Association Between Dietary Protein Sources and Nutrient Intake in the Diet of Canadian Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Adjusting for Misreporting
2.3. Definition of Protein Groups
2.4. Nutrient Intakes Analysis
2.5. Protein Quality Assessment
2.6. Statistical Analyses
3. Results
3.1. Nutrient Density by Protein Grouping
3.2. Energy and Nutrient Intakes by Age and Gender
3.2.1. Females 9–13 Years
3.2.2. Males 9–13 Years
3.2.3. Females 14–18 Years
3.2.4. Males 14–18 Years (Table 6)
| Plant Protein/Total % | 0–24.9% (n = 181) | 25–49.9% (n = 270) | 50–74.9% (n = 58) | 75–100% (n = 7) | RDA AI |
|---|---|---|---|---|---|
| Total energy (kcal) | 2479.44 ± 67.04 | 2369.28 ± 68.59 | 2490.8 ± 94.07 | 2384.35 ± 309.98 | |
| Total fat (g) | 92.92 ± 5.17 | 88.79 ± 4.21 | 82.6 ± 5.72 | 55.25 ± 13.44 * | ND |
| Total protein (g) | 136 ± 9.08 *** (262%) | 86.89 ± 3.02 (167%) | 88.87 ± 7.57 (171%) | 56.57 ± 13.53 (109%) | 52 |
| Total carbohydrate (g) | 275.01 ± 10.88 * (212%) | 311.87 ± 8.69 (240%) | 353.82 ± 14.59 * (272%) | 428.3 ± 91.37 (329%) | 130 |
| Total dietary fiber (g) | 15.06 ± 0.84 *** (40%) | 19.27 ± 0.87 (51%) | 25.4 ± 1.71 ** (67%) | 24.37 ± 7.83 (64%) | 38 |
| Total saturated fatty acids (g) | 32.02 ± 2.09 | 30.1 ± 1.31 | 24.81 ± 1.99 | 16.11 ± 1.65 *** | As low as possible |
| Linoleic fatty acids (g) | 15.24 ± 0.93 (95%) | 15.29 ± 1.39 (96%) | 16.87 ± 1.38 (105%) | 12.42 ± 4.98 (78%) | 16 |
| Linolenic fatty acids (g) | 1.79 ± 0.12 (112%) | 1.78 ± 0.18 (111%) | 1.7 ± 0.15 (106%) | 1.95 ± 0.7 (122%) | 1.6 |
| Vitamin D (mcg) | 8.34 ± 0.82 (56%) | 5.94 ± 0.62 (40%) | 5.82 ± 1.37 (39%) | 2.45 ± 1.89 (16%) | 15 |
| Folate (mcg) | 208.89 ± 13.38 (52%) | 211.85 ± 7.43 (53%) | 239.75 ± 36.42 (60%) | 354.6 ± 150.51 (89%) | 400 |
| Vitamin B12 (mcg) | 8.51 ± 1.08 ** (355%) | 4.51 ± 0.31 (188%) | 3.26 ± 0.46 (136%) | 1.45 ± 0.74 * (60%) | 2.4 |
| Thiamin (mg) | 2 ± 0.12 (167%) | 2 ± 0.11 (167%) | 2.83 ± 0.32 (236%) | 2.7 ± 0.66 (225%) | 1.2 |
| Riboflavin (mg) | 2.88 ± 0.33 * (222%) | 2.18 ± 0.11 (168%) | 2.38 ± 0.3 (183%) | 1.99 ± 0.44 (153%) | 1.3 |
| Niacin (mg) | 67.29 ± 6.01 *** (421%) | 41.79 ± 1.43 (261%) | 50.27 ± 6 (314%) | 40.02 ± 10.16 (250%) | 16 |
| Vitamin B6 (mg) | 3.13 ± 0.51 *** (241%) | 1.72 ± 0.09 (132%) | 1.93 ± 0.27 (148%) | 1.52 ± 0.98 (117%) | 1.3 |
| Phosphorus (mg) | 1956.44 ± 107.68 ** (157%) | 1530.62 ± 54.71 (122%) | 1546.66 ± 111.27 (124%) | 1201.77 ± 269.95 (96%) | 1250 |
| Magnesium (mg) | 366.77 ± 33.82 (89%) | 317.94 ± 10.28 * (78%) | 434.89 ± 46.39 * (106%) | 340.3 ± 124.92 (83%) | 410 |
| Zinc (mg) | 16.97 ± 1.14 ** (154%) | 11.66 ± 0.53 (106%) | 12.37 ± 1.27 (112%) | 7.52 ± 1.97 (68%) | 11 |
