Journal Description
Reproductive Medicine
Reproductive Medicine
is an international, peer-reviewed, open access journal on obstetrics and gynecology published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, FSTA, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 27.1 days after submission; acceptance to publication is undertaken in 13.6 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
1.3 (2024);
5-Year Impact Factor:
1.2 (2024)
Latest Articles
Persistent Right Umbilical Vein: Clinical Case and Literature Review
Reprod. Med. 2025, 6(4), 36; https://doi.org/10.3390/reprodmed6040036 - 6 Nov 2025
Abstract
►
Show Figures
Background and Clinical Significance: This article presents a clinical case of persistent umbilical vein of the extrahepatic type in a fetus. The features, diagnosis, and prognosis of this rare vascular anomaly, as well as the applied pregnancy monitoring tactics, are reviewed. Case Presentation:
[...] Read more.
Background and Clinical Significance: This article presents a clinical case of persistent umbilical vein of the extrahepatic type in a fetus. The features, diagnosis, and prognosis of this rare vascular anomaly, as well as the applied pregnancy monitoring tactics, are reviewed. Case Presentation: A 34-year-old woman was referred to a tertiary-level hospital at 25th weeks’ gestation for evaluation of a suspected fetal heart defect. Persistent right umbilical vein of the extrahepatic type, cardiomegaly with predominant atrial enlargement, a primum atrial septal defect, and hydropericardium were diagnosed. At 33 + 5 weeks of gestation, signs of decompensation emerged, including progressive cardiomegaly, hydropericardium, and newly developed ascites, leading to the decision to induce labor. Imaging was performed using a Voluson E8 ultrasound system (GE Healthcare, Zipf, Austria). Despite all efforts, the severity of the condition ultimately proved fatal in this clinical case. Conclusions: Patients carrying fetuses suspected or diagnosed with PRUV should receive coordinated management by a multidisciplinary team of specialists. Delivery should be planned in a tertiary-level hospital.
Full article
Open AccessArticle
Hemodynamic Comparison of Inferior Vena Cava Collapsibility Index in Patients with Preeclampsia vs. Controls: A Pilot Study
by
Rachael Sampson, Patricia Rojas Mendez and Viren Kaul
Reprod. Med. 2025, 6(4), 35; https://doi.org/10.3390/reprodmed6040035 - 1 Nov 2025
Abstract
►▼
Show Figures
Background/Objectives: There is a paucity of research studying point-of-care ultrasound in the pregnant population, despite the rising incidence of maternal medical complications and, in particular, preeclampsia. This study sought to compare the inferior vena cava collapsibility index (IVC-CI) between patients with preeclampsia with
[...] Read more.
Background/Objectives: There is a paucity of research studying point-of-care ultrasound in the pregnant population, despite the rising incidence of maternal medical complications and, in particular, preeclampsia. This study sought to compare the inferior vena cava collapsibility index (IVC-CI) between patients with preeclampsia with severe features (PECS) and gestational age-matched controls and to assess whether pulse pressure (PP) correlates with IVC-CI in PECS. Methods: This was a prospective pilot study of patients recruited at an inpatient hospital and an outpatient office. The case group included admitted patients with a diagnosis of PECS considered to be stable for prolonged antepartum expectant management. One patient per gestational age week from 23 to 34 weeks with PECS was compared to a gestational age-matched patient without any form of preeclampsia and/or gestational hypertension. Patients on magnesium sulfate, those with multiple gestation, large-for-gestational age fetus, fetal growth restriction, polyhydramnios, oligohydramnios, and/or an anomalous fetus were excluded. Results: IVC-CI was significantly lower in the PECS group compared with controls (mean 20.1% vs. 48.3%, 95% CI = −0.40–−0.16, p < 0.001). There was an inverse relationship between IVC-CI and pulse pressure in patients with PECS. For each additional 1 mmHg in pulse pressure, the odds of having IVC-CI greater than 50% decreased by 13%. Conclusions: Patients with preeclampsia exhibit detectable changes in inferior vena cava diameter that can be assessed with bedside ultrasound and correlated with maternal PP. Future research should focus on validating these findings and exploring the clinical significance of these measurements.
Full article

