Nutritional Status of Iodine and Association with Iron, Selenium, and Zinc in Population Studies: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Registration of Review
2.2. Inclusion and Exclusion Criteria
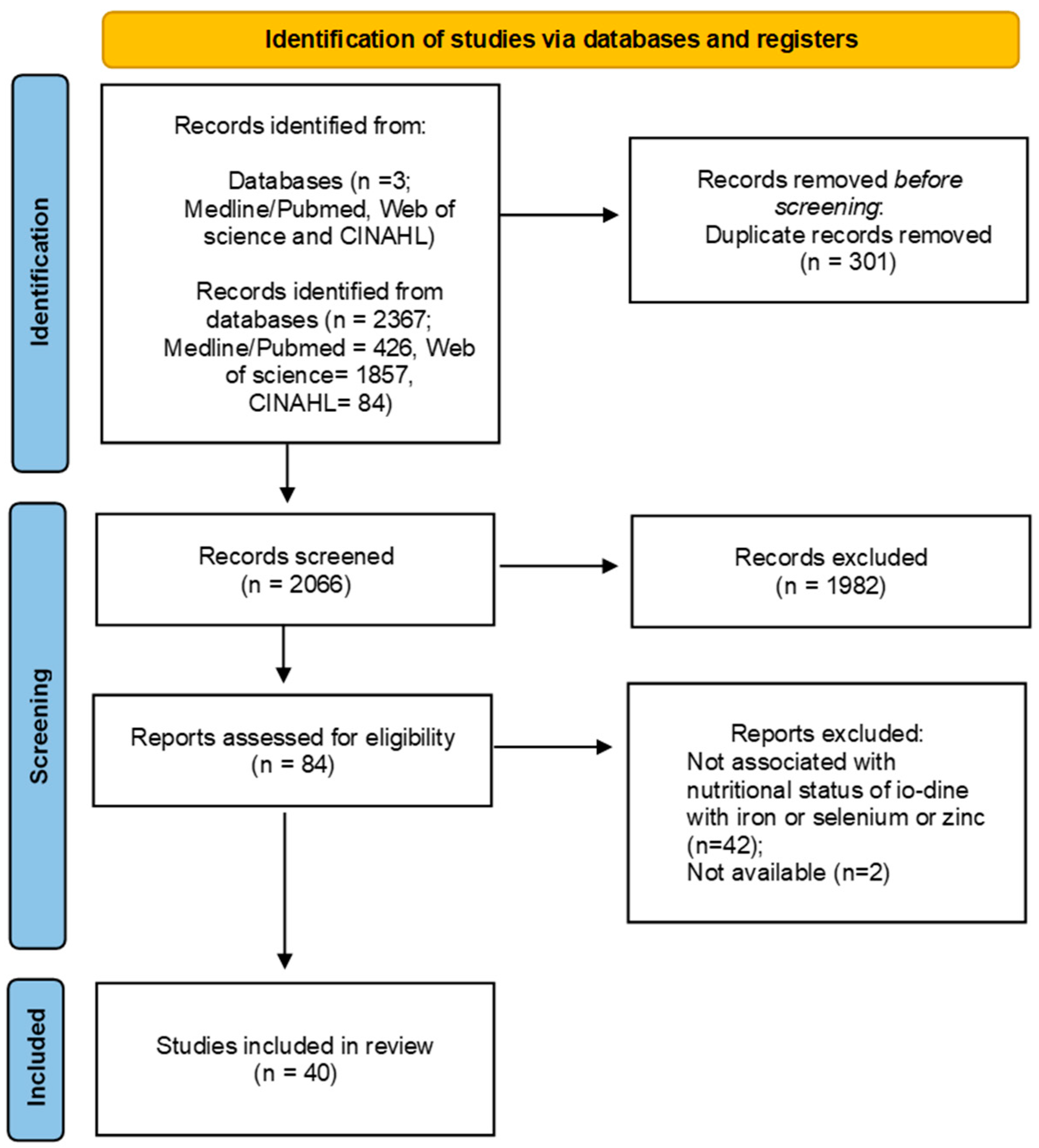
2.3. Search and Selection of Articles
2.4. Selection of Studies
2.5. Data Extraction
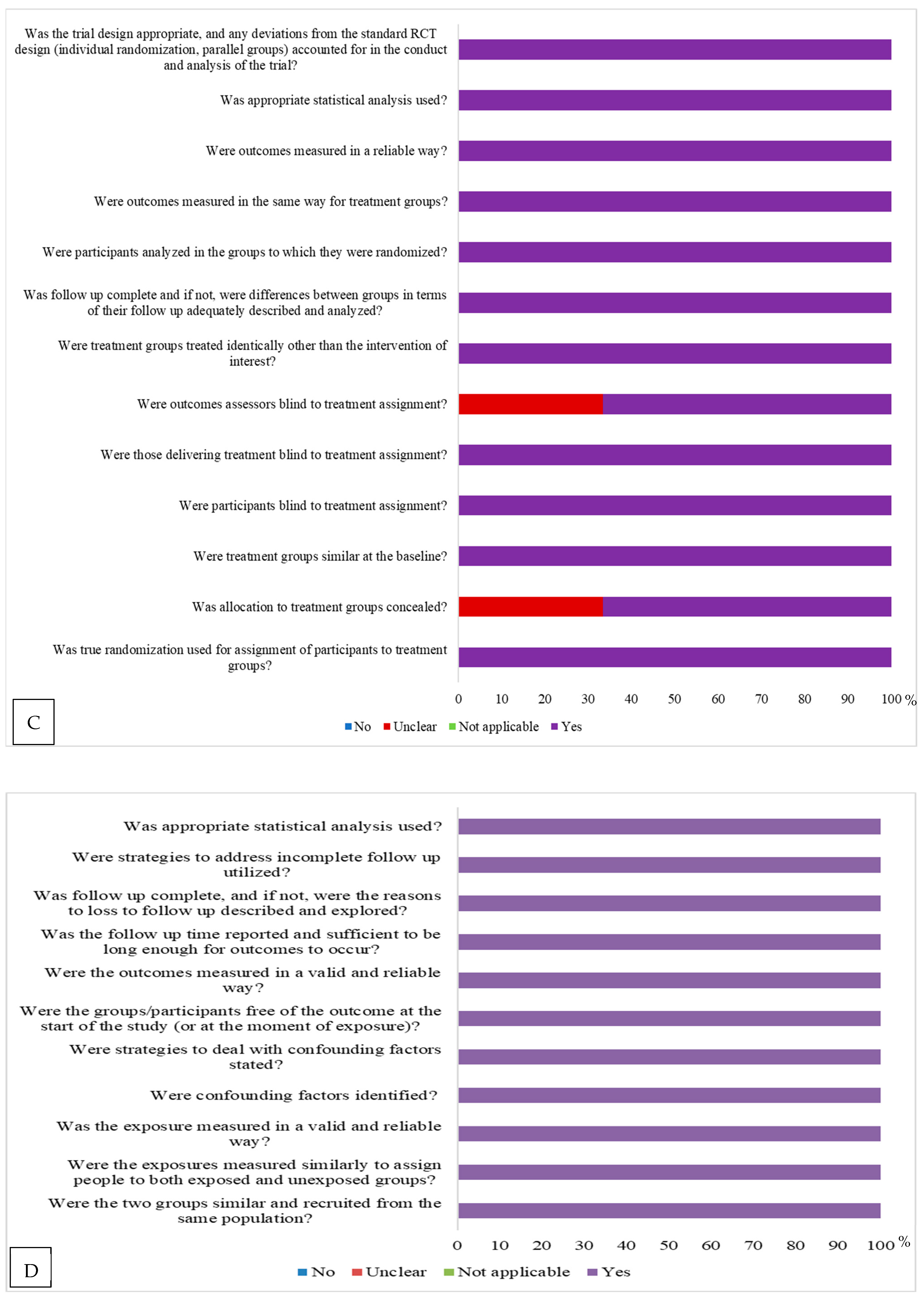
2.6. Evaluation of the Methodological Quality of the Selected Articles
2.7. Data Synthesis and Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Bailey, R.L.; West, K.P., Jr.; Black, R.E. The Epidemiology of Global Micronutrient Deficiencies. Ann. Nutr. Metab. 2015, 66, 22–33. [Google Scholar] [CrossRef]
- Soares, M.S. Nutritional Assessment of Selenium in Adults from the City of Manaus, Amazonas. Ph.D. Thesis, University of São Paulo, São Paulo, Brazil, 2018. [Google Scholar] [CrossRef]
- Krela-Kaźmierczak, I.; Czarnywojtek, A.; Skoracka, K.; Rychter, A.M.; Ratajczak, A.E.; Szymczak-Tomczak, A.; Ruchała, M.; Dobrowolska, A. Is there an ideal diet to protect against iodine deficiency? Nutrients 2021, 13, 513. [Google Scholar] [CrossRef]
- Francis, A.K.; Tayie, K.J. Hypertension, Dietary Salt Restriction, and Iodine Deficiency Among Adults. Am. J. Hypertens. 2010, 23, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Biban, B.G.; Lichiardopol, C. Iodine Deficiency, Still a Global Problem? Curr. Health Sci. J. 2017, 43, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Köhrle, J.; Gärtner, R. Selenium and thyroid. Best Pract. Res. Clin. Endocrinol. Metab. 2009, 23, 815–827. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Aki, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Lopes, S.O. Iodine Nutritional Status and Associated Socioeconomic, Demographic, Health and Nutritional Factors in Family Farmers in the Immediate Geographic Region of Viçosa-MG. Ph.D. Thesis, University of Viçosa, Viçosa, Brazil, 2023. [Google Scholar]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS peer review of electronic search strategies: 2015 guideline statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. Critical Appraisal tools for use in JBI Systematic Reviews. 2020. Available online: https://jbi.global/critical-appraisal-tools (accessed on 2 April 2025).
- Costa, A.B.; Zoltowski, A.P.C.; Koller, S.H.; Teixeira, M.A.P. Construção de uma escala para avaliar a qualidade metodológica de revisões sistemáticas. Ciênc. Saúde Coletiva 2015, 20, 2441–2452. [Google Scholar] [CrossRef]
- BalduzzI, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Wolde-Gebriel, Z.; West, C.E.; Gebru, H.; Tadesse, A.S.; Fisseha, T.; Gabre, P.; Aboye, C.; Ayana, G.; Hautvast, J.G.A.J. Interrelationship between vitamin A, iodine and iron status in schoolchildren in Shoa Region, central Ethiopia. Br. J. Nutr. 1993, 70, 593–607. [Google Scholar] [CrossRef]
