A Case of Double Superior Vena Cava with a Rare Accessory Hemiazygos Arch Crossing over the Descending Aorta in a Male Body Donor
Abstract
1. Introduction
2. Materials and Methods
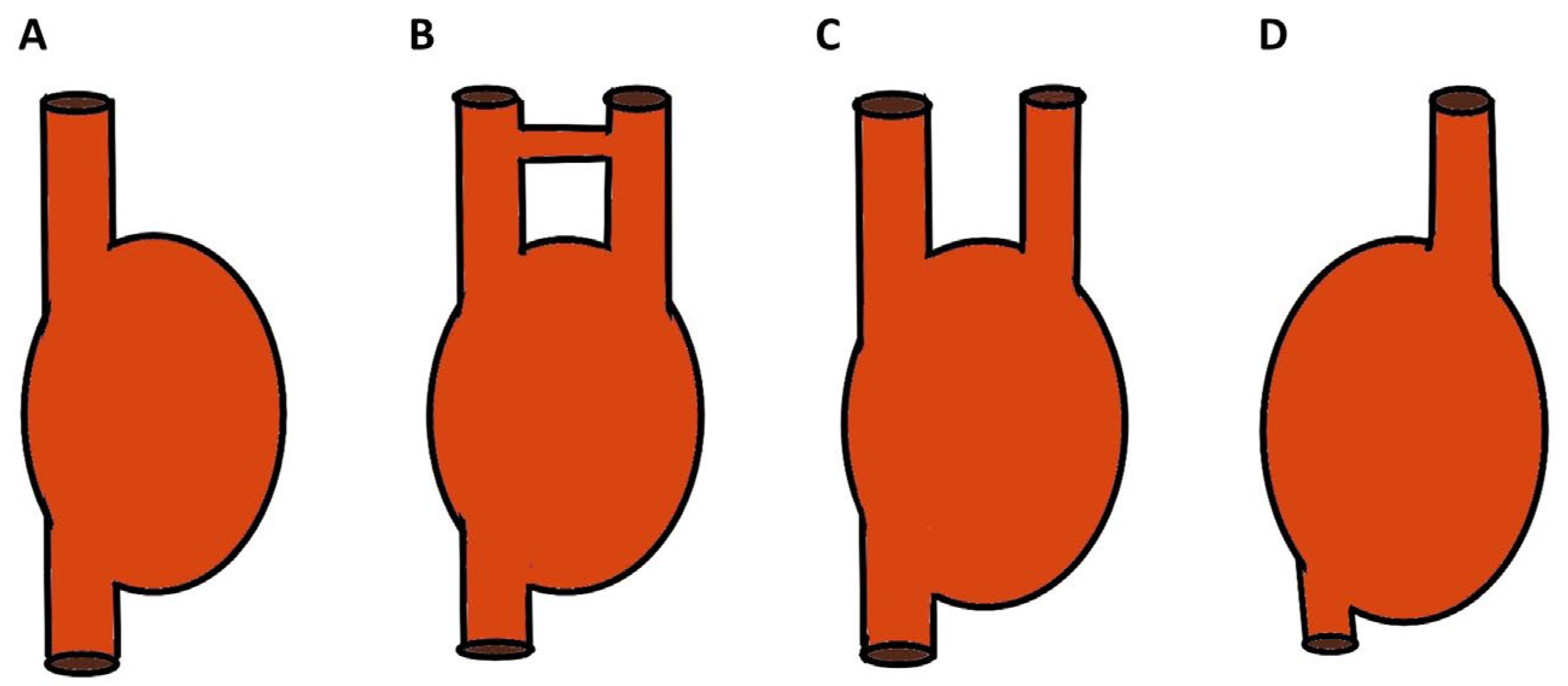
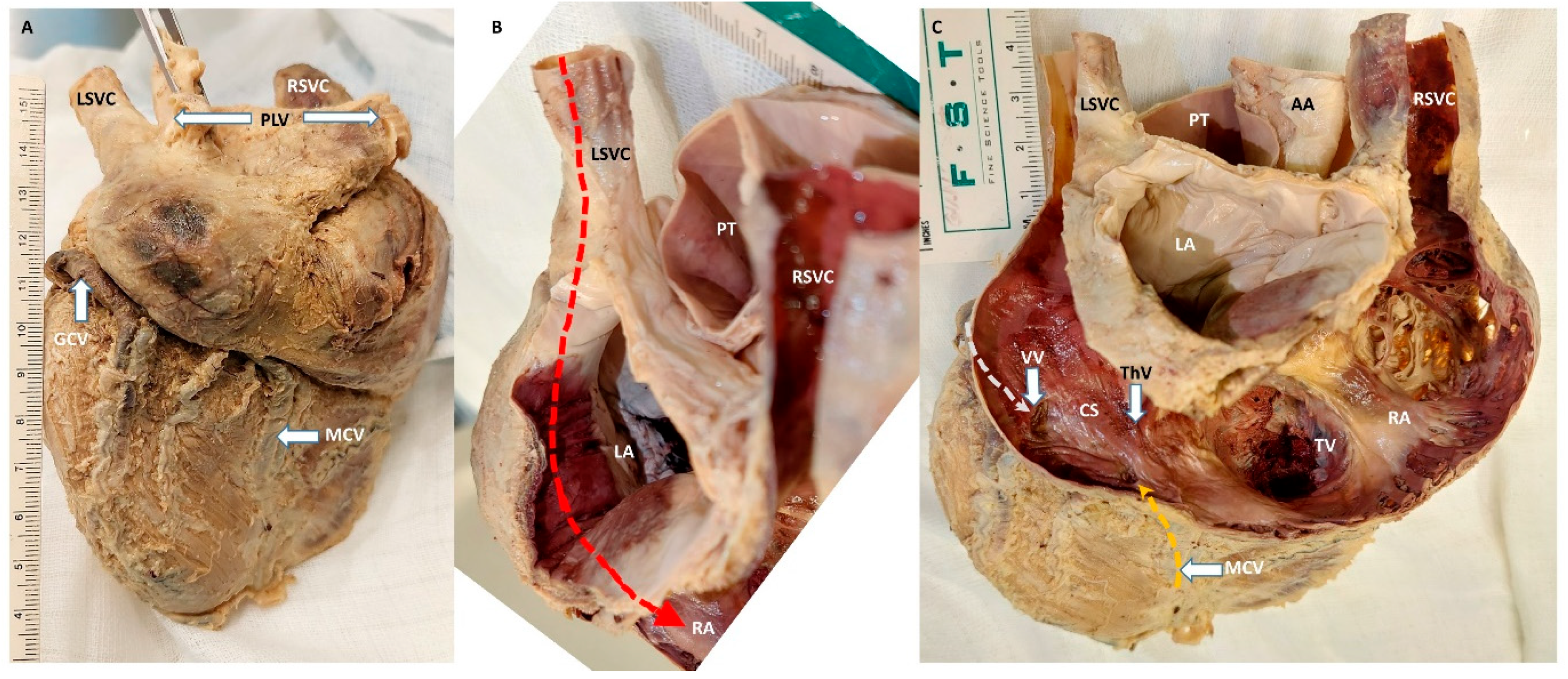
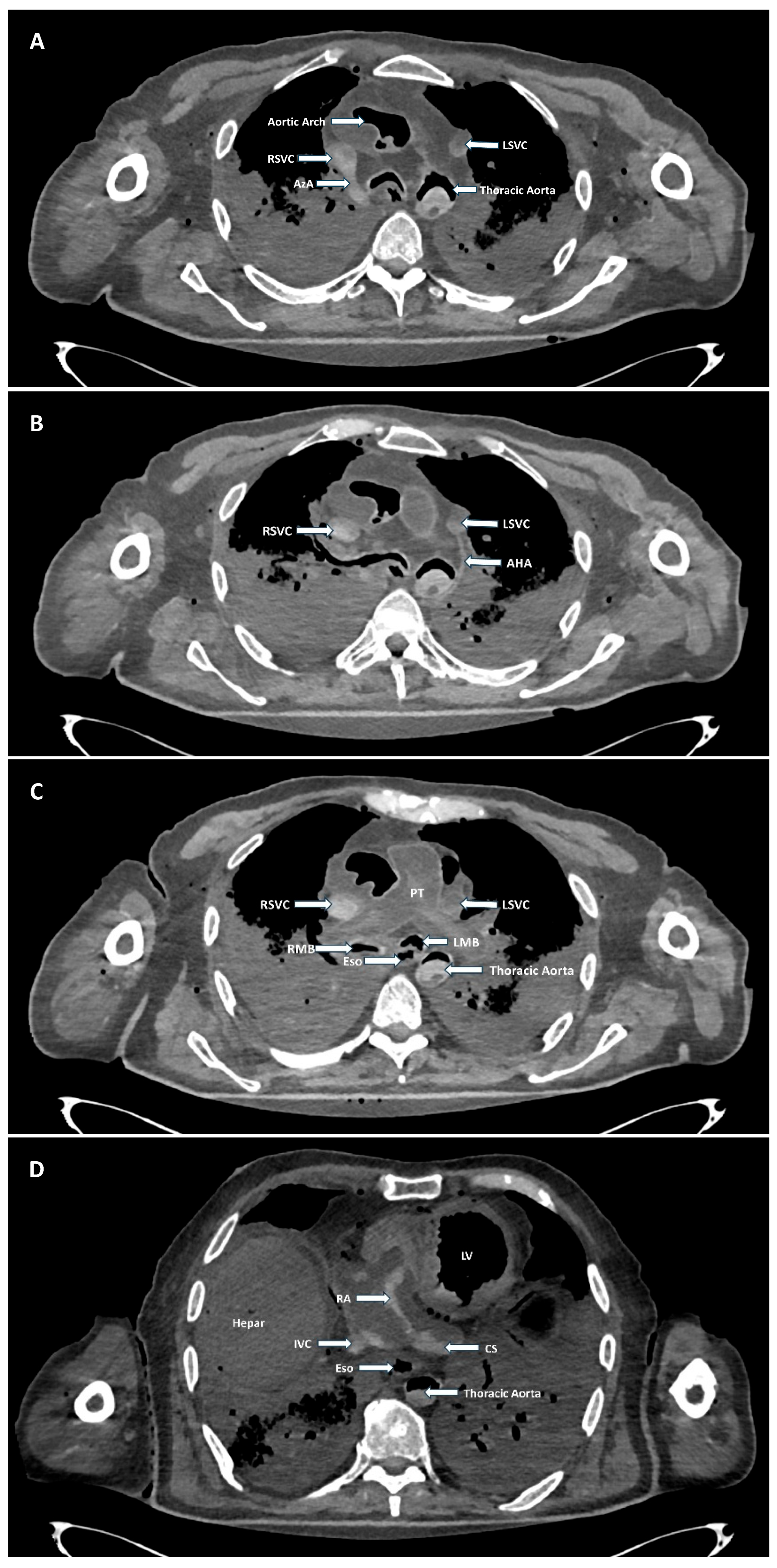
3. Findings
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AA | Ascending aorta |
| AHA | Accessory hemiazygos arch |
| AzA | Azygos arch |
| CS | Coronary sinus |
| CT | Computed tomography |
| GCV | Great cardiac vein |
| ICD | Implantable cardioverter-defibrillator |
| IVC | Inferior vena cava |
| LAD | Left anterior descending artery |
| LBV | Left brachiocephalic vein |
| LMB | Left main bronchus |
| LPA | Left pulmonary artery |
| LSVC (Ip) | Left superior vena cava (intrapericardial) |
| LSVC(Ep) | Left superior vena cava (extrapericardial) |
| MCV | Middle cardiac vein |
| PLVs | Pulmonary veins |
| PT | Pulmonary trunk |
| RA | Right atrium |
| RBV | Left brachiocephalic vein |
| RITA | Right internal thoracic artery |
| RITV | Right internal thoracic vein |
| RSVC | Right superior vena cava |
| SVC | Superior vena cava |
| ThV | Thebesian valve |
| TV | Tricuspid valve |
| VV | Vieussens valve |
References
- Standring, S. (Ed.) Thorax: Overview and Surface Anatomy. In Gray’s Anatomy; Elsevier: Amsterdam, The Netherlands, 2021; pp. 990–996.e2. [Google Scholar]
- Moore, K.L.; Persaud, T.V.N.; Torchia, M.G. (Eds.) Embryologie: Entwicklungsstadien, Frühentwicklung, Organogenese, Klinik, 6th ed.; Elsevier, Urban & Fischer: München, Germany, 2013. [Google Scholar]
- Couvreur, T.; Benoît, G. Left Superior Vena Cava. In Integrated Cardiothoracic Imaging with Mdct; Rémy-Jardin, M., Rémy, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 289–305. [Google Scholar]
- Persaud, T.V.N.; Torchia, M.G. (Eds.) Cardiovascular System. In The Developing Human; Saunders: Philadelphia, PA, USA, 2025; pp. 265–316. [Google Scholar]
