Abstract
Objective: To investigate the association between combined physical activity (PA) levels and sedentary behavior (SB) with dynapenic abdominal obesity (DAO) and dynapenic obesity (DO) in older adults. Methods: This cross-sectional, population-based epidemiological study included 207 community-dwelling older adults (58.90% women). PA and SB were assessed using the International Physical Activity Questionnaire. Participants were categorized into four groups: (G1) sufficiently active and low SB; (G2) sufficiently active and high SB; (G3) insufficiently active and low SB; and (G4) insufficiently active and high SB. DAO and DO were defined as the coexistence of dynapenia with abdominal and general obesity, respectively. Prevalence ratios (PR) and 95% confidence intervals (CI) were estimated using Poisson regression with robust variance. Results: The prevalence of DAO was 11.10% and DO was 6.80%. In the adjusted analysis, participants classified as insufficiently active with high SB (G4) had 5.54 times the prevalence of DAO (PR: 5.54, 95% CI: 1.91–16.03) and 6.54 times the prevalence of DO (PR: 6.54, 95% CI: 1.68–36.66) compared to the reference group (G1) (sufficiently active and low SB). Conclusions: Insufficient PA combined with high SB was positively associated with both DAO and DO in the studied population of older adults.
1. Introduction
Abdominal obesity and general obesity are characterized by excessive fat accumulation in the central trunk and overall body adipose tissue, respectively [1]. These conditions are prevalent among older adults [2], partly due to age-related hormonal changes, such as decreased estrogen and progesterone in women and declining testosterone in men [3].
Dynapenia, another condition common in older adults, results from natural aging processes [4]. It is defined by muscle weakness primarily stemming from neuromuscular alterations, including reductions in muscle fiber number and cross-sectional area, and a diminished ability to activate and recruit motor units [3,4]. The simultaneous occurrence of obesity and dynapenia leads to dynapenic abdominal obesity (DAO) [5,6] and dynapenic obesity (DO) [7,8]. Epidemiological studies among older adults have reported DAO prevalence rates ranging from 6.10% [5] to 10.76% [6] and DO prevalence rates from 6.16% [8] to 24.10% [7].
This epidemiological scenario presents a significant challenge for geriatric healthcare, as DAO and DO are associated with an increased probability of reduced mobility, slow gait speed [6], and dependency when performing daily activities [5]. Furthermore, the co-occurrence of obesity and dynapenia is linked to heightened risks of falls and fractures [7], cardiometabolic diseases [9], and mortality [10].
Insufficient physical activity (PA) and prolonged sedentary behavior (SB) appear to exacerbate the physiological effects of aging [11]. Both behaviors are independently associated with dynapenia [12] and obesity [13] in older adults. Consequently, it is plausible to hypothesize that the combination of insufficient PA and high SB is associated with an increased likelihood of DAO and DO. However, despite the recognized independent associations, a notable gap exists in epidemiological research specifically investigating the combined effect of insufficient PA and high SB on DAO and DO in older adults.
Addressing this gap through population-based health surveys is crucial, as findings can inform health surveillance actions and facilitate more targeted interventions by elucidating the impact of these behavioral patterns on the physical performance and nutritional status of older populations. Therefore, this study aimed to investigate the association between combined PA levels and SB with DAO and DO in older adults.
2. Materials and Methods
2.1. Study Design, Setting, and Population
This cross-sectional, population-based epidemiological study was conducted following a census approach and adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [14]. Data collection involved the complete enumeration of older adults residing in the urban area of Aiquara, a municipality in the South-Central territory of Bahia state, Brazil. All participants were enrolled through the Family Health Strategy registry, Brazil’s primary healthcare initiative operating under the Unified Health System, ensuring comprehensive municipal coverage [15].
Aiquara has 4447 residents and a Human Development Index of 0.583. Among Bahia’s 417 municipalities, Aiquara ranks 410th by population size, representing a small urban environment conducive to comprehensive epidemiological assessment [16].