- Kvícala, J.; Zamrazil, V.; Soutorová, M.; Tomíska, F. Correlations between parameters of body selenium status and peripheral thyroid parameters in the low selenium region. Analyst 1995, 120, 959–965. [Google Scholar] [CrossRef]
- Hampel, R.; Kühlberg, T.; Schneider, K.P.; Glass, A.; Zöllner, H. Serum zinc levels and goitre epidemiology in Germany. Z. Ernahrungswissenschaft 1997, 36, 12–15. [Google Scholar] [CrossRef]
- Ozata, M.; Salk, M.; Aydin, A.; Sayin, S.; Oktenli, C.; Beyham, Z.; Isimer, A.; Ozdemir, I.C. Iodine and zinc, but not selenium and copper, deficiency exists in a male Turkish population with endemic goiter. Biol. Trace Elem. Res. 1999, 69, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Zagrodzki, P.; Szmigiel, H.; Ratajczak, R.; Szybinski, Z.; Zachwieja, Z. The role of selenium in iodine metabolism in children with goiter. Environ. Health Perspect. 2000, 108, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Erdoğan, M.F.; Erdoğan, G.; Sav, H.; Güllü, S.; Kamel, N. Endemic goiter, thiocyanate overload, and selenium status in school-age children. Biol. Trace Elem. Res. 2001, 79, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Aydin, K.; Kendirci, M.; Kurtoğlu, S.; Karaküçük, E.I.; Kiriş, A. Iodine and selenium deficiency in school-children in an endemic goiter area in Turkey. J. Pediatr. Endocrinol. Metab. 2002, 15, 1027–1031. [Google Scholar] [CrossRef]
- Azizi, F.; Mirmiran, P.; Sheikholeslam, R.; Hedayati, M.; Rastmanesh, R. The relation between serum ferritin and goiter, urinary iodine and thyroid hormone concentration. Int. J. Vitam. Nutr. Res. 2002, 72, 296–299. [Google Scholar] [CrossRef]
- Eftekhari, M.H.; Keshavarz, S.A.; Jalali, M.; Elguero, E.; Eshraghian, M.R.; Simondon, K.B. The relationship between iron status and thyroid hormone concentration in iron-deficient adolescent Iranian girls. Asia Pac. J. Clin. Nutr. 2006, 15, 50. [Google Scholar]
- Thurlow, R.A.; Winichagoon, P.; Pongcharoen, T.; Gowachirapant, S.; Boonpraderm, A.; Manger, M.S.; Bailey, K.B.; Wasantwisut, E.; Gibson, R.S. Risk of zinc, iodine and other micronutrient deficiencies among school children in North East Thailand. Eur. J. Clin. Nutr. 2006, 60, 623–632. [Google Scholar] [CrossRef]
- Dabbaghmanesh, M.H.; Sadegholvaad, A.; Zarei, F.; Omrani, G. Zinc Status and Relation to Thyroid Hormone Profile in Iranian Schoolchildren. J. Trop. Pediatr. 2008, 54, 58–61. [Google Scholar] [CrossRef]
