The Role of Artificial Intelligence in Healthcare Quality Improvement: A Scoping Review and Critical Appraisal of Operational Efficiency, Patient Outcomes, and Implementation Challenges
Abstract
1. Introduction
1.1. Rationale and Gap of the Study
1.2. Research Questions
- What is the scope and nature of evidence describing the impact of AI on key indicators of operational efficiency and patient outcomes within healthcare settings?
- What organisational, technical, ethical, and regulatory factors are identified in the literature as key challenges (barriers) and opportunities (enablers) for the successful implementation of AI in healthcare?
1.3. Research Aim and Objective
- To map and categorise the evidence describing AI’s impact on specific operational efficiency metrics (e.g., workflow automation, resource management) and patient outcomes (e.g., diagnostic accuracy, patient safety).
- To identify and synthesise the key organisational, technical, and ethical factors reported in the literature as barriers and enablers to AI implementation in healthcare.
- To identify key characteristics of the existing research landscape, including standard methodologies and conceptual approaches, and to highlight knowledge gaps to inform future research and policy.
1.4. Significance of the Study
2. Materials and Methods
2.1. Research Design
2.2. Search Strategy
2.3. Selection Criteria
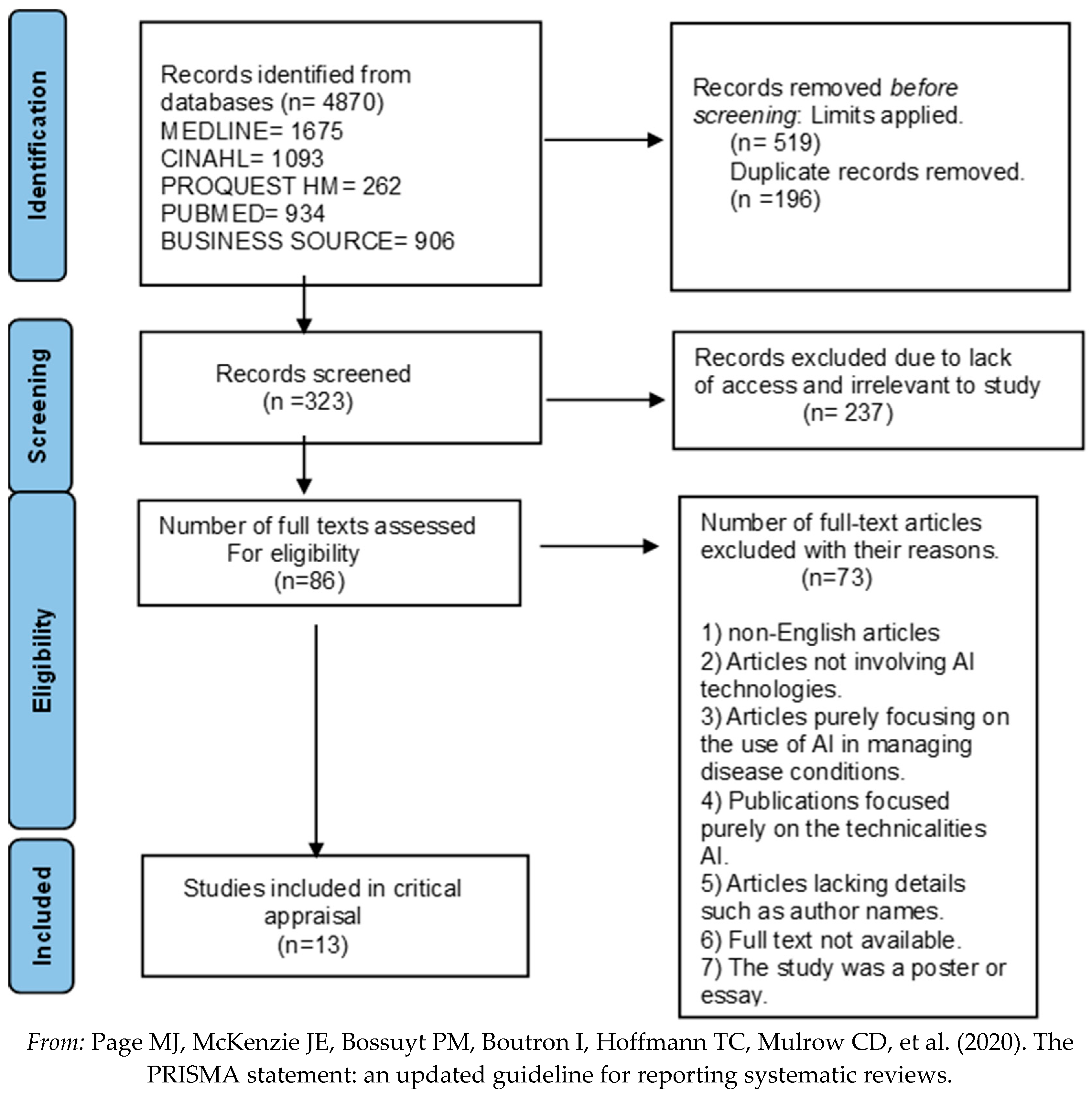
2.4. Search Outcome
2.5. Data Extraction and Charting
2.6. Data Synthesis
2.7. Quality Assessment
| (a) Qualitative Studies | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Critical appraisal criteria | Was there a clear statement of research aims | Is the methodology appropriate? | Was the research design appropriate for the objectives | Was the recruitment strategy appropriate to the research aims? | Was the data collected in a way that addressed the research issue? | Has the relationship between the researcher and participant been considered? | Have ethical issues been considered | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | How valuable is the research? | Total score | ||||
| [60] | ✓ | ✓ | ✓ | ✓ | ✓ | X | X | ✓ | ✓ | ✓ | 8 | ||||
| [61] | ✓ | ✓ | ✓ | ✓ | ✓ | X | ✓ | ✓ | ✓ | ✓ | 9 | ||||
| [62] | ✓ | ✓ | ✓ | ✓ | ✓ | X | ✓ | ✓ | ✓ | ✓ | 9 | ||||
| [63] | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✓ | ✓ | ✓ | 9 | ||||
| [64] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 10 | ||||
| [65] | ✓ | ✓ | ✓ | ✓ | ✓ | X | ✓ | ✓ | ✓ | ✓ | 9 | ||||
| [66] | ✓ | ✓ | ✓ | ✓ | ✓ | X | X | ✓ | ✓ | ✓ | 8 | ||||
| [67] | ✓ | ✓ | ✓ | ✓ | ✓ | X | ✓ | ✓ | ✓ | ✓ | 9 | ||||
| (b) Systematic Reviews | |||||||||||||||
| Critical appraisal criteria | Did the review address a clearly focused question | Did the authors look for the right papers | Were all essential relevant papers included? | Did the authors do enough to assess the quality of the included studies? | Was it reasonable to combine results | What are the overall results of the review? | How precise are the results? | Can the results be applied to the local population? | Were all important outcomes considered? | Are the benefits worth the harms and costs? | Score out of 10 | ||||
| [68] | ✓ | ✓ | X | ✓ | ✓ | Highlights the transformative potential of Healthcare 4.0 (H4.0) technologies and operational excellence tools for improving health services and operations. Furthermore, it advocates for their integration into healthcare organisations. | Although there is no statistical measurement of accuracy like confidence interval, this study appears to be quite precise as it provides a detailed comprehensive account with both bibliometric and cluster analysis. It recognises four clusters and propsoes managerial implications. | ✓ | X | ✓ | 8 | ||||
| [69] | ✓ | ✓ | ✓ | ✓ | ✓ | A comprehensive evaluation of AI technologies and applications in Chinese EDs, focusing on resource optimisation, clinical decision support and patient monitoring. There is also the exploration of challenges and opportunities of integration | The results provide a detailed account of AI applications and design recommendations for Chinese EDs, thus somewhat precise. | X | ✓ | ✓ | 9 | ||||
| [70] | ✓ | ✓ | X | ✓ | ✓ | Provides an analysis of several opportunities and challenges of implementing AI technologies in healthcare | The results of this study appear to be precise, as the quality of the included studies was assessed using Kitchenham’s criteria. Results were also synthesised from empirical data which further may enhance precision. | ✓ | ✓ | ✓ | 9 | ||||
| (c) Cohort Studies | |||||||||||||||
| Critical appraisal criteria | Did the study address a clearly focused issue | Was the cohort recruited acceptably? | Was the exposure accurately measured to minimise bias? | Was the outcome accurately measured to minimise bias? | Have the authors identified all important confounding factors? | Have they considered the confounding factors in the design and or analysis? | Was the follow up of the subjects complete enough? | Was the follow up of the subjects long enough? | What are the results? | How precise are the results? | Do you believe the results? | Can the results be applied to the local population? | Do the results of this study fit with other available evidence? | What are the implications for practice? | Score out of 14 |
