- 2.8Impact Factor
- 5.6CiteScore
- 17 daysTime to First Decision
Challenges and Perspectives of Neurological Disorders
This special issue belongs to the section “Systems Neuroscience“.
Special Issue Information
Dear Colleagues,
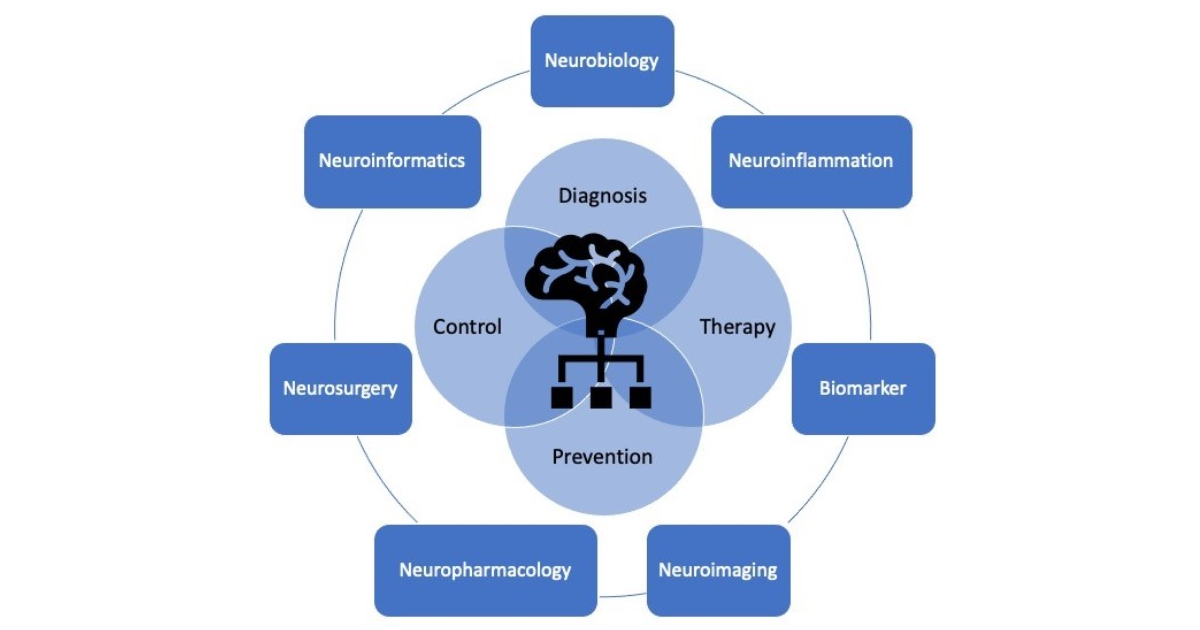
Neurological disorders are increasingly recognized as one of the most prevalent disorders worldwide, with a high burden on patients, families, and society as a whole. Neurological disorders can affect the brain, spinal cord, and other nerves throughout the body. The results can be bothersome or even detrimentally devastating. There are many different etiologies per se. Neurological disorders refer not only to common neurodegenerative diseases, such as neurovascular disorders, neuro-oncological diseases, neuroinflammation, and infection, as well as traumatic brain/spinal cord injuries, but also to a category of other less common pathogeneses.
The burden of neurological disorders has increased in the past and is likely to increase in the future, due to the aging population worldwide, thus placing an increasing demand on already overstretched resources and services for patients with neurological disorders. There is an urgent need to improve the prevention and management of neurological disorders across the globe.
The detection and targeting of neuronal damage involves a spectrum of multifaceted technologies. We encourage all basic and clinical contributions pertaining to neurological disorders, without restrictions on the type of article. The findings of this topic will be useful to advance healthcare planning and resource allocation, to prevent and reduce the burden of neurological disorders.
Dr. Woon-Man Kung
Dr. Dina Nur Anggraini Ningrum
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 250 words) can be sent to the Editorial Office for assessment.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Brain Sciences is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2200 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- nervous system disease
- prevention and control
- diagnosis and therapy
- neurobiology
- neuroinflammation
- biomarker
- neuroimaging
- neuropharmacology
- neurosurgery
- neuroinformatics
Benefits of Publishing in a Special Issue
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- e-Book format: Special Issues with more than 10 articles can be published as dedicated e-books, ensuring wide and rapid dissemination.