Figure 1
Open AccessArticle
Evaluating the Impact of Intralipid Infusion on Pregnancy Outcomes in Infertility Treatments: A Retrospective Study
by
Shajna Kinarulla Kandi, Osama Oro Shareef, Abdelrahim Obeid, Mandy Abushama, Badreldeen Ahmed and Justin C. Konje
Reprod. Med. 2025, 6(4), 34; https://doi.org/10.3390/reprodmed6040034 - 1 Nov 2025
Abstract
Background: Infertility is a multifactorial condition that causes significant emotional distress and financial burden for couples. Despite advances in assisted reproductive technologies (ARTs), many patients experience recurrent implantation failure (RIF) or pregnancy loss. Intralipid, an intravenous lipid emulsion, has been proposed as
[...] Read more.
Background: Infertility is a multifactorial condition that causes significant emotional distress and financial burden for couples. Despite advances in assisted reproductive technologies (ARTs), many patients experience recurrent implantation failure (RIF) or pregnancy loss. Intralipid, an intravenous lipid emulsion, has been proposed as an adjunctive therapy due to its immune-modulatory effects, particularly in reducing elevated natural killer (NK) cell activity, which may be associated with poor reproductive outcomes. This study evaluated the effect of intralipid infusion on pregnancy rates and miscarriage rates in women with recurrent implantation failure undergoing in vitro fertilization (IVF). Materials and Methods: This was a retrospective study of women who had suffered from recurrent implantation failure and underwent IVF between September 2023 and September 2024. A comparative group undergoing IVF but who did not have recurrent implantation failure matched for age was selected. Outcomes of clinical pregnancy, miscarriage and livebirth rates were compared in both groups. Results: A total of 113 women undergoing IVF were identified and 51 received intralipid. Intralipid was initiated at varying stages of the IVF process, a day before embryo transfer (ET) (18 or 35.3%), on the day of ET (20 or 39.2%) and after ET (13 or 25.5%). The clinical pregnancy rate was 44.2% in the treatment group compared to 29% in the comparator group (p < 0.05) while the miscarriage rates were 13.7% versus 11.3% (p > 0.05). Elevated NK cells were present in 65.4% of the patients who received intralipid, but the correlation between NK cell levels and pregnancy outcomes was weak (Spearman ρ = 0.032). No adverse effects were reported in any of the women. Conclusions: Intralipid infusion increased the successful pregnancy rates in women who had recurrent implantation failure during IVF. The successful pregnancy rate was significantly higher than that in those undergoing ART who had not suffered from RIF. These findings support several studies on the potential benefit and safety of intralipids in women undergoing ART, but the numbers remain small and more prospective studies are needed to confirm these findings
Full article
Open AccessArticle
Exploring the Link Between Vaginal Delivery and Postpartum Dyspareunia: An Observational Study
by
Rebecca Rachel Zachariah, Susanne Forst, Nikolai Hodel and Verena Geissbuehler
Reprod. Med. 2025, 6(4), 33; https://doi.org/10.3390/reprodmed6040033 - 1 Nov 2025
Abstract
►▼
Show Figures
Background/Objective: Dyspareunia negatively affects women’s lives. Up to 35% suffer from postpartum dyspareunia. Many factors may influence the occurrence of postpartum dyspareunia, but little is known about them. This study aimed to look at the frequency of dyspareunia one year postpartum in a
[...] Read more.
Background/Objective: Dyspareunia negatively affects women’s lives. Up to 35% suffer from postpartum dyspareunia. Many factors may influence the occurrence of postpartum dyspareunia, but little is known about them. This study aimed to look at the frequency of dyspareunia one year postpartum in a cohort of primiparae. Which perinatal factors influence the frequency of postpartum dyspareunia? Methods: A total of 3264 primiparae were included in this observational cohort study. Perinatal factors were documented, and a specially designed questionnaire was sent to them one year postpartum. The primary outcome was the frequency of dyspareunia one year postpartum. The secondary outcomes included potential influencing factors such as birthing method (spontaneous bed delivery, spontaneous delivery other than bed, water delivery, and vacuum-assisted delivery); perineal injuries (first- and second-degree perineal tears, obstetric anal sphincter injuries (OASIs), and episiotomies); and the use of oxytocin. Results: Postpartum dyspareunia was observed in 15% of the 3264 primiparae. In multivariate analysis, there were influences found in the perineal injury group, especially for first- and second-degree perineal tears and OASIs. In the oxytocin group, a trend toward a higher rate of postpartum dyspareunia was observed. No influence of the different birthing methods was found. Conclusions: Postpartum dyspareunia, affecting 15% of women one year after vaginal delivery, is associated with perineal injuries, particularly minor perineal tears and OASIs. This highlights the importance of good preparation of the perineum and pelvic floor before delivery, efficient perineal protection during labor, and the use of a precise repair technique for all perineal injuries.
Full article

Figure 1
Open AccessArticle
Assessing Thrombophilic Risk via Placental Histopathology: A Comparative Scoring Analysis
by
Viorela-Romina Murvai, Anca Huniadi, Radu Galiș, Gelu Florin Murvai, Brenda-Cristiana Bernad, Carmen Ioana Marta, Timea Claudia Ghitea and Ioana Cristina Rotar
Reprod. Med. 2025, 6(4), 32; https://doi.org/10.3390/reprodmed6040032 - 1 Nov 2025
Abstract
►▼
Show Figures
Introduction: Maternal thrombophilia is associated with numerous obstetric complications, often occurring without overt clinical manifestations during pregnancy. Histological evaluation of the placenta can provide valuable insights into the etiology of these complications. Objective: To compare the placental histopathological profile in pregnancies
[...] Read more.
Introduction: Maternal thrombophilia is associated with numerous obstetric complications, often occurring without overt clinical manifestations during pregnancy. Histological evaluation of the placenta can provide valuable insights into the etiology of these complications. Objective: To compare the placental histopathological profile in pregnancies with thrombophilia versus physiological pregnancies and to develop a synthetic score capable of retrospectively indicating thrombophilic risk. Materials and Methods: A retrospective observational study was conducted on two groups (n = 80 thrombophilia, n = 31 control). Macroscopic and histopathological placental parameters were analyzed. A histological score (range 0–5 points) was constructed based on the presence of villous stasis, stromal fibrosis, infarction, acute atherosis, and intervillous thrombosis. Results: The mean histological score was significantly higher in the thrombophilia group (2.20 ± 1.4) compared to the control group (1.18 ± 1.1; p = 0.0011). A score ≥ 3 was present in 39.1% of thrombophilic cases versus 13.6% in controls. Regression analysis showed that only placental diameter was significantly correlated with the histological score (p = 0.0379). Conclusions: The proposed histological score may serve as a simple and effective tool for the indirect identification of potential thrombophilic risk in complicated pregnancies. Its validation in future studies could support its implementation in routine obstetric and histopathological practice.
Full article