- Zagrodzki, P.; Ratajczak, R. Selenium status, sex hormones, and thyroid function in young women. J. Trace Elem. Med. Biol. 2008, 22, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Doupis, J.; Stavrianos, C.; Saltiki, K.; Mantzou, E.; Mastrokostopoulos, A.; Philippou, G.; Alevizaki, M. Thyroid volume, selenium levels and nutritional habits in a rural region in Albania. Hormones 2009, 8, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Keshteli, A.H.; Hashemipour, M.; Siavash, M.; Kelishadi, R.; Amini, M. High prevalence of goiter in schoolchildren in Isfahan; zinc deficiency does not play a role. Endokrynol. Pol. 2010, 61, 287–290. [Google Scholar] [PubMed]
- Moaddab, M.H.; Keshteli, A.H.; Dastjerdi, M.S.; Rezvanian, H.; Aminorroaya, A.; Amini, M.; Kachuei, A.; Hashemipour, M. Zinc status in goitrous school children of Semirom, Iran. J. Res. Med. Sci. 2009, 14, 165–170. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC3129056/ (accessed on 3 April 2025).
- Hashemipour, M.; Soheilipour, F.; Keshteli, A.H.; Siavash, M.; Amini, M.; Kelishadi, R. Association between serum ferritin and goitre in Iranian school children. J. Health Popul. Nutr. 2010, 28, 137–142. [Google Scholar] [CrossRef]
- Keshteli, A.H.; Hashemipour, M.; Siavash, M.; Amini, M. Selenium deficiency as a possible contributor of goiter in schoolchildren of Isfahan, Iran. Biol. Trace Elem. Res. 2009, 129, 70–77. [Google Scholar] [CrossRef]
- Henjum, S.; Barikm, I.; Strand, T.A.; Oshaug, A.; Torheim, L.E. Iodine-induced goitre and high prevalence of anaemia among Saharawi refugee women. Public Health Nutr. 2012, 15, 1512–1518. [Google Scholar] [CrossRef]
- Sanjari, M.; Gholamhoseinian, A.; Nakhaee, A. Serum zinc levels and goiter in Iranian school children. J. Trace Elem. Med. Biol. 2012, 26, 42–45. [Google Scholar] [CrossRef]
- Liu, Y.; Huang, H.; Zeng, J.; Sun, C. Thyroid volume, goiter prevalence, and selenium levels in an iodine-sufficient area: A cross-sectional study. BMC Public Health 2013, 13, 1153. [Google Scholar] [CrossRef]
- Yavuz, Ö.; Yavuz, T.; Kahraman, C.; Yeşildal, N.; Bundak, R. The relationship between iron status and thyroid hormones in adolescents living in an iodine deficient area. J. Pediatr. Endocrinol. Metab. 2004, 17, 1443–1450. [Google Scholar] [CrossRef]
- Khatiwada, S.; Gelal, B.; Baral, N.; Lamsal, M. Association between iron status and thyroid function in Nepalese children. Thyroid. Res. 2016, 9, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Hendryx, M.; Dinh, P.; He, K. Association of iodine and iron with thyroid function. Biol. Trace Elem. Res. 2017, 179, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Suhail, N.; Alsel, B.T.A.; Batool, S. Prevalence and association of thyroid dysfunction with anemia/body iron status among northern Border Saudi population. Int. J. Med. Res. Health Sci. 2020, 9, 1–7. Available online: https://www.ijmrhs.com/medical-research/prevalence-and-association-of-thyroid-dysfunction-with-anemiabody-iron-status-among-northern-border-saudi-population.pdf (accessed on 3 April 2025).
