Bifidobacterium adolescentis SBT2786 Improves Sleep Quality in Japanese Adults with Relatively High Levels of Stress: A Randomized, Double-Blind, Placebo-Controlled Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Statement
2.2. Participants
2.3. Sample Size
2.4. Randomization
2.5. Test Foods
2.6. Outcomes
2.7. Measurement and Analysis of Sleep Electroencephalogram
2.8. Sleepiness and Physical Condition Assessment Using Questionnaires
2.9. Evaluation of Biological Indicators
2.10. Safety Assessments
2.11. Statistical Analysis
3. Results
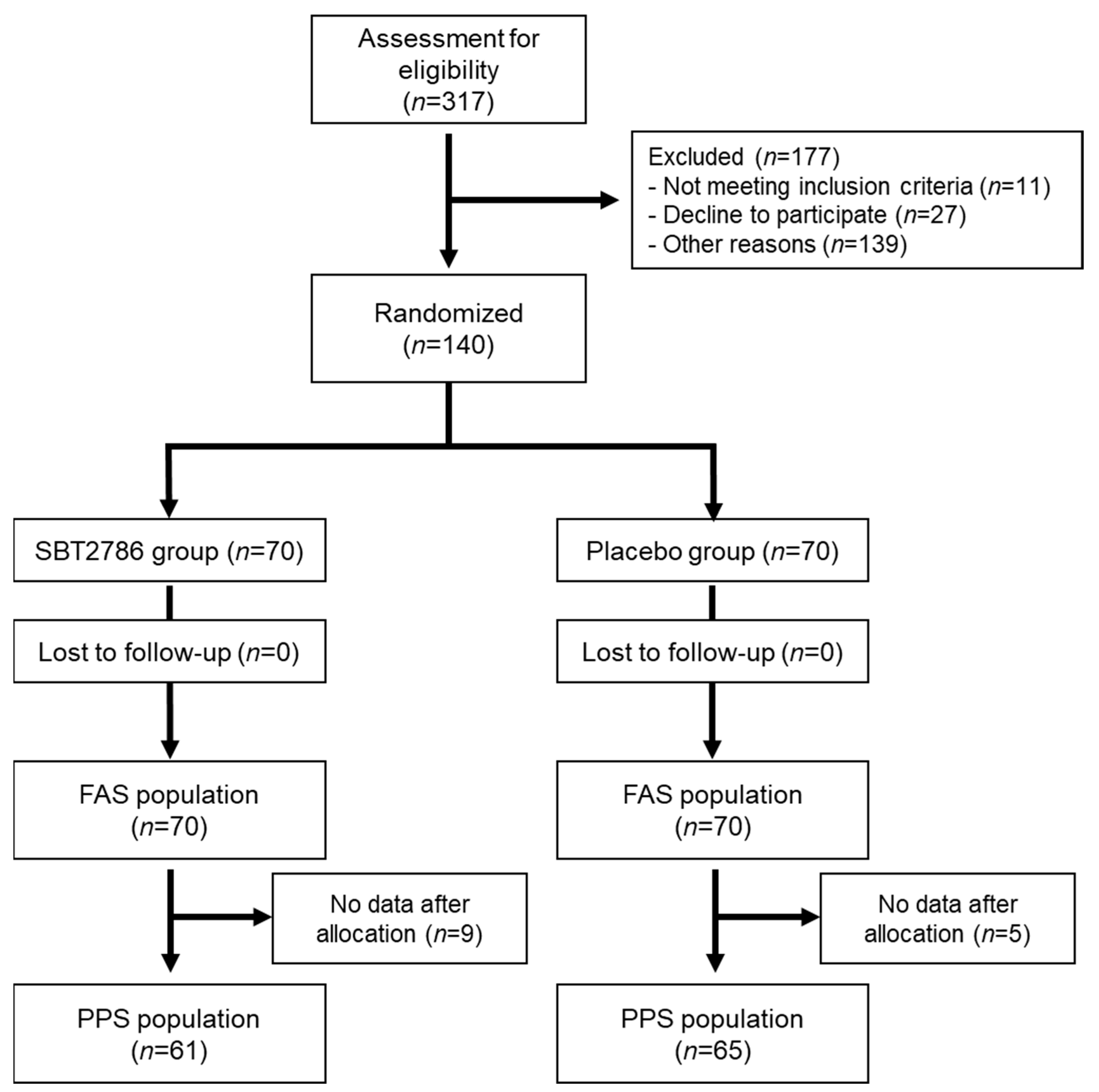
3.1. Participants
3.2. Participant Information
3.3. Primary Outcome
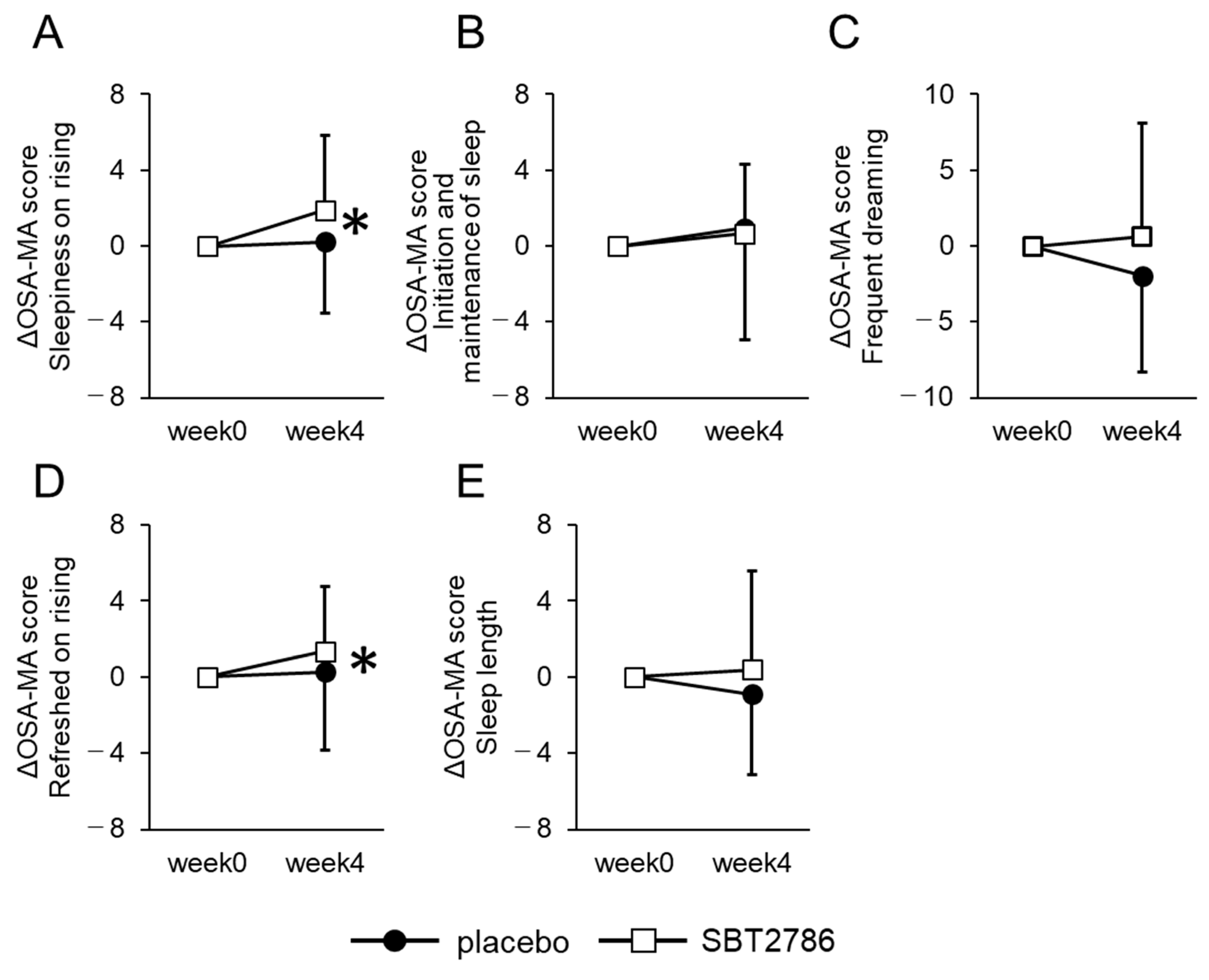
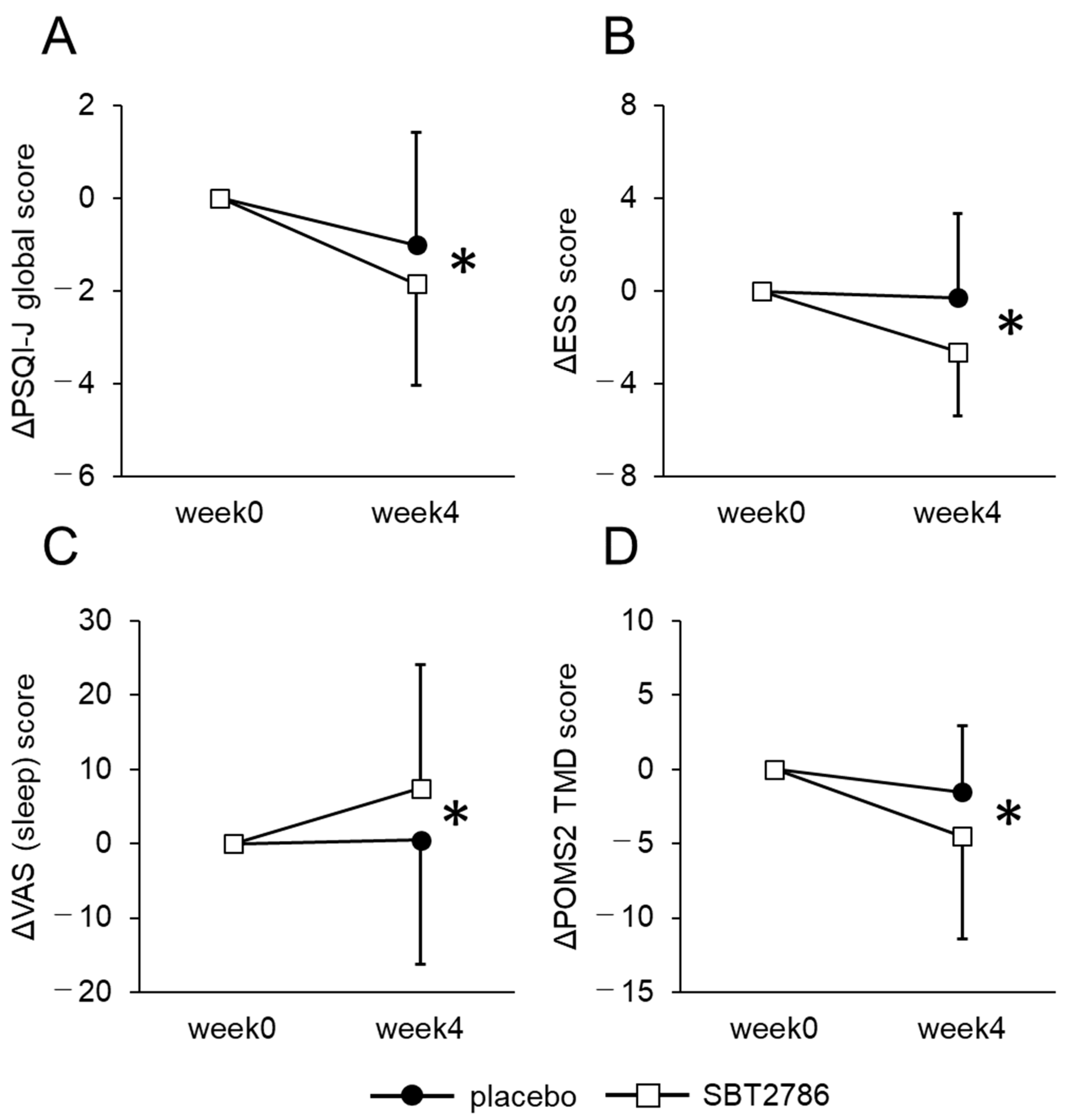
3.4. Secondary Outcomes
3.5. Subgroup Analysis
3.6. Safety Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hafner, M.; Stepanek, M.; Taylor, J.; Troxel, W.; Stolk, C. Why Sleep Matters—The Economic Costs of Insufficient Sleep: A Cross-Country Comparative Analysis; RAND Corporation: Santa Monica, CA, USA, 2016. [Google Scholar]
- Basner, M.; Fomberstein, K.M.; Razavi, F.M.; Banks, S.; William, J.H.; Rosa, R.R.; Dinges, D.F. American Time Use Survey: Sleep Time and Its Relationship to Waking Activities. Sleep 2007, 30, 1085–1095. [Google Scholar] [CrossRef]
- Ikehara, S.; Iso, H.; Date, C.; Kikuchi, S.; Watanabe, Y.; Wada, Y.; Inaba, Y.; Tamakoshi, A. Association of Sleep Duration with Mortality from Cardiovascular Disease and Other Causes for Japanese Men and Women: The JACC Study. Sleep 2009, 32, 295–301. [Google Scholar] [CrossRef]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index. PLoS Med. 2004, 1, 210–217. [Google Scholar] [CrossRef]
