- Article
Infective Endocarditis in a Tertiary Hospital in Porto—Is There Anything New?
- Carolina Gomes,
- Isabel Gomes Abreu and
- Lurdes Santos
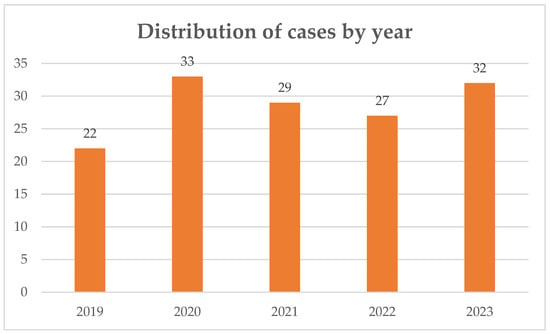
Background/Objectives: Infective endocarditis (IE) remains a severe and complex disease despite advances in diagnosis and treatment. The changing epidemiological profile, with an ageing population, has reshaped its presentation and management. This study describes the epidemiological, clinical and microbiological characteristics of IE at a Portuguese tertiary referral hospital prior to the establishment of a multidisciplinary Endocarditis Team. Methods: A retrospective analysis was conducted including all adult patients diagnosed with definite or possible IE according to the 2015 ESC criteria, admitted to ULS São João, Porto, between January 2019 and December 2023. Data were collected from electronic medical records and included demographic characteristics, comorbidities, microbiology, imaging, surgical indications and outcomes. Results: A total of 143 IE episodes were identified. Median age was 71 years, with a predominance of heterologous material-related infections (81%). Enterococcus faecalis, viridans group streptococci and coagulase-negative staphylococci were the most frequent pathogens. Surgical indication was present in 74% of cases, although surgery was not performed in 22% due to comorbidities or frailty, contributing to a high in-hospital mortality rate. Conclusions: This study provides a contemporary overview of IE in Portugal, reflecting an elderly, comorbid population and a predominance of prosthetic disease. The results highlight the need for multidisciplinary management and early surgical decisions, supporting the creation of Endocarditis Teams in tertiary centres.
25 December 2025