- Campos, R.O.; de Jesus, L.M.; Morais, D.A.; Júnior, W.T.d.S.; Souza, V.C.d.O.; Oliveira, C.A.; Júnior, F.B.; Macedo, M.; Hegedüs, L.; Ramos, H.E. Low urinary selenium levels are associated with iodine deficiency in Brazilian schoolchildren and adolescents. Endocrine 2021, 73, 609–616. [Google Scholar] [CrossRef]
- Islam, R.; Akter, K.M.; Rahman, A.; Khanam, N.N.; Al Azad, S.; Islam, M.R.; Farjana, M.; Rahman, M.H.; Badal, M.N.U.; Ahmed, S. The Serological Basis of the Correlation between Iron Deficiency Anemia and Thyroid Disorders in Women: A Community Based Study. J. Pharm. Res. Int. 2021, 33, 69–81. [Google Scholar] [CrossRef]
- Turan, E.; Turksoy, V.A. Selenium, zinc, and copper status in euthyroid nodular goiter: A cross-sectional study. Int. J. Prev. Med. 2021, 12, 46. [Google Scholar] [CrossRef]
- Berger, J.; Finlayson, J.; von Hurst, P.R.; Brough, L. Iodine and selenium intakes and status and thyroid function in midlife women with low bread intakes in New Zealand. Nutr. Diet. 2025; ahead of print. [Google Scholar] [CrossRef]
- Ravaglia, G.; Forti, P.; Maioli, F.; Nesi, B.; Pratelli, L.; Savarino, L.; Cucinotta, D.; Cavalli, G. Blood micronutrient and thyroid hormone concentrations in the oldest-old. J. Clin. Endocrinol. Metab. 2000, 85, 2260–2265. [Google Scholar] [CrossRef]
- Cinaz, P.; Karakas, D.S.; Camurdan, M.O.; Bideci, A.; Ayvali, E.D.; Yücel, C. Goiter prevalence, serum selenium, and urine iodine status in a previously iodine-deficient area in Turkey. Biol. Trace Elem. Res. 2004, 100, 185–194. [Google Scholar] [CrossRef]
- Hekimsoy, Z.; Biberoglu, S.; Kirkali, G.; Bicer, N.; Erbayraktar, Z. Plasma selenium and urinary iodine in patients with goiter. Trace Elem. Electrolytes 2004, 21, 145–149. [Google Scholar] [CrossRef]
- Kandhro, G.A.; Kazi, T.G.; Afridi, H.I.; Kazi, N.; Arain, M.B.; Sarfraz, R.A.; Sirajuddin; Syed, N.; Baig, J.A.; Shah, A.Q. Evaluation of iron in serum and urine and their relation with thyroid function in female goitrous patients. Biol. Trace Elem. Res. 2008, 125, 203–212. [Google Scholar] [CrossRef]
- Kishosha, P.A.; Galukande, M.; Gakwaya, A.M. Selenium deficiency a factor in endemic goiter persistence in sub-Saharan Africa. World J. Surg. 2011, 35, 1540–1545. [Google Scholar] [CrossRef] [PubMed]
- Çelik, T.; Savaş, N.; Kurtoğlu, S.; Sangün, Ö.; Aydın, Z.; Mustafa, D.; Öztürk, O.H.; Mısırlıoğlu, S.; Öktem, M. Iodine, copper, zinc, selenium and molybdenum levels in children aged between 6 and 12 years in the rural area with iodine deficiency and in the city center without iodine deficiency in Hatay. Turk. Arch. Pediatr. 2014, 49, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Olivieri, O.; Girelli, D.; Azzini, M.; Stanzial, A.M.; Russo, C.; Ferroni, M.; Corrocher, R. Low selenium status in the elderly influences thyroid hormones. Clin. Sci. 1995, 89, 637–642. [Google Scholar] [CrossRef] [PubMed]
- Olivieri, O.; Girelli, D.; Stanzial, A.M.; Rossi, L.; Bassi, A.; Corrocher, R. Selenium, zinc, and thyroid hormones in healthy subjects. Biol. Trace Elem. Res. 1996, 51, 31–41. [Google Scholar] [CrossRef]
- Gashu, D.; Marquis, G.S.; Bougma, K.; Stoecker, B.J. Selenium inadequacy hampers thyroid response of young children after iodine repletion. J. Trace Elem. Med. Biol. 2018, 50, 291–295. [Google Scholar] [CrossRef]
- Rasmussen, L.B.; Schomburg, L.; Köhrle, J.; Pedersen, I.B.; Hollenbach, B.; Hög, A.; Ovesen, L.; Perrild, H.; Laurberg, P. Selenium status, thyroid volume, and multiple nodule formation in an area with mild iodine deficiency. Eur. J. Endocrinol. 2011, 164, 585–590. [Google Scholar] [CrossRef]
- El-Masry, H.; Hamed, A.M.M.; Hassan, M.H.; Abdelzaher, M.H. Thyroid Function among Children with Iron Deficiency Anaemia: Pre and Post Iron Replacement Therapy. J. Clin. Diagn. Res. 2018, 12, BC1–BC5. [Google Scholar] [CrossRef]
- Gu, Y.; Chi, V.T.Q.; Zhang, Q.; Liu, L.; Meng, G.; Wu, H.; Bao, X.; Zhang, S.; Sun, S.; Wang, X.; et al. Low-Normal thyroid function predicts incident Anemia in the general population with Euthyroid status. J. Clin. Endocrinol. Metab. 2019, 104, 5693–5702. [Google Scholar] [CrossRef]
- Candido, A.C.; Azevedo, F.M.; Ribeiro, S.A.V.; Navarro, A.M.; Macedo, M.d.S.; Fontes, E.A.F.; Crispim, S.P.; de Carvalho, C.A.; Pizato, N.; da Silva, D.G.; et al. Iodine Deficiency and Excess in Brazilian Pregnant Women: A Multicenter Cross-Sectional Study (EMDI-Brazil). Nutrients 2025, 17, 2753. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 2015, 3, 286–295. [Google Scholar] [CrossRef] [PubMed]
- Sorrenti, S.; Baldini, E.; Pironi, D.; Lauro, A.; D’orazi, V.; Tartaglia, F.; Tripodi, D.; Lori, E.; Gagliardi, F.; Praticò, M.; et al. Iodine: Its role in thyroid hormone biosynthesis and beyond. Nutrients 2021, 13, 4469. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization—WHO. Assessment of the Iodine Deficiency Disorders and Monitoring Their Elimination; WHO: Geneva, Switzerland, 2007; Available online: https://iris.who.int/bitstream/handle/10665/43781/9789241595827_eng.pdf?sequence=1 (accessed on 16 September 2025).
- Leung, A.M.; Braverman, L.E. Consequences of excess iodine. Nat. Rev. Endocrinol. 2014, 10, 136–142. [Google Scholar] [CrossRef]
- Rigutto-Farebrother, J.; Zimmermann, M.B. Salt reduction and iodine fortification policies are compatible: Perspectives for public health advocacy. Nutrients 2024, 16, 2517. [Google Scholar] [CrossRef]
- Candido, A.C.; Azevedo, F.M.; Macedo, M.S.; Priore, S.E.; Franceschini, S.C.C. Critical analysis of indicators of iodine nutritional status in individuals and populations: A systematic review. Sci. Public Health 2021, 26, 4859–4870. [Google Scholar] [CrossRef]
- Jayasuriya, M.S.; Choy, K.W.; Chin, L.K.; Doery, J.; Stewart, A.; Bergman, P.; Lu, Z.X. Reference intervals for neonatal thyroid function tests in the first 7 days of life. J. Pediatr. Endocrinol. Metab. 2018, 31, 1113–1116. [Google Scholar] [CrossRef]
- Segni, M. Disorders of the Thyroid Gland in Infancy, Childhood and Adolescence in Comprehensive Free Online Endrocrinology Book. 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK279032/ (accessed on 14 September 2025).