- Ayas, N.T.; White, D.P.; Al-Delaimy, W.K.; Manson, J.E.; Stampfer, M.J.; Speizer, F.E.; Patel, S.; Hu, F.B. A Prospective Study of Self-Reported Sleep Duration and Incident Diabetes in Women. Diabetes Care 2003, 26, 380–384. [Google Scholar] [CrossRef]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a Predictor of Depression: A Meta-Analytic Evaluation of Longitudinal Epidemiological Studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Ciorba, M.A. A Gastroenterologist’s Guide to Probiotics. Clin. Gastroenterol. Hepatol. 2012, 10, 960–968. [Google Scholar] [CrossRef]
- Yan, F.; Polk, D.B. Probiotics and Immune Health. Curr. Opin. Gastroenterol. 2011, 27, 496–501. [Google Scholar] [CrossRef]
- Shi, L.H.; Balakrishnan, K.; Thiagarajah, K.; Mohd Ismail, N.I.; Yin, O.S. Beneficial Properties of Probiotics. Trop. Life Sci. Res. 2016, 27, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Savignac, H.M.; Tramullas, M.; Kiely, B.; Dinan, T.G.; Cryan, J.F. Bifidobacteria Modulate Cognitive Processes in an Anxious Mouse Strain. Behav. Brain Res. 2015, 287, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Bravo, J.A.; Forsythe, P.; Chew, M.V.; Escaravage, E.; Savignac, H.M.; Dinan, T.G.; Bienenstock, J.; Cryan, J.F. Ingestion of Lactobacillus Strain Regulates Emotional Behavior and Central GABA Receptor Expression in a Mouse via the Vagus Nerve. Proc. Natl. Acad. Sci. USA 2011, 108, 16050–16055. [Google Scholar] [CrossRef]
- Smith, R.P.; Easson, C.; Lyle, S.M.; Kapoor, R.; Donnelly, C.P.; Davidson, E.J.; Parikh, E.; Lopez, J.V.; Tartar, J.L. Gut Microbiome Diversity Is Associated with Sleep Physiology in Humans. PLoS ONE 2019, 14, e0222394. [Google Scholar] [CrossRef]
- Kato-Kataoka, A.; Nishida, K.; Takada, M.; Kawai, M.; Kikuchi-Hayakawa, H.; Suda, K.; Ishikawa, H.; Gondo, Y.; Shimizu, K.; Matsuki, T.; et al. Fermented Milk Containing Lactobacillus casei Strain Shirota Preserves the Diversity of the Gut Microbiota and Relieves Abdominal Dysfunction in Healthy Medical Students Exposed to Academic Stress. Appl. Environ. Microbiol. 2016, 82, 3649–3658. [Google Scholar] [CrossRef] [PubMed]