2.2. Ethical Considerations
Data were obtained from a broader epidemiological investigation titled “Health conditions and lifestyle of older adults living in a small-sized municipality.” The research protocol was approved by the Research Ethics Committee of the State University of Southwest Bahia (Protocol No. 171464; Certificate of Presentation for Ethical Appraisal No. 10786212300000055), ensuring compliance with the World Medical Association’s Declaration of Helsinki and Brazilian National Health Council Resolution 466/2012.
Before data collection, all older adults received comprehensive information about the study’s objectives and procedures. Voluntary participation was confirmed by a signed Informed Consent Form from each participant, guaranteeing ethical conduct throughout the investigation.
2.3. Eligibility Criteria
Participants were recruited based on the following inclusion criteria: aged 60 years or older, community dwelling, and permanent residence within Aiquara’s urban boundaries [2]. Exclusion criteria included: cognitive impairment, assessed using the validated abbreviated Mini-Mental State Examination (MMSE) [17] with a cutoff score of ≤12 [18]; being bedridden; or having neurological or auditory disorders [2]. These criteria were implemented to ensure data integrity, precision, and participants’ complete comprehension of research protocols.
2.4. Data Collection
Data collection occurred in two distinct phases. In the first phase, socioeconomic, behavioral, and health-related information was collected through structured interviews during household visits. The second phase, conducted two to three days after the initial contact, involved anthropometric assessments and handgrip strength (HGS) testing. These physical evaluations took place at facilities provided by the Municipal Health Department of Aiquara, Bahia, Brazil. Further details on the procedures for both collection phases are documented in Santos et al. [19].
2.5. Independent Variables
PA was assessed using the first four domains of the long-form International Physical Activity Questionnaire (IPAQ) [20], an instrument validated for older Brazilian adults [21,22]. The weekly duration (min/week) of moderate-to-vigorous PA across work, transportation, domestic activities, and leisure-time domains was summed [23]. Participants were then classified as either insufficiently active (<150 min/week of total PA) or sufficiently active (≥150 min/week) [24].
SB was evaluated using the IPAQ’s fifth domain, which captures time spent sitting or reclining while awake on weekdays and weekend days [20]. A weighted average of daily SB was calculated using the formula: [(weekday sitting duration × 5) + (weekend sitting duration × 2)]/7 [23]. High SB was defined as being at or above the 75th percentile of this weighted average, corresponding to ≥342.85 min/day [25]. This approach, utilizing a percentile of the distribution within the study population, is commonly employed in epidemiological studies to identify the group with the highest exposure to the behavior when universal, clinically established cut-off points are not available for the specific measurement method and population.
Based on their PA and SB levels, participants were stratified into four groups: (G1) sufficiently active and low SB; (G2) sufficiently active and high SB; (G3) insufficiently active and low SB; and (G4) insufficiently active and high SB [26].
2.6. Dependent Variables
Waist circumference (WC) was measured with participants in a standing position, with their arms crossed over the shoulders and feet together. The measurement was taken at the narrowest region between the last rib and the superior border of the iliac crest [1]. Three consecutive measurements were recorded to the nearest 0.1 cm immediately after a normal expiration using a flexible, non-elastic anthropometric tape (Sanny®, São Bernardo do Campo, Brazil); the average of these measurements was used for analysis [2].
Body mass (BM) was measured in kilograms (kg) using a digital scale (Plena®, São Paulo, Brazil). Participants wore minimal clothing, were barefoot, and stood erect during the assessment [27]. Stature (St) was measured in meters (m) using a portable compact stadiometer (Wiso®, Campinas, Brazil), assembled according to manufacturer specifications. Participants stood barefoot with their feet together, ensuring their heels, buttocks, and scapulae were in contact with the wall, while maintaining their head in the Frankfurt Plane [27]. Body Mass Index (BMI) was subsequently calculated as BM/St2 (kg/m2) [1].
HGS was assessed using a Saehan hydraulic hand dynamometer (Model SH5002®, Saehan Corporation, Changwon, Republic of Korea) [28]. The test was performed with the dominant upper extremity while the participant was seated, arm adducted and parallel to the torso, elbow flexed at 90°, and forearm in a neutral position. The dynamometer grip was adjusted to fit individual hand sizes [16,28]. Participants were verbally encouraged to exert maximum grip force for five seconds. Two trials were performed for each hand, with a one-minute rest period between trials. The highest value, recorded in kilogram-force (kgf), was used for analysis [16,28].