Figure 1
Open AccessSystematic Review
Development and Clinical Significance of the Human Fetal Adrenal Gland as a Key Component of the Feto-Placental System: A Systematic Review
by
Martiniuc Ana-Elena, Laurentiu-Camil Bohiltea, Pop Lucian Gheorghe and Suciu Nicolae
Reprod. Med. 2025, 6(4), 31; https://doi.org/10.3390/reprodmed6040031 - 13 Oct 2025
Abstract
►▼
Show Figures
Background: The human fetal adrenal gland is a unique endocrine organ with distinct morphology and functional dynamics, which is significantly different from the postnatal adrenal. Its rapid growth and vital steroidogenic role during gestation have positioned it as a key regulator of fetal
[...] Read more.
Background: The human fetal adrenal gland is a unique endocrine organ with distinct morphology and functional dynamics, which is significantly different from the postnatal adrenal. Its rapid growth and vital steroidogenic role during gestation have positioned it as a key regulator of fetal development and pregnancy maintenance. Objectives: To provide a comprehensive overview of the morphogenesis, function, regulatory mechanisms, and clinical implications of the human fetal adrenal gland, highlighting recent advances in understanding its development and its role in prenatal and postnatal health outcomes. Methods: A systematic review was conducted, including original research articles focused on human fetuses or validated animal models, examining the genetic, molecular, and hormonal mechanisms underlying adrenal development and function. Studies were excluded if they were editorials, case reports, focused on adult adrenal physiology, had small sample sizes, or were non-English publications. Study quality was evaluated using PRISMA guidelines. Results: The fetal adrenal gland develops from both mesodermal and ectodermal origins, forming three primary zones: fetal, transitional, and definitive. Each zone has distinct functions and developmental pathways. The fetal zone, which predominates, is responsible for producing dehydroepiandrosterone sulfate, DHEA-S, which is crucial for placental estrogen synthesis. The adrenal gland undergoes rapid growth and functional maturation, regulated by ACTH, placental CRH, IGF, and the renin–angiotensin system. Disruption of adrenal function is associated with conditions such as preterm birth, adrenal hypoplasia, congenital adrenal hyperplasia, and intrauterine growth restriction. Emerging evidence suggests that fetal adrenal hormones may influence long-term health through fetal programming mechanisms. Conclusions: The fetal adrenal gland plays a critical and multifaceted role in fetal and placental development. This gland influences placental development via steroid precursors (DHEA-S → estrogen synthesis), while also being regulated by placental factors such as the corticotropin-releasing hormone. Understanding its complex structure–function relationships and regulatory networks is essential for predicting and managing prenatal and postnatal pathologies. Future research should focus on elucidating molecular mechanisms, improving diagnostic tools, and exploring long-term outcomes of altered fetal adrenal function.
Full article

Figure 1
Open AccessReview
Telemedicine in Obstetrics: Building Bridges in Reproductive Healthcare—A Literature Review
by
Zahi Hamdan, Rhianon Bou Deleh, Joenne Al Khoury, Somar Soufan, Rafi Haddad, Emile Dabaj, Sami Azar, Hilda E. Ghadieh and Marouan Zoghbi
Reprod. Med. 2025, 6(4), 30; https://doi.org/10.3390/reprodmed6040030 - 9 Oct 2025
Abstract
Telemedicine has emerged as a promising tool in obstetric and reproductive healthcare, offering new possibilities for patient-centered care delivery. This literature review explores its impact across key areas, including abortion, assisted reproduction, childbirth, contraception, gestational diabetes, mental health, opioid and smoking cessation, and
[...] Read more.
Telemedicine has emerged as a promising tool in obstetric and reproductive healthcare, offering new possibilities for patient-centered care delivery. This literature review explores its impact across key areas, including abortion, assisted reproduction, childbirth, contraception, gestational diabetes, mental health, opioid and smoking cessation, and perinatal care during the COVID-19 pandemic. A structured narrative approach was applied, with studies identified through PubMed and Scopus databases for screening, with selection based on predefined inclusion and exclusion criteria, and synthesized narratively with attention to clinical outcomes, access, satisfaction, and barriers to implementation. Perspectives on the acceptance of telemedicine among healthcare providers, technological advancements enhancing reproductive outcomes, and telemedicine’s pivotal role in maintaining continuity of care during crises, such as the COVID-19 pandemic, are examined. The review also addresses challenges and barriers, including technological proficiency and patient acceptance, while emphasizing telemedicine’s potential to improve accessibility, patient satisfaction, and healthcare outcomes across diverse reproductive health services.
Full article
Open AccessSystematic Review
Adiponectin as a Biomarker of Preeclampsia: A Systematic Review
by
Inês Carrilho, Melissa Mariana and Elisa Cairrao
Reprod. Med. 2025, 6(4), 29; https://doi.org/10.3390/reprodmed6040029 - 7 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Classified as a hypertensive disorder of pregnancy, preeclampsia is one of the leading causes of maternal and fetal morbidity and mortality. The abnormal trophoblast invasion that leads to a failed transformation of the uterine spiral arteries during placentation remains the most probable
[...] Read more.
Background/Objectives: Classified as a hypertensive disorder of pregnancy, preeclampsia is one of the leading causes of maternal and fetal morbidity and mortality. The abnormal trophoblast invasion that leads to a failed transformation of the uterine spiral arteries during placentation remains the most probable cause for preeclampsia. It is known that adiponectin acts on the placenta, playing a regulatory role in placentation processes. Therefore, the aim of this systematic review is to compile scientific evidence to evaluate the role of adiponectin as a biomarker for preeclampsia. Methods: The protocol for this systematic review was registered on the PROSPERO database (ID CRD42024542403) and follows the PRISMA 2020 guidelines. Overall, twenty-nine studies were selected from the PubMed and Scopus databases, including case–control, prospective and retrospective cohort, cross-sectional, and bidirectional Mendelian randomization studies. Results: From the articles analyzed, nine studies indicated an increase in adiponectin levels in preeclampsia, eleven reported a decrease, eight detected no significant changes, and in two studies, it was not possible to determine the glycoprotein levels. Analysis of the evidence quality revealed that moderate and low evidence levels predominate, with stronger evidence for decreased adiponectin levels. Conclusions: Promoting the advancement of scientific research is crucial, particularly exploring the association between adiponectin and other biomarkers. This approach could facilitate the development of screening and diagnostic methods, enabling the implementation of specific preventive and therapeutic strategies.
Full article