- Nishida, K.; Sawada, D.; Kuwano, Y.; Tanaka, H.; Rokutan, K. Health Benefits of Lactobacillus gasseri Cp2305 Tablets in Young Adults Exposed to Chronic Stress: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients 2019, 11, 1859. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.C.N.; Wang, Q.P.; Morimoto, J.; Senior, A.M.; Lihoreau, M.; Neely, G.G.; Simpson, S.J.; Ponton, F. Gut Microbiota Modifies Olfactory-Guided Microbial Preferences and Foraging Decisions in Drosophila. Curr. Biol. 2017, 27, 2397–2404.e4. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, J.C.; Finn, S.M.; Panckeri, K.A.; Chavkin, J.; Williams, J.A.; Sehgal, A.; Pack, A.I. Rest in Drosophila Is a Sleep-like State. Neuron 2000, 25, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.J.; Cirelli, C.; Greenspan, R.J.; Tononi, G.; Campbell, S.S.; Tobler, I.; Zepelin, H.; Rechtschaffen, A.; Rechtschaffen, A.; Tobler, I.; et al. Correlates of Sleep and Waking in Drosophila melanogaster. Science 2000, 287, 1834–1837. [Google Scholar] [CrossRef] [PubMed]
- Ly, S.; Pack, A.I.; Naidoo, N. The Neurobiological Basis of Sleep: Insights from Drosophila. Neurosci. Biobehav. Rev. 2018, 87, 67–86. [Google Scholar] [CrossRef] [PubMed]
- Ko, T.; Murakami, H.; Kobayashi, S.; Kamikouchi, A.; Ishimoto, H. Behavioral Screening of Sleep-Promoting Effects of Human Intestinal and Food-Associated Bacteria on Drosophila melanogaster. Genes Cells 2023, 28, 433–446. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Tanaka, H.; Takase, M.; Yamazaki, K.; Azumi, K.; Shirakawa, S. Standardization of Revised Version of OSA Sleep Inventory for Middle Age and Aged. Brain Sci. Ment. Disord. 1999, 10, 401–409. [Google Scholar]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M.; Kim, K.; Shibui, K.; Kamei, Y. Psychometric Assessment of Subjective Sleep Quality Using the Japanese Version of the Pittsburgh Sleep Quality Index (PSQI-J) in Psychiatric Disordered and Control Subjects. Psychiatry Res. 2000, 97, 165–172. [Google Scholar] [CrossRef]
