- Article
Scope, Features, and Utility of Australian Penicillin Allergy Delabelling Protocols: A Descriptive Analysis
- Claire Chitty,
- Lerato Obadimeji and
- Sandra M. Salter
- + 8 authors
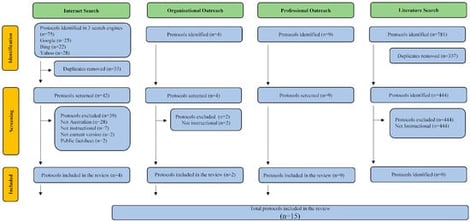
Penicillin allergy delabelling improves patient outcomes, reduces healthcare costs, and supports antimicrobial stewardship. While PADL protocols (PADL-P) are increasingly used in clinical practice, the consistency of Australian PADL-Ps and their alignment with established guidance remain unclear. A cross-sectional study (from June to August 2025) identified Australian PADL-Ps through organisational and professional outreach, the literature, and structured internet searches. Protocol features were extracted iteratively and deductively. Citation counts and overlap were determined using the Graphical Representation of Overlap for OVErviews (GROOVE) methodology. Protocols were applied to 20 validated penicillin allergy scenarios, and the Australasian Society for Clinical Immunology and Allergy (ASCIA) Consensus Statement for the Management of Suspected Penicillin Allergy and risk alignment were compared. Fifteen Australian PADL-Ps were identified. They shared similar features; however, differences were observed in the no/low-risk criteria and subsequent delabelling actions. Protocols cited a mean of nine references (mean of 4.7 (43.9%) unique), with one protocol citing no references. When applied to clinical scenarios, protocol-assigned risk did not consistently align with the ASCIA risk classification (54.6% of adult and 77.8% of paediatric protocols assigned scenarios to the same risk level). Adult protocol alignment was lowest for no-risk (31.9%) and low-risk (50.0%) scenarios and highest for moderate-risk scenarios (78.8%), whereas paediatric protocol alignment was 33.3% for moderate risk and 100% for low and high-risk scenarios. Although Australian PADL-Ps shared core structural features, incongruencies in risk criteria and alignment with established guidelines may result in different clinical outcomes for patients with similar penicillin allergy histories. These findings emphasise the complexity of clinical decision-making around penicillin allergy and suggest a need for standardisation of PADL-Ps to maximise delabelling benefits and safety across Australian healthcare settings.
9 February 2026