Figure 1
Open AccessReview
Addressing Common Oral Contraceptive Pill Concerns for the Primary Care Provider
by
Amelia C. Inclan, Danielle Snyder, Sophie G. Tillotson, Katelyn E. Flaherty, Angelica Byrd, Alyssa Pasvantis and Charlotte Chaiklin
Reprod. Med. 2025, 6(4), 28; https://doi.org/10.3390/reprodmed6040028 - 4 Oct 2025
Abstract
►▼
Show Figures
Primary care providers are increasingly tasked with providing basic gynecologic care, including contraceptive therapy, to their patients. In the United States, oral contraceptive pills are the most frequently prescribed form of contraception; thus, it is critical that primary care providers are well versed
[...] Read more.
Primary care providers are increasingly tasked with providing basic gynecologic care, including contraceptive therapy, to their patients. In the United States, oral contraceptive pills are the most frequently prescribed form of contraception; thus, it is critical that primary care providers are well versed in addressing common patient questions. Well-documented concerns relating to oral contraception initiation include changes in weight, mood, cancer risk, libido, acne, and infertility. Herein, we provide a clinical case example of a patient with these common concerns, review the related evidence, and suggest appropriate counseling with the goal of helping primary care clinicians provide the highest level of evidence-based oral contraceptive care.
Full article
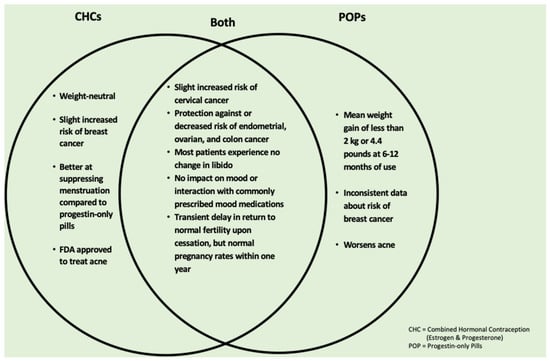
Figure 1
Open AccessCase Report
Laparoscopic Management of Hemoperitoneum Due to a Cornual Pregnancy After an Ipsilateral Tubal Pregnancy: A Case Report
by
Raffaele Tinelli, Federica Savasta, Stefano Angioni, Giorgio Bogani, Livio Leo, Alessandro Messina and Alessandro Libretti
Reprod. Med. 2025, 6(4), 27; https://doi.org/10.3390/reprodmed6040027 - 2 Oct 2025
Abstract
Background: Cornual pregnancy (CP) is a rare but life-threatening form of ectopic pregnancy. Severe complications include uterine rupture and massive hemorrhage, often requiring complex surgical management despite prompt intervention. We report a case of a ruptured left CP at 12 weeks, occurring three
[...] Read more.
Background: Cornual pregnancy (CP) is a rare but life-threatening form of ectopic pregnancy. Severe complications include uterine rupture and massive hemorrhage, often requiring complex surgical management despite prompt intervention. We report a case of a ruptured left CP at 12 weeks, occurring three months after ipsilateral salpingectomy for a tubal pregnancy. Case Presentation: A 27-year-old woman, gravida 2, with a history of left salpingectomy, presented at 12 weeks of amenorrhea with severe pelvic pain and irregular uterine bleeding. Clinical examination, serum β-hCG testing, and transvaginal ultrasound confirmed hemoperitoneum due to rupture of a cornual pregnancy. Emergency laparoscopy was performed, with drainage of massive hemoperitoneum, excision of the ectopic gestation, and uterine wall repair. Uterine integrity was preserved, and the patient was discharged without complications. Discussion: Cornual ectopic pregnancy remains diagnostically and surgically challenging, with high risk of catastrophic hemorrhage. Transvaginal ultrasonography, supported by 3D ultrasound or MRI in equivocal cases, facilitates early diagnosis. Laparoscopy is increasingly recognized as the gold standard, offering reduced morbidity, faster recovery, and preservation of fertility compared with laparotomy, though it requires advanced surgical expertise. Long-term follow-up is essential due to the risk of uterine rupture in subsequent pregnancies, and elective cesarean delivery is often advised. Conclusion: This case demonstrates that minimally invasive laparoscopic management of ruptured CP with massive hemoperitoneum is feasible and safe when performed by experienced surgeons, but further studies are needed to optimize standardized protocols and assess reproductive outcomes.
Full article
(This article belongs to the Special Issue Pathology and Diagnosis of Gynecologic Diseases, 3rd Edition)
Open AccessReview
Treatment of Type 1 Diabetes Mellitus During Pregnancy Using an Insulin Pump with an Advanced Hybrid Closed-Loop System: A Narrative Review
by
Ingrid Dravecká
Reprod. Med. 2025, 6(4), 26; https://doi.org/10.3390/reprodmed6040026 - 25 Sep 2025
Abstract
►▼
Show Figures
Pregnancy in women with type 1 diabetes mellitus (T1DM) is associated with a high risk of maternal and perinatal complications, and achieving optimal glycaemic control remains a clinical challenge. This article presents a narrative review of the evidence on advanced hybrid closed loop
[...] Read more.
Pregnancy in women with type 1 diabetes mellitus (T1DM) is associated with a high risk of maternal and perinatal complications, and achieving optimal glycaemic control remains a clinical challenge. This article presents a narrative review of the evidence on advanced hybrid closed loop (AHCL) insulin delivery systems in pregnancy, with a focus on maternal glycaemic outcomes, neonatal outcomes, and psychosocial aspects. The relevant literature was identified through a structured search of PubMed, Scopus, and Web of Science (2010–2025), supplemented by guideline documents and reference screening. Eligible studies included randomised controlled trials, observational studies, and qualitative investigations. Data were synthesised thematically. Findings from key trials, including CONCEPTT, AiDAPT, and CRISTAL, demonstrate that AHCL systems improve time in range, lower mean glucose, and reduce hyperglycaemia without increasing hypoglycaemia. Some evidence also suggests improved neonatal outcomes, though statistical significance varies. Qualitative studies highlight reduced anxiety, improved sleep, and enhanced quality of life for women using AHCL during pregnancy. In conclusion, AHCL systems show strong promise in optimising maternal glycaemic control and potentially improving perinatal outcomes. However, larger, unbiased studies and real-world evaluations are needed to confirm their benefits and support broader clinical implementation.
Full article

