- Article
Nurse Staffing and Hospital-Acquired Infections in Rural Versus Non-Rural Hospitals
- Kimberly Jones-Rudolph,
- Lorraine Brown and
- Soumya Upadhyay
- + 1 author
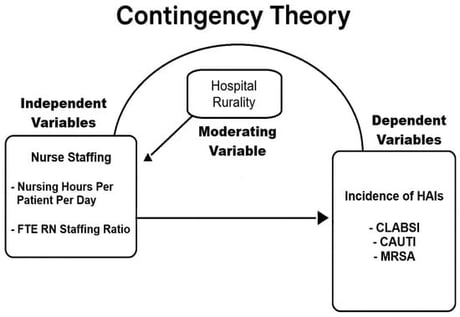
This study explores how hospital location (rural/non-rural) may moderate the nurse staffing ratio’s impact on three hospital-acquired infections. This study used data from 2022 to 2024 on nurse staffing and hospital characteristics from the American Hospital Association Annual Survey and data on hospital-acquired infection rates from the Medicare Care Compare dataset provided by the Centers for Medicare and Medicaid Services. After removing missing values, the final dataset included 7997 hospital-year observations across the US. Independent variables include rural hospital designation, nursing hours per patient day, and RN FTE per adjusted day. The dependent variables included infection rates of Central Line-Associated Bloodstream Infection, Catheter-Associated Urinary Tract Infection, and Methicillin-Resistant Staphylococcus aureus. Multiple regression was performed in Stata 18. Our research found that across all three infection types, an increase in nursing hours per patient day is significantly associated with a decrease in the infection rate, and that impact was not moderated by hospital rurality. Extra time spent with patients in either a rural or non-rural hospital decreased hospital-acquired infection rates. While RN FTEs were included in the model, total nursing hours per patient day emerged as the more consistent predictor of lower hospital-acquired infection rates.
5 February 2026