- Article
Morphometric and Morphological Analysis of the Pulmonary Auscultatory Triangle in Human Fetuses: Anatomical Insights for Thoracic Surgery
- Caio Siqueira Kuhn,
- Marcelo Lucas de Lima Prado and
- José Aderval Aragão
- + 4 authors
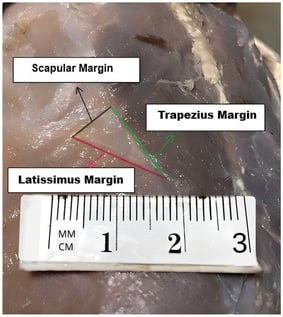
Objectives: The Pulmonary Auscultatory Triangle (PAT) is a bilateral region on the back delimited by the trapezius, latissimus dorsi, and scapula. Beyond its relevance for pulmonary auscultation, PAT also represents an important anatomical window for posterior thoracic approaches. While its anatomy has been extensively described in adults, data on its developmental morphology during fetal life remain scarce. This original morphometric study aimed to characterize the morphometry and morphology of the PAT in human fetuses and to evaluate differences according to sex, side, and gestational age. Methods: A total of 80 PATs from 40 human fetuses (20 male and 20 female) were examined. Using ImageJ software 1.54k, we measured margin lengths (inferior trapezius, medial scapular, and superior latissimus), area, and perimeter. Morphological classification was performed based on internal angles. Associations with sex, side, and gestational age were statistically assessed. Results: The mean gestational age was 28.6 weeks. PAT had a mean area of 103.2 mm2 and a mean perimeter of 49.1 mm. Mean margin lengths were 20.1 mm for the trapezius, 12.4 mm for the scapular margin, and 16.6 mm for the latissimus dorsi. Three morphologies were observed: acute (42.5%), obtuse (25.0%), and rectangular (32.5%). A significant asymmetry in shape distribution was found between sides (p = 0.034). Weak but statistically significant positive correlations with gestational age were found for perimeter and for the trapezius and latissimus dorsi margins, indicating progressive enlargement with fetal growth. Conclusions: This study provides the first detailed morphometric and morphological description of the PAT in human fetuses. The findings establish a developmental anatomical baseline for the posterior thoracic wall and highlight growth-related changes and side-related variability.
9 February 2026



![(A) A representation of the level of experimental transection performed by H.E. Hering in the atrioventricular bundle of 4 dog hearts. Published in Tawara, S. [21]. Anatomisch-Histologische Nachprüfung der Schnittfuhrung an den von Prof. H.E. Hering Ubersandten Hundeherzen. Zentralblatt für Physiologie 1906 111:300–302 “(Anatomical–histological verification of the incision made by Prof. H.E. Herring on dog hearts. Central Journal of Physiology.1906 111:300–302)”. K = atrioventricular node; S = atrioventricular fibrous septum [fibrous skeleton of heart]; W = experimental transection; t = bifurcating bundle; r = right branch; ll = left bundle branches. (B) A didactic representation of the human His bundle and important reference points for planning the experimental transection. Published in S. Tawara [19]. “Das Reizleitungssystem Des Säugetier herzens. Eine Anatomisch-Histologische Studie Über Das Atrioventrikularbündel Und Die Purkinjeschen Fäden (The conduction system of the mammalian heart. An anatomical–histological study of the atrioventricular bundle and Purkinje’s network) Jena: Gustav Fischer. Right side view = superior drawing; left side view = inferior drawing; P = membranous septum; t = bifurcating bundle; right branch (r) and left bundle branches (ll); X = frontier between atrium and ventricle; m = aortic mitral leaflet; a = center of membranous septum; ac = verical imaginary line; ba–ad = septal and superior tricuspid leaflet position; ef = suggested transection line; vsd = right coronary aortic leaflet; vsp = noncoronary aortic leaflet.](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/anatomia/anatomia-05-00003/article_deploy/html/images/anatomia-05-00003-g001-550.jpg)
![A schematic illustration of possible anatomical variants of the persistent superior vena cava [8]: (A) normal anatomical configuration with the right superior vena cava (RSVC); (B) presence of both RSVC and a persistent left superior vena cava (LSVC) connected by the left brachiocephalic vein (LBV); (C) double superior vena cava, similar to (B), but without the LBV; (D) persistent LSVC in the absence of the RSVC. Image: Prof. Schulze-Tanzil.](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/anatomia/anatomia-05-00002/article_deploy/html/images/anatomia-05-00002-g001-550.jpg)