Figure 1
Open AccessArticle
The Role of the Setting in Controlling Anxiety and Pain During Outpatient Operative Hysteroscopy: The Experience of a Hysteroscopy Unit in North Italy
by
Alessandro Messina, Alessio Massaro, Eleonora Dalmasso, Ilaria Giovannini, Giovanni Lipari, Paolo Alessi, Tiziana Bruno, Sofia Vegro, Daniela Caronia, Federica Savasta, Valentino Remorgida, Alessandro Libretti and Bianca Masturzo
Reprod. Med. 2025, 6(3), 25; https://doi.org/10.3390/reprodmed6030025 - 12 Sep 2025
Abstract
Background/Objectives: Outpatient operative hysteroscopy is a cornerstone in the management of intrauterine pathologies within reproductive medicine. However, procedural pain and anxiety remain key barriers leading to failed procedures and referrals for surgery under general anesthesia. This study aimed to assess whether a comfort-enhanced
[...] Read more.
Background/Objectives: Outpatient operative hysteroscopy is a cornerstone in the management of intrauterine pathologies within reproductive medicine. However, procedural pain and anxiety remain key barriers leading to failed procedures and referrals for surgery under general anesthesia. This study aimed to assess whether a comfort-enhanced procedural environment could reduce perceived pain and increase procedural success rates. Methods: Analysis of 970 consecutive patients who underwent outpatient operative hysteroscopy at the Hysteroscopy Unit of “Degli Infermi” Hospital (Biella, Italy): 470 in 2023 under standard conditions, 500 in 2024 with an enhanced setting. Surgical technique, analgesic/sedation policies and operators were unchanged. The primary outcome was referral to the OR for completion of the procedure. Secondary outcomes included patient-reported pain assessed by Visual Analog Scale (VAS) in a consecutive subsample. Differences between years were evaluated with appropriate parametric/non-parametric tests. Results: Implementation of the enhanced environment was associated with a lower OR referral rate in 2023 versus 2024. Post hoc power for this comparison was approximately 60%. Mean VAS scores also decreased in 2024, with post hoc power >99%. No adverse events were recorded. Conclusions: Environmental and interpersonal modifications were associated with meaningful decline in reported pain and OR referrals. Prospective studies incorporating systematic case-mix and validated anxiety measures are warranted to confirm these results.
Full article
(This article belongs to the Special Issue Pathology and Diagnosis of Gynecologic Diseases, 3rd Edition)
►▼
Show Figures

Figure 1
Open AccessArticle
Possibilities of Titanium Nickelide Implant Application in Radical Trachelectomy in Patients of Reproductive Age with Invasive Cervical Cancer
by
Alyona Chernyshova, Michael Krylyshkin, Alexander Chernyakov, Julia Truschuk, Ekaterina S. Marchenko, Sergey Fursov, Olga Tkachuk and Svetlana Tamkovich
Reprod. Med. 2025, 6(3), 24; https://doi.org/10.3390/reprodmed6030024 - 10 Sep 2025
Abstract
►▼
Show Figures
Objectives: The aim of this study is to demonstrate the efficacy of the modified technique of radical organ-preserving surgery of invasive cervical cancer (CC) in patients of reproductive age. Methods: This study included 118 patients of reproductive age (34.9 ± 4.8
[...] Read more.
Objectives: The aim of this study is to demonstrate the efficacy of the modified technique of radical organ-preserving surgery of invasive cervical cancer (CC) in patients of reproductive age. Methods: This study included 118 patients of reproductive age (34.9 ± 4.8 years) with a morphologically verified diagnosis of invasive CC (T1a-1bNxM0). All patients underwent organ-preserving surgery in the scope of radical trachelectomy. A shape memory mesh implant woven in the form of a stocking from superelastic nickelide titanium thread with subsequent fixation with separate sutures around the perimeter was used to form the uterine closure apparatus and to strengthen the utero-vaginal anastomosis. The mesh implant was made of superelastic thin nickelide titanium threads with a diameter of 60–40 microns on a metal knitting machine. All patients were prospectively followed up for a mean of 120 months. Results: No intraoperative or postoperative complications were revealed when using a shape memory implant made of titanium nickelide during radical trachelectomy to form a locking apparatus and strengthen the anastomosis zone. No cervical stenoses or mesh failures were noted in any case. The 5-year overall and recurrence-free survival rates were 100% and 98%, respectively. Two patients indicated recurrence; it occurred in 3 and 36 months. There were 42 spontaneous pregnancies, and 29 resulted in full-term delivery, whereas 2 and 11 ended in miscarriage and early abortion, respectively. Currently, 18 patients are at different stages of the use of assisted reproductive technologies. Conclusions: The shape memory implant made of titanium nickelide integrates well into the surrounding tissues and successfully imitates the effect of the cervix. The use of this sparing-surgery technique has shown reasonably good results in carrying the pregnancy to term and good reproductive outcomes.
Full article