- Carlson, B.M. Development of the Vascular System. In Reference Module in Biomedical Sciences; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Standring, S. (Ed.) Heart. In Gray’s Anatomy; Elsevier: Amsterdam, The Netherlands, 2021; pp. 1068–1096.e1. [Google Scholar]
- D’Cruz, I.A.; Shala, M.B.; Johns, C. Echocardiography of the Coronary Sinus in Adults. Clin. Cardiol. 2000, 23, 149–154. [Google Scholar] [CrossRef]
- Demșa, I.; Crișu, D.; Haba, C.M.Ș.; Ursaru, A.M.; Afrăsânie, V.-A.; Costache, I.I.; Petriș, A.O.; Tesloianu, D.N. Persistent Left Superior Vena Cava with Absent Right Superior Vena Cava and Discrete Subaortic Stenosis Diagnosed in a Patient with Sick Sinus Syndrome: A Case Report and Brief Review of the Literature. Diagnostics 2020, 10, 847. [Google Scholar] [CrossRef]
- Hammer, N.; Löffler, S.; Feja, C.; Sandrock, M.; Schmidt, W.; Bechmann, I.; Steinke, H. Ethanol-Glycerin Fixation with Thymol Conservation: A Potential Alternative to Formaldehyde and Phenol Embalming. Anat. Sci. Educ. 2012, 5, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Silawal, S.; Bucher, P.; Kursawe, S.; Hammer, N.; Werner, C.; Shrestha, R.; Schulze-Tanzil, G. Unilateral Subclavian Vein Fenestration Featuring a Traversing Brachial Plexus Nerve Branch and Associated Vascular Dysgeneses in a Female Body Donor. Anatomia 2025, 4, 3. [Google Scholar] [CrossRef]
- Tyrak, K.W.; Holda, J.; Holda, M.K.; Koziej, M.; Piatek, K.; Klimek-Piotrowska, W. Persistent Left Superior Vena Cava. Cardiovasc. J. Afr. 2017, 28, e1–e4. [Google Scholar] [CrossRef] [PubMed]
- Sarodia, B.D.; Stoller, J.K. Persistent Left Superior Vena Cava: Case Report and Literature Review. Respir Care 2000, 45, 411–416. [Google Scholar] [PubMed]
- Umamaheswaran, D.; Sakkarai, J.; Devi, R. Case Report of Persistent Left Superior Vena Cava with Absent Papillary Muscle—Unusual Coexistence. J. Anat. Soc. India 2022, 71, 324–328. [Google Scholar] [CrossRef]
