 to 26.7 U L−1) and total bilirubin (0.12 to 0.07 mg dL−1) levels. Although glucose metabolism parameters had no significant differences, a trend toward improved insulin sensitivity was observed. These results suggest that the aqueous HSL extract may exert cardioprotective, hepatoprotective, and anti-obesity effects, supporting its potential as a complementary therapeutic agent in obesity and related metabolic disorders.
Full article
(This article belongs to the Special Issue The Impact of Food Compounds on Obesity Mechanisms)
►▼
Show Figures

Figure 1
Open AccessArticle
Cross-European Patterns of Obesity: Where Does Croatia Stand?—Descriptive Analysis of Waves 2015–2022 of the Survey of Health, Ageing and Retirement in Europe (SHARE) Including Adults Aged Over 50
by
Manuela Maltarić, Mirela Kolak, Branko Kolarić, Darija Vranešić Bender and Jasenka Gajdoš Kljusurić
Obesities 2025, 5(3), 66; https://doi.org/10.3390/obesities5030066 - 18 Sep 2025
Abstract
►▼
Show Figures
This paper investigates the prevalence of obesity and its links to health and dietary habits in middle-aged and older populations in Europe (50+), with a particular focus on Croatia. In Croatia, only 33.9% of adults have a normal BMI, while almost two-thirds (64.8%)
[...] Read more.
This paper investigates the prevalence of obesity and its links to health and dietary habits in middle-aged and older populations in Europe (50+), with a particular focus on Croatia. In Croatia, only 33.9% of adults have a normal BMI, while almost two-thirds (64.8%) are classified as overweight or obese, placing Croatia among the EU countries with the highest prevalence of overweight. Obesity significantly increases the risk of serious health complications, including cardiovascular disease (CVD) and type 2 diabetes. Therefore, we used data from the SHARE (Survey of Health, Ageing and Retirement in Europe), for the last four waves (wave 6–wave 9). The nutritional status was investigated (using the body mass index, BMI) as well as its relationship with cardiovascular disease and dietary habits. Different BMI categorizations were used (i) for the population under and (ii) over 65 years of age, and the results show that a significant proportion of the middle-aged and older European population is overweight or obese. When it comes to dietary habits, statistically significant differences in meat, fish, or chicken consumption were noted (p < 0.001): the Croatian population, especially men, consumes them significantly more often on a daily basis compared to the EU average. Similar patterns of dairy, legumes/eggs, and fruit/vegetable consumption were observed between the EU and Croatia, although there are some statistically significant differences in daily dairy consumption among the older population and in consumption of legumes/eggs and fruit/vegetables 3–6 times a week among the older population. The prevalence of CVD generally increases with increasing BMI in both regions and age groups. However, Croatia has a statistically significantly lower prevalence of high cholesterol compared to the EU in both age groups. Also, the trend of diabetes is more pronounced in the middle-aged population in Croatia compared to the EU. These results indicate specific differences in dietary habits and the association of BMI with certain CVDs in Croatia compared to the European Union average.
Full article

Figure 1
Open AccessArticle
Associations Between Occupational Stress, Disordered Eating, and Obesity Among Police Officers in North Carolina
by
Ya-Ke Wu and Hanxin Liu
Obesities 2025, 5(3), 65; https://doi.org/10.3390/obesities5030065 - 15 Sep 2025
Abstract
Obesity is a major public health concern among police officers, yet the links between occupational stress, disordered eating, and obesity remain unclear. This cross-sectional study examined 496 North Carolina officers to (1) assess severity of occupational stress (posttraumatic stress disorder [PTSD] symptoms, anti-police
[...] Read more.
Obesity is a major public health concern among police officers, yet the links between occupational stress, disordered eating, and obesity remain unclear. This cross-sectional study examined 496 North Carolina officers to (1) assess severity of occupational stress (posttraumatic stress disorder [PTSD] symptoms, anti-police sentiment, fear of victimization), disordered eating (binge eating and loss-of-control eating), and obesity by county type, region, and sex; (2) evaluate associations between occupational stress and disordered eating; and (3) explore relationships between disordered eating and weight-related measures. Officers completed online surveys, and trained staff measured body mass index (BMI), waist and hip circumferences, and waist-to-hip ratio. Nearly 60 percent of officers were classified as obese (BMI ≥ 30 kg/m2), and over 20 percent reported moderate to severe binge eating. Rural officers reported higher PTSD symptoms, binge eating, and loss-of-control eating than those in urban or suburban areas. Coastal Plain and Piedmont officers had higher BMI and larger waist and hip circumferences than those in the Mountain region. Higher occupational stress was linked to more severe disordered eating, which was associated with greater BMI and adiposity, although the effect sizes were modest. Findings support targeted interventions addressing occupational stress and disordered eating to prevent obesity and enhance officer well-being.
Full article
Open AccessReview
Obesity–Housing Nexus: An Integrative Conceptualization of the Impact of Housing and Built Environment on Obesity
by
Kritika Rana and Ritesh Chimoriya
Obesities 2025, 5(3), 64; https://doi.org/10.3390/obesities5030064 - 20 Aug 2025
Abstract
►▼
Show Figures
Obesity has emerged as one of the most significant public health challenges of the 21st century, with its prevalence increasing at an alarming rate globally. While individual factors such as diet and physical inactivity are well-known contributors, the built environment, particularly housing, plays
[...] Read more.