- Takegami, M.; Suzukamo, Y.; Wakita, T.; Noguchi, H.; Chin, K.; Kadotani, H.; Inoue, Y.; Oka, Y.; Nakamura, T.; Green, J.; et al. Development of a Japanese Version of the Epworth Sleepiness Scale (JESS) Based on Item Response Theory. Sleep Med. 2009, 10, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Hsiao, Y.-Y.; Wang, M. Test Review: The Profile of Mood States 2nd Edition. J. Psychoeduc. Assess. 2014, 32, 273–277. [Google Scholar] [CrossRef]
- Mao, Y.; Raju, G.; Zabidi, M.A. Association between Occupational Stress and Sleep Quality: A Systematic Review. Nat. Sci. Sleep 2023, 15, 931–947. [Google Scholar] [CrossRef] [PubMed]
- Nater, U.M.; Rohleder, N.; Gaab, J.; Berger, S.; Jud, A.; Kirschbaum, C.; Ehlert, U. Human Salivary Alpha-Amylase Reactivity in a Psychosocial Stress Paradigm. Int. J. Psychophysiol. 2005, 55, 333–342. [Google Scholar] [CrossRef]
- Takai, N.; Yamaguchi, M.; Aragaki, T.; Eto, K.; Uchihashi, K.; Nishikawa, Y. Effect of Psychological Stress on the Salivary Cortisol and Amylase Levels in Healthy Young Adults. Arch. Oral Biol. 2004, 49, 963–968. [Google Scholar] [CrossRef]
- O’Donnell, K.; Kammerer, M.; O’Reilly, R.; Taylor, A.; Glover, V. Salivary α-Amylase Stability, Diurnal Profile and Lack of Response to the Cold Hand Test in Young Women. Stress 2009, 12, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Cespuglio, R.; Marinesco, S.; Baubet, V.; Bonnet, C.; El Kafi, B. Evidence for a Sleep-Promoting Influence of Stress. Adv. Neuroimmunol. 1995, 5, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Sohail, N. Stress and Academic Performance among Medical Students. J. Coll. Physicians Surg. Pak. 2013, 23, 67–71. [Google Scholar]
- Chang, P.P.; Ford, D.E.; Mead, L.A.; Cooper-Patrick, L.; Klag, M.J. Insomnia in Young Men and Subsequent Depression. The Johns Hopkins Precursors Study. Am. J. Epidemiol. 1997, 146, 105–114. [Google Scholar] [CrossRef]