| [71] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | The study revealed 29.02% of patients were readmitted and the best predictive model for pneumonia readmission was the regularised logistic regression(RegLR) | The study did not include a range of confidence intervals. However, it utilised cross validation, class imbalance handling, model selection and the area under receiver operating characteristic curve (AUROC) and other metrics like the positive and negative predictive values, sensitivity, specificity and F1 score to assess predictive models which could also indicate precision. | ✓ | X | ✓ | The study suggests that high risk patients can be identified with predictive models enabling targeted interventions to reduce readmission rates. This could improve hospital resource allocation and utimately health services. | 13 |
| [72] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | For predicting cardiopulmonary arrest, the pDEWS demonstrated exceptional performance surpassing conventional methods including the modified PEWS, random forest and logistic regression models with a higher AUROC of 0.923 and fewer false alarms. | The results are precise with narrow confidence intervals for AUROC and area under the precision-recall curve(AUPRC). This indicates reliability. | ✓ | ✓ | ✓ | The potential benefits of the integration of pDEWS into critical care could improve the early detection of critical cases, the efficiency of response teams and clinical outcomes. | 14 |
| Item No. | Appraisal | |
|---|---|---|
| TITLE AND ABSTRACT | 1. | (a) The title is clear and informative and indicates key variables, study population and type of analysis. (b) The abstract provides a well-balanced summary of the study. |
| INTRODUCTION | ||
| Background/rationale | 2. | The study’s background is clear and highlights the importance of healthcare information and performance in the context of Saudi Arabia. |
| Objectives | 3. | The objectives and hypotheses are specified and aim to address the impact of technology and innovation efforts on healthcare performance in Saudi Arabia. |
| METHODS | ||
| study design | 4. | The cross-sectional design is appropriate to the research question and is explicitly stated. |
| setting | 5. | The study setting, location and relevant dates (July 2021 and March 2022) are clearly described. |
| participants | 6. | The study includes senior healthcare practitioners from 241 organisations in Saudi Arabia, selected through emails and referrals. A simple random sampling technique was used to distribute questionnaires. |
| variables | 7. | The main variables (technology innovation, innovation efforts, and healthcare performance) are defined and translated into specific metrics that can be assessed through the survey instrument. |
| Data sources/measurements | 8. | A questionnaire was used as the data source and was descriptive in nature. |
| bias | 9. | Bias was not well addressed and was quite limited. |
| study size | 10. | The study provides some information on the sample size and the appropriateness of the chosen statistical method. However, there was no information on the reduced responses and power calculations. |
| quantitative variables | 11. | The quantitative variables were adequately handled. They seemed to be treated as continuous measures in the SEM analysis, which is well-suited to Likert-scale measurements. The article does not indicate any groupings made. |
| Statistical methods | 12. | (a) The study used the SEM analysis, particularly the partial least squares method (SMART PLS 3 programme), and correlation analysis. There was no mention of confounding controls. (b) There was no information on the examination of subgroups or interactions. (c) There was no explicit mention of how missing data were handled. (d) The simple random sampling technique was used to distribute questionnaires, but there was no mention of its use in the analysis. (e) There was no information on sensitivity analysis. |
| RESULTS | ||
| Participants | 13. | (a) The study did not address the number of participants at each stage. However, it does mention that 241 healthcare organisations were included. (b) The reason for non-participation was not documented. However, it did acknowledge that only 241 responses were received out of the 385 expected responses. (c) There was no flow diagram depicting the participant selection process. |
| Descriptive data | 14. | (a) The study provided demographic characteristics (age) of participants, but no details on clinical and or social characteristics. (b) There is no explicit information about the number of participants with missing data. |
