- Review
Lateral Patellar Compression Syndrome: Surgical Techniques and Treatment
- Mason Nolan,
- Ethan Marting and
- Benjamin C. Taylor
- + 4 authors
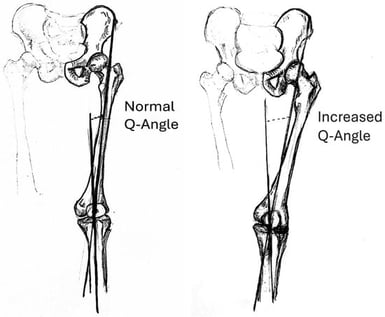
Anterolateral knee pain is a common complaint that can be debilitating for patients if not treated properly. Lateral Patellar Compression Syndrome (LPCS), characterized by the maltracking of the patella with flexion, placing undue stress on the lateral patellar facet, is a common mechanism causing anterolateral knee pain. Symptoms tend to be exacerbated with deep/prolonged flexion as the lateral patellar facet is compressed on the lateral trochlear groove of the femur. While conservative treatment methods are often sufficient, persistent pain may indicate surgical intervention to correct mechanical malalignment. The surgical treatment of LPCS is not widely agreed upon, with numerous techniques being practiced and no single procedure being considered optimal. This narrative review synthesizes the available literature on surgical techniques for LPCS treatment. A comprehensive search strategy was not employed, limiting the systematic nature of our findings.
22 January 2026



![(A) A representation of the level of experimental transection performed by H.E. Hering in the atrioventricular bundle of 4 dog hearts. Published in Tawara, S. [21]. Anatomisch-Histologische Nachprüfung der Schnittfuhrung an den von Prof. H.E. Hering Ubersandten Hundeherzen. Zentralblatt für Physiologie 1906 111:300–302 “(Anatomical–histological verification of the incision made by Prof. H.E. Herring on dog hearts. Central Journal of Physiology.1906 111:300–302)”. K = atrioventricular node; S = atrioventricular fibrous septum [fibrous skeleton of heart]; W = experimental transection; t = bifurcating bundle; r = right branch; ll = left bundle branches. (B) A didactic representation of the human His bundle and important reference points for planning the experimental transection. Published in S. Tawara [19]. “Das Reizleitungssystem Des Säugetier herzens. Eine Anatomisch-Histologische Studie Über Das Atrioventrikularbündel Und Die Purkinjeschen Fäden (The conduction system of the mammalian heart. An anatomical–histological study of the atrioventricular bundle and Purkinje’s network) Jena: Gustav Fischer. Right side view = superior drawing; left side view = inferior drawing; P = membranous septum; t = bifurcating bundle; right branch (r) and left bundle branches (ll); X = frontier between atrium and ventricle; m = aortic mitral leaflet; a = center of membranous septum; ac = verical imaginary line; ba–ad = septal and superior tricuspid leaflet position; ef = suggested transection line; vsd = right coronary aortic leaflet; vsp = noncoronary aortic leaflet.](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/anatomia/anatomia-05-00003/article_deploy/html/images/anatomia-05-00003-g001-550.jpg)
![A schematic illustration of possible anatomical variants of the persistent superior vena cava [8]: (A) normal anatomical configuration with the right superior vena cava (RSVC); (B) presence of both RSVC and a persistent left superior vena cava (LSVC) connected by the left brachiocephalic vein (LBV); (C) double superior vena cava, similar to (B), but without the LBV; (D) persistent LSVC in the absence of the RSVC. Image: Prof. Schulze-Tanzil.](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/anatomia/anatomia-05-00002/article_deploy/html/images/anatomia-05-00002-g001-550.jpg)