- Morin, C.M.; Rodrigue, S.; Ivers, H. Role of Stress, Arousal, and Coping Skills in Primary Insomnia. Psychosom. Med. 2003, 65, 259–267. [Google Scholar] [CrossRef]
- Vineetha, R.; Pai, K.-M.; Vengal, M.; Gopalakrishna, K.; Narayanakurup, D.; Professor, A. Usefulness of Salivary Alpha Amylase as a Biomarker of Chronic Stress and Stress Related Oral Mucosal Changes—A Pilot Study. J. Clin. Exp. Dent. 2014, 6, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Yoshiike, T.; Utsumi, T.; Matsui, K.; Nagao, K.; Saitoh, K.; Otsuki, R.; Aritake-Okada, S.; Suzuki, M.; Kuriyama, K. Mortality Associated with Nonrestorative Short Sleep or Nonrestorative Long Time-in-Bed in Middle-Aged and Older Adults. Sci. Rep. 2022, 12, 189. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Kaneita, Y.; Tanaka, K.; Itani, O.; Matsumoto, Y.; Kuriyama, K. Longitudinal Assessment of Lifestyle Factors Associated with Nonrestorative Sleep in Japan. Sleep Med. 2023, 101, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, H.; Itoh, H.; Kiriyama, H.; Kamon, T.; Fujiu, K.; Morita, K.; Michihata, N.; Jo, T.; Takeda, N.; Morita, H.; et al. Restfulness from Sleep and Subsequent Cardiovascular Disease in the General Population. Sci. Rep. 2020, 10, 19674. [Google Scholar] [CrossRef] [PubMed]
- Nishida, K.; Sawada, D.; Kuwano, Y.; Tanaka, H.; Sugawara, T.; Aoki, Y.; Fujiwara, S.; Rokutan, K. Daily Administration of Paraprobiotic Lactobacillus gasseri CP2305 Ameliorates Chronic Stress-Associated Symptoms in Japanese Medical Students. J. Funct. Foods 2017, 36, 112–121. [Google Scholar] [CrossRef]