| Outcome data | 15. | The summary did not report any specific summary measures like mean and median for the outcome variables. |
| Main results | 16. | (a) The study presents unadjusted estimates from the SEM but does not report confounder-adjusted estimates. (b) There was no reporting of category boundaries of the variables. (c) Not applicable. The results are not reported in terms of relative or absolute risk but as path weights and significance levels. |
| Other analysis | 17. | The study presents results from the SEM analysis and correlation analysis, but no additional analyses on subgroups. |
| DISCUSSION | ||
| Key results | 18. | (1) Technology innovation positively influenced healthcare performance (0.233 units increase) (2) Innovation efforts had a marked positive impact on technology innovation (0.739 units increase) and healthcare performance (0.338 units increase) (3) All 5 hypotheses were confirmed by the study. (4) Research and development, training, medical equipment acquisition and software acquisition were revealed to play a critical role in technology innovation, innovation efforts and healthcare service delivery. (5) Technology innovations like AI, telemedicine, mobile technology, digitalisation of health records had positive effects on healthcare performance. (6) The findings supported the resource-based view theory demonstrating that tangible and intangible resources are necessary for an organisation’s performance. These findings support the study objectives and provide empirical evidence for the positive relationship between technology innovation, innovation efforts and health services in Saudi Arabia. |
| Limitations | 19. | (1) The geographical focus of the study on Saudi Arabia may limit the generalisability of this research to other healthcare systems. (2) The sample size could potentially introduce bias, as results could be under or overestimated. The authors admit that the sample size could be larger. (3) The study’s cross-sectional design offers insights at a point in time rather than an extended period. The need for more diverse, longitudinal studies was suggested by the authors to understand trends over time. (4) Some core health technologies (e.g., surgical and drug innovations) were not included in the scope of research. |
| Interpretation | 20. | Although the results are in line with the resource-based view theory and some previous studies, applying the results of this study to practice would require caution. Additional studies, particularly longitudinal studies would strengthen the conclusions and applicability to other healthcare systems. |
| Generalisability | 21. | Within the scope and parameters of the study design, the study attempts to address external validity. However, it does not explore extensively all potential limitations to generalisability. |
| OTHER INFORMATION | ||
| Funding | 22. | The role of funders in not applicable in this study as the study explicitly states it received no external funding. |
2.8. Inter-Rater Reliability
| Intraclass Correlation b | 95% Confidence Interval | Value | F Test with | True Value 0 | Sig. | ||
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | df1 | df2 | ||||
| Single Measures | 0.947 a | 0.742 | 0.985 | 54.200 | 12 | 12 | <0.001 |
| Average Measures | 0.973 c | 0.852 | 0.993 | 54.200 | 12 | 12 | <0.001 |
3. Results
3.1. Search Results and Study Selection
3.2. Study Characteristics
| Author, Year | Region, Setting | Primary Objective | Methodology Type | Key Finding |
|---|---|---|---|---|
| [60] | USA, Healthcare Industry | Trends, Potential, and Barriers of AI in Medicine. | Qualitative (Thematic Analysis of symposium) | Integration barriers include data privacy, bias, and process issues; physician experience is key. |
| [61] | UK, Public Health System | Explore AI solutions for patient inflow issues in mental health. | Narrative Literature Review & Qualitative (Interviews) | AI can enhance workflow efficiency, workforce planning, and demand prediction. |
| [62] | Vietnam, Private & Public Hospitals | Discover the advantages of big data analytics in addressing operational challenges. | Qualitative (Case Study Approach) | Big data has led to enhanced resource allocation and utilisation, as well as improved patient care. |
| [63] | Malaysia, Hospital setting | Determine the benefits and challenges of AI in care delivery. | Narrative Literature Review | The benefits of AI outweigh the negative implications, with significant opportunities existing. |
| [68] | India/Europe, Diverse Healthcare Settings | Analyse the relationship between operational efficiency and Healthcare 4.0 (AI/big data). | Systematic Literature Review (Bibliometric Analysis) | AI integration has the potential to transform patient outcomes and workflow. |
| [71] | Philippines, Public Tertiary Hospital | Evaluate the effectiveness of predictive models for pneumonia readmission. | Retrospective Observational Cohort (Quantitative) | Predictive models significantly reduced patient readmission rates (demonstrating AI insight). |