DAO was defined by the concurrent presence of elevated WC (women: ≥88 cm; men: ≥102 cm) [1] and muscle weakness (dynapenia, defined as HGS: women: ≤18.37 kgf; men: ≤26.75 kgf) [29]. DO was defined by the simultaneous presence of elevated BMI (general obesity, defined as BMI > 27 kg/m2) [30] and muscle weakness (dynapenia, defined as HGS: women: ≤18.37 kgf; men: ≤26.75 kgf) [29].
2.7. Adjustment Variables (Covariables)
Multivariate model adjustment included the following variables:
- Socioeconomic: age (continuous, in years), sex (male or female), educational attainment (formal schooling: yes or no), and monthly income (≤1 minimum wage or >1 minimum wage).
- Behavioral: tobacco use (current user: yes or no), alcohol consumption (current consumer: yes or no), fruit, vegetable, or legume intake (≥2 times/day: yes or no), dairy product (e.g., milk, cheese) consumption (daily: yes or no), and protein source (e.g., eggs, beans, lentils, soy) intake (weekly: yes or no).
- Health-related: self-reported physician diagnosis of hypertension (yes or no), self-reported physician diagnosis of diabetes mellitus (yes or no), and occurrence of fall episodes in the 12 months preceding data collection (yes or no).
2.8. Statistical Analysis
Descriptive analysis of participant characteristics was performed by calculating absolute and relative frequencies for categorical variables, and means and standard deviations for continuous variables. The response rate for each variable was also determined [31].
To assess the combined association of PA level and SB exposure with DAO and DO, Poisson regression with robust variance estimation was employed. This approach allowed for the calculation of Prevalence Ratios (PR) and their respective 95% Confidence Intervals (CIs) [32].
For the construction of the multivariate models, a backward stepwise elimination method was used. All of the adjustment variables listed in Section 2.7 were initially included in the model. Variables were then sequentially removed based on the highest p-values (Wald test), with only those variables demonstrating a p-value ≤ 0.10 being retained in the final models [33]. Data analyses were conducted using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA). A significance level of 5% (p ≤ 0.05) was adopted for all inferential analyses.
3. Results
Initially, a comprehensive census was conducted to enumerate all older adults residing within the urban boundaries of Aiquara, Bahia, Brazil. Through complete household visitation, facilitated by Community Health Agents from the Family Health Strategy, 263 older adults were identified [34]. Following the application of pre-established eligibility criteria, 207 of these individuals (58.90% women) constituted the final study population, as detailed in Figure 1.
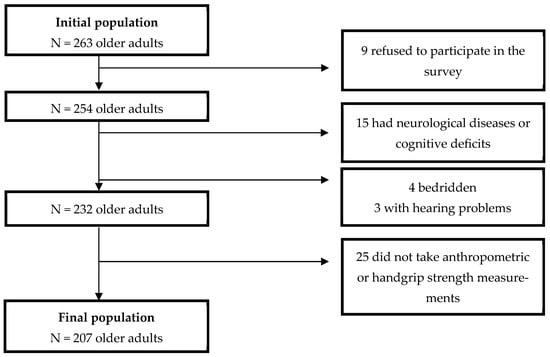
Figure 1.
Flowchart describing the eligibility process of older adults included in the study.
The mean age was 71.05 ± 6.76 years for women and 72.24 ± 8.16 years for men. The prevalence of DAO was 11.10% (women: 16.40%; men: 3.50%), while the prevalence of DO was 6.80% (women: 9%; men: 3.50%). Furthermore, 44.90% of participants presented with abdominal obesity, 38.20% with general obesity, and 24.60% were classified as having dynapenia.
Regarding socioeconomic, behavioral, and health characteristics of the participants, 87.10% reported an income equal to or below one minimum wage, 61.40% had no formal education, and 58.90% reported a physician diagnosis of hypertension. Concerning lifestyle patterns, 51.20% of participants were insufficiently active, 27.30% had high SB exposure, and 16.90% exhibited both insufficient PA levels and high SB exposure. Additional characteristics of the study population are presented in Table 1.