| Calcium (mg) | 1240.58 ± 69.62 (95%) | 1115.52 ± 67.04 (86%) | 1043.74 ± 99.06 (80%) | 783.44 ± 196.3 (60%) | 1300 |
| Iron (mg) | 16.16 ± 1.4 (147%) | 15.48 ± 0.69 (141%) | 20.07 ± 1.93 (182%) | 16.02 ± 3.47 (146%) | 11 |
| Sodium (mg) | 3706.14 ± 222.95 (247%) | 3558.97 ± 210.45 (237%) | 3490.21 ± 173.58 (233%) | 3624.96 ± 719.27 (242%) | 1500 |
| Potassium (mg) | 3324.9 ± 121.42 * (111%) | 2847.72 ± 110.26 (95%) | 3145.88 ± 226.31 (105%) | 2958.59 ± 1612.81 (99%) | 3000 |
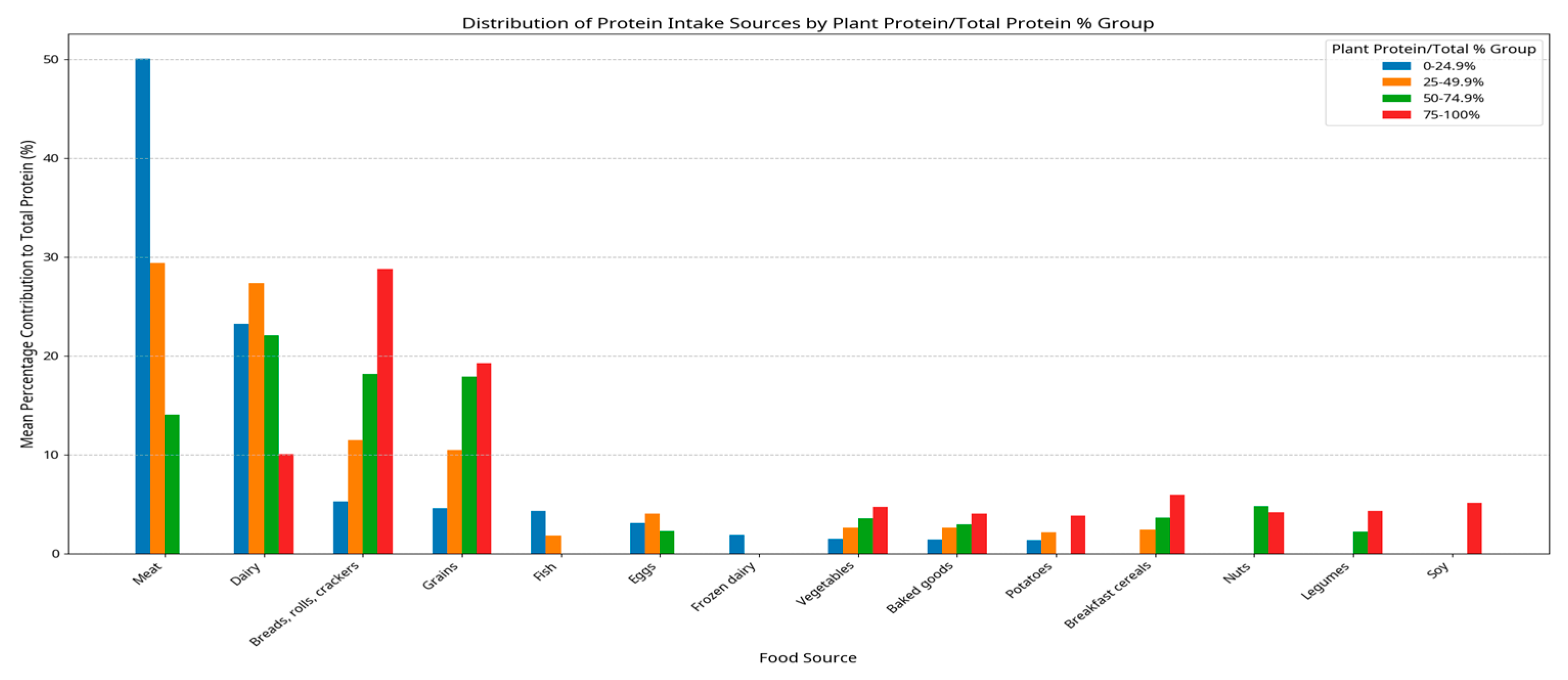
3.3. Protein Sources and Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Darnton-Hill, I.; Nishida, C.; James, W. A life course approach to diet, nutrition and the prevention of chronic diseases. Public Health Nutr. 2004, 7, 101–121. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, L.; Flores-Barrantes, P.; Moreno, L.A.; Manios, Y.; Gonzalez-Gil, E.M. The influence of parental dietary behaviors and practices on children’s eating habits. Nutrients 2021, 13, 1138. [Google Scholar] [CrossRef] [PubMed]
- Tugault-Lafleur, C.N.; Black, J.L. Lunch on school days in Canada: Examining contributions to nutrient and food group intake and differences across eating locations. J. Acad. Nutr. Diet. 2020, 120, 1484–1497. [Google Scholar] [CrossRef]
- Hack, S.; Jessri, M.; L’abbé, M.R. Nutritional quality of the food choices of Canadian children. BMC Nutr. 2021, 7, 16. [Google Scholar] [CrossRef]
- Food and Nutrition Highlights 2021. Helping You Maintain and Improve Your Health. 2021. Available online: https://www.canada.ca/en/health-canada/services/publications/food-nutrition/highlights-2021.html (accessed on 1 March 2025).
- Barr, S.I. Is the 2019 Canada’s food guide snapshot nutritionally adequate? Appl. Physiol. Nutr. Metab. 2019, 44, 1387–1390. [Google Scholar] [CrossRef]
- Fabek, H.; Sanchez-Hernandez, D.; Ahmed, M.; Marinangeli, C.P.; House, J.D.; Anderson, G.H. An examination of contributions of animal- and plant-based dietary patterns on the nutrient quality of diets of adult Canadians. Appl. Physiol. Nutr. Metab. 2021, 46, 877–886. [Google Scholar] [CrossRef]
- Auclair, O.; Burgos, S.A. Protein consumption in Canadian habitual diets: Usual intake, inadequacy, and the contribution of animal-and plant-based foods to nutrient intakes. Appl. Physiol. Nutr. Metab. 2021, 46, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Dietary Reference Intakes Tables: Overview. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/dietary-reference-intakes/tables.html (accessed on 1 March 2025).
- Reference Guide to Understanding and Using the Data. 2017. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/reference-guide-understanding-using-data-2015.html (accessed on 1 March 2025).