| [64] | UK, Public Health System (NHS) | Examine the barriers and factors that influence the adoption of AI in the NHS. | Qualitative (Thematic Analysis of interviews) | Identified barriers like IT infrastructure issues and unclear AI language; suggested solutions like training. |
| [65] | Sweden, Healthcare Organisations | Explore healthcare leaders’ perceptions on AI implementation. | Qualitative (CFIR-based interviews) | Leaders saw benefits (early diagnosis, decision support) but expressed concerns over data security, transparency, and high cost. |
| [69] | China, Emergency Departments (ED) | Explore integration of AI with ED facilities design (opportunities/challenges). | Systematic Literature Review | AI can optimise ED efficiency and improve patient outcomes, but challenges such as data privacy and high costs exist. |
| [70] | Ethiopia, Diverse Healthcare Settings | Synthesise empirical studies on AI adoption challenges and opportunities. | Systematic Literature Review | AI has the potential to transform healthcare, but it must address ethical and privacy issues. |
| [67] | Saudi Arabia, Healthcare Organisations | Assess the nature of technology innovation and its effects on healthcare performance. | Quantitative (Correlation/SEM, Cross-sectional) | Found a strong positive correlation between technological innovation (AI) and healthcare performance. |
| [66] | USA, Non-profit Healthcare Organisation | Showcase how AI implementation can improve patient outcomes. | Case Study Report (Qualitative & Quantitative) | Showed markedly improved patient management using AI innovations like big data analytics. |
| [72] | South Korea, Tertiary Care Hospital | Develop and evaluate a deep learning-based paediatric early warning system (pDEWS). | Retrospective Observational Cohort (Quantitative) | The pDEWS outperformed existing tools (PEWS) and improved operational efficiencies and clinical outcomes. |
3.3. Quality Appraisal Summary
3.4. Conceptual Framework Showing Theme Relationships
3.5. AI Impact on Operational Efficiency and Patient Outcomes [RQ1]
3.6. Implementation Challenges and Potential Opportunities [RQ2]
4. Discussion and Recommendations
Practical Implications and Recommendations
5. Conclusions
6. Limitations
6.1. Methodological Limitations
- Protocol Preregistration: The lack of a pre-registered protocol increases the potential for reporting bias and reduces transparency in the review process.
- Database Coverage: We excluded key databases relevant to technological innovation—such as Scopus, IEEE Xplore, and the ACM Digital Library—from the search, which was confined to five databases specific to healthcare and management. This decision may have resulted in the omission of pertinent technical and interdisciplinary studies.
- Publication and Language Bias: Excluding grey literature, such as government reports and unpublished dissertations, we restricted the search only to peer-reviewed, English-language articles. This strategy likely introduced publication bias by favouring the publication of studies with statistically significant or positive findings, which could overstate the benefits of AI.
6.2. Limitations of the Evidence Base
- Limited Empirical Evidence: Although the review identified several articles discussing the potential of AI, it included only three empirical case studies that provided concrete evidence of its current impact on operational efficiency and patient outcomes. This small evidence base makes it difficult to draw definitive conclusions.
- Geographic Concentration: The geographic concentration of included studies, predominantly in Asia and Europe, limits the applicability of the findings to healthcare systems in regions such as North America, Africa, and Latin America, which face different contextual challenges.
- Lack of Cost-Effectiveness Data: A significant gap in the literature was the absence of detailed cost-effectiveness or cost–benefit analyses. While one study reported a high return on investment, the broader economic implications and viability of implementing and scaling AI systems in diverse healthcare settings remain largely unexamined.
- Absence of Patient Perspectives: The reviewed literature primarily focused on administrative and clinical viewpoints. There was a notable lack of studies investigating the patient perspective, including their experiences, acceptance, and concerns regarding AI-driven healthcare.
6.3. Temporal Limitations
- Rapid Evolution of AI: Artificial intelligence is a rapidly advancing field. Given that the review covers literature from the past 5 years, some of the technologies and findings discussed may already be outdated or superseded by more advanced innovations.
- Limited Longitudinal Data: Cross-sectional or short-term observational studies dominate the evidence base. Researchers rarely conduct longitudinal studies that track the long-term effects of AI integration on patient outcomes, organisational performance, and workforce dynamics over several years.