Obesity has emerged as one of the most significant public health challenges of the 21st century, with its prevalence increasing at an alarming rate globally. While individual factors such as diet and physical inactivity are well-known contributors, the built environment, particularly housing, plays a critical yet understudied role in shaping obesity-related behaviors. This study examines the multilayered relationship between housing and obesity, focusing on built and neighborhood environment, affordability, and the social environment. Poor housing quality, such as overcrowding and inadequate ventilation, can potentially lead to chronic stress and sedentary behaviors, while housing design influences physical activity through characteristics such as design features and outdoor spaces. Housing location affects access to amenities such as parks and healthy food options, with disparities in access contributing to obesity in low-income areas. Similarly, neighborhood walkability, influenced by infrastructure and land use, encourages active transportation and recreation. Housing affordability also impacts dietary choices and access to recreational facilities, particularly for low-income families. Moreover, the social environment within housing communities can foster or hinder healthy behaviors through social networks and community engagement. This study emphasizes the need for health-conscious urban planning and policies that address these housing-related factors to combat obesity and promote healthier lifestyles. By integrating these Obesity–Housing Nexus, policymakers can create environments that support physical activity, healthy eating, as well as overall health and well-being.
Full article

Figure 1
Open AccessArticle
“Super-Responders” to Liraglutide Monotherapy and the Growing Evidence of Efficacy of GLP-1 Analogues in Obesity Management: A Longitudinal Prospective Cohort Study
by
Ellina Lytvyak, Eduardo Grunvald, Devika Shreekumar, Peter Rye, Olexandr Troshyn, Sarah Cawsey, Aldo J. Montano-Loza, Arya M. Sharma and Renuca Modi
Obesities 2025, 5(3), 63; https://doi.org/10.3390/obesities5030063 - 20 Aug 2025
Abstract
►▼
Show Figures
Aims: Individual weight loss results achieved with Glucagon-like Peptide-1 receptor agonists (GLP-1RA) vary significantly. Our aim was to describe the characteristics of patients with obesity who achieved ≥ 20% total weight loss (TWL) on liraglutide and appraise those findings through the prism
[...] Read more.
Aims: Individual weight loss results achieved with Glucagon-like Peptide-1 receptor agonists (GLP-1RA) vary significantly. Our aim was to describe the characteristics of patients with obesity who achieved ≥ 20% total weight loss (TWL) on liraglutide and appraise those findings through the prism of an evolving spectrum of GLP-1RA. Methods: This longitudinal prospective cohort study included 21 patients (90.5% females, age 50 (IQR 17) years, class II/III obesity (Body Mass Index ≥ 35 kg/m2) followed at the Edmonton Adult Bariatric Clinic for 65.1 (IQR 15.5) weeks. All patients received treatment with liraglutide 3.0 mg subcutaneously daily along with involvement in an integrated lifestyle modification program. Results: Liraglutide was well-tolerated, with its benefits experienced by >90% of patients. The vast majority were consistently tracking calories (95.2%, n = 20) and protein intake (90.5%, n = 19), achieving a calorie deficit of 651 (IQR 323) kcal/day, and had their mental health conditions and psychological issues successfully managed. At 16, 26, and 52 weeks, TWL was 14.3% (IQR 3.7), 18.7% (IQR 8.8), and 25.9% (IQR 9.6), respectively (p < 0.001). Over 20% TWL was achieved by 72.2% of patients by week 52. Conclusions: A select number of patients with obesity will attain weight loss that rivals bariatric surgery using liraglutide monotherapy. Despite liraglutide being less effective compared to newer agents on the market, some individuals will respond strongly and should be considered when other therapies are inaccessible. Given the societal burden and numerous challenges faced by people with obesity, GLP-1RA should be pursued in clinical practice to assist in achieving weight loss goals while being convenient and safe.
Full article

Figure 1
Open AccessArticle
Adherence to the Mediterranean Diet and Carotid Intima-Media Thickness in University Students: A Cross-Sectional Study
by
Sónia Mateus, Ana Miguel Amaral, Patrícia Coelho and Francisco Rodrigues
Obesities 2025, 5(3), 62; https://doi.org/10.3390/obesities5030062 - 18 Aug 2025
Abstract
Introduction: Subclinical atherosclerosis is increasingly recognized in younger populations, often progressing silently until the onset of overt cardiovascular events. Carotid intima-media thickness (CIMT) is a validated, non-invasive biomarker of early vascular alterations. Although the Mediterranean diet (MD) is well established as cardioprotective, its
[...] Read more.
Introduction: Subclinical atherosclerosis is increasingly recognized in younger populations, often progressing silently until the onset of overt cardiovascular events. Carotid intima-media thickness (CIMT) is a validated, non-invasive biomarker of early vascular alterations. Although the Mediterranean diet (MD) is well established as cardioprotective, its relationship with CIMT in young adults remains insufficiently studied. Objective: To assess sex-specific adherence to the Mediterranean diet and its association with carotid intima-media thickness in a cohort of university students. Methods: A cross-sectional study was performed involving 60 university students (50% male, aged 17–25 years), selected through stratified probabilistic sampling. Data were collected on sociodemographic characteristics, vascular risk factors, MD adherence via the PREDIMED questionnaire, and CIMT measured using a high-resolution carotid Doppler ultrasound. Statistical analyses included chi-square tests and descriptive statistics, with significance set at ρ ≤ 0.05. Results: A notable 95% of participants showed low adherence to the Mediterranean diet. Significant sex differences in dietary patterns were identified: males consumed more red meat (ρ = 0.023), while females reported higher fish intake (ρ = 0.037). Despite behavioral risk factors, all CIMT values remained within normal ranges (≤0.9 mm). No significant association was found between MD adherence and CIMT (ρ = 0.554). Conclusion: This exploratory study reveals a high prevalence of modifiable cardiovascular risk factors, including poor dietary adherence, among young adults, despite the absence of detectable vascular structural changes. Although no significant association was found, the findings reflect the dietary and behavioral profiles of a young, low-risk population.