- Garofalo, V.; Condorelli, R.A.; Cannarella, R.; Aversa, A.; Calogero, A.E.; La Vignera, S. Relationship between iron deficiency and thyroid function: A systematic review and meta-analysis. Nutrients 2023, 15, 4790. [Google Scholar] [CrossRef]
- Lopes, S.O.; Abrantes, L.C.S.; Azevedo, F.M.; Morais, N.S.; Morais, D.C.; Gonçalves, V.S.S.; Fontes, E.A.F.; Franceschini, S.C.C.; Priore, S.E. Food insecurity and micronutrient deficiency in adults: A systematic review and meta-analysis. Nutrients 2023, 15, 1074. [Google Scholar] [CrossRef]
- Hess, S.Y. The impact of common micronutrient deficiencies on iodine and thyroid metabolism: The evidence from human studies. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 117–132. [Google Scholar] [CrossRef]
- Hotz, C.S.; Fitzpatrick, D.W.; Trick, K.D.; L’Abbe, M.R. Dietary iodine and selenium interact to affect thyroidhormone metabolism of rats. J. Nutr. 1997, 127, 1214–1218. [Google Scholar] [CrossRef]
- Beckett, G.J.; Nicol, F.; Proudfoot, D.; Dyson, K.; Loucaides, G.; Arthur, J.R. The changes in hepatic enzyme expression caused by selenium deficiency and hypothyroidism in rats are produced by independent mechanisms. Biochem. J. 1990, 266, 743–747. [Google Scholar] [CrossRef] [PubMed]
- Meinhold, H.; Campos-Barros, A.; Walzog, B.; Köhler, R.; Müller, F.; Behne, D. Effects of selenium and iodine deficiency on type I, type II and type III iodothyronine deiodinases and circulating thyroid hormones in the rat. Exp. Clin. Endocrinol. Diabetes 1993, 101, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Arthur, J.R.; Nicol, F.; Beckett, G.J. The role of selenium in thyroid hormone metabolism and effects of selenium deficiency on thyroid hormone and iodine metabolism. Biol. Trace Elem. Res. 1992, 33, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Beckett, G.J.; Nicol, F.; Rae, P.W.; Beech, S.; Guo, Y.; Arthur, J.R. Effects of combined iodine and selenium deficiency on thyroid hormone metabolism in rats. Am. J. Clin. Nutr. 1993, 57, 240S–243S. [Google Scholar] [CrossRef]
- Ruz, M.; Codoceo, J.; Galgani, J.; Muñoz, L.; Gras, N.; Muzzo, S.; Leiva, L.; Bosco, C. Single and multiple selenium-zinc-iodine deficiencies affect rat thyroid metabolism and ultrastructure. J. Nutr. 1999, 129, 174–180. [Google Scholar] [CrossRef]



| Author/Year | Place | Design | Sample (N; Sex; Age/Age Group) | Main Objective |
|---|---|---|---|---|
| Wolde-Gebriel et al., 1993 [14] | Shoa/Ethiopia | Cross-sectional | 14,740; both sexes; 6–18 years | Examine the interrelations between three nutritional conditions (vitamin A, iodine, and iron deficiencies). |
| Kvíčala et al., 1995 [15] | Prague/Czech Republic | Cross-sectional | 380; both sexes; 6–65 years | Evaluate the influence of selenium on the thyroid, hormonal parameters, and peripheral effects in selenium-deficient regions. |
| Hampel et al., 1997 [16] | Germany | Cross-sectional | 5932; both sexes (3.692 women: 41 ± 17 years; 2.240 men: 39 ± 18 years) | Record goiter prevalence and iodine supply in Germany. |
| Ozata et al., 1999 [17] | Turkey | Cross-sectional | 280; men; with goiter: n = 140 de 22.2 ± 0.19 aged; without goiter: n = 140 de 21.8 ± 0.28 aged | Determine the levels of iodine, zinc, selenium, and copper in patients with endemic goiter in order to investigate their role in the etiopathogenesis of endemic goiter in Turkey. |
| Zagrodzki et al., 2000 [18] | Poland | Cross-sectional | 136; both sexes; 7–16 years | Investigate the role of selenium in iodine metabolism among children with goiter. |
| Erdoğan et al., 2001 [19] | Ancara, Kastamonu, Bayburt e Trabzon/Turkey | Cross-sectional | 251 schoolchildren; both sexes; 9–11 years | Evaluate selenium level and thiocyanate (SCN-) overload and the possible contribution of this overload to endemic goiter and the thyroid hormone profile. |
| Aydin et al., 2002 [20] | Kayseri/Turkey | Cross-sectional | 73 schoolchildren; both sexes; 7–12 years | Establish the effects of iodine and selenium levels on the size and functions of the thyroid gland in healthy schoolchildren. |
| Azizi et al., 2002 [21] | Iran | Cross-sectional | 36,178 schoolchildren; both sexes; 8–10 years | Determine the relationship between serum ferritin and goiter, urinary iodine and thyroid hormones after iodine supplementation through iodized salt. |
| Eftekhari et al., 2006 [22] | Home/Iran | Cross-sectional | 103 adolescents; women; 14–18 years | Determine thyroid hormone status in adolescent girls with iron deficiency. |
| Thurlow et al., 2006 [23] | Ubon Ratchathani/Thailand | Cross-sectional | 567 children; both sexes; 6–13 years | Evaluate the prevalence of zinc and iodine deficiencies and their interrelations with vitamin A deficiency and anemia as well as associations with socioeconomic status, hemoglobin type, and anthropometry through a cross-sectional study. |
| Dabbaghmanesh et al., 2007 [24] | Marvdasht/Iran | Cross-sectional | 1188; both sexes; 8–13 years | Determine the prevalence of zinc deficiency and current zinc status in schoolchildren with goiter. |
| Zagrodzki; Ratajczak, 2008 [25] | Poland | Cross-sectional | 58; women; 23.57 ± 0.6 years | Identify parameters that characterize selenium status and secretion of sex hormones responsible for changes in indicators of thyroid function. In addition, reveal the correlation structure of parameters that express selenium status, sex hormone secretion, and thyroid function. |
| Doupis et al., 2009 [26] | Gyrocaster/Albania | Cross-sectional | 112; both sexes; 52.8 ± 12.1 years | Study the thyroid status of people living in the Gyrocaster region of Southwestern Albania. |
| Keshteli et al., 2009 [27] | Isfahan/Iran | Cross-sectional | 2330 schoolchildren; both sexes; 6–13 years | Estimate the prevalence of goiter and iodine status and investigate the role of selenium status as a possible contributor to endemic goiter among schoolchildren in Isfahan, 15 years after the start of a salt iodization program. |