7. Future Research
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Henfridsson, O.; Bygstad, B. The Generative Mechanisms of Digital Infrastructure Evolution. MIS Q. 2013, 37, 907–931. [Google Scholar] [CrossRef]
- Jonsson, K.; Mathiassen, L.; Holmström, J. Representation and Mediation in Digitalized Work: Evidence from Maintenance of Mining Machinery. J. Inf. Technol. 2018, 33, 216–232. [Google Scholar] [CrossRef]
- Woods, L.; Dendere, R.; Eden, R.; Grantham, B.; Krivit, J.; Pearce, A.; McNeil, K.; Green, D.; Sullivan, C. Perceived Impact of Digital Health Maturity on Patient Experience, Population Health, Health Care Costs, and Provider Experience: Mixed Methods Case Study. J. Med. Internet Res. 2023, 25, e45868. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.H. The AI Advantage: How to Put the Artificial Intelligence Revolution to Work; MIT Press: Cambridge, MA, USA, 2018. [Google Scholar]
- Hinings, B.; Gegenhuber, T.; Greenwood, R. Digital Innovation and Transformation: An Institutional Perspective. Inf. Organ. 2018, 28, 52–61. [Google Scholar] [CrossRef]
- Naylor, C.D. On the Prospects for a (Deep) Learning Health Care System. JAMA 2018, 320, 1099–1100. [Google Scholar] [CrossRef]
- Schönberger, D. Artificial Intelligence in Healthcare: A Critical Analysis of the Legal and Ethical Implications. Int. J. Law Inf. Technol. 2019, 27, 171–203. [Google Scholar] [CrossRef]
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The Role of Artificial Intelligence in Healthcare: A Structured Literature Review. BMC Med. Inform. Decis. Mak. 2021, 21, 125. [Google Scholar] [CrossRef]
- Chen, M.; Decary, M. Artificial Intelligence in Healthcare: An Essential Guide for Health Leaders. Healthc. Manag. Forum 2019, 33, 10–18. [Google Scholar] [CrossRef]
- Dash, S.; Shakyawar, S.K.; Sharma, M.; Kaushik, S. Big Data in Healthcare: Management, Analysis and Future Prospects. J. Big Data 2019, 6, 54. [Google Scholar] [CrossRef]
- Bhatia, R. Emerging Health Technologies and How They Can Transform Healthcare Delivery. J. Health Manag. 2021, 23, 63–73. [Google Scholar] [CrossRef]
- Ball, H.C. Improving Healthcare Cost, Quality, and Access Through Artificial Intelligence and Machine Learning Applications. J. Healthc. Manag. 2021, 66, 271–279. [Google Scholar] [CrossRef]
- Bekbolatova, M.; Mayer, J.; Ong, C.W.; Toma, M. Transformative Potential of AI in Healthcare: Definitions, Applications, and Navigating the Ethical Landscape and Public Perspectives. Healthcare 2024, 12, 125. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.; Fox, J.; Purohit, M.P. Artificial Intelligence-Enabled Healthcare Delivery. J. R. Soc. Med. 2018, 112, 22–28. [Google Scholar] [CrossRef]
- Helm, J.M.; Swiergosz, A.M.; Haeberle, H.S.; Karnuta, J.M.; Schaffer, J.L.; Krebs, V.E.; Spitzer, A.I.; Ramkumar, P.N. Machine Learning and Artificial Intelligence: Definitions, Applications, and Future Directions. Curr. Rev. Musculoskelet. Med. 2020, 13, 69–76. [Google Scholar] [CrossRef]
- Hirani, R.; Noruzi, K.; Khuram, H.; Hussaini, A.S.; Aifuwa, E.I.; Ely, K.E.; Lewis, J.M.; Gabr, A.E.; Smiley, A.; Tiwari, R.K.; et al. Artificial Intelligence and Healthcare: A Journey Through History, Present Innovations, and Future Possibilities. Life 2024, 14, 557. [Google Scholar] [CrossRef]
- Rajpurkar, P.; Chen, E.; Banerjee, O.; Topol, E.J. AI in Health and Medicine. Nat. Med. 2022, 28, 31–38. [Google Scholar] [CrossRef]
- Benzidia, S.; Makaoui, N.; Bentahar, O. The Impact of Big Data Analytics and Artificial Intelligence on Green Supply Chain Process Integration and Hospital Environmental Performance. Technol. Forecast. Soc. Change 2021, 165, 120557. [Google Scholar] [CrossRef]
- Kelly, C.J.; Karthikesalingam, A.; Suleyman, M.; Corrado, G.; King, D. Key Challenges for Delivering Clinical Impact with Artificial Intelligence. BMC Med. 2019, 17, 195. [Google Scholar] [CrossRef]
- Kluge, E.H. The Ethics of Artificial Intelligence in Healthcare: From Hands-On Care to Policy-Making. Healthc. Manag. Forum 2024, 37, 406–408. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.N.; Lee, D. Artificial Intelligence and Robots in Healthcare: What Are the Success Factors for Technology-Based Service Encounters? Int. J. Healthc. Manag. 2019, 12, 218–225. [Google Scholar] [CrossRef]
- Rigby, M.J. Ethical Dimensions of Using Artificial Intelligence in Health Care. AMA J. Ethics 2019, 21, 121–124. [Google Scholar] [CrossRef]
- Lee, D.; Yoon, S.N. Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges. Int. J. Environ. Res. Public Health 2021, 18, 271. [Google Scholar] [CrossRef]
- Randell, R.; Honey, S.; Alvarado, N.; Greenhalgh, J.; Hindmarsh, J.; Pearman, A.; Jayne, D.; Gardner, P.; Gill, A.; Kotze, A.; et al. Factors Supporting and Constraining the Implementation of Robot-Assisted Surgery: A Realist Interview Study. BMJ Open 2019, 9, e028635. [Google Scholar] [CrossRef] [PubMed]
- Bini, S. Artificial Intelligence, Machine Learning, Deep Learning, and Cognitive Computing: What Do These Terms Mean and How Will They Impact Health Care? J. Arthroplast. 2018, 33, 2358–2361. [Google Scholar] [CrossRef]
- Dicuonzo, G.; Donofrio, F.; Fusco, A.; Shini, M. Healthcare System: Moving Forward with Artificial Intelligence. Technovation 2023, 120, 102510. [Google Scholar] [CrossRef]