Full article
Open AccessArticle
Phase Angle Is Related with Visceral Obesity in Young Adults
by
Izabela Mandryk, Joanna Bonior and Magdalena Koszarska
Obesities 2025, 5(3), 61; https://doi.org/10.3390/obesities5030061 - 15 Aug 2025
Abstract
►▼
Show Figures
Obesity is a global problem, increasing interest in adipose tissue (AT) biology. One of the techniques for analyzing visceral adipose tissue (VAT) and phase angle (PhA) is bioelectrical impedance analysis (BIA). PhA is considered an indicator of cell integrity and health and can
[...] Read more.
Obesity is a global problem, increasing interest in adipose tissue (AT) biology. One of the techniques for analyzing visceral adipose tissue (VAT) and phase angle (PhA) is bioelectrical impedance analysis (BIA). PhA is considered an indicator of cell integrity and health and can be a prognostic marker in diseases and clinical conditions. The aim of the study was to assess the nutritional status and level of visceral fat area (VFA) to investigate the association between phase angle (PhA) and content of visceral adipose tissue in young adults. Our cohort consisted of 292 young adults (18–25), both sexes. Body composition was performed by the inBody 770 analyzer. We confirmed the relationship between PhA and gender (female vs. male: 5.3 vs. 6.5; p < 0.001) and BMI (female vs. male: 22.56 kg/m2 vs. 23.78 kg/m2; p = 0.013). A total of 20.2% of examined students had a VFA of more than 100 cm2 (Visceral Obesity, VO). We demonstrated a dependence between VFA and PhA value (PhA = 5.4 (VFA > 100 cm2) vs. PhA = 5.7 (VFA < 100 cm2), p = 0.003). Students with VO and normal BMI had a significantly lower PhA than those with VO and BMI ≥ 30 kg/m2 (p = 0.021). PhA may be a useful indicator for assessing nutritional status and physiological differences related to gender, BMI, and visceral obesity in young adults.
Full article

Figure 1
Open AccessArticle
Associations Between Self-Perceived Psychosocial Stress and Markers of Adiposity in Ga Mashie, Urban Ghana: Evidence from a Cross-Sectional Population-Based Survey
by
Emeline Rougeaux, Samuel Amon, Leonard Baatiema, Sandra Boatemaa Kushitor, Mawuli Komla Kushitor, Sedzro Kojo Mensah, Rolando Leiva-Granados, Akanksha A. Marphatia, Jonathan C. K. Wells, Carlos Salvador Grijalva-Eternod, Irene Akwo Kretchy and Edward Fottrell
Obesities 2025, 5(3), 60; https://doi.org/10.3390/obesities5030060 - 9 Aug 2025
Abstract
►▼
Show Figures
Prior research from Ghana suggests psychosocial stress is associated with lower body mass index (BMI) and waist circumference (WC), both markers of adiposity, contrasting with meta-analyses showing positive associations in other settings. This study aimed to explore how stress was associated with markers
[...] Read more.
Prior research from Ghana suggests psychosocial stress is associated with lower body mass index (BMI) and waist circumference (WC), both markers of adiposity, contrasting with meta-analyses showing positive associations in other settings. This study aimed to explore how stress was associated with markers of adiposity in urban Ghanaian adults. Data included 854 adults from the Contextual Awareness, Response and Evaluation Diabetes in Ghana survey carried out in November–December 2022 in Ga Mashie, a deprived area of the capital Accra. Associations between self-perceived stress (Perceived Stress Scale 10, categorized into low and average–high stress) and BMI or WC-for-height ratio (WHR) were assessed using linear regression. Results were adjusted for survey design and confounders and stratified by sex. Greater stress was associated with higher BMI and WHR in females (adjusted coeff. [95% CI]: BMI: 2.3 [0.5, 4.0], WHR: 0.03 [0.00, 0.06]). No associations were found in males. These findings highlight the need to understand the complex interactions between gender, stress, and increasing burdens of obesity and other associated non-communicable diseases in urban African settings, with a view to designing context-specific interventions to reduce risk.
Full article

Figure 1
Open AccessReview
Resetting Time: The Role of Exercise Timing in Circadian Reprogramming for Metabolic Health
by
Stuart J. Hesketh
Obesities 2025, 5(3), 59; https://doi.org/10.3390/obesities5030059 - 7 Aug 2025
Abstract
►▼
Show Figures
Circadian rhythms are intrinsic 24 h cycles that regulate metabolic processes across multiple tissues, with skeletal muscle emerging as a central node in this temporal network. Muscle clocks govern gene expression, fuel utilisation, mitochondrial function, and insulin sensitivity, thereby maintaining systemic energy homeostasis.
[...] Read more.