- Garriguet, D. Accounting for misreporting when comparing energy intake across time in Canada. Health Rep. 2018, 29, 3–12. [Google Scholar]
- Gorber, S.C.; Shields, M.; Tremblay, M.S.; McDowell, I. The feasibility of establishing correction factors to adjust self-reported estimates of obesity. Health Rep. 2008, 19, 71–82. [Google Scholar]
- BMI-for-Age (5–19 Years). Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (accessed on 1 March 2025).
- Tarasuk, V.; Beaton, G.H. Day-to-day variation in energy and nutrient intake: Evidence of individuality in eating behaviour? Appetite 1992, 18, 43–54. [Google Scholar] [CrossRef]
- Anderson, G.H.; Peterson, R.D.; Beaton, G.H. Estimating nutrient deficiencies in a population from dietary records: The use of probability analyses. Nutr. Res. 1982, 2, 409–415. [Google Scholar] [CrossRef]
- Beaton, G.H. The Use of Nutritional Requirements and Allowances. In Proceedings of the Western Hemisphere Nutrition Congress III; White, P.L., Selvey, N., Eds.; Futura Publishing Co., Inc.: Mount Kisco, NY, USA, 1971; pp. 356–363. [Google Scholar]
- Beaton, G.H. Evaluation of nutrient intake: New statistical approaches. Sep. Arch. Lationoamericanos Nutricion 1975, 25, 31–43. [Google Scholar]
- Marinangeli, C.P.; Fabek, H.; Ahmed, M.; Sanchez-Hernandez, D.; Foisy, S.; House, J.D. The effect of increasing intakes of plant protein on the protein quality of Canadian diets. Appl. Physiol. Nutr. Metab. 2021, 46, 771–780. [Google Scholar] [CrossRef] [PubMed]
- Tugault-Lafleur, C.N.; Black, J.L. Differences in the Quantity and Types of Foods and Beverages Consumed by Canadians between 2004 and 2015. Nutrients 2019, 11, 526. [Google Scholar] [CrossRef]
- Barbosa, F.d.S.; Sichieri, R.; Junger, W.L. Assessing usual dietary intake in complex sample design surveys: The National Dietary Survey. Rev. Saude Publica 2013, 47, 171–176. [Google Scholar] [CrossRef]
- Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids; National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Smit, E.; Nieto, F.J.; Crespo, C.J.; Mitchell, P. Estimates of animal and plant protein intake in US adults: Results from the Third National Health and Nutrition Examination Survey, 1988–1991. J. Am. Diet. Assoc. 1999, 99, 813–820. [Google Scholar] [CrossRef]
- Hoy, K.; Clemens, J.; Moshfegh, A. Estimated Protein Intake From Animal and Plant Foods by U.S. Adults, What We Eat in America, NHANES, 2015–2016. Curr. Dev. Nutr. 2021, 5, 133. [Google Scholar] [CrossRef]
- Grasso, A.C.; Olthof, M.R.; van Dooren, C.; Broekema, R.; Visser, M.; A Brouwer, I. Protein for a Healthy Future: How to Increase Protein Intake in an Environmentally Sustainable Way in Older Adults in the Netherlands. J. Nutr. 2020, 151, 109–119. [Google Scholar] [CrossRef]
- Valdes, M.; Conklin, A.; Veenstra, G.; Black, J.L. Plant-based dietary practices in Canada: Examining definitions, prevalence and correlates of animal source food exclusions using nationally representative data from the 2015 Canadian Community Health Survey–Nutrition. Public Health Nutr. 2021, 24, 777–786. [Google Scholar] [CrossRef]
- Chen, Z.H.; Mousavi, S.; Mandhane, P.J.; Simons, E.; Turvey, S.E.; Moraes, T.J.; Subbarao, P.; Miliku, K. Ultraprocessed Food Consumption and Obesity Development in Canadian Children. JAMA Netw. Open 2025, 8, e2457341. [Google Scholar] [CrossRef]
- Sodium Intake of Canadians in 2017. Available online: https://www.canada.ca/en/health-canada/services/publications/food-nutrition/sodium-intake-canadians-2017.html (accessed on 1 March 2025).
- Hosseini, S.H.; Papanikolaou, Y.; Isalm, N.; Rashmi, P.; Shamloo, A.; Vatanparast, H. Consumption Patterns of Grain-Based Foods among Children and Adolescents in Canada: Evidence from Canadian Community Health Survey-Nutrition 2015. Nutrients 2019, 11, 623. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, C.; Soto-Méndez, M.J.; Hernández-Ruiz, Á.; Valero, T.; Ávila, J.M.; Ruiz, E.; Villoslada, F.L.; Leis, R.; de Victoria, E.M.; Moreno, J.M.; et al. Energy Intake, Macronutrient Profile and Food Sources of Spanish Children Aged One to <10 Years—Results from the EsNuPI Study. Nutrients 2020, 12, 893. [Google Scholar] [CrossRef]
- Vatanparast, H.; Whiting, S.; Hossain, A.; Mirhosseini, N.; Merchant, A.T.; Szafron, M. National pattern of grain products consumption among Canadians in association with body weight status. BMC Nutr. 2017, 3, 59. [Google Scholar] [CrossRef]
- Munasinghe, L.L.; Yuan, Y.; Willows, N.D.; Faught, E.L.; Ekwaru, J.P.; Veugelers, P.J. Vitamin D deficiency and sufficiency among Canadian children residing at high latitude following the revision of the RDA of vitamin D intake in 2010. Br. J. Nutr. 2017, 117, 457–465. [Google Scholar] [CrossRef]
- Rizzoli, R. Dairy products, yogurts, and bone health123. Am. J. Clin. Nutr. 2014, 99, 1256S–1262S. [Google Scholar] [CrossRef]
- Wang, W.; Wu, Y.; Zhang, D. Association of dairy products consumption with risk of obesity in children and adults: A meta-analysis of mainly cross-sectional studies. Ann. Epidemiol. 2016, 26, 870–882.e2. [Google Scholar] [CrossRef] [PubMed]
- Dougkas, A.; Barr, S.; Reddy, S.; Summerbell, C.D. A critical review of the role of milk and other dairy products in the development of obesity in children and adolescents. Nutr. Res. Rev. 2018, 32, 106–127. [Google Scholar] [CrossRef] [PubMed]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Recommended dairy intake is associated with healthy dietary habits, better physical fitness, less obesity and a healthier lifestyle profile in school age children. Br. J. Nutr. 2022, 128, 2046–2053. [Google Scholar] [CrossRef]
- Marketing Authorization for Vitamin D in Milk, Goat’s Milk and Margarine: SOR/2021-278. 2021. Available online: https://gazette.gc.ca/rp-pr/p2/2022/2022-01-19/html/sor-dors278-eng.html (accessed on 1 March 2025).