- Holmes, J.H.; Elliott, T.E.; Brown, J.S.; Raebel, M.A.; Davidson, A.; Nelson, A.F.; Chung, A.; La Chance, P.; Steiner, J.F. Clinical Research Data Warehouse Governance for Distributed Research Networks in the USA: A Systematic Review of the Literature. J. Am. Med. Inform. Assoc. 2014, 21, 730–736. [Google Scholar] [CrossRef]
- Matheny, M.E.; Whicher, D.; Thadaney Israni, S. Artificial Intelligence in Health Care: A Report from the National Academy of Medicine. JAMA 2020, 323, 509–510. [Google Scholar] [CrossRef]
- Sazu, M.H.; Jahan, S.A. Big Data Analytics & Artificial Intelligence in Management of Healthcare: Impacts and Current State. Manag. Sustain. Dev. 2022, 14, 36–42. [Google Scholar] [CrossRef]
- Bodenheimer, T.M.D.; Sinsky, C.M.D. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Ann. Fam. Med. 2014, 12, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J. High-Performance Medicine: The Convergence of Human and Artificial Intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar] [CrossRef]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial Intelligence in Healthcare: Past, Present and Future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef]
- Jung, C.L. The Perils of Artificial Intelligence in Healthcare: Disease Diagnosis and Treatment. J. Comput. Biol. Bioinform. Res. 2019, 9, 1–6. [Google Scholar] [CrossRef]
- Keles, E.; Bagci, U. The Past, Current, and Future of Neonatal Intensive Care Units with Artificial Intelligence: A Systematic Review. npj Digit. Med. 2023, 6, 220. [Google Scholar] [CrossRef]
- Liu, X.; He, X.; Wang, M.; Shen, H. What Influences Patients’ Continuance Intention to Use AI-Powered Service Robots at Hospitals? The Role of Individual Characteristics. Technol. Soc. 2022, 70, 101996. [Google Scholar] [CrossRef]
- Aiwerioghene, E.M.; Lewis, J.; Rea, D. Maturity Models for Hospital Management: A Literature Review. Int. J. Healthc. Manag. 2024, 18, 902–915. [Google Scholar] [CrossRef]
- Reed, G.W.; Tushman, M.L.; Kapadia, S.R. Operational Efficiency and Effective Management in the Catheterization Laboratory: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2018, 72, 2507–2517. [Google Scholar] [CrossRef]
- Lebcir, R.; Hill, T.; Atun, R.; Cubric, M. Stakeholders’ Views on the Organisational Factors Affecting Application of Artificial Intelligence in Healthcare: A Scoping Review Protocol. BMJ Open 2021, 11, e044074. [Google Scholar] [CrossRef]
- Panch, T.; Szolovits, P.; Atun, R. Artificial Intelligence, Machine Learning and Health Systems. J. Glob. Health 2018, 8, 020303. [Google Scholar] [CrossRef] [PubMed]
- Perkmann, M.; Schildt, H. Open Data Partnerships Between Firms and Universities: The Role of Boundary Organizations. Res. Policy 2015, 44, 1133–1143. [Google Scholar] [CrossRef]
- Sharwood, L.N. AI Use for Injury Surveillance in Emergency Departments. JAMA Netw. Open 2025, 8, e2524162. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Cooper, I.D. What Is a “Mapping Study?”. J. Med. Libr. Assoc. 2016, 104, 76–78. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing Between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for Conducting Systematic Scoping Reviews. JBI Evid. Implement. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Matthew, J.P.; Joanne, E.M.; Patrick, M.B.; Isabelle, B.; Tammy, C.H.; Cynthia, D.M.; Larissa, S.; Jennifer, M.T.; Elie, A.A.; Sue, E.B.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Rethlefsen, M.L.; Kirtley, S.; Waffenschmidt, S.; Ayala, A.P.; Moher, D.; Page, M.J.; Koffel, J.B.; Blunt, H.; Brigham, T.; Chang, S.; et al. PRISMA-S: An Extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst. Rev. 2021, 10, 39. [Google Scholar] [CrossRef]
- Bramer, W.A.-O.; de Jonge, G.B.; Rethlefsen, M.A.-O.; Mast, F.; Kleijnen, J. A Systematic Approach to Searching: An Efficient and Complete Method to Develop Literature Searches. J. Med. Libr. Assoc. 2018, 106, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Sara Efrat, E.; Ruth, R. Writing the Literature Review: A Practical Guide; The Guilford Press: New York, NY, USA, 2019. [Google Scholar]
- Shaw, J.; Rudzicz, F.; Jamieson, T.; Goldfarb, A. Artificial Intelligence and the Implementation Challenge. J. Med. Internet Res. 2019, 21, e13659. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated Methodological Guidance for the Conduct of Scoping Reviews. JBI Evid. Implement. 2021, 19, 105–111. [Google Scholar] [CrossRef]
- Booth, A.; Sutton, A.; Papaioannou, D. Systematic Approaches to a Successful Literature Review, 2nd ed.; Sage: London, UK, 2016. [Google Scholar]
- Gough, D. Weight of Evidence: A Framework for the Appraisal of the Quality and Relevance of Evidence. Res. Pap. Educ. 2007, 22, 213–228. [Google Scholar] [CrossRef]
- Fowkes, F.G.; Fulton, P.M. Critical Appraisal of Published Research: Introductory Guidelines. BMJ 1991, 302, 1136–1140. [Google Scholar] [CrossRef]
- Long, H.A.; French, D.P.; Brooks, J.M. Optimising the Value of the Critical Appraisal Skills Programme (CASP) Tool for Quality Appraisal in Qualitative Evidence Synthesis. Res. Methods Med. Health Sci. 2020, 1, 31–42. [Google Scholar] [CrossRef]
- Critical Appraisal Skills Programme. CASP (Qualitative Studies) Checklist. 2018. Available online: https://casp-uk.net/casp-tools-checklists/qualitative-studies-checklist/ (accessed on 14 October 2025).