Circadian rhythms are intrinsic 24 h cycles that regulate metabolic processes across multiple tissues, with skeletal muscle emerging as a central node in this temporal network. Muscle clocks govern gene expression, fuel utilisation, mitochondrial function, and insulin sensitivity, thereby maintaining systemic energy homeostasis. However, circadian misalignment, whether due to behavioural disruption, nutrient excess, or metabolic disease, impairs these rhythms and contributes to insulin resistance, and the development of obesity, and type 2 diabetes mellitus. Notably, the muscle clock remains responsive to non-photic cues, particularly exercise, which can reset and amplify circadian rhythms even in metabolically impaired states. This work synthesises multi-level evidence from rodent models, human trials, and in vitro studies to elucidate the role of skeletal muscle clocks in circadian metabolic health. It explores how exercise entrains the muscle clock via molecular pathways involving AMPK, SIRT1, and PGC-1α, and highlights the time-of-day dependency of these effects. Emerging data demonstrate that optimally timed exercise enhances glucose uptake, mitochondrial biogenesis, and circadian gene expression more effectively than time-agnostic training, especially in individuals with metabolic dysfunction. Finally, findings are integrated from multi-omic approaches that have uncovered dynamic, time-dependent molecular signatures that underpin circadian regulation and its disruption in obesity. These technologies are uncovering biomarkers and signalling nodes that may inform personalised, temporally targeted interventions. By combining mechanistic insights with translational implications, this review positions skeletal muscle clocks as both regulators and therapeutic targets in metabolic disease. It offers a conceptual framework for chrono-exercise strategies and highlights the promise of multi-omics in developing precision chrono-medicine approaches aimed at restoring circadian alignment and improving metabolic health outcomes.
Full article

Figure 1
Open AccessArticle
Closing the Gap in Behavioral Weight Loss Therapy: Prospective Analysis of Clinical Real-World Data of a Four-Year Health Insurance-Financed Program
by
Sarah Victoria Frenzel, Hans-Christian Puls, Susan Vogl, Franziska Frölich, Hannes Felten, Nicole Schlenz, Michael Stumvoll, Mathias Fasshauer, Matthias Blüher, Anja Hilbert and Haiko Schlögl
Obesities 2025, 5(3), 58; https://doi.org/10.3390/obesities5030058 - 21 Jul 2025
Abstract
►▼
Show Figures
Our four-year interdisciplinary behavioral weight loss program is fully covered by public health insurance for patients with a body mass index of ≥35 kg/m2. We evaluated the real-world outcomes of anthropometric, metabolic and psychologic parameters collected prior to the start (t
[...] Read more.
Our four-year interdisciplinary behavioral weight loss program is fully covered by public health insurance for patients with a body mass index of ≥35 kg/m2. We evaluated the real-world outcomes of anthropometric, metabolic and psychologic parameters collected prior to the start (t0, n = 381, 71% women) and after each segment of the program (t1–4, n = 243, 126, 94, and 77). It is a prospective evaluation of clinical real-world data including all patients who started the first segment of behavioral treatment until they quit/finished the program. The mean dropout rates per treatment segment were 23%. Body weight after one year decreased from 127.3 kg to 122.2 (p < 0.001). Average hemoglobin A1c value decreased from 5.8% to 5.6% in all patients (p < 0.001) and from 6.6% to 6.2% in patients with type 2 diabetes (p < 0.001). Further metabolic and psychological parameters improved significantly as well. The average weight nadir was reached after two segments, co-occurring with the most beneficial changes in laboratory parameters. Afterwards, mean weight slightly increased accompanied by a discrete loss of benefits in laboratory parameters. Our real-world data with significant health improvements adds important value to discussions about the funding of obesity therapy and thus has the chance to improve therapy availability for obesity patients worldwide.
Full article

Figure 1
Open AccessArticle
A Combination of Insufficient Physical Activity and Sedentary Behavior Associated with Dynapenic Abdominal Obesity and Dynapenic Obesity in Older Adults: A Cross-Sectional Analysis
by
Lucas dos Santos, Paulo da Fonseca Valença Neto, Claudio Bispo de Almeida, Raildo da Silva Coqueiro, Douglas de Assis Teles Santos, José Ailton Oliveira Carneiro, Pabline dos Santos Santana, Elayny Lopes Costa, Lucas Lima Galvão and Cezar Augusto Casotti
Obesities 2025, 5(3), 57; https://doi.org/10.3390/obesities5030057 - 18 Jul 2025
Abstract
►▼
Show Figures
Objective: To investigate the association between combined physical activity (PA) levels and sedentary behavior (SB) with dynapenic abdominal obesity (DAO) and dynapenic obesity (DO) in older adults. Methods: This cross-sectional, population-based epidemiological study included 207 community-dwelling older adults (58.90% women). PA and SB
[...] Read more.
Objective: To investigate the association between combined physical activity (PA) levels and sedentary behavior (SB) with dynapenic abdominal obesity (DAO) and dynapenic obesity (DO) in older adults. Methods: This cross-sectional, population-based epidemiological study included 207 community-dwelling older adults (58.90% women). PA and SB were assessed using the International Physical Activity Questionnaire. Participants were categorized into four groups: (G1) sufficiently active and low SB; (G2) sufficiently active and high SB; (G3) insufficiently active and low SB; and (G4) insufficiently active and high SB. DAO and DO were defined as the coexistence of dynapenia with abdominal and general obesity, respectively. Prevalence ratios (PR) and 95% confidence intervals (CI) were estimated using Poisson regression with robust variance. Results: The prevalence of DAO was 11.10% and DO was 6.80%. In the adjusted analysis, participants classified as insufficiently active with high SB (G4) had 5.54 times the prevalence of DAO (PR: 5.54, 95% CI: 1.91–16.03) and 6.54 times the prevalence of DO (PR: 6.54, 95% CI: 1.68–36.66) compared to the reference group (G1) (sufficiently active and low SB). Conclusions: Insufficient PA combined with high SB was positively associated with both DAO and DO in the studied population of older adults.
