- Review
Urticaria and Urticaria-like Dermatoses in Pregnancy: Clinical Spectrum, Differential Diagnosis and Management
- Federica Trovato,
- Antonio Di Guardo and
- Giovanni Pellacani
- + 4 authors
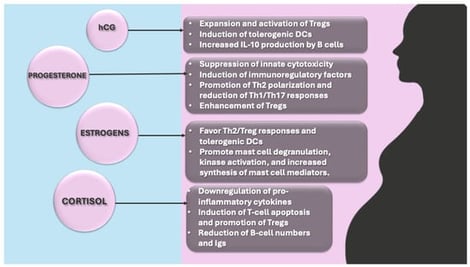
Urticaria is a mast cell-mediated disorder commonly encountered in women of reproductive age, making its interaction with pregnancy clinically relevant. Gestation induces profound hormonal and immunologic adaptations—including shifts between Th1/Th17 and Th2/Treg responses and sustained exposure to sex steroids and placental hormones—that can modulate mast cell reactivity. As a result, chronic urticaria (CU) shows heterogeneous behavior during pregnancy: approximately half of patients improve, one third worsen, and the remainder remain stable. Pregnancy also presents several urticaria-like dermatoses, notably polymorphic eruption of pregnancy (PEP/PUPPP), atopic eruption of pregnancy (AEP) and pemphigoid gestationis (PG), as well as rare hormone-induced hypersensitivity reactions. Additionally, systemic disorders such as intrahepatic cholestasis of pregnancy (ICP), chronic kidney disease–associated pruritus and urticarial vasculitis may mimic urticaria but differ markedly in prognosis, maternal–fetal risk and management. Given this complexity, accurate diagnosis requires integration of temporal pattern, lesion morphology and duration, distribution, systemic features and targeted investigations, as outlined in the diagnostic algorithm proposed. Most pregnancy-specific eruptions are benign, whereas PG, ICP and urticarial vasculitis warrant prompt recognition due to potential fetal implications. Management of CU in pregnancy generally follows standard guidelines, with second-generation H1-antihistamines as first-line therapy and omalizumab reserved for severe refractory cases.
25 February 2026