Figure 1
Open AccessArticle
Self-Reported Use and Effectiveness of Marijuana for Pelvic Pain Among Women with Endometriosis
by
Anna E. Reinert, Maria Bolshakova, Alexander S. Wong and Victoria K. Cortessis
Reprod. Med. 2025, 6(3), 23; https://doi.org/10.3390/reprodmed6030023 - 8 Sep 2025
Abstract
►▼
Show Figures
Background/Objectives: Legal access to cannabinoids is increasing, and patients with chronic pelvic pain from endometriosis were hypothesized to explore and find benefit from the use of marijuana for symptom management. A survey of women with endometriosis was conducted with the objective of characterizing
[...] Read more.
Background/Objectives: Legal access to cannabinoids is increasing, and patients with chronic pelvic pain from endometriosis were hypothesized to explore and find benefit from the use of marijuana for symptom management. A survey of women with endometriosis was conducted with the objective of characterizing their experience with marijuana for management of pelvic pain: exploring symptom benefit, characteristics of use, and factors contributing to use and discontinuation. Methods: A descriptive cross-sectional survey was undertaken using an anonymous online questionnaire. Participants were recruited from an outpatient gynecology clinic using endometriosis ICD-10 diagnostic codes, and from the Endometriosis Association mailing list. Results: Marijuana use for symptom relief was reported by 78 (32.2%) Endometriosis Association participants, and 58 (46.8%) clinic participants. Within both populations, marijuana was considered very or moderately effective by most users (68.0 to 75.9%). Legality of recreational and medicinal marijuana in the state of residence was strongly associated with use (OR 7.13 [95% CI: 2.57–19.8]). Among users specifying current or past use, discontinuation was reported by 45% (54 of 121), and most frequently attributed to non-clinical factors of legal/employment risk and obstacles to marijuana access; 64.8% of former users attributed discontinuation to non-clinical factors only. Lack of symptom relief from other clinical management was the most cited motivation for initiation (55.1% clinic, 39.7% EA users). Conclusions: Marijuana use is common among women with endometriosis and chronic, refractory pelvic pain. Legality and access appear to impact use and discontinuation. While legal access to marijuana is associated with increased use, marijuana obtained outside of legal routes is also commonly being used for symptom relief.
Full article

Figure 1
Open AccessSystematic Review
Exploring the Role of Anti-Adhesion Gel in Outpatient Operative Hysteroscopy
by
Alessandro Messina, Safae El Motarajji, Ilaria Giovannini, Alessandro Libretti, Federica Savasta, Valentino Remorgida, Livio Leo and Bianca Masturzo
Reprod. Med. 2025, 6(3), 22; https://doi.org/10.3390/reprodmed6030022 - 28 Aug 2025
Abstract
Background: Outpatient operative hysteroscopy is a minimally invasive procedure widely used for the diagnosis and treatment of intrauterine pathologies, including intrauterine adhesions (IUAs), which significantly affect fertility. Despite its therapeutic potential, the procedure itself may predispose patients to de novo adhesion formation. This
[...] Read more.
Background: Outpatient operative hysteroscopy is a minimally invasive procedure widely used for the diagnosis and treatment of intrauterine pathologies, including intrauterine adhesions (IUAs), which significantly affect fertility. Despite its therapeutic potential, the procedure itself may predispose patients to de novo adhesion formation. This review evaluates the effectiveness of anti-adhesion gels, particularly hyaluronic-acid-based formulations, in preventing IUAs and improving reproductive outcomes after outpatient operative hysteroscopy. Materials and Methods: A systematic search was performed in PubMed, CINAHL, Embase, and Web of Science for studies published between January 2020 and May 2025. Inclusion and exclusion criteria were defined using PICO guidelines. Relevant studies were screened and selected by two independent reviewers. Results: Anti-adhesion gels, especially hyaluronic acid and its derivatives, were associated with a lower recurrence of IUAs and improved reproductive outcomes. Combination therapies, such as hyaluronic acid gel with intrauterine devices (IUDs), showed better efficacy than monotherapy. Several studies also reported increased endometrial thickness, higher implantation rates, and improved pregnancy outcomes, although live birth rates remained inconsistent. Conclusions: Hyaluronic-acid-based anti-adhesion gels appear effective in reducing postoperative adhesion formation and enhancing reproductive outcomes in outpatient hysteroscopy. The best results are seen with multimodal preventive strategies. However, heterogeneity across studies highlights the need for standardized, prospective, randomized controlled trials to establish optimal clinical use.
Full article
(This article belongs to the Special Issue Pathology and Diagnosis of Gynecologic Diseases, 3rd Edition)
►▼
Show Figures