| Moaddab et al., 2009 [28] | Semirom/Iran | Cross-sectional | 1828; both sexes; schoolchildren | Associate goiter with serum zinc in a mountainous region of Iran. |
| Hashemipour et al., 2010 [29] | Isfahan/Iran | Cross-sectional | 2331 schoolchildren; both sexes; 6–13 years | Estimate the prevalence of goiter and iodine status and investigate the role of iron deficiency as a possible contributor to endemic goiter in schoolchildren of Isfahan, 15 years after the start of a salt iodization program. |
| Keshteli et al., 2010 [30] | Isfahan/Iran | Cross-sectional | 2331 schoolchildren; both sexes; 6–13 years | Determine the association between zinc status and goiter in schoolchildren of Isfahan. |
| Henjum et al., 2011 [31] | Algeria | Cross-sectional | 394; women; 15–45 years | Assess iodine status (thyroid volume and urinary iodine concentration) and its determinants in Saharawi refugee women. |
| Sanjari; Gholamhoseiniana; Nakhaee, 2012 [32] | Kerman/Iran | Cross-sectional | 5380 schoolchildren; both sexes; 8–12 years | Determine the difference in serum zinc levels between children with and without goiter aimed at finding evidence on the probable role of zinc deficiency in endemic goiter. |
| Liu et al., 2013 [33] | Chengdu/China | Cross-sectional | 1205; both sexes; 18 years or older | Investigate the relationship between selenium level, thyroid volume, and goiter in an area with sufficient iodine. |
| Yavuz et al., 2014 [34] | Turkey | Cross-sectional | 330; both sexes; ±14 years | Evaluate the effect of iron level on thyroid hormone profile in adolescents living in a mild iodine-deficient area in Turkey |
| Khatiwada et al., 2016 [35] | Sankhuwasabha e Dhankuta/Nepal | Cross-sectional | 227 schoolchildren; both sexes; 6–12 years | Investigate the association between iron level and thyroid function among Nepalese children living in mountainous regions. |
| Luo et al., 2017 [36] | United States of America | Cross-sectional | 7672; both sexes; 20 years or older | Investigate the combined association of serum iron and urinary iodine concentrations with serum thyroid hormone measurements using a national representative sample from the National Health and Nutrition Examination Survey (NHANES). |
| Suhail; Alsel.; Batool, 2020 [37] | Saudi Arabia | Cross-sectional | 150; both sexes; 24–76 years | Estimate the prevalence and association of thyroid dysfunction with anemia/body iron status in the Saudi population of the northern border. |
| Campos et al., 2021 [38] | Bahia/Brazil | Cross-sectional | 982 schoolchildren; both sexes; 6–14 years | Evaluate the nutritional status of selenium and iodine in schoolchildren. |
| Islam et al., 2021 [39] | Bangladesh | Cross-sectional | 405; women; 0–81 years | Inspect the correlation between iron deficiency anemia and thyroid disorders in Bangladeshi women. |
| Turan; Turksoy, 2021 [40] | Yozgat/Turkey | Cross-sectional | 181 (98 with goiter and 83 without goiter); both sexes; 18–65 years | Compare serum levels of trace elements, such as selenium, zinc, and copper in patients with euthyroid nodular goiter and healthy participants. |
| Berger et al., 2025 [41] | New Zealand | Cross-sectional | 37; women; 40–63 years | Investigate the effect of low bread intake on iodine and selenium intake and status, and thyroid function in mid-life women in New Zealand. |
| Ravaglia et al., 2000 [42] | Bolonha, Emilia Romagna/Italy | Control case | 132; both sexes; control: aged 20–64 years; elderly group: n = 44 aged 65–89 years; oldest-old group: n = 44 aged 90–107 years (24 were 100 years old or older) | Evaluate the relationships between thyroid function and blood levels of selenium, zinc, retinol, and alpha-tocopherol in a selected group of healthy free-living Italian subjects. |
| Cinaz et al., 2004 [43] | Turkey | Control case | 905; both sexes; 6–12 years | Investigating the prevalence of goiter, serum selenium, and urine iodine status among school children in the Ankara region of Turkey. |
| Hekimsoy et al., 2004 [44] | Turkey | Control case | 102; both sexes; with goiter n = 72 aged 43 ± 11 years; without goiter: n = 30 aged 40.6 ± 13.6 years | Measure iodine excretion rates in patients with diffuse or nodular goiter and examine plasma selenium concentrations in order to verify whether selenium deficiency may be related to the genesis of goiter in the studied region. |
| Kandhro et al., 2008 [45] | Sindh/Pakistan | Control case | 186; women; with goiter: n = 69 without goiter: n = 117; 21–45 years | Evaluate iron concentration in biological samples (serum and urine) and other biochemical parameters such as TSH, free triiodothyronine, and free Thyroxine in goiter patients and compare them with healthy women of the same age residing in the same area. |
| Kishosha; Galukand; Gakwaya 2011 [46] | Uganda | Control case | 92; both sexes; 18–35 years | Determine serum selenium levels in goiter patients and non-goiter controls and determine the association between goiter and selenium levels in these patients. |
| Çelik et al., 2014 [47] | Hatay/Turkey | Control case | 214 schoolchildren; both sexes; 6–12 years | Investigate urine iodine, selenium, zinc, copper, or molybdenum deficiencies in children aged 6 to 12 years in two schools in the Hatay province. |
| Olivieri et al., 1995 [48] | Vicenza/Italy | Randomized clinical trial | 109; both sexes; Group I: n = 36 adults aged 20–44 years Group II: n = 36 individuals aged 20–44 years; Group III: n = 37 elderly aged 65 years and older | Investigate the relationships between age, selenium status, and thyroid hormones in three groups of healthy free-living individuals of different ages, paired by sex distribution. |
