- Review
Beyond Clinical Features: Multidimensional Insights into Eating Behavior Disturbances in Frontotemporal Lobar Degeneration and Alzheimer’s Disease
- Serafeim Ioannidis,
- Antonios Katsarolis and
- Panagiotis Ioannidis
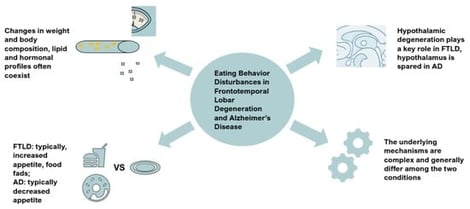
Eating behavior disturbances are increasingly recognized as clinically relevant features of dementias. Although underappreciated, such alterations affect nutritional status, metabolic state, and disease burden. Alzheimer’s disease (AD) and frontotemporal lobar degeneration (FTLD) exhibit a wide range of manifestations in eating and appetite regulation. In behavioral variant frontotemporal dementia (bvFTD), hyperorality, increased appetite, preference for sweet and high-fat foods, altered table manners, and consumption of inedible objects are common and may appear early. In contrast, AD patients usually present with decreased appetite, early dysphagia, and weight loss, although increased appetite may also occur. Beyond clinical manifestations, this review synthesizes current evidence regarding the prevalence, metabolic and hormonal profiles, and neuroimaging patterns of eating behavior disturbances in FTLD and AD, provides insight into the complex underlying mechanisms causing these changes, and underlines the lack of clear treatment strategies in these cases.
8 February 2026