Graphical abstract
Open AccessCase Report
Outpatient Hysteroscopic Treatment of Cervical Ectopic Pregnancy in a Primigravida Using the Ho:YAG Laser: A Case Report and Operative Protocol Evaluation
by
Dimitar Cvetkov, David Lukanovic and Angel Yordanov
Reprod. Med. 2025, 6(3), 21; https://doi.org/10.3390/reprodmed6030021 - 27 Aug 2025
Cited by 1
Abstract
►▼
Show Figures
Background and Clinical Significance: Cervical ectopic pregnancy (CEP) is a rare and potentially serious condition, in which the embryo implants within the cervical canal rather than the uterine cavity and is present in less than 1% of all ectopic pregnancies. There are
[...] Read more.
Background and Clinical Significance: Cervical ectopic pregnancy (CEP) is a rare and potentially serious condition, in which the embryo implants within the cervical canal rather than the uterine cavity and is present in less than 1% of all ectopic pregnancies. There are different treatment options depending on the particular situation and the woman’s reproductive desire but conservative approaches as the first line of treatment is preferred in all cases and hysteroscopic resection of the fetus is one of these options. Several types of laser systems are available for use in hysteroscopic surgery, including neodymium:YAG (Nd:YAG) lasers, KTP and Argon lasers, as well as diode lasers. The holmium:YAG (Ho:YAG) laser, although more commonly used in urology due to its ability to cut, coagulate, and vaporize tissue, has gained interest in gynecologic procedures because of its precision and favorable safety profile. Case Presentation: We present the case of a 32-year-old woman, pregnant for the first time, who was diagnosed with CEP and successfully treated using a Ho:YAG laser during an outpatient hysteroscopic procedure. As far as we know, this is the first published case using this approach. Conclusions: The Ho:YAG laser is a proven tool for outpatient hysteroscopic procedures like septum and adhesion removal. Its ability to both cut and coagulate offers a minimally invasive, fertility-sparing option for managing cervical ectopic pregnancy. With the right patient and proper backup plans in place, this approach could be a promising alternative to more aggressive treatments.
Full article

Figure 1
Open AccessArticle
Exploring Pregnancy-Related Acute Kidney Injury: Risk Factors and Maternal Outcomes in High-Risk Women in Mwanza, Tanzania
by
Kahibi Bernard, Fridolin Mujuni, Dismas Matovelo, Edgar Ndaboine, Richard Kiritta and Ladius Rudovick
Reprod. Med. 2025, 6(3), 20; https://doi.org/10.3390/reprodmed6030020 - 19 Aug 2025
Abstract
►▼
Show Figures
Background/Objective: Pregnancy-related acute kidney injury (PRAKI) remains a serious complication, with high rates of maternal morbidity and mortality, particularly in developing countries where delayed diagnosis and treatment are common. This study aimed to determine the proportion, associated risk factors, and maternal outcomes
[...] Read more.
Background/Objective: Pregnancy-related acute kidney injury (PRAKI) remains a serious complication, with high rates of maternal morbidity and mortality, particularly in developing countries where delayed diagnosis and treatment are common. This study aimed to determine the proportion, associated risk factors, and maternal outcomes among pregnant and postpartum women at high risk of developing AKI. Methods: This cross-sectional analytical study was conducted at Bugando Medical Centre in Mwanza, Tanzania, from May 2023 to February 2024, targeting high-risk obstetric patients. Results: Out of 4588 admissions, 420 patients were identified as being at risk of developing PRAKI. Among them, 101 (24.22%) were diagnosed with PRAKI, while 316 (75.78%) did not develop the condition. The leading associated risk factors were pre-eclampsia (40.59%) and postpartum hemorrhage (PPH) (40.24%), followed by sepsis (11.8%) and abortion-related complications (5.94%). Multivariate analysis revealed that living in rural areas and having a lower level of education were significantly associated with PRAKI. Patients from rural areas had an adjusted odds ratio (AOR) of 5.37 (p < 0.001), while those with informal or primary education had an AOR of 4.21 (p = 0.048). Conclusions: The study also found that maternal mortality was significantly higher among patients with PRAKI, particularly those affected by PPH. These findings highlight the urgent need for improved management of obstetric emergencies to reduce PRAKI incidence and improve maternal outcomes in high-risk populations.
Full article

Figure 1
Open AccessArticle
Polygenic Embryo Risk Scores: A Survey of Public Perception
by
Alexandra Peyser, Cailey Brogan, Lilli Zimmerman and Randi H. Goldman
Reprod. Med. 2025, 6(3), 19; https://doi.org/10.3390/reprodmed6030019 - 31 Jul 2025
Abstract
►▼
Show Figures
Background: Preimplantation genetic testing for polygenic diseases (PGT-P) is a reproductive technology that has made it possible to assign risk scores to embryos for various complex polygenic conditions such as diabetes, hypertension, breast cancer, and schizophrenia. Whether there is public interest in utilizing
[...] Read more.
Background: Preimplantation genetic testing for polygenic diseases (PGT-P) is a reproductive technology that has made it possible to assign risk scores to embryos for various complex polygenic conditions such as diabetes, hypertension, breast cancer, and schizophrenia. Whether there is public interest in utilizing PGT-P and what public opinions are regarding this technology is unknown. Therefore, the objective of our study was to evaluate the opinion of the general United States (US) public regarding PGT-P. Methods: A web-based questionnaire consisting of 25 questions was administered to a nationally representative sample of adult US residents according to age and sex. The survey contained a description of PGT-P, followed by questions with Likert-scale responses ranging from strongly agree to strongly disagree. Results: Of the 715 respondents recruited, 673 (94%) completed the survey. Most respondents agreed that use of PGT-P is ethical (54%), and another 37% were neutral; however, approximately 9% of respondents disagreed and were opposed to the use of PGT-P. Those that opposed PGT-P cited that it was “unethical” (46%) or “not natural” (39%), believed children could be negatively affected (31%), or stated that it went against their religion (15%). The majority of respondents did not know whether PGT-P was safe for embryos (68%) or children (67%) and felt that anyone should be able to utilize it (53%). Conclusions: Participants who were younger, were Atheist, or were Democrats were more likely to agree that “PGT-P is ethical”. This study identified that more than half of respondents supported the use of PGT-P. However, concerns regarding its safety and ethical implications persist.
Full article