Table 1.
Description of the socioeconomic, behavioral and health-related aspects of the study population.
After controlling for potential confounding socioeconomic, behavioral, and health-related variables, the combined association of PA and SB levels with DAO and DO was evaluated. The adjusted analysis revealed that, compared to participants who were sufficiently active with low SB exposure (G1), those classified as insufficiently active with high SB exposure (G4) had 5.54 times the prevalence of DAO (PR: 5.54, 95% CI: 1.91–16.03) and 6.54 times the prevalence of DO (PR: 6.54, 95% CI: 1.68–36.66). These findings, along with results for other PA/SB combination groups, are presented in Table 2.

Table 2.
Combined association between physical activity level and sedentary behavior exposure with dynapenic abdominal obesity and dynapenic obesity in the study population.
4. Discussion
The principal findings of this epidemiological investigation revealed that insufficient PA levels, when combined with SB exposure, were positively associated with DAO and DO in the study population. Given the limited research examining the combined association of PA and SB with DAO and DO in older adults, these findings represent important evidence that may help address the existing knowledge gap regarding the impact of the simultaneous occurrence of these behaviors on such outcomes.
Although no previous studies were identified that specifically examined the combined association of PA and SB with both DAO and DO, a cross-sectional investigation by Smith et al. [35] evaluated the association between high SB exposure and DAO in a large, representative sample (n = 20,198; mean age: 69.30 ± 13.10 years) of older adults from six countries (China, Ghana, India, Mexico, Russia, and South Africa) who participated in the Study on Global AGEing and Adult Health (SAGE). Their main finding demonstrated that exposure to ≥8 h per day of SB was associated with 52% greater odds of DAO (OR: 1.52; 95% CI: 1.11–2.07).
The literature also indicates independent associations between PA levels or SB exposure and obesity-related outcomes. For instance, a systematic review by Silveira et al. [13], which analyzed 23 studies encompassing 638,000 adults and older adults, found higher odds of obesity among those with high SB exposure and those who were insufficiently active. Additionally, Ramsey et al. [12], in a systematic review of 122 studies (43,796 older adults), reported that greater time spent in PA and lower SB exposure were associated with better upper and lower limb muscle strength among older adults.
Within this context, a previous cross-sectional study conducted with the older adult population of Aiquara, Bahia, Brazil, demonstrated that combined PA levels and SB exposure were associated with dynapenia. Compared to older adults who were sufficiently active and had low SB exposure (the reference group), insufficiently active participants with low SB exposure had 2.28 times the prevalence of dynapenia (PR: 2.28; 95% CI: 1.09–4.76), and those who were insufficiently active and had high SB exposure exhibited 4.14 times the prevalence of dynapenia (PR: 4.14; 95% CI: 1.09–4.76) [26].
These associations between insufficient PA combined with high SB exposure likely stem from the detrimental physiological effects these behaviors exert [11]. Prolonged periods of physical immobility, or hypokinesia, represent a primary effect [36]. This state can lead to a homeostatic imbalance characterized by decreased protein synthesis capacity and increased degradation of skeletal muscle proteins, ultimately resulting in muscle atrophy and reduced force-generating capacity [11]. Furthermore, hypokinesia may result in declines in mitochondrial volume and function, diminishing the capacity for energy generation via oxidative phosphorylation for muscle contractions [37].
Prolonged sedentary time not only decreases the skeletal muscle’s ability to utilize energy but also impairs its capacity to absorb glucose, as extended SB and insufficient PA can reduce insulin sensitivity [11,37]. Consequently, excess glucose may be shunted to the liver, converted into fatty acids, and subsequently stored excessively in adipose tissue, thereby contributing to the development of abdominal and general obesity [38].
Considering these adverse effects, adopting an active lifestyle combined with low SB exposure is widely recommended [23,25,26,36]. Accordingly, the World Health Organization (WHO) recommends that older adults engage in at least 150–300 min of moderate-intensity aerobic PA per week, or 75–150 min of vigorous-intensity aerobic PA per week, or an equivalent combination of both [24]. The WHO guidelines also emphasize that older adults can start with small amounts of PA and gradually increase frequency, intensity, and duration. Additionally, they recommend multicomponent PA that includes muscle-strengthening activities on three or more days per week. Regarding SB, the WHO advises minimizing sedentary time and replacing it with PA of any intensity, including light activity [24].