| Olivieri et al., 1996 [49] | Vicenza/Italy | Randomized clinical trial | 109; both sexes; Group I: n = 36 adults aged 20–44 years Group II: n = 36 individuals aged 20–44 years; Group III: n = 37 elderly aged 65 years and older | Investigate the relationships between age, selenium levels, and thyroid hormones in three groups of healthy free-living individuals of different ages, paired by sex distribution. Further, measure serum and erythrocyte zinc to assess possible interactions with circulating levels of thyroid hormones. |
| Gashu et al., 2009 [50] | Amhara/Ethiopia | Randomized clinical trial | 624; both sexes; 6–60 months | Investigate the influence of selenium inadequacy on thyroid response in children. |
| El-masry et al., 2018 [51] | Assiut e Qena/Egypt | Clinical trial | 805; both sexes; women aged 18–22, 40–45 and 60–65 years; men aged 60–65 years | Study the associations between serum selenium concentration, thyroid volume, and the risk of thyroid gland enlargement in an area with mild iodine deficiency before and after the introduction of iodine fortification. |
| Rasmussen et al., 2011 [52] | Denmark | Cohort | 120; (60 anemic and 60 non-anemic); both sexes; 2–16 years | Investigate the possible occurrence of thyroid dysfunction among children with isolated iron deficiency anemia of various severities and test whether oral iron replacement therapy alone can reverse the associated thyroid function disorders, and if additional or present therapies are needed. |
| Gu et al., 2019 [53] | Tianjin/China | Cohort | 12,310; both sexes; 45.5 (±11.4) years | Examine whether thyroid hormones under physiological conditions can affect the development of anemia in the general population |
| Author/Year | Method Evaluation | Association Between Nutritional Status of Iodine and Micronutrients | |
|---|---|---|---|
| Nutritional Status of Iodine | Micronutrient (Method Used) | ||
| Wolde-Gebriel et al., 1993 [14] | UIC; TSH; T3; T4; Thyroxine-Binding Globulin; thyroid palpation | Hemoglobin; ferritin; serum iron; total iron binding capacity; transferrin; hematocrit; mean corpuscular volume | Negative correlation between T3, T4, and Thyroxine Binding Globulin with hemoglobin. |
| Kvíčala et al., 1995 [15] | UIC; TSH; T3; T4; thyroid ultrasound | Serum selenium; urinary selenium; urinary selenium/creatinine; and creatinine concentration (hair) | Positive correlation between T3 and serum selenium and selenium/creatinine; positive correlation between thyroid volume, serum selenium, and urinary selenium; positive correlation between T4/T3 and serum selenium; negative correlation between thyroid volume and selenium/creatinine; negative correlation between T4, serum selenium and urinary selenium. |
| Olivieri et al., 1995 [48] | TSH; T3; T4 | Serum selenium and erythrocyte Glutathione Peroxidase | Negative correlation between T4, positive T3/T4, and selenium (all population). In older individuals, negative with T4 and positive T3/T4. |
| Olivieri et al., 1996 [49] | TSH; T3; T4 | Serum selenium; Glutathione Peroxidase; serum zinc; and red blood cells | Positive correlation in the older individual’s group between T3/T4, selenium status, and Glutathione Peroxidase. |
| Hampel et al., 1997 [16] | UIC; thyroid palpation | Serum zinc | NA |
| Ozata et al., 1999 [17] | UIC; TSH; T3; T4 | Serum zinc; selenium; and copper | UIC and zinc were lower in the group with goiter than in the group without goiter. |
| Ravaglia et al., 2000 [41] | TSH; T3; T4 | Selenium and serum zinc | Positive correlation between T3 and T3/T4 with zinc in individuals under 90 years of age. |
| Zagrodzki et al., 2000 [18] | UIC; TSH; T4 | Serum selenium and Glutathione Peroxidase | Lower selenium concentrations and Glutathione Peroxidase activity in the group with goiter compared to the group without goiter. |
| Erdoğan et al., 2001 [19] | UIC; TSH; T3; T4; thyroid ultrasound; thyroglobulin | Serum selenium | NA |
| Aydin et al., 2002 [20] | Thyroid ultrasound | Serum selenium | Positive correlation between thyroid volume and selenium; selenium and iodine levels in children with goiter were lower. |
| Azizi et al., 2002 [21] | UIC; TSH; T3; T4; thyroid palpation | Ferritin | Lower goiter rates in children with higher ferritin concentrations. |
| Cinaz et al., 2004 [42] | UIC; TSH; T3; T4; Anti-TPO; thyroid ultrasound | Serum selenium | Selenium level was lower in goiter group. |
| Hekimsoy et al., 2004 [43] | UIC; TSH; T3 and T4; total and free; thyroid ultrasound | Serum selenium | NA |
| Eftekhari et al., 2006 [22] | UIC; TSH; T3; T4; T3 and T4 free; uptake of triiodothyronine resin; reverse triiodothyronine concentrations | Hemoglobin; ferritin; total iron binding capacity; serum selenium | Positive correlation between T4, negative TSH, negative T3/T4 with ferritin; ferritin contributed to T3 concentration. |
| Thurlow et al., 2006 [23] | UIC | Serum zinc; hemoglobin; and ferritin | NA |
| Dabbaghmanesh et al., 2008 [24] | TSH; T3 and T4 free; thyroid palpation | Serum zinc | NA |
| Kandhro et al., 2008 [44] | TSH; T3; T4 | Hemoglobin; serum and urinary iron; transferrin receptor; mean corpuscular volume; mean corpuscular hemoglobin concentration; zinc protoporphyrin | Serum and urinary iron concentrations were reduced in the group with goiter and increased TSH. |
| Zagrodzki; Ratajczak, 2008 [25] | TSH; T3; T4 Plasma Glutathione Peroxidase; anti-TPO; thyroid ultrasound | Serum selenium | NA |
| Doupis et al., 2009 [26] | UIC; TSH; T3; T4 liver; anti-TPO; anti-TG; thyroid ultrasound | Serum selenium | NA |
| Gashu et al., 2009 [49] | UIC; TSH; T3; T4; thyroglobulin | Serum selenium | Positive correlation between T3 and T4, and negative correlation between TSH, thyroglobulin, and selenium. Despite adequate iodine status, children with low selenium levels had lower T3 and T4 and higher TSH concentrations. |