Full article

Figure 1
Open AccessArticle
Diet Therapy Improves Body Composition, Blood Pressure and Glycemic Status in Individuals Living with Type 2 Diabetes: A Prospective Cohort Study
by
Collins Afriyie Appiah, Harriet Wugah, Janet Adede Carboo, Mary Amoako, Michael Akenteng Wiafe and Frank Ekow Atta Hayford
Obesities 2025, 5(3), 56; https://doi.org/10.3390/obesities5030056 - 17 Jul 2025
Abstract
►▼
Show Figures
Westernization of traditional diets has been implicated in the rising burden of overweight/obesity and type 2 diabetes, especially in developing countries. In recent times, diet therapy is increasingly being recognized as an essential component of diabetes care. This study assessed the effect of
[...] Read more.
Westernization of traditional diets has been implicated in the rising burden of overweight/obesity and type 2 diabetes, especially in developing countries. In recent times, diet therapy is increasingly being recognized as an essential component of diabetes care. This study assessed the effect of diet therapy on body composition, antioxidant nutrient intake, and glycemic status in individuals living with type 2 diabetes (ILWT2D). In this prospective observational cohort study, 45 ILWT2D who were receiving diet therapy (personalized dietary counseling) in addition to standard medical treatment (intervention group) were compared with 45 ILWT2D receiving only standard medical treatment (comparator group). Antioxidant micronutrient intake was assessed using a 24-h dietary recall. Body composition indices, including body mass index (BMI), percentage body fat (%BF), and visceral fat (VF), were assessed. Participants’ fasting blood glucose (FBG), glycated hemoglobin (HbA1C) levels, and blood pressure (BP) were measured. All measurements were performed before and after a three-month period. There were significant improvements in BMI (27.8 ± 6.0 kg/m2 vs. 26.9 ± 5.5 kg/m2, p = 0.003), %BF (37.8 ± 11.9% vs. 35.5 ± 10.5%, p < 0.001), visceral fat (9.8 ± 3.4 vs. 9.1 ± 3.2, p < 0.001), systolic BP (136.9 ± 19.9 mmHg vs. 124.6 ± 13.0 mmHg, p < 0.001), FBG (8.8 ± 2.8 mmol/L vs. 6.7 ± 1.5 mmol/L, p < 0.001), and HbA1c (7.3 ± 1.0% vs. 6.4 ± 0.8%, p < 0.001) in the intervention group from baseline to endline, but not in the comparator group. In contrast, %BF increased within the comparator group (39.9 ± 7.8 vs. 40.7 ± 7.4; p = 0.029). Vitamin A intake increased significantly (227.5 ± 184.3 µg vs. 318.8 ± 274.7 µg, p = 0.038) within the intervention group but not in the comparator group (174.9 ± 154.3 µg, 193.7 ± 101.4 µg, p = 0.54). There were no significant changes in zinc, copper, selenium, and vitamin C intakes (p > 0.05) in the intervention group from the baseline to endline, unlike those in the comparator group who showed a significant increase in the intake of these nutrients. There was a significant increase in vitamin A intake among the ILWT2D who received dietary counseling as an intervention compared to those who did not. Additionally, the ILWT2D who received dietary counseling had significant improvements in their body composition (BMI, body fat, and visceral fat) and systolic blood pressure, compared to those who did not. The ILWT2D who received the intervention had significantly better glycemic control (FBG and HbA1c) than their counterparts who did not. Thus, this study suggests the potential of diet therapy as a viable non-pharmacological treatment approach for individuals living with type 2 diabetes.
Full article

Figure 1
Open AccessArticle
Cross-Sectional Analysis of Food Group Consumption and Obesity in Children Aged 6–23 Months with Normal and Stunted Growth Patterns in Pakistan
by
Asif Khaliq, Izzan Ahmed Usmani, Yusra Rizwan, Mishaim Khan, Akif Shahid Khan, Noor ul Ain Saleem and Muhammad Junaid
Obesities 2025, 5(3), 55; https://doi.org/10.3390/obesities5030055 - 16 Jul 2025
Abstract
►▼
Show Figures
Background: Worldwide, the awareness about childhood obesity as a public health concern is increasing, particularly in developing countries like Pakistan. Obesity during early childhood may persist into later ages, increasing the risk of chronic illnesses such as diabetes and hypertension. Objective: The aim
[...] Read more.
Background: Worldwide, the awareness about childhood obesity as a public health concern is increasing, particularly in developing countries like Pakistan. Obesity during early childhood may persist into later ages, increasing the risk of chronic illnesses such as diabetes and hypertension. Objective: The aim of this study was to examine the relationship of different types of food groups with obesity among children with normal and stunted growth trajectories in Pakistan. Methods: This cross-sectional study conducted a secondary analysis of Pakistan Demographic and Health Surveys (PDHSs) conducted in the years 2012–2013 and 2017–2018. Data of 1230 healthy and obese children with either normal or stunted growth were analysed after excluding those who were aged below six months, wasted, underweight, or had missing anthropometric or dietary data. The relationship of different food groups with obesity among the children with normal and stunted growth was analysed by bivariate logistic regression. Results: The prevalence of paediatric obesity dropped from 7.3% in 2012–2013 to 2.4% in 2017–2018. However, the coexistence of stunting with obesity—termed the nutritional paradox—slightly increased from 2.8% in 2012–2013 to 3% in 2017–2018. Among the different food groups, the continuation of breastmilk was associated with lowering the odds of obesity by 69% (25% to 88%) among children with normal growth. Conversely, among children with stunted growth, the continuation of breastmilk was associated with an increase in the odds of obesity by 3.71 (1.08 to 12.62) times. Conclusion: Despite the 4.9% reduction in paediatric obesity, cases of the nutritional paradox are still escalating in Pakistan. This reflects an urgent need for targeted nutritional interventions to mitigate the impact of obesogenic diets and reduce the prevalence of childhood obesity in Pakistan.