- Critical Appraisal Skills Programme. CASP (Systematic Reviews) Checklist. 2018. Available online: https://casp-uk.net/casp-tools-checklists/systematic-review-checklist/ (accessed on 14 October 2025).
- Critical Appraisal Skills Programme. CASP (Cohort Studies) Checklist. 2018. Available online: https://casp-uk.net/casp-tools-checklists/cohort-study-checklist/ (accessed on 14 October 2025).
- Borgstadt, J.T.; Kalpas, E.A.; Pond, H.M. A Qualitative Thematic Analysis of Addressing the Why: An Artificial Intelligence (AI) in Healthcare Symposium. Cureus 2022, 14, e23704. [Google Scholar] [CrossRef]
- Dawoodbhoy, F.M.; Delaney, J.; Cecula, P.; Yu, J.; Peacock, I.; Tan, J.; Cox, B. AI in Patient Flow: Applications of Artificial Intelligence to Improve Patient Flow in NHS Acute Mental Health Inpatient Units. Heliyon 2021, 7, e06993. [Google Scholar] [CrossRef]
- Khan, A.; Aoun, M. Improving Hospital Operations and Resource Management in Vietnam Through Big Data Analytics. J. Hum. Behav. Soc. Sci. 2022, 6, 52–62. [Google Scholar] [CrossRef]
- Khaled, N.; Turki, A.; Aidalina, M. Implications of Artificial Intelligence in Healthcare Delivery in the Hospital Settings: A Literature Review. Int. J. Public Health Clin. Sci. 2019, 6, 22–38. [Google Scholar] [CrossRef]
- Morrison, K. Artificial Intelligence and the NHS: A Qualitative Exploration of the Factors Influencing Adoption. Future Healthc. J. 2021, 8, e648–e654. [Google Scholar] [CrossRef] [PubMed]
- Neher, M.; Petersson, L.; Nygren, J.M.; Svedberg, P.; Larsson, I.; Nilsen, P. Innovation in Healthcare: Leadership Perceptions about the Innovation Characteristics of Artificial Intelligence—A Qualitative Interview Study with Healthcare Leaders in Sweden. Implement. Sci. Commun. 2023, 4, 81. [Google Scholar] [CrossRef]
- Schlicher, J.; Metsker, M.T.; Shah, H.; Demirkan, H. From NASA to Healthcare: Real-Time Data Analytics (Mission Control) Is Reshaping Healthcare Services. Perspect. Health Inf. Manag. 2021, 18, 1g. [Google Scholar] [PubMed Central]
- Akinwale, Y.O.; AboAlsamh, H.M. Technology Innovation and Healthcare Performance Among Healthcare Organizations in Saudi Arabia: A Structural Equation Model Analysis. Sustainability 2023, 15, 3962. [Google Scholar] [CrossRef]
- Detwal, P.K.; Agrawal, R.; Samadhiya, A.; Kumar, A.; Garza-Reyes, J.A. Revolutionizing Healthcare Organizations with Operational Excellence and Healthcare 4.0: A Systematic Review of the State-of-the-Art Literature. Int. J. Lean Six Sigma 2024, 15, 80–102. [Google Scholar] [CrossRef]
- Tan, S.; Mills, G. Designing Chinese Hospital Emergency Departments to Leverage Artificial Intelligence—A Systematic Literature Review on the Challenges and Opportunities. Front. Med. Technol. 2024, 6, 1307625. [Google Scholar] [CrossRef]
- Wubineh, B.Z.; Deriba, F.G.; Woldeyohannis, M.M. Exploring the Opportunities and Challenges of Implementing Artificial Intelligence in Healthcare: A Systematic Literature Review. Urol. Oncol. 2024, 42, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Landicho, J.A. Predicting One-Year Readmission of Adult Patients with Pneumonia Using Machine Learning Approaches: A Case Study in the Philippines. Int. J. Healthc. Manag. 2024, 18, 285–293. [Google Scholar] [CrossRef]
- Park, S.J.; Cho, K.J.; Kwon, O.; Park, H.; Lee, Y.; Shim, W.H.; Park, C.R.; Jhang, W.K. Development and validation of a deep-learning-based pediatric early warning system: A single-center study. Biomed. J. 2022, 45, 155–168. [Google Scholar] [CrossRef]
- Von Elm, E.D.; Altman, D.G.P.; Egger, M.P.; Pocock, S.J.P.; Gøtzsche, P.C.M.D.; Vandenbroucke, J.P.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]


| P | Population | Clinical and non-clinical staff, including healthcare workers, leaders, managers, administrators, and doctors |
| C | Concept | Enhancing healthcare delivery with AI integration. |
| C | Context | Global healthcare systems, organisations, and hospitals. |
| Database | Search Strategy |
|---|---|
| Medline, Cinahl Ultimate, Proquest Health Management, Pubmed, Business Source Complete Search Date: 2 June 2025–4 June 2025 | “healthcare delivery” OR “healthcare services” OR “delivery of healthcare” OR “quality care” OR “healthcare provision” AND “operational efficiency” OR “operations performance” OR “workflow efficiency” OR “operational effectiveness” AND “artificial intelligence” OR “AI” OR “machine learning” OR “deep learning” OR “intelligent systems” OR “healthcare 4.0 tehnologies” |
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Population | Publications involving AI interventions in healthcare systems and organisations. | Articles focusing purely on AI implementation in medicine. Grey literature. |