| Keshteli et al., 2009 [30] | UIC; TSH; T4; anti-TPO; anti-TG | Serum selenium | Mean serum selenium in children with and without goiter were different. The prevalence of selenium deficiency was higher in boys and girls with goiter than without goiter. |
| Moaddab et al., 2009 [28] | UIC; T4; Thyroid palpation | Serum zinc | NA |
| Hashemipour et al., 2010 [29] | UIC; TSH; T4; anti-thyroglobulin; anti-thyroperoxidase | Ferritin | Positive correlation between UIC and ferritin. |
| Keshteli et al., 2010 [27] | UIC; TSH; T4 | Serum zinc | Mean serum zinc levels in children with and without goiter were different. |
| Kishosha; Galukand; Gakwaya 2011 [45] | Thyroid palpation | Serum selenium | Selenium levels between the populations with and without goiter were different; selenium levels above 102.8 μg/L presented a protective effect against goiter. |
| Rasmussen et al., 2011 [50] | UIC; thyroid ultrasound | Serum selenium | Serum selenium concentration was associated with the enlargement of the thyroid gland. |
| Henjum et al., 2012 [31] | UIC; thyroid ultrasound | Hemoglobin | NA |
| Sanjari; Gholamhoseiniana; Nakhaee, 2012 [32] | Thyroid palpation | Serum zinc | NA |
| Liu et al., 2013 [33] | UIC; TSH; T3; T4 livers; anti-TPO; anti-TG; thyroid ultrasound | Serum selenium | NA |
| Çelik et al., 2014 [46] | UIC; thyroid palpation | Urinary zinc and selenium | Positive correlation between selenium and zinc with iodine. |
| Yavuz et al., 2014 [34] | TSH; T3 and T4 free | Hemoglobin; ferritin; serum iron; mean corpuscular volume; and total serum iron binding capacity | NA |
| Khatiwada et al., 2016 [35] | UIC; TSH; T3; T4 | Hemoglobin; serum iron; total iron binding capacity; transferrin saturation | Mean TSH level was higher in the anemic; T3 was higher in children with sufficient iron; serum iron level and transferrin saturation were different in iodine-deficient and iodine-sufficient children. Negative correlation between TSH, transferrin saturation, and hemoglobin; the risk of having hypothyroidism in anemic and iron-deficient children was 5.513 and 1.939, respectively, compared to non-anemic and iron-sufficient children. |
| Luo et al., 2017 [36] | UIC; TSH; T3; T4; T3 and T4 free | Serum iron | When serum iron concentrations were normal, a high urinary iodine concentration was associated with reduced free T3 and increased risk of elevated TSH. When serum iron and iodine levels were low, there was an association with reduced free T3 level and increased TSH level. |
| El-masry et al., 2018 [51] | UIC; TSH; T3; T4 | Hemoglobin; ferritin; hematocrit; red blood cell count; mean corpuscular volume; mean corpuscular hemoglobin; red blood cell distribution width; iron concentration; total iron binding capacity; transferrin saturation; and iron binding capacity | Positive correlation between T3 and negative TSH with serum iron; positive between TSH and red cell distribution width; positive T3 and red blood cell count; negative between TSH with hemoglobin, hematocrit, and red blood cell count. |
| Gu et al., 2019 [52] | TSH; T3 and T4 free | Hemoglobin | Increased T3 and T4 concentrations were associated with decreased incidence of anemia. There was an association between T3, T4, and annual changes in hemoglobin. |
| Suhail; Alsel; Batool, 2020 [37] | TSH; T3; T4 | Hemoglobin; Ferritin; Serum iron; transferrin saturation; mean corpuscular volume; mean corpuscular hemoglobin | TSH has a negative correlation with hemoglobin, serum iron, ferritin, transferrin saturation, mean corpuscular volume, and mean corpuscular hemoglobin; T4 has a positive correlation with hemoglobin, serum iron, ferritin, transferrin saturation, mean corpuscular volume, and mean corpuscular hemoglobin. |
| Campos et al., 2021 [38] | UIC; TSH | Urinary selenium | Positive correlation between UIC and selenium. |
| Islam et al., 2021 [39] | TSH; T4 | Hemoglobin; ferritin; serum iron; total iron binding capacity | Positive correlation between hypothyroidism and iron deficiency anemia (IDA); association between congenital hypothyroidism and IDA. |
| Turan; Turksoy, 2021 [40] | Thyroid ultrasound | Serum selenium and zinc | Serum zinc and selenium levels were higher in individuals without goiter compared to those with goiter. |
| Berger et al., 2025 [41] | UIC; TSH; T3 free; T4 free, TG; anti-TPO; anti-TG | Plasma and urinary selenium | Plasma selenium and urinary iodine excretion as predictors of the T3:T4 ratio were significant in explaining 13% of the model. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopes, S.O.; Mayer, E.M.; Azevedo, F.M.; Candido, A.C.; Bittencourt, J.M.; Morais, D.d.C.; Franceschini, S.d.C.C.; Priore, S.E. Nutritional Status of Iodine and Association with Iron, Selenium, and Zinc in Population Studies: A Systematic Review and Meta-Analysis. Nutrients 2025, 17, 3432. https://doi.org/10.3390/nu17213432
Lopes SO, Mayer EM, Azevedo FM, Candido AC, Bittencourt JM, Morais DdC, Franceschini SdCC, Priore SE. Nutritional Status of Iodine and Association with Iron, Selenium, and Zinc in Population Studies: A Systematic Review and Meta-Analysis. Nutrients. 2025; 17(21):3432. https://doi.org/10.3390/nu17213432
Chicago/Turabian StyleLopes, Sílvia Oliveira, Edna Miranda Mayer, Francilene Maria Azevedo, Aline Carrare Candido, Jersica Martins Bittencourt, Dayane de Castro Morais, Sylvia do Carmo Castro Franceschini, and Silvia Eloiza Priore. 2025. "Nutritional Status of Iodine and Association with Iron, Selenium, and Zinc in Population Studies: A Systematic Review and Meta-Analysis" Nutrients 17, no. 21: 3432. https://doi.org/10.3390/nu17213432
APA StyleLopes, S. O., Mayer, E. M., Azevedo, F. M., Candido, A. C., Bittencourt, J. M., Morais, D. d. C., Franceschini, S. d. C. C., & Priore, S. E. (2025). Nutritional Status of Iodine and Association with Iron, Selenium, and Zinc in Population Studies: A Systematic Review and Meta-Analysis. Nutrients, 17(21), 3432. https://doi.org/10.3390/nu17213432