Despite its valuable contributions, this study has limitations that should be acknowledged when interpreting the findings. First, PA and SB were evaluated using a self-report questionnaire (IPAQ). While the IPAQ is a widely used instrument in epidemiological studies, it provides an indirect measure of these behaviors and is subject to potential recall and social desirability biases. Furthermore, it primarily captures total time spent in different intensity levels and does not fully account for sedentary time patterns, such as the frequency and duration of breaks in sedentary time. Second, the study population consisted of older adults residing in a specific small municipality in Northeastern Brazil. Although the census-based approach allowed for a comprehensive investigation within this context, the demographic, socioeconomic, and cultural characteristics of this population may limit the direct generalizability of our findings to older adults in significantly different geographical, socioeconomic, or healthcare access settings. However, these results are likely relevant for municipalities with similar profiles.
Further investigation into how specific local socio-cultural, economic, or environmental characteristics (e.g., access to health services, predominant cultural norms related to PA, or aspects of the built environment) might modulate these associations in diverse settings would enhance the applicability of these findings. Finally, despite controlling for several important potential confounding variables, the possibility of residual confounding by unmeasured factors (e.g., detailed dietary intake, specific chronic disease severity or duration, lifetime PA/SB trajectories) cannot be entirely excluded.
Notwithstanding these limitations, the present study also possesses notable strengths. One such strength is the use of the MMSE as a criterion to exclude older adults with cognitive impairment, thereby aiming to minimize potential recall bias in the self-reported measures. Another strength lies in the assessment of muscle strength through HGS, a method considered a gold standard for evaluating muscle weakness in older adults [39]. The census-based recruitment approach adopted in this research is also noteworthy, as this strategy enabled the investigation of associations between insufficient PA combined with high SB exposure and DAO and DO in a population of older adults living in a small-sized municipality in an understudied region of Northeastern Brazil.
The findings of this research, demonstrating a strong association between the combination of insufficient PA and high SB exposure and a substantially higher prevalence of DAO and DO in older adults, carry significant practical implications for public health and clinical practice. While traditional interventions often prioritize increasing PA, our results highlight the critical need for dual approaches that simultaneously promote increased activity levels and a substantial reduction in time spent sedentary. Health professionals, particularly those working in primary care settings and contexts with limited resources, can utilize validated questionnaires, such as the IPAQ (employed in this study), to screen older adults for both PA levels and sedentary time. Identifying individuals who present this unfavorable combination of behaviors (insufficient PA and high SB) allows for targeting more specific and potentially more effective interventions.
Public health policies and health promotion programs aimed at the older adult population should, therefore, incorporate messaging and strategies that emphasize the importance of ‘moving more and sitting less’ throughout the day, extending beyond structured exercise sessions alone. Tailored, combined interventions, which might include community programs promoting both regular exercise (incorporating strength training appropriate for older adults) and practical strategies to reduce and interrupt daily sitting time (such as educational campaigns on the benefits of regular movement breaks and improvements in community walkability), could be instrumental in the prevention and management of dynapenic obesity, which represents a considerable health challenge in older populations, especially in municipalities with socioeconomic and healthcare access characteristics similar to Aiquara, Bahia, Brazil. Understanding these associations in such contexts provides a foundation for developing localized, impactful health initiatives.
Collectively, the findings of this research suggest etiological hypotheses regarding the influence of combined insufficient PA and high SB exposure on DAO and DO in older adults. These findings may provide a robust foundation for future epidemiological research. Longitudinal studies, such as prospective cohorts, are crucial to more definitively establishing temporal relationships and the magnitude of risk. Such studies should ideally incorporate objective measures of PA and SB (e.g., accelerometers) to overcome self-report limitations and better characterize activity and sedentary patterns (including breaks in sedentary time). Furthermore, future research could also explore the efficacy of multifaceted interventions designed to mitigate these combined risks in older populations.