| Interest | Research papers evaluating the effect of AI technologies on healthcare delivery, including their advantages, challenges, and future opportunities. | Research papers on the use of AI in non-healthcare settings. |
| Study design | All study designs utilising quantitative, qualitative, or mixed methods, particularly observational (cohort) and qualitative (case–control) studies. | Publications focusing on the technicalities and science of AI. |
| Date | Peer-reviewed articles published within the last 5 years. | Studies older than 5 years. |
| Language | English language studies with full-text availability. | Non-English articles. |
| Opportunities and Challenges | |||
|---|---|---|---|
| Potential Opportunities | Challenges | ||
| Enhanced decision-making | AI innovations and big data analytics can provide hospitals with evidence-based decision-making, which could inform strategies for the delivery of quality care [61,62,63,65,69,70,71,72]. | Resource requirements | Implementing AI within healthcare organisations could be expensive, requiring significant funding, staff training and upgrading of current IT infrastructure to support its use [61,63,65,69,70,71]. |
| Predictive healthcare | Healthcare organisations can leverage technological innovations to forecast patient outcomes and promote personalised treatment, allowing early interventions, ultimately leading to enhanced efficiency and improved population health [61,64,65,67,69,70,72] | Data security and Privacy issues | The lack of a robust regulatory framework, together with the integration of big data and AI with highly sensitive patient information, poses a significant risk to data security [60,61,62,70]. |
| Improved healthcare performance | Repetitive and discrete tasks could be automated to minimise human errors, thus reducing the workload and fatigue of healthcare workers [64,65,69,72] | Data quality and biases | Inconsistent and inaccurate data collection may result from human errors, dynamic healthcare units and variability in patient’s length of stay. This may lead to poor data quality and algorithmic biases [61,62,64,69,70] |
| Improved healthcare access | AI-enabled devices can provide vital information for patient monitoring within hospitals and also remotely [69,70] | Resistance to change | A poor understanding and ignorance of the potential benefits of AI can lead to an unwillingness to embrace its implementation [60,62,64,70] |
| Innovations and development | Technological innovations like AI could accelerate the development of innovations, ultimately reducing the cost for patients and healthcare organisations [67,70] | Lack of interoperability | Several health organisations seemed to operate as siloed, each working independently with minimal communication and data sharing [60,64,65,70] |
| Patient empowerment | Patients can become active participants in their care with personalised AI devices, providing them with more up-to-date information on their health status [65] | “black box AI” | The decision-making processes underlining AI systems were considered not easily explainable and interpretable, indicating a lack of transparency and unreliability [60,64,65,70] |
| Lack of an evaluation framework | The absence of a standard framework to assess the impact of AI innovations in healthcare organisations poses difficulties for implementation [60,64,70] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aiwerioghene, E.M.; Osuchukwu, V.C. The Role of Artificial Intelligence in Healthcare Quality Improvement: A Scoping Review and Critical Appraisal of Operational Efficiency, Patient Outcomes, and Implementation Challenges. Hospitals 2025, 2, 27. https://doi.org/10.3390/hospitals2040027
Aiwerioghene EM, Osuchukwu VC. The Role of Artificial Intelligence in Healthcare Quality Improvement: A Scoping Review and Critical Appraisal of Operational Efficiency, Patient Outcomes, and Implementation Challenges. Hospitals. 2025; 2(4):27. https://doi.org/10.3390/hospitals2040027
Chicago/Turabian StyleAiwerioghene, Erhauyi Meshach, and Vivian Chinonso Osuchukwu. 2025. "The Role of Artificial Intelligence in Healthcare Quality Improvement: A Scoping Review and Critical Appraisal of Operational Efficiency, Patient Outcomes, and Implementation Challenges" Hospitals 2, no. 4: 27. https://doi.org/10.3390/hospitals2040027
APA StyleAiwerioghene, E. M., & Osuchukwu, V. C. (2025). The Role of Artificial Intelligence in Healthcare Quality Improvement: A Scoping Review and Critical Appraisal of Operational Efficiency, Patient Outcomes, and Implementation Challenges. Hospitals, 2(4), 27. https://doi.org/10.3390/hospitals2040027