- Islam, N.; Shafiee, M.; Vatanparast, H. Trends in the consumption of conventional dairy milk and plant-based beverages and their contribution to nutrient intake among Canadians. J. Hum. Nutr. Diet. 2021, 34, 1022–1034. [Google Scholar] [CrossRef]
- Singhal, S.; Baker, R.D.; Baker, S.S. A Comparison of the Nutritional Value of Cow’s Milk and Nondairy Beverages. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 799–805. [Google Scholar] [CrossRef]
- Morency, M.E.; Birken, C.S.; Lebovic, G.; Chen, Y.; L’Abbé, M.; Lee, G.J.; Maguire, J.L. Association between noncow milk beverage consumption and childhood height. Am. J. Clin. Nutr. 2017, 106, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Vanderhout, S.M.; Keown-Stoneman, C.D.G.; Birken, C.S.; O’connor, D.L.; Thorpe, K.E.; Maguire, J.L. Cow’s milk fat and child adiposity: A prospective cohort study. Int. J. Obes. 2021, 45, 2623–2628. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.A.; Bertolo, R.F.; Duncan, A.M.; Phillips, S.M.; Elango, R.; Ma, D.W.L.; Desroches, S.; Grantham, A.; House, J.D. Translating “protein foods” from the new Canada’s Food Guide to consumers: Knowledge gaps and recommendations. Appl. Physiol. Nutr. Metab. 2020, 45, 1311–1323. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Martínez Steele, E.; Du, M.; Pomeranz, J.L.; O’Connor, L.E.; Herrick, K.A.; Luo, H.; Zhang, X.; Mozaffarian, D.; Zhang, F.F. Trends in Consumption of Ultraprocessed Foods Among US Youths Aged 2–19 Years, 1999–2018. J. Am. Med. Assoc. 2021, 326, 519. [Google Scholar] [CrossRef]
| Plant Protein Groups 1 | ||||
|---|---|---|---|---|
| 0–24.9% | 25–49.9% | 50–74.9% | 75–100% | |
| All Children (n = 2324) | ||||
| N | 691 (29.73%) | 1246 (53.61%) | 324 (13.94%) | 63 (2.71%) |
| Weight (kg) | 55.74 ± 1.24 | 54.84 ± 1.02 | 55.62 ± 2.16 | 50.37 ± 5.19 |
| Height (m) | 1.6 ± 0.01 | 1.58 ± 0.01 | 1.59 ± 0.02 | 1.58 ± 0.03 |
| BMI | 21. 42 ± 0.29 | 21.47 ± 0.27 | 21.55 ± 0.47 | 20.02 ± 1.54 |
| Age (y) | 13.58 ± 0.17 | 13.06± 0.13 | 13.3± 0.29 | 13.55± 0.66 |
| Females (n = 1151) | ||||
| N | 300 (26.06%) | 623 (54.13%) | 183 (15.90%) | 45 (3.91%) |
| Weight (kg) | 53.72 ± 1.37 * | 51.64 ± 1 | 51.98 ± 1.82 | 50.06 ± 6.72 |
| Height (m) | 1.57 ± 0.01 | 1.55 ± 0.01 | 1.56 ± 0.01 | 1.56 ± 0.03 |
| BMI | 21.59 ± 0.41 | 21.12 ± 0.34 | 21.08 ± 0.56 | 20. 24 ± 2.21 |
| Age (y) | 13.75 ± 0.23 | 12.92 ± 0.16 | 13.36 ± 0.3 | 13.83 ± 0.8 |
| Males (n = 1173) | ||||
| N | 391 (33.33%) | 623 (53.11%) | 141 (12.02%) | 18 (1.53%) |
| Weight (kg) | 57.43 ± 1.86 | 57.56 ± 1.63 | 59.92 ± 4.7 | 51.19 ± 6.99 |
| Height (m) | 1.62 ± 0.01 | 1.6 ± 0.01 | 1.62 ± 0.03 | 1.61 ± 0.07 |
| BMI 2 | 21.28 ± 0.41 | 21.77 ± 0.43 | 22.10 ± 0.96 | 19.42 ± 1.31 |
| Age (y) | 13.44 ± 0.26 | 13.18 ± 0.19 | 13.23 ± 0.53 | 12.82 ± 1.31 |
| Plant Protein/Total % | 0–24.9% (n = 691) | 25–49.9% (n = 1246) | 50–74.9% (n = 324) | 75–100% (n = 63) |
|---|---|---|---|---|
| Total fat (g) | 37.93 ± 0.62 ** | 35.61 ± 0.38 | 32.77 ± 0.76 ** | 28.4 ± 1.83 ** |
| Total protein (g) | 51.1 ± 1.72 *** | 37.14 ± 0.37 | 31.9 ± 1.23 ** | 27.98 ± 1.5 *** |