5. Conclusions
The findings of this study support the proposed hypothesis, demonstrating that the combination of insufficient PA and SB exposure was associated with a substantially higher prevalence of DAO and DO among the older adults investigated.
Author Contributions
Conceptualization, L.d.S., P.d.F.V.N., C.B.d.A., D.d.A.T.S. and C.A.C.; methodology, L.d.S., P.d.F.V.N., C.B.d.A., D.d.A.T.S. and C.A.C.; validation, L.d.S., P.d.F.V.N., D.d.A.T.S., R.d.S.C., J.A.O.C. and C.A.C.; formal analysis, L.d.S., P.d.F.V.N., D.d.A.T.S., R.d.S.C., J.A.O.C. and C.A.C.; investigation, L.d.S., P.d.F.V.N. and C.A.C.; resources, L.d.S., P.d.F.V.N. and C.A.C.; data curation, L.d.S., P.d.F.V.N. and C.A.C.; writing—original draft preparation, L.d.S., P.d.F.V.N., C.B.d.A., L.L.G., P.d.S.S., E.L.C. and C.A.C.; writing—review and editing, L.d.S., P.d.F.V.N., C.B.d.A., L.L.G., P.d.S.S., E.L.C. and C.A.C.; visualization, L.d.S., P.d.F.V.N., C.B.d.A., R.d.S.C., D.d.A.T.S., J.A.O.C., L.L.G., P.d.S.S., E.L.C. and C.A.C.; supervision, P.d.F.V.N., C.B.d.A. and C.A.C.; project administration, L.d.S., P.d.F.V.N., C.B.d.A. and C.A.C.; funding acquisition, L.d.S., P.d.F.V.N., C.B.d.A. and C.A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Fundação de Amparo à Pesquisa do Estado da Bahia (FAPESB; Bahia State Research Support Foundation), grant number [BOL0436/2020].
Institutional Review Board Statement
The research protocol was approved by the Research Ethics Committee of the State University of Southwest Bahia (Protocol No. 171464; Certificate of Presentation for Ethical Appraisal No. 10786212300000055), ensuring compliance with the World Medical Association’s Declaration of Helsinki and Brazilian National Health Council Resolution 466/2012.
Informed Consent Statement
Before data collection, all older adults received comprehensive information about the study’s objectives and procedures. Voluntary participation was confirmed by a signed Informed Consent Form from each participant, guaranteeing ethical conduct throughout the investigation.
Data Availability Statement
The data sets generated and/or analyzed during the study are available from the corresponding author upon request.
Acknowledgments
The authors also wish to express their sincere gratitude to the Municipal Health Department of Aiquara, Bahia, Brazil, for their invaluable support and cooperation during the study, and especially to the older adults of Aiquara for their generous participation.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Physical Status: The Use of and Interpretation of Anthropometry, Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995; Available online: https://apps.who.int/iris/handle/10665/37003 (accessed on 10 December 2024).
- Santos, L.; Pedreira, R.B.S.; Silva, R.R.; Barbosa, R.S.; Valença Neto, P.F.; Casotti, C.A. Anthropometric indicators of adiposity as predictors of systemic arterial hypertension in older people: A cross-sectional analysis. Rev. Nutr. 2023, 36, e220137. [Google Scholar] [CrossRef]
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 2018, 9, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.C.; Manini, T.M. What is dynapenia? Nutrition 2012, 28, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Silva Alexandre, T.; Scholes, S.; Santos, J.L.F.; Oliveira Duarte, Y.A.; Oliveira, C. The combination of dynapenia and abdominal obesity as a risk factor for worse trajectories of IADL disability among older adults. Clin. Nutr. 2018, 37, 2045–2053. [Google Scholar] [CrossRef] [PubMed]