Full article

Figure 1
Open AccessArticle
Influences of Sex and BMI on Body Image, Weight Bias, Disordered Eating, and Psychological Well-Being: A Multivariate Analysis
by
Marios Argyrides, Lina Efthyvoulou, Konstantina Zamba, Elly Anastasiades and Zoe Charalambous
Obesities 2025, 5(3), 54; https://doi.org/10.3390/obesities5030054 - 11 Jul 2025
Cited by 1
Abstract
Body image and mental health outcomes are influenced by both sex and body weight. This study investigated how sex and BMI category (participants classified with healthy weight, overweight, or with obesity) relate to body image, disordered eating, weight bias, global self-esteem and depression.
[...] Read more.
Body image and mental health outcomes are influenced by both sex and body weight. This study investigated how sex and BMI category (participants classified with healthy weight, overweight, or with obesity) relate to body image, disordered eating, weight bias, global self-esteem and depression. Participants (N = 642; 278 (43.3%) males; 364 females (56,7%)) provided self-report measures of appearance satisfaction, body appreciation, overweight preoccupation, disordered eating scores, weight bias, depression, and self-esteem. The results indicated that women and participants classified with overweight and obesity based on BMI categories reported lower appearance satisfaction and body appreciation and a higher preoccupation with overweight and depression. Interaction effects showed that women participants with overweight and obesity reported particularly low appearance satisfaction and body appreciation. Individuals classified with healthy BMI category reported higher disordered eating scores than those classified with overweight. No significant effects were found for global self-esteem. These findings suggest that sex and BMI contribute to the study’s variables of interest, with some effects more pronounced in women with a higher BMI. The results align with sociocultural theories of appearance pressure but indicate complexity in disordered eating patterns. The findings underscore the importance of adopting intersectional, weight-inclusive, and sex-responsive approaches in both research and clinical practice.
Full article
Open AccessArticle
Participant Experiences of Cognitive Remediation Therapy for Obesity (CRT-O): A Qualitative Thematic Analysis
by
Jayanthi Raman, Priyanka Thapliyal, Evelyn Smith, Aparna Anoop and Phillipa Hay
Obesities 2025, 5(3), 53; https://doi.org/10.3390/obesities5030053 - 9 Jul 2025
Abstract
►▼
Show Figures
Objective: The present study is a qualitative analysis of participant experiences and perspectives from people who received cognitive remediation therapy for adult obesity (CRT-O). Method: Post-intervention data were generated from an open-ended question requesting the participants to write, in the form of a
[...] Read more.
Objective: The present study is a qualitative analysis of participant experiences and perspectives from people who received cognitive remediation therapy for adult obesity (CRT-O). Method: Post-intervention data were generated from an open-ended question requesting the participants to write, in the form of a letter to their therapist, about their experiences and reflections upon taking part in cognitive remediation therapy for adult obesity. Participants’ letters were thematically analyzed. Results: Four themes and nested subthemes emerged from participant responses, including (1) motivation and initial response to CRT-O for the adult obesity study eligibility process with the nested subthemes of initial apprehension pre-intervention and awareness and acknowledgement of one’s problematic eating behaviors; (2) perceived benefits from cognitive remediation therapy for adult obesity with the nested subthemes of the strategies and techniques that were found beneficial and the role of the cognitive remediation therapy for adult obesity therapists in facilitating positive change; (3) perceived outcomes post-intervention with the nested subthemes of changed relationship with food, self-acceptance and gaining control to effect positive lifestyle change; and (4) expectations and beliefs about the longer-term impact of cognitive remediation therapy for adult obesity with the nested subthemes of using the cognitive remediation therapy for adult obesity strategies as a lifestyle routine, apprehension about not having follow-up therapist support, and concern about potential relapse. Conclusion: Our analysis found helpful insights into the consumer perception of this novel intervention and highlighted the clinical utility of implementing cognitive remediation therapy in those living with a higher body weight.
Full article
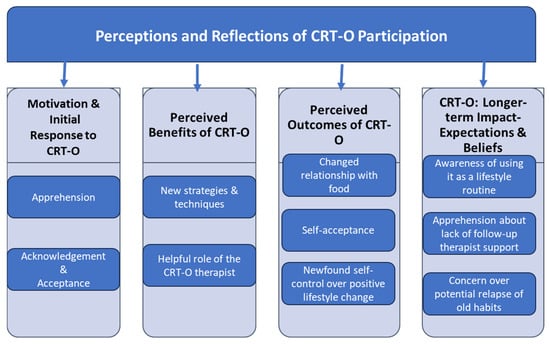
Figure 1
Open AccessArticle
Trends and Subgroup Comparisons of Obesity and Severe Obesity Prevalence Among Mississippi Adults, 2011–2021
by
Stephanie McLeod, Xiaoshan Z. Gordy, Jana Bagwell, Christina Ferrell, Jerome Kolbo and Lei Zhang
Obesities 2025, 5(3), 52; https://doi.org/10.3390/obesities5030052 - 4 Jul 2025
Abstract
►▼
Show Figures
Mississippi has long been one of the most obese states in the U.S., with its obesity rates consistently exceeding the national average. The state’s severe obesity rate is also among the highest in the nation. This study utilized the 2011 to 2021 data
[...] Read more.