| Total carbohydrate (g) | 114.69 ± 2.01 *** | 135.66 ± 0.93 | 148.31 ± 1.69 *** | 163.65 ± 4.1 *** |
| Total dietary fiber (g) | 6.43 ± 0.18 *** | 8.49 ± 0.15 | 10.53 ± 0.26 *** | 13.26 ± 0.85 *** |
| Total saturated fatty acids (g) | 14.08 ± 0.32 ** | 12.58 ± 0.17 | 10.24 ± 0.29 *** | 8.51 ± 0.62 *** |
| Cholesterol (mg) | 173.83 ± 5.59 *** | 121.42 ± 4.35 | 64.81 ± 4.83 *** | 36.76 ± 6.49 *** |
| MUFA (g) | 13.85 ± 0.3 * | 12.87 ± 0.17 | 12.06 ± 0.46 | 9.63 ± 0.93 ** |
| PUFA (g) | 6.66 ± 0.17 | 6.95 ± 0.19 | 7.34 ± 0.24 | 7.06 ± 0.83 |
| Linoleic fatty acids (g) | 5.56 ± 0.16 | 5.97 ± 0.18 | 6.46 ± 0.22 | 6.11 ± 0.76 |
| Linolenic fatty acids (g) | 0.7 ± 0.02 | 0.73 ± 0.03 | 0.74 ± 0.03 | 0.79 ± 0.09 |
| Vitamin D (mcg) | 3.71 ± 0.24 ** | 2.81 ± 0.1 | 2.33 ± 0.26 | 1.55 ± 0.22 *** |
| Folate (mcg) | 82.61 ± 2.71 ** | 94.11 ± 1.99 | 101.26 ± 6.89 | 128.74 ± 11.13 * |
| Folic acid (mcg) | 50.75 ± 4.85 *** | 76.85 ± 2.43 | 99.92 ± 7.14 * | 102.55 ± 10.52 |
| Dietary folate equivalents (mcg) | 183.59 ± 9.98 *** | 250.01 ± 4.11 | 297.64 ± 10.2 *** | 328.42 ± 26.74 ** |
| Folacin (mcg) | 133.58 ± 6.72 *** | 170.59 ± 2.41 | 201.32 ± 6.72 ** | 231.63 ± 12.94 *** |
| Vitamin B12 (mcg) | 3.29 ± 0.23 *** | 2.21 ± 0.29 | 1.25 ± 0.09 *** | 0.68 ± 0.09 *** |
| Thiamin (mg) | 0.81 ± 0.02 ** | 0.9 ± 0.02 | 1.01 ± 0.05 | 1.27 ± 0.11** |
| Riboflavin (mg) | 1.11 ± 0.04 ** | 0.99 ± 0.02 | 0.89 ± 0.04 | 0.8 ± 0.05** |
| Niacin (mg) | 23.74 ± 0.99 *** | 17.52 ± 0.22 | 16.72 ± 0.66 | 16.03 ± 0.82 |
| Vitamin B6 (mg) | 1.01 ± 0.06 *** | 0.74 ± 0.02 | 0.71 ± 0.03 | 0.75 ± 0.07 |
| Phosphorus (mg) | 772.93 ± 18.36 *** | 671.76 ± 7.36 | 618.67 ± 21.35 * | 539.61 ± 33.4** |
| Magnesium (mg) | 138.66 ± 5.27 | 137.83 ± 1.72 | 156.42 ± 6.15 * | 167.45 ± 10.29* |
| Zinc (mg) | 6.73 ± 0.34 *** | 4.9 ± 0.08 | 4.41 ± 0.19 | 3.84 ± 0.2 *** |
| Calcium (mg) | 522.6 ± 19.1 | 512.21 ± 9.63 | 446.78 ± 20.54 ** | 372.56 ± 40.69** |
| Iron (mg) | 6.14 ± 0.24 *** | 6.88 ± 0.1 | 7.6 ± 0.27 * | 7.95 ± 0.45* |
| Sodium (mg) | 1450.65 ± 40.61 | 1477.51 ± 24.18 | 1389.12 ± 30.16 | 1328.79 ± 77.08 |
| Potassium (mg) | 1377.01 ± 22.57 ** | 1274.95 ± 21.22 | 1225.47 ± 38.81 | 1258.76 ± 127.09 |
| Plant Protein/Total % | 0–24.9% (n = 146) | 25–49.9% (n = 350) | 50–74.9% (n = 97) | 75–100% (n = 16) | RDA AI |
|---|---|---|---|---|---|
| Total energy (kcal) | 1919.7 ± 37.04 | 1878.03 ± 54.76 | 1816.85 ± 48.07 | 1765.69 ± 138.18 | |
| Total fat (g) | 71.93 ± 2.64 | 64.9 ± 2.38 | 56.35 ± 2.73 | 47.67 ± 8.82 | ND |
| Total protein (g) | 93.25 ± 4.22 *** (274%) | 67.78 ± 2.05 (199%) | 52.58 ± 2.1 *** (155%) | 49.71 ± 7.42 (146%) | 34 |
| Total carbohydrate (g) | 228.5 ± 8.95 ** (176%) | 261.46 ± 8.14 (201%) | 281.73 ± 9.37 (217%) | 291.49 ± 32.34 (224%) | 130 |
| Total dietary fiber (g) | 12.93 ± 0.8 ** (50%) | 16.19 ± 0.63 (62%) | 17.69 ± 0.99 (68%) | 17.74 ± 2.2 (68%) | 26 |
| Total saturated fatty acids (g) | 27.56 ± 1.31 * | 23.43 ± 0.85 | 18.57 ± 1.12 ** | 15.02 ± 2.58 * | As low as possible |
| Linoleic fatty acids (g) | 9.87 ± 0.79 (99%) | 10.76 ± 0.58 (108%) | 10.93 ± 0.72 (109%) | 9.29 ± 2.78 (93%) | 10 |