- Araújo, F.C.D.; Silva, K.S.D.; Ohara, D.G.; Matos, A.P.; Pinto, A.C.P.N.; Pegorari, M.S. Prevalence of and risk factors for dynapenic abdominal obesity in community-dwelling older adults: A cross-sectional study. Ciênc. Saúde Colet. 2022, 27, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Zbehlik, A.J.; Pidgeon, D.; Bartels, S.J. Dynapenic obesity and the effect on long-term physical function and quality of life: Data from the osteoarthritis initiative. BMC Geriatr. 2015, 15, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Jiang, J.; Hao, Q.; Luo, L.; Dong, B. Dynapenic obesity and lower extremity function in elderly adults. J. Am. Med. Dir. Assoc. 2015, 16, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Sénéchal, M.; Dionne, I.J.; Brochu, M. Dynapenic abdominal obesity and metabolic risk factors in adults 50 years of age and older. J. Aging Health 2012, 24, 812–826. [Google Scholar] [CrossRef] [PubMed]
- Silva Alexandre, T.; Scholes, S.; Santos, J.F.; Oliveira Duarte, Y.A.; Oliveira, C. Dynapenic abdominal obesity increases mortality risk among English and Brazilian older adults: A 10-year follow-up of the ELSA and SABE studies. J. Nutr. Health Aging 2018, 22, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.J.; Bergouignan, A.; Dempsey, P.C.; Roschel, H.; Owen, N.; Gualano, B.; Dunstan, D.W. Physiology of sedentary behavior. Physiol. Rev. 2023, 103, 2561–2622. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, K.A.; Rojer, A.G.; D’Andrea, L.; Otten, R.H.; Heymans, M.W.; Trappenburg, M.C.; Maier, A.B. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2021, 67, 101266. [Google Scholar] [CrossRef] [PubMed]
- Silveira, E.A.; Mendonça, C.R.; Delpino, F.M.; Souza, G.V.E.; Souza Rosa, L.P.; Oliveira, C.; Noll, M. Sedentary behavior, physical inactivity, abdominal obesity and obesity in adults and older adults: A systematic review and meta-analysis. Clin. Nutr. ESPEN 2022, 50, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. S1), S31–S34. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde. Política Nacional de Atenção Básica: PNAB (Portaria nº 2.436, de 21 de Setembro de 2017); Ministério da Saúde: Brasília, Brazil, 2017. [Google Scholar]
- Silva, D.J.; Santos, L.; Souza, Y.S.; Valença Neto, P.F.; Santana, P.S.; Almeida, C.B.; Casotti, C.A. Physical fitness according to the level of physical activity in older people: A cross-sectional analysis. Fisioter. Mov. 2023, 36, e36134. [Google Scholar] [CrossRef]
- Icaza, M.G.; Albala, C. Minimental State Examinations (MMSE) del Estudio de Demencia en Chile: Análisis Estadístico; Organización Panamericana de la Salud: Washington, DC, USA, 1999; pp. 18–28. [Google Scholar]
- Bertolucci, P.H.; Brucki, S.; Campacci, S.R.; Juliano, Y. O mini-exame do estado mental em uma população geral: Impacto da escolaridade. Arq. Neuro Psiquiatr. 1994, 52, 1–7. [Google Scholar] [CrossRef]
- Santos, E.S.; Santos, L.; Caires, S.S.; Silva, D.J.; Souza, Y.S.; Valença Neto, P.F.; Casotti, C.A. Functional performance indicators associated with hypertension in older people. Fisioter. Mov. 2023, 36, e36113. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Oja, P. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, T.R.B.; Antunes, P.D.C.; Rodriguez-Añez, C.R.; Mazo, G.Z.; Petroski, É.L. Reprodutibilidade e validade do Questionário Internacional de Atividade Física (IPAQ) em homens idosos. Rev. Bras. Med. Esporte 2007, 13, 11–16. [Google Scholar] [CrossRef]
- Benedetti, T.R.B.; Mazo, G.Z.; Barros, M.V. Aplicação do questionário internacional de atividades físicas para avaliação do nível de atividades física de mulheres idosas: Validade concorrente e reprodutibilidade teste-reteste. Rev. Bras. Ciênc. Mov. 2004, 12, 25–34. [Google Scholar]