- Steckiewicz, R.; Stolarz, P.; Marchel, M.; Michalak, M.; Konecki, D.; Szczerba, E.; Kowara, M.; Grabowska-Derlatka, L.; Grabowski, M. Double Superior Vena Cava and Left Brachiocephalic Vein Agenesis: A Rare Systemic Vein Anomaly and Potential Source of Cardiac Implantable Electronic Device and Central Venous Catheter Placement Complications. Folia Morphol. 2022, 81, 1066–1071. [Google Scholar] [CrossRef]
- Dave, V.; Sesham, K.; Mehra, S.; Roy, T.; Ahuja, M. Persistent Left Superior Vena Cava: An Anatomical Variation. Med. J. Armed Forces India 2022, 78, S277–S281. [Google Scholar] [CrossRef]
- Prasanna, L.C.; Thomas, H.R.; Das, A.; Kumar, R. Left-Sided Persistent Superior Vena Cava with Superior Hemiazygos Arch. J. Clin. Diagn. Res. 2016, 10, AD03–AD05. [Google Scholar] [CrossRef]
- Kowalski, M.; Maynard, R.; Ananthasubramaniam, K. Imaging of Persistent Left Sided Superior Vena Cava with Echocardiography and Multi-Slice Computed Tomography: Implications for Daily Practice. Cardiol. J. 2011, 18, 332–336. [Google Scholar] [PubMed]
- Murli, L.; Ranjit, M.S.; Shah, P. Unroofed Coronary Sinus: An Unusual Interatrial Communication and a Rare Childhood Entity. Ann. Pediatr. Cardiol. 2019, 12, 64–65. [Google Scholar] [CrossRef] [PubMed]
- Ootaki, Y.; Yamaguchi, M.; Yoshimura, N.; Oka, S.; Yoshida, M.; Hasegawa, T. Unroofed Coronary Sinus Syndrome: Diagnosis, Classification, and Surgical Treatment. J. Thorac. Cardiovasc. Surg. 2003, 126, 1655–1656. [Google Scholar] [CrossRef] [PubMed]
- Catanchin, A.; Castellanos, E.; Marjan, J.; Ward, D. Wolff-Parkinson-White Syndrome with an Unroofed Coronary Sinus without Persistent Left Superior Vena Cava Treated with Catheter Cryoablation. Indian Pacing Electrophysiol. J. 2008, 8, 227–233. [Google Scholar]
- Bisbee, C.R.; Sherard, C.; Rajab, T.K. Left Superior Vena Cava Draining to Left Atrium: A Case Report, Review of the Literature, and Classification. Pediatr. Cardiol. 2024, 45, 1838–1840. [Google Scholar] [CrossRef]