| Linolenic fatty acids (g) | 1.31 ± 0.1 (131%) | 1.34 ± 0.06 (134%) | 1.43 ± 0.14 (143%) | 1.09 ± 0.31 (109%) | 1 |
| Vitamin D (mcg) | 7.14 ± 1.04 (48%) | 5.42 ± 0.25 (36%) | 4.51 ± 0.66 (30%) | 2.21 ± 0.61 ** (15%) | 15 |
| Folate equivalents(mcg) | 170.82 ± 9.44 (57%) | 182.78 ± 10.44 (61%) | 165.06 ± 13.11 (55%) | 212.26 ± 57.32 (71%) | 300 |
| Vitamin B12 (mcg) | 5.54 ± 0.45 ** (308%) | 5.32 ± 1.67 (296%) | 2.04 ± 0.2 *** (113%) | 1.06 ± 0.24 *** (59%) | 1.8 |
| Thiamin (mg) | 1.6 ± 0.1 (178%) | 1.72 ± 0.07 (191%) | 1.95 ± 0.19 (217%) | 1.95 ± 0.26 (217%) | 0.9 |
| Riboflavin (mg) | 2.1 ± 0.09 (233%) | 1.91 ± 0.11 (212%) | 1.61 ± 0.11 (179%) | 1.4 ± 0.24 (156%) | 0.9 |
| Niacin Equivalents (mg) | 42.04 ± 2.56 *** (350%) | 31.59 ± 1.08 (263%) | 27.78 ± 1.34 (232%) | 28.19 ± 2.6 (235%) | 12 |
| Vitamin B6 (mg) | 1.74 ± 0.09 ** (174%) | 1.34 ± 0.05 (134%) | 1.15 ± 0.09 (115%) | 1.01 ± 0.2 (101%) | 1.0 |
| Phosphorus (mg) | 1476.75 ± 56.15* (118%) | 1252.3 ± 37.14 (100%) | 1017.66 ± 54.28** (81%) | 835.56 ± 128.6 * (67%) | 1250 |
| Magnesium (mg) | 260.3 ± 7.45 (108%) | 256.89 ± 7.26 (107%) | 245.08 ± 12.49 (102%) | 234.44 ± 22.5 (98%) | 240 |
| Zinc (mg) | 11.71 ± 0.68 *** (146%) | 9.06 ± 0.32 (113%) | 7 ± 0.31 *** (88%) | 5.92 ± 0.84 * (74%) | 8.0 |
| Calcium (mg) | 1040.39 ± 82.36 (80%) | 985.14 ± 41.27 (76%) | 822.08 ± 100.72 (63%) | 542.93 ± 139.08 * (42%) | 1300 |
| Iron (mg) | 11.86 ± 0.41 ** (148%) | 13.85 ± 0.42 (173%) | 13.92 ± 0.55 (174%) | 14.1 ± 0.99 (176%) | 8 |
| Sodium (mg) | 2696.09 ± 124.01 (225%) | 2644.24 ± 93.01 (220%) | 2583.63 ± 125.65 (215%) | 2300.3 ± 295.81 (192%) | 1200 |
| Potassium (mg) | 2745.27 ± 89.76 ** (119%) | 2438.86 ± 91.87 (106%) | 2144.69 ± 166 (93%) | 1964.31 ± 269.35 (85%) | 2300 |
| Plant Protein/Total% | 0–24.9% (n = 210) | 25–49.9% (n = 353) | 50–74.9% (n = 83) | 75–100% (n = 11) | RDA AI |
|---|---|---|---|---|---|
| Total energy (kcal) | 2055.53 ± 49.24 | 2022.08 ± 47.28 | 1870.76 ± 56.86 | 2086.8 ± 185.15 | |
| Total fat (g) | 79.45 ± 2.62 | 71.55 ± 2.12 | 62.57 ± 4.6 | 66.54 ± 7.69 | ND |
| Total protein (g) | 95.79 ± 4.47 ** (282%) | 75.47 ± 2.23 (222%) | 59.67 ± 3.37 ** (176%) | 49.37 ± 6.45 ** (145%) | 34 |
| Total carbohydrate (g) | 243.61 ± 8.59 ** (187%) | 275.14 ± 6.68 (212%) | 274.62 ± 9.19 (211%) | 332.17 ± 30.65 (256%) | 130 |
| Total dietary fiber (g) | 13.62 ± 0.8 ** (44%) | 17.47 ± 0.74 (56%) | 21.07 ± 1.34 * (68%) | 28.18 ± 6.76 (91%) | 31 |
| Total saturated fatty acids (g) | 30.67 ± 1.31 ** | 25.49 ± 0.99 | 20.49 ± 1.09 * | 17.07 ± 2.91 | As low as possible |
| Linoleic fatty acids (g) | 10.95 ± 0.74 (91%) | 11.83 ± 0.44 (99%) | 12.08 ± 1.46 (101%) | 13.83 ± 2.19 (115%) | 12 |
| Linolenic fatty acids (g) | 1.35 ± 0.07 (113%) | 1.5 ± 0.08 (125%) | 1.53 ± 0.16 (128%) | 1.3 ± 0.2 (108%) | 1.2 |
| Vitamin D (mcg) | 6.55 ± 0.6 (44%) | 5.74 ± 0.38 (38%) | 4.13 ± 0.48 (28%) | 4.07 ± 1.22 (27%) | 15 |
| Folate (mcg) | 154.08 ± 9.3 * (51%) | 185.41 ± 7.8 (62%) | 199.39 ± 21.83 (66%) | 210.34 ± 38.88 (70%) | 300 |
| Vitamin B12 (mcg) | 5.95 ± 0.35 *** (331%) | 3.85 ± 0.19 (214%) | 2.43 ± 0.25 *** (135%) | 1.36 ± 0.51 ** (76%) | 1.8 |