Figure 1
Open AccessCase Report
Cervical Cancer During Pregnancy: A Multidisciplinary Approach to a Complex Oncological Case
by
Balázs Vida, Richárd Tóth, Petra Merkely, Nándor Ács, Zoltán Novák, Boglárka Balázs, Lilla Madaras, Ferenc Bánhidy, Ádám Tabányi, Márton Keszthelyi and Balázs Lintner
Reprod. Med. 2025, 6(3), 18; https://doi.org/10.3390/reprodmed6030018 - 31 Jul 2025
Abstract
►▼
Show Figures
Background: Cervical cancer is the fourth most common malignancy among women, posing significant diagnostic and therapeutic challenges during pregnancy. Case presentation: This case report presents the treatment of a 32-year-old pregnant woman diagnosed with cervical cancer. Following the diagnosis at 7 weeks of
[...] Read more.
Background: Cervical cancer is the fourth most common malignancy among women, posing significant diagnostic and therapeutic challenges during pregnancy. Case presentation: This case report presents the treatment of a 32-year-old pregnant woman diagnosed with cervical cancer. Following the diagnosis at 7 weeks of gestation, histological and imaging examinations were performed, leading to the initiation of neoadjuvant chemotherapy. Due to the tumor progression noticed under therapy, cesarean section was performed at 29 weeks, immediately followed by radical hysterectomy. Conclusions: The management of cervical cancer during pregnancy necessitates a multidisciplinary approach, based on the patient’s condition, tumor stage, and fetal maturity. This case highlights the limitations and complexities of treating cervical cancer during pregnancy and emphasizes the importance of individualized oncological and surgical planning.
Full article

Figure 1
Open AccessCommunication
Improvement in Sperm Recovery Rate and Total Motile Sperm Count Using α-Chymotrypsin in Highly Viscous Semen Sample Without Adversely Affecting Assisted Reproductive Technology Outcomes
by
Archana Ayyar, Marian Khalil, Maggie Wong, Rebecca Chung, Kathryn Coyne, Joseph Findley, Rachel Weinerman, Rebecca Flyckt, Katelyn Perroz Sofaly and Sung Tae Kim
Reprod. Med. 2025, 6(3), 17; https://doi.org/10.3390/reprodmed6030017 - 2 Jul 2025
Abstract
►▼
Show Figures
Objectives: To investigate the impact of α-chymotrypsin treatment on sperm recovery rate and total motile sperm count (TMC) in highly viscous semen for intrauterine insemination (IUI) and in vitro fertilization (IVF), particularly in cases of severely low sperm count. Methods: High
[...] Read more.
Objectives: To investigate the impact of α-chymotrypsin treatment on sperm recovery rate and total motile sperm count (TMC) in highly viscous semen for intrauterine insemination (IUI) and in vitro fertilization (IVF), particularly in cases of severely low sperm count. Methods: High viscosity was defined by the inability to form a thread exceeding 2 cm from a semen drop after 30 min of incubation at 37 °C with repeated pipetting. Semen samples were treated with 5 mg of α-chymotrypsin for 5–10 min at 37 °C and washed using a 90% gradient solution. A total of 35 patients were included, with comparisons made to the same patients’ prior untreated samples using paired t-tests. Severely low sperm count was classified as TMC below 10 million. Results: Treatment with α-chymotrypsin significantly improved TMC (22.2 million vs. 11.6 million, p = 0.0004) and motile sperm recovery rate (38.9% vs. 16.2%, p = 0.00002). In cases of severely low sperm count, α-chymotrypsin treatment resulted in a marked increase in recovery rate (43.0% vs. 10.0%, p = 0.02) and TMC (5.89 million vs. 1.21 million, p = 0.004). Fertilization using treated samples achieved an 87.8% success rate, with a 56.4% usable blastocyst rate, comparable to standard IVF outcomes (n = 9, average age = 34.9 years). Conclusions: α-chymotrypsin treatment significantly enhances sperm recovery and TMC in highly viscous semen, demonstrating particular efficacy in patients with severely low sperm counts without affecting fertilization or blastocyst rate in IVF.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Endocrines, IJMS, JCM, Women, Reprod. Med.
Gynecological Endocrinology Updates
Topic Editors: Alessandro Genazzani, Stefano LuisiDeadline: 30 November 2025
Topic in
CIMB, IJMS, Reprod. Med., Biology, Life
Recent Research in Germ Cells
Topic Editors: Malgorzata Kloc, Jacek KubiakDeadline: 31 May 2026

Special Issues
Special Issue in
Reprod. Med.
Pathology and Diagnosis of Gynecologic Diseases, 3rd Edition
Guest Editors: Cinzia Giacometti, Mariateresa MirandolaDeadline: 31 December 2025
Special Issue in
Reprod. Med.
Application of Artificial Intelligence in Fetal Medicine
Guest Editors: Giorgio Pagani, Anna Fichera, Valentina StagnatiDeadline: 30 June 2026
Special Issue in
Reprod. Med.
Update in Reproductive Surgery
Guest Editor: Simone FerreroDeadline: 31 July 2026
Topical Collections
Topical Collection in
Reprod. Med.
Recent Advances in Preeclampsia
Collection Editor: Berthold Huppertz
Topical Collection in
Reprod. Med.
Reproductive Medicine in Europe
Collection Editor: Simone Ferrero