- Raghib, G.; Ruttenberg, H.D.; Anderson, R.C.; Amplatz, K.; Adams, P., Jr.; Edwards, J.E. Termination of Left Superior Vena Cava in Left Atrium, Atrial Septal Defect, and Absence of Coronary Sinus; a Developmental Complex. Circulation 1965, 31, 906–918. [Google Scholar] [CrossRef]
- Tobbia, P.; Norris, L.A.; Lane, T. Persistent Left Superior Vena Cava Draining into the Left Atrium. BMJ Case Rep. 2013, 2013, 010167. [Google Scholar] [CrossRef]
- Lendzian, T.; Vogt, J.; Krasemann, T. Are Anomalies of the Caval Veins More Common in Complex Congenital Heart Disease? Herz Kardiovaskuläre Erkrank. 2007, 32, 657–664. [Google Scholar] [CrossRef]
- Dahran, N.; Soames, R. Anatomical Variations of the Azygos Venous System: Classification and Clinical Relevance. Int. J. Morphol. 2016, 34, 1128–1136. [Google Scholar] [CrossRef]
- Sahai, A.N.; D’Alesio, L.M.; Dugaesescu, A.L.; Bauman, J.M. The Interazygos Vein: A Case Report and Review of Preaortic Hemiazygos Anastomoses. Cureus 2025, 17, e83800. [Google Scholar] [CrossRef]
- Shiri, E.; Madadi, S. An Abnormal Course of the Interazygos Vein: A Case Report. J. Med. Case Rep. 2020, 14, 232. [Google Scholar] [CrossRef]
- Liu, F.; Ruze, A.; Amuti, S.; Wang, S.; Chen, S.; Yiming, A.; Xiong, K. A Rare Variation of the Hemiazygos Vein Draining into the Persistent Left Superior Vena Cava. Anat. Sci. Int. 2019, 94, 269–273. [Google Scholar] [CrossRef]
- Seib, G.A. The Azygos System of Veins in American Whites and American Negroes, Including Observations on the Inferior Caval Venous System. Am. J. Phys. Anthr. 1934, 19, 39–163. [Google Scholar] [CrossRef]
- Syska, B.; Veer, A.S.; Matusik, P.S.; Jarczewski, J.D.; Krzanowska, K.; Popiela, T.J. Malposition of Central Venous Catheter into Coronary Sinus Throughout the Persistent Left Superior Vena Cava and Other Complications Related to Catheterization. Diagnostics 2024, 14, 1038. [Google Scholar] [CrossRef]
