Cataract Surgery and Postoperative Care – Part II
A special issue of Journal of Clinical Medicine (ISSN 2077-0383). This special issue belongs to the section "Ophthalmology".
Deadline for manuscript submissions: closed (23 May 2023) | Viewed by 31268
Special Issue Editors
2. Department of Ophthalmology, Kymenlaakso Central Hospital, 48210 Kotka, Finland
Interests: cataract surgery; corneal diseases; presbyopic-correcting surgery; registry-based studies; refractive lens exchange
Special Issues, Collections and Topics in MDPI journals
Interests: refractive surgery; optical coherence tomography; cataract surgery; phacoemulsification; posterior capsule opacification; anti-inflammatory medication; pseudophakic cystoid macular edema; quality-of-life
Special Issues, Collections and Topics in MDPI journals
Special Issue Information
Dear Colleagues,
In January 2020, the first volume of the Special Issue “Cataract Surgery and Postoperative Care” was launched (https://www.mdpi.com/journal/jcm/special_issues/Cataract_Postoperative). We received many excellent papers on cataract surgery. Now, we would like to launch the second volume on this topic.
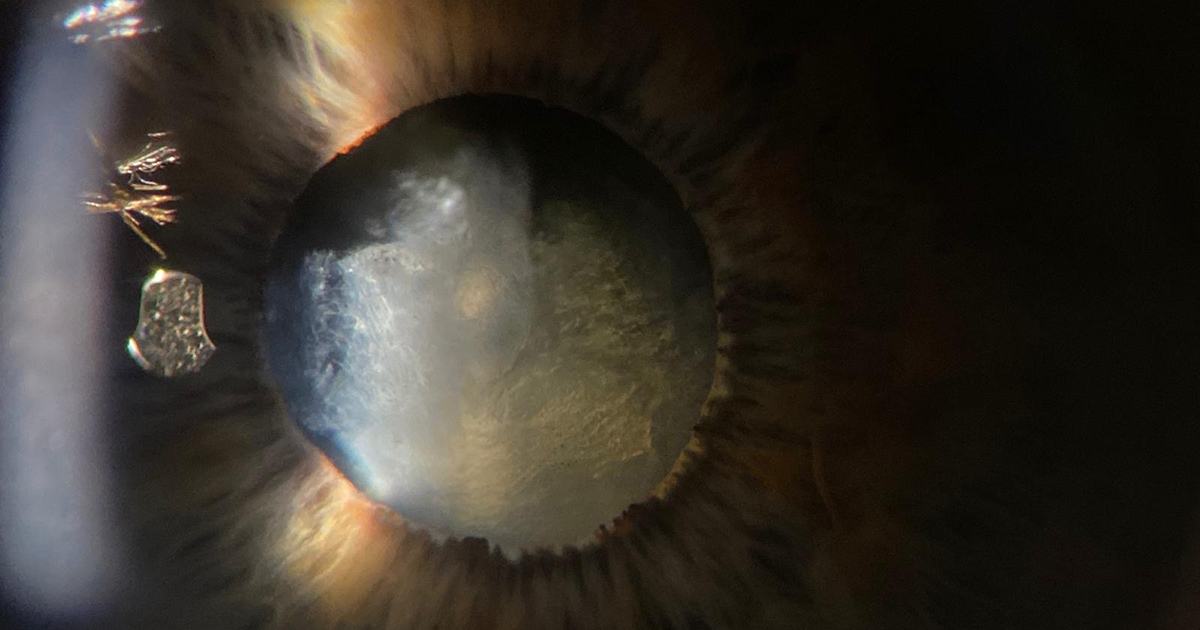
Cataract surgery is one of the most frequently performed surgical procedures in many countries. The surgical procedure itself is considered safe and efficient with good visual outcomes, and the development of modern surgical techniques and technologies has considerably reduced the frequency of complications. Furthermore, these advancements, yielding a precise postoperative refractive result, have raised the patient’s expectations for excellent uncorrected distance visual acuity. Multifocal intraocular lenses (MIOLs) are used more commonly and to a considerable extent for refractive purposes in non-cataractous eyes.
Complications are still a substantial burden because of the sheer number of cataract surgeries performed worldwide each year. Pseudophakic cystoid macular edema (PCME; Irvine–Gass syndrome) is one of the most common causes of visual impairment after cataract surgery. PCME may occur even in the absence of complications and risk factors. Intraoperative complications including capsule rupture, vitreous loss, and iris trauma are associated with a higher risk for PCME. Other risk factors include uveitis, poor glycemic control of diabetes, and various posterior segment diseases. Currently, there is no common definition for PCME; therefore, the incidences vary greatly among previously published studies.
Pre- and postsurgical medical interventions are employed in order to minimize postoperative inflammation and the risk of developing PCME. Other points of interest when comparing different anti-inflammatory drugs have been the speed of visual recovery, drug tolerability, and patient satisfaction to new treatment protocols such as “dropless” cataract surgery. Other interesting aspects involve the quality of life after RLE/MIOLs.
Achieving the best outcomes and preventing later complications requires diligent postoperative care, which also necessitates adequate patient compliance.
Dr. Raimo Tuuminen
Dr. Piotr Kanclerz
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- anti-inflammatory therapy
- aqueous flare
- cataract surgery
- complication management
- intraocular lens
- phacoemulsification
- posterior capsule opacification
- pseudophakic cystoid macular edema
- quality-of-life
- refractive lens exchange
Benefits of Publishing in a Special Issue
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- Reprint: MDPI Books provides the opportunity to republish successful Special Issues in book format, both online and in print.
Further information on MDPI's Special Issue policies can be found here.