| Thiamin (mg) | 1.57 ± 0.1 * (174%) | 1.85 ± 0.06 (206%) | 1.78 ± 0.16 (198%) | 2.78 ± 0.43 * (309%) | 0.9 |
| Riboflavin (mg) | 2.2 ± 0.1 (244%) | 2.01 ± 0.07 (223%) | 1.56 ± 0.07 *** (173%) | 1.73 ± 0.31 (192%) | 0.9 |
| Niacin (mg) | 42.95 ± 1.98 * (358%) | 35.46 ± 0.98 (296%) | 29.38 ± 1.29 ** (245%) | 31.36 ± 4.57 (261%) | 12 |
| Vitamin B6 (mg) | 1.73 ± 0.09 (173%) | 1.51 ± 0.05 (151%) | 1.25 ± 0.1 (125%) | 1.77 ± 0.27 (177%) | 1.0 |
| Phosphorus (mg) | 1506.03 ± 51.02 (120%) | 1366.13 ± 40.28 (109%) | 1223 ± 51.2 (98%) | 1104.14 ± 151.52 (88%) | 1250 |
| Magnesium (mg) | 264.26 ± 11.26 (110%) | 277.22 ± 7.72 (116%) | 280.34 ± 13.55 (117%) | 348.99 ± 52.12 (145%) | 240 |
| Zinc (mg) | 13.34 ± 0.94 ** (167%) | 9.93 ± 0.34 (124%) | 8.31 ± 0.44 (104%) | 7.61 ± 1.25 (95%) | 8.0* |
| Calcium (mg) | 1091.97 ± 49.88 (84%) | 1043.29 ± 40.21 (80%) | 902.89 ± 65 (69%) | 591.26 ± 90.62 *** (45%) | 1300 |
| Iron (mg) | 12.58 ± 0.64 (157%) | 14.39 ± 0.48 (180%) | 14.24 ± 0.89 (178%) | 15.24 ± 1.83 (190%) | 8 |
| Sodium (mg) | 3003.33 ± 145.77 (250%) | 3069.49 ± 98.86 (256%) | 2731.4 ± 114.66 (228%) | 2576.68 ± 225.74 (215%) | 1200 |
| Potassium (mg) | 2752.18 ± 101.77 (110%) | 2629.57 ± 82.74 (105%) | 2233.12 ± 153.28 (89%) | 2595 ± 360.22 (104%) | 2500 |
| Plant Protein/Total % | 0–24.9% (n = 154) | 25–49.9% (n = 273) | 50–74.9% (n = 86) | 75–100% (n = 29) | RDA AI |
|---|---|---|---|---|---|
| Total energy (kcal) | 1882.86 ± 62.56 | 1836.29 ± 29.25 | 1823.57 ± 53.93 | 1637.49 ± 53.8 * | |
| Total fat (g) | 74.83 ± 3.68 | 66.67 ± 1.67 | 62.25 ± 3.46 | 47.74 ± 3.46 ** | ND |
| Total protein (g) | 95.5 ± 6.07 (208%) | 69.97 ± 1.85 (152%) | 56.33 ± 2.95 ** (122%) | 48.81 ± 4.23 *** (106%) | 46 |
| Total carbohydrate (g) | 207.97 ± 11.14 ** (160%) | 244.41 ± 4.59 (188%) | 269.09 ± 9.54 * (207%) | 263.54 ± 13.02 (203%) | 130 |
| Total dietary fiber (g) | 11.55 ± 0.91 ** (44%) | 15.19 ± 0.85 (58%) | 19.49 ± 1.19 * (75%) | 25.97 ± 2.92 ** (100%) | 26 |
| Total saturated fatty acids (g) | 28.16 ± 1.82 | 23.75 ± 0.84 | 18.32 ± 1.27 * | 14.6 ± 1.61 *** | As low as possible |
| Linoleic fatty acids (g) | 10.92 ± 0.7 (99%) | 11.29 ± 0.47 (103%) | 12.37 ± 0.98 (112%) | 10.91 ± 2.24 (99%) | 11 |
| Linolenic fatty acids (g) | 1.44 ± 0.11 (131%) | 1.39 ± 0.08 (126%) | 1.24 ± 0.08 (113%) | 1.46 ± 0.28 (133%) | 1.1 |
| Vitamin D (mcg) | 8.42 ± 1.12 ** (56%) | 4.95 ± 0.3 (33%) | 4.04 ± 0.86 (27%) | 2.79 ± 0.6 * (19%) | 15 |
| Folate (mcg) | 153.35 ± 9.01 (38%) | 176.24 ± 7.93 (44%) | 200.95 ± 27.01 (50%) | 220.72 ± 20.6 (55%) | 400 |
| Vitamin B12 (mcg) | 6.76 ± 1.01 ** (282%) | 3.37 ± 0.15 (140%) | 2.22 ± 0.36 * (93%) | 1.2 ± 0.3 ** (50%) | 2.4 |
| Thiamin (mg) | 1.47 ± 0.1 (147%) | 1.6 ± 0.08 (160%) | 1.59 ± 0.1 (159%) | 2.24 ± 0.33 (224%) | 1.0 |
| Riboflavin (mg) | 2.01 ± 0.11 (201%) | 1.8 ± 0.05 (180%) | 1.61 ± 0.14 (161%) | 1.26 ± 0.1 ** (126%) | 1.0 |
| Niacin (mg) | 43.48 ± 3.23 (311%) | 32.85 ± 1.01 (235%) | 28.41 ± 1.22 * (203%) | 25.74 ± 1.64 ** (184%) | 14 |
| Vitamin B6 (mg) | 1.75 ± 0.12 * (146%) | 1.32 ± 0.09 (110%) | 1.31 ± 0.11 (109%) | 1.41 ± 0.13 (118%) | 1.2 |