- Shakhshir, A.; Abdul-Hafez, H.A.; Takhman, M.; Qasrawi, H.; Kittaneh, M.; Saada, S. Double Superior Vena Cava Incidentally Found During Permanent Catheter Placement: A Case Report and Literature Review. Radiol. Case Rep. 2025, 20, 442–448. [Google Scholar] [CrossRef]
- Van Walleghem, J.; Depuydt, S.; Schepers, S. Insertion of a Totally Implantable Venous Access Port in a Patient with Persistent Left Superior Vena Cava (Plsvc). Acta Chir. Belg. 2018, 118, 68–71. [Google Scholar] [CrossRef]
- Hajeh, H.; Garcia, A.; Mishra, S.; Radicic, K. Malposition of the Central Venous Catheter Secondary to Accessory Hemiazygos Vein Variant. J. Vasc. Access 2024, 25, 995–997. [Google Scholar] [CrossRef]
- Padovan, R.S.; Paar, M.H.; Aurer, I. (Mis)Placed Central Venous Catheter in the Left Superior Intercostal Vein. Radiol. Oncol. 2011, 45, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Tej, U.; Mishra, A.K.; Mittal, A.; Saini, K.; George, A. Surgical Correction of Total Anomalous Pulmonary Venous Connection to Persistent Left-Sided Superior Vena Cava: A Case Report. Eur. Heart J. Case Rep. 2024, 8, ytae290. [Google Scholar] [CrossRef]
- Kayashima, K.; Imai, K.; Murashima, K. Internal Jugular Vein Duplication with Absent Carotid Sheath Detected During Ultrasound-Guided Pediatric Central Venous Catheter Placement. J. Anesth. 2013, 27, 972–973. [Google Scholar] [CrossRef] [PubMed]
- Sondermeijer, B.M.; MacGillavry, M.R.; Tan, H.L. Left Superior Vena Cava, a Remnant of Embryological Development. Neth. Heart J. 2008, 16, 173–174. [Google Scholar] [CrossRef] [PubMed]
- Jeong, E.R.; Kang, E.-J.; Jeun, J.H. Pictorial Essay: Understanding of Persistent Left Superior Vena Cava and Its Differential Diagnosis. J. Korean Soc. Radiol. 2022, 83, 846–860. [Google Scholar] [CrossRef]
- Azizova, A.; Onder, O.; Arslan, S.; Ardali, S.; Hazirolan, T. Persistent Left Superior Vena Cava: Clinical Importance and Differential Diagnoses. Insights Imaging 2020, 11, 110. [Google Scholar] [CrossRef]