- Takada, M.; Nishida, K.; Gondo, Y.; Kikuchi-Hayakawa, H.; Ishikawa, H.; Suda, K.; Kawai, M.; Hoshi, R.; Kuwano, Y.; Miyazaki, K.; et al. Beneficial Effects of Lactobacillus casei Strain Shirota on Academic Stress-Induced Sleep Disturbance in Healthy Adults: A Double-Blind, Randomised, Placebo-Controlled Trial. Benef. Microbes 2017, 8, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Alenghat, T.; Artis, D. Epigenomic Regulation of Host-Microbiota Interactions. Trends Immunol. 2014, 35, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Gagliano, H.; Delgado-Morales, R.; Sanz-Garcia, A.; Armario, A. High Doses of the Histone Deacetylase Inhibitor Sodium Butyrate Trigger a Stress-like Response. Neuropharmacology 2014, 79, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, A.; Lehto, S.M.; Harty, S.; Dinan, T.G.; Cryan, J.F.; Burnet, P.W.J. Psychobiotics and the Manipulation of Bacteria–Gut–Brain Signals. Trends Neurosci. 2016, 39, 763–781. [Google Scholar] [CrossRef] [PubMed]
- Duranti, S.; Ruiz, L.; Lugli, G.A.; Tames, H.; Milani, C.; Mancabelli, L.; Mancino, W.; Longhi, G.; Carnevali, L.; Sgoifo, A.; et al. Bifidobacterium adolescentis as a Key Member of the Human Gut Microbiota in the Production of GABA. Sci. Rep. 2020, 10, 14112. [Google Scholar] [CrossRef]
- Guo, Y.; Xie, J.P.; Deng, K.; Li, X.; Yuan, Y.; Xuan, Q.; Xie, J.; He, X.M.; Wang, Q.; Li, J.J.; et al. Prophylactic Effects of Bifidobacterium adolescentis on Anxiety and Depression-like Phenotypes after Chronic Stress: A Role of the Gut Microbiota-Inflammation Axis. Front. Behav. Neurosci. 2019, 13, 126. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Lee, K.; Kim, D. The Preventive and Curative Effects of Lactobacillus reuteri NK33 and Bifidobacterium Adolescentis NK98 on Immobilization Stress-Induced Anxiety/Depression and Colitis in Mice. Nutrients 2019, 11, 819. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.M.; Kim, D.H. Bifidobacterium adolescentis IM38 Ameliorates High-Fat Diet–Induced Colitis in Mice by Inhibiting NF-ΚB Activation and Lipopolysaccharide Production by Gut Microbiota. Nutr. Res. 2017, 41, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Sawada, D.; Sugawara, T.; Ishida, Y.