| Phosphorus (mg) | 1438.73 ± 59.32 * (115%) | 1246.94 ± 33.94 (100%) | 1160.88 ± 100.49 (93%) | 958.56 ± 85.43 * (77%) | 1250 |
| Magnesium (mg) | 251.5 ± 9.08 (70%) | 255 ± 10.45 (71%) | 299.57 ± 21.91 (83%) | 311.95 ± 22.83 * (87%) | 360 |
| Zinc (mg) | 12.77 ± 1.35 * (142%) | 8.96 ± 0.39 (100%) | 7.76 ± 0.43 (86%) | 7.11 ± 0.58 (79%) | 9 |
| Calcium (mg) | 972.51 ± 88.83 (75%) | 945.08 ± 35.09 (73%) | 805.35 ± 92.1 (62%) | 726.1 ± 120.05 (56%) | 1300 |
| Iron (mg) | 10.78 ± 0.5 (72%) | 11.75 ± 0.49 (78%) | 13.02 ± 0.78 (87%) | 14.11 ± 1.31 * (94%) | 15 |
| Sodium (mg) | 2688.5 ± 190.71 (179%) | 2702.66 ± 67.29 (180%) | 2267.82 ± 107.39 ** (151%) | 2140.68 ± 257.74 (143%) | 1500 |
| Potassium (mg) | 2555.75 ± 93.39 * (111%) | 2269.72 ± 77.24 (99%) | 2254.66 ± 151.48 (98%) | 2181.56 ± 234.46 (95%) | 2300 |
| Protein Source | All Children (n = 2324) | Females (n = 1151) | Males (n = 1173) |
|---|---|---|---|
| Animal protein (%) | 64.20 ± 0.71 | 62.75 ± 1.02 | 65.53 ± 0.87 |
| Plant protein (%) | 35.80 ± 0.71 | 37.25 ± 1.02 | 34.47 ± 0.87 |
| Plant Protein Group 1 | |||||
|---|---|---|---|---|---|
| 0–24.9% (n = 691) | 25–49.9% (n = 1246) | 50–74.9% (n = 324) | 75–100% (n = 63) | Requirements (RDA) | |
| PDCAAS | 0.99 ± 0.002 *** | 0.97 ± 0.003 | 0.86 ± 0.008 *** | 0.67 ± 0.027 *** | ~1 |
| Total protein (g) | 106.12 ± 3.46 *** | 75.29 ± 1.12 | 63.68 ± 3.46 ** | 50.07 ± 3.95 *** | range: 34–52, depending on age/sex |
| Energy from protein (kcal) | 20.37 ± 0.71 *** | 14.69 ± 0.15 | 12.54 ± 0.49 ** | 10.94 ± 0.57 *** | 10–30% of total energy intake |
| Protein by weight (g/kg) | 2.02 ± 0.05 *** | 1.52 ± 0.03 | 1.24 ± 0.04 *** | 1.06 ± 0.08 *** | range: 0.85–0.95, depending on age group |
| Corrected protein by weight (g/kg) | 1.99 ± 0.05 *** | 1.47 ± 0.03 | 1.03 ± 0.04 *** | 0.68 ± 0.06 *** | range: 0.85–0.95, depending on age group |
| Corrected protein (g) | 104.09 ± 3.41 *** | 72.34 ± 1.12 | 53.37 ± 3.17 *** | 32.16 ± 3.64 *** | range: 34–52, depending on age/sex |
| Energy from corrected protein (kcal) | 20.07 ± 0.69 *** | 14.28 ± 0.16 | 10.71 ± 0.48 *** | 7.23 ± 0.66 *** | 10–30% of total energy intake |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabek, H.; Salamat, S.; Anderson, G.H. Association Between Dietary Protein Sources and Nutrient Intake in the Diet of Canadian Children. Nutrients 2025, 17, 1834. https://doi.org/10.3390/nu17111834
Fabek H, Salamat S, Anderson GH. Association Between Dietary Protein Sources and Nutrient Intake in the Diet of Canadian Children. Nutrients. 2025; 17(11):1834. https://doi.org/10.3390/nu17111834
Chicago/Turabian StyleFabek, Hrvoje, Shekoufeh Salamat, and G. Harvey Anderson. 2025. "Association Between Dietary Protein Sources and Nutrient Intake in the Diet of Canadian Children" Nutrients 17, no. 11: 1834. https://doi.org/10.3390/nu17111834
APA StyleFabek, H., Salamat, S., & Anderson, G. H. (2025). Association Between Dietary Protein Sources and Nutrient Intake in the Diet of Canadian Children. Nutrients, 17(11), 1834. https://doi.org/10.3390/nu17111834