- Hsu, T.Y.-T.; D’SIlva, K.M.; Patel, N.J.; Fu, X.; Wallace, Z.S.; Sparks, J.A. Incident Systemic Rheumatic Disease Following COVID-19. Lancet Rheumatol. 2021, 3, e402–e404. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Wang, X.; Zhao, F.; Guo, T.; Po, S.S.; Lu, Z. The Ligament of Marshall and Arrhythmias: A Review. Pacing Clin. Electrophysiol. 2021, 44, 792–799. [Google Scholar] [CrossRef] [PubMed]
- Sundhu, M.; Syed, M.; Gul, S.; Saqi, B.; Mosteller, R. Pacemaker Placement in Persistent Left Superior Vena Cava. Cureus 2017, 9, e1311. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Silawal, S.; Kandemir, M.; Stelzl, F.; Oberguggenberger, V.; Martinovic, K.; Kokozidou, M.; Hammer, N.; Schulze-Tanzil, G. A Case of Double Superior Vena Cava with a Rare Accessory Hemiazygos Arch Crossing over the Descending Aorta in a Male Body Donor. Anatomia 2026, 5, 2. https://doi.org/10.3390/anatomia5010002
Silawal S, Kandemir M, Stelzl F, Oberguggenberger V, Martinovic K, Kokozidou M, Hammer N, Schulze-Tanzil G. A Case of Double Superior Vena Cava with a Rare Accessory Hemiazygos Arch Crossing over the Descending Aorta in a Male Body Donor. Anatomia. 2026; 5(1):2. https://doi.org/10.3390/anatomia5010002
Chicago/Turabian StyleSilawal, Sandeep, Mustafa Kandemir, Franz Stelzl, Valentina Oberguggenberger, Kristinko Martinovic, Maria Kokozidou, Niels Hammer, and Gundula Schulze-Tanzil. 2026. "A Case of Double Superior Vena Cava with a Rare Accessory Hemiazygos Arch Crossing over the Descending Aorta in a Male Body Donor" Anatomia 5, no. 1: 2. https://doi.org/10.3390/anatomia5010002
APA StyleSilawal, S., Kandemir, M., Stelzl, F., Oberguggenberger, V., Martinovic, K., Kokozidou, M., Hammer, N., & Schulze-Tanzil, G. (2026). A Case of Double Superior Vena Cava with a Rare Accessory Hemiazygos Arch Crossing over the Descending Aorta in a Male Body Donor. Anatomia, 5(1), 2. https://doi.org/10.3390/anatomia5010002