Mississippi has long been one of the most obese states in the U.S., with its obesity rates consistently exceeding the national average. The state’s severe obesity rate is also among the highest in the nation. This study utilized the 2011 to 2021 data from the Mississippi Behavioral Risk Factor Surveillance System (BRFSS) to conduct a comprehensive analysis of obesity and severe obesity trends in Mississippi by sex, age, and race and ethnicity. The data set included a BMI variable calculated by using self-reported height and weight, which the authors categorized into two obesity classification groups—obesity (BMI: 30.00 to 39.99) and severe obesity (BMI: 40.00 or greater)—and demographic characteristics such as sex, age, race and ethnicity. The data were analyzed using SAS 9.4 software to account for the complex design. Weighted prevalence estimates and associated standard errors (SEs) for obesity and severe obesity were calculated. Changes in the prevalence over time were assessed using logistic regression models. The prevalence estimates and SEs were exported to Joinpoint software to calculate the annual percentage change (APC) and associated 95% confidence intervals (CIs) and p-values for the trends. Our analysis of the data revealed a consistent increase in severe obesity, regardless of age, sex, or race. A concerning trend exists where individuals are moving from the obese category to the severely obese category, indicating a worsening trend in overall weight status. This is likely to accelerate the development of chronic disease and, hence, place additional strain on an economically disadvantaged state. Future research should explore the underlying drivers of this shift, including biological, behavioral, and socioeconomic factors, while also evaluating the effectiveness of existing obesity prevention and treatment programs.
Full article

Figure 1
Open AccessBrief Report
Multicomponent-Type High-Intensity Interval Training Improves Vitamin D Status in Adults with Overweight/Obesity
by
Maria Protopapa, Dimitrios Draganidis, Alexandra Avloniti, Ioannis G. Fatouros, Theodoros Stampoulis, Dimitrios Pantazis, Dimitrios Balampanos, Nikolaos Orestis Retzepis, Athanasios Poulios, Nikolaos Zaras, Maria Bampali, Ioannis Karakasiliotis, George Mastorakos, Theodore J. Angelopoulos, Maria Michalopoulou, Antonis Kambas, Athanasios Z. Jamurtas and Athanasios Chatzinikolaou
Obesities 2025, 5(3), 51; https://doi.org/10.3390/obesities5030051 - 4 Jul 2025
Abstract
►▼
Show Figures
Vitamin D deficiency is highly prevalent in individuals with overweight/obesity and this can be largely attributed to the entrapment of VitD in adipose tissue due to impaired lipolytic stimulation. Considering the well-described role of exercise in stimulating lipolysis, the present study investigated the
[...] Read more.
Vitamin D deficiency is highly prevalent in individuals with overweight/obesity and this can be largely attributed to the entrapment of VitD in adipose tissue due to impaired lipolytic stimulation. Considering the well-described role of exercise in stimulating lipolysis, the present study investigated the efficacy of multicomponent-type high-intensity interval training (m-HIIT) in increasing 25-hydroxyvitamin D [25(OH)D] levels in males with overweight/obesity. Twenty middle-aged males (43.5 ± 5 years, BMI: 30.7 ± 3.3 kg/m2) participated in three weekly supervised m-HIIT sessions over a 12-week period and underwent assessments at baseline, 6, and 12 weeks. Primary outcomes were total body fat mass, android fat, hepatorenal index, and serum 25(OH)D. Participants’ daily physical activity and dietary intake habits remained unaltered throughout the 12-week training period. The m-HIIT intervention reduced fat mass (by 3% at 12 weeks), android fat (by 3.7% at 6 weeks and 4.4% at 12 weeks), and hepatorenal index (by 8% at 12 weeks). Serum 25(OH)D levels increased by ~14% (+3.21 ng/mL, p = 0.002) and ~31% (+7.24 ng/mL, p < 0.001) at 6 and 12 weeks, respectively. The elevation of 25(OH)D levels at 12 weeks was inversely related to fat mass loss (R = 0.53, p = 0.016). Plasma SGPT, SGOT, ALP, γ-GT, fetuin-A, and calcium levels remained unaltered after the 12-week training period. In conclusion, m-HIIT may be useful as a non-pharmacological intervention to increase circulating VitD levels in adults with overweight/obesity.