- Santos, L.; Almeida, C.B.; Valença Neto, P.F.; Silva, R.R.; Santos, I.C.; Casotti, C.A. Habitual physical activity and sedentary behavior as predictors of dynapenia in older adults: A cross-sectional study. São Paulo Med. J. 2024, 142, e2023070. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Santos, L.; Silva, R.R.; Santana, P.S.; Valença Neto, P.F.; Almeida, C.B.; Casotti, C.A. Factors associated with dynapenia in older adults in the Northeast of Brazil. J. Phys. Educ. 2022, 33, e3342. [Google Scholar] [CrossRef]
- Santos, L.; Valença Neto, P.F.; Pedreira, R.B.S.; Silva, R.R.; Galvão, L.L.; Almeida, C.B.; Santos, D.A.T.; Casotti, C.A. Association of physical activity combined with sedentary behavior with dynapenia in older adults. J. Phys. Educ. 2023, 34, e3430. [Google Scholar] [CrossRef]
- Frisancho, A.R. New standards of weight and body composition by frame size and height for assessment of nutritional status of adults and the elderly. Am. J. Clin. Nutr. 1984, 40, 808–819. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, I.M.; Sampaio, R.F.; Mancini, M.C.; Silva, F.C.M.; Souza, M.A.P. Test of grip strength using the Jamar dynamometer. Acta Fisiátr. 2007, 14, 104–110. [Google Scholar] [CrossRef]
- Santos, L.; Santana, P.S.; Caires, S.S.; Barbosa, R.S.; Rodrigues, S.C.; Almeida, C.B.; Valença Neto, P.F.; Casotti, C.A. Força e massa muscular em idosos do Nordeste brasileiro. Res. Soc. Dev. 2021, 10, e570101422270. [Google Scholar] [CrossRef]
- Gonçalves, T.J.M.; Horie, L.M.; Gonçalves, S.E.A.B.; Bacchi, M.K.; Bailer, M.C.; Barbosa-Silva, T.G. Diretriz BRASPEN de Terapia Nutricional no Envelhecimento. Braspen J. 2019, 34, 1–68. Available online: https://nutritotal.com.br/pro/wp-content/uploads/sites/3/2019/11/Material-1-diretriz-TN-no-envelhecimento.pdf (accessed on 10 December 2024).
- Mishra, P.; Pandey, C.M.; Singh, U.; Gupta, A.; Sahu, C.; Keshri, A. Descriptive statistics and normality tests for statistical data. Ann. Card. Anaesth. 2019, 22, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, L.; Scazufca, M.; Menezes, P.R. Methods for estimating prevalence ratios in cross-sectional studies. Rev. Saúde Pública 2008, 42, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S.; Daniel, R.; Pearce, N. Outcome modelling strategies in epidemiology: Traditional methods and basic alternatives. Int. J. Epidemiol. 2016, 45, 565–575. [Google Scholar] [CrossRef] [PubMed]
- Valença Neto, P.F.; Santos, L.; Rodrigues, S.C.; Almeida, C.B.; Casotti, C.A. Prevalência e fatores associados à suspeição de transtornos mentais comuns em idosos: Um estudo populacional. J. Bras. Psiquiatr. 2023, 72, 100–110. [Google Scholar] [CrossRef]
- Smith, L.; López Sánchez, G.F.; Rahmati, M.; Tully, M.A.; Pizzol, D.; Veronese, N.; Koyanagi, A. Association between sedentary behavior and dynapenic abdominal obesity among older adults from low-and middle-income countries. Aging Clin. Exp. Res. 2024, 36, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Raffin, J.; de Souto Barreto, P.; Le Traon, A.P.; Vellas, B.; Aubertin-Leheudre, M.; Rolland, Y. Sedentary behavior and the biological hallmarks of aging. Ageing Res. Rev. 2023, 83, 101807. [Google Scholar] [CrossRef] [PubMed]
- Le Roux, E.; De Jong, N.P.; Blanc, S.; Simon, C.; Bessesen, D.H.; Bergouignan, A. Physiology of physical inactivity, sedentary behaviours and non-exercise activity: Insights from the space bedrest model. J. Physiol. 2022, 600, 1037–1051. [Google Scholar] [CrossRef] [PubMed]
- Meneguci, J.; Santos, D.A.T.; Silva, R.B.; Santos, R.G.; Sasaki, J.E.; Tribess, S.; Júnior, J.S.V. Comportamento sedentário: Conceito, implicações fisiológicas e os procedimentos de avaliação. Motricidade 2015, 11, 160–174. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Zamboni, M. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).