Full article
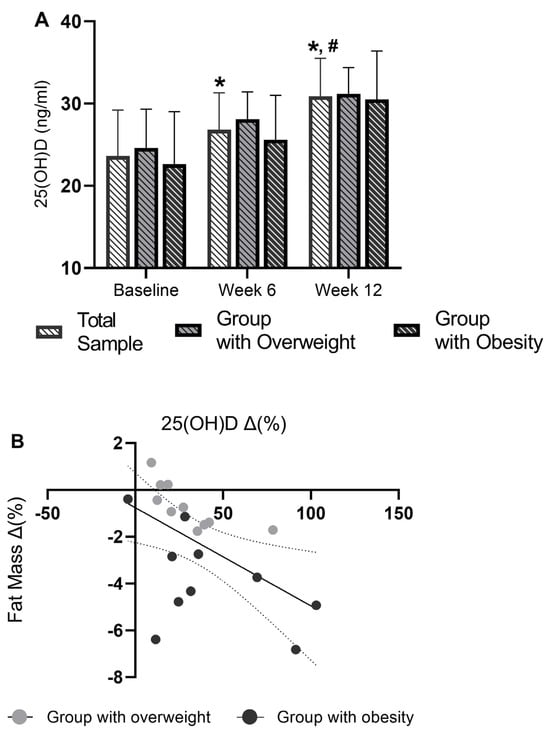
Figure 1
Open AccessArticle
Investigating Environmental and Socioeconomic Contributors to Adult Obesity in the Rio Grande Valley
by
John Nicholas Cauba, Jihoo Woo, Russell W. Wiggins and Shizue Mito
Obesities 2025, 5(3), 50; https://doi.org/10.3390/obesities5030050 - 1 Jul 2025
Abstract
►▼
Show Figures
Obesity in the Rio Grande Valley (RGV) of Texas remains a critical public health concern, with rates (46.9%) significantly exceeding those of Texas (36%) and the U.S. (34%) (p < 0.001). This study used 2024 County Health Rankings data to analyze environmental
[...] Read more.
Obesity in the Rio Grande Valley (RGV) of Texas remains a critical public health concern, with rates (46.9%) significantly exceeding those of Texas (36%) and the U.S. (34%) (p < 0.001). This study used 2024 County Health Rankings data to analyze environmental and socioeconomic contributors to obesity across 240 Texas counties, with a population-weighted focus on Hidalgo, Cameron, Starr, and Willacy counties. The RGV exhibited markedly poorer access to exercise, higher rates of physical inactivity, lower Food Environment Index scores (FEI = 4.3 vs. 5.7 in Texas), higher rates of uninsurance, worse patient-to–primary care physician (PCP) ratios (2152:1 vs. Texas 1660:1), and increased preventable hospitalizations. Multiple linear regression identified physical inactivity (β = 0.6, p = 0.01) and access to exercise (β = −0.02, p = 0.02) as significant predictors of obesity. Notably, higher uninsured rates were associated with lower reported obesity, likely due to underdiagnosis in the absence of routine care. These findings emphasize the need for targeted interventions addressing food access, environmental and recreational infrastructure, along with healthcare infrastructure in the RGV, where socioeconomic disadvantage and structural barriers magnify the impact of national obesity trends on the regional level.
Full article
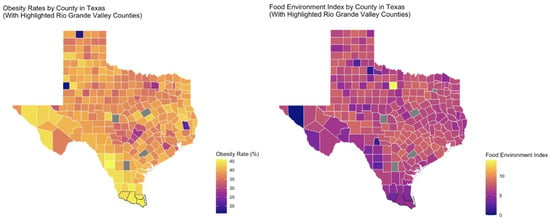
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
3 September 2025
Join Us at the MDPI at the University of Toronto Career Fair, 23 September 2025, Toronto, ON, Canada
Join Us at the MDPI at the University of Toronto Career Fair, 23 September 2025, Toronto, ON, Canada

1 September 2025
MDPI INSIGHTS: The CEO’s Letter #26 – CUJS, Head of Ethics, Open Peer Review, AIS 2025, Reviewer Recognition
MDPI INSIGHTS: The CEO’s Letter #26 – CUJS, Head of Ethics, Open Peer Review, AIS 2025, Reviewer Recognition
Topics
Topic in
Behavioral Sciences, Children, Healthcare, IJERPH, JFMK, Obesities
The Effect of Physical Activity on the Population's Health
Topic Editors: Stefania Paduano, Federica ValerianiDeadline: 31 August 2026
Topic in
Geriatrics, IJMS, Life, Sports, Neurology International, Obesities
Exercise and Human Aging: Physiological and Psychological Functions
Topic Editors: Samuel Da Silva Aguiar, Ismael Perez-SuarezDeadline: 20 September 2026
Topic in
Nutrients, Metabolites, Healthcare, Children, Obesities, Life
Non-Communicable Diseases Silent Killer: Metabolic and Obesity Risks of Sedentary Behaviors
Topic Editors: Kotsedi Daniel Monyeki, Machoene Derrick SekgalaDeadline: 30 September 2026
Topic in
Dietetics, Nutrients, Obesities, Diseases, IJMS, Metabolites
Dietary Habits in Liver Health and Disease: Preclinical and Clinical Studies
Topic Editors: Evelyn Nunes Goulart Da Silva Pereira, Rosane Harter Griep, Anissa DaliryDeadline: 31 December 2026

Conferences
Special Issues
Special Issue in
Obesities
The Impact of Food Compounds on Obesity Mechanisms
Guest Editor: Nobuyuki TakahashiDeadline: 30 November 2025
Special Issue in
Obesities
How to Prevent Obesity and Inflammatory Disease 2025
Guest Editor: Sara BaldassanoDeadline: 31 December 2025
Special Issue in
Obesities
Obesity in the 21st Century: Public Health Perspectives and Population Solutions
Guest Editors: Ritesh Chimoriya, Kritika RanaDeadline: 31 March 2026
Special Issue in
Obesities
Obesity and Its Comorbidities: Prevention and Therapy 2026
Guest Editor: Carmine FinelliDeadline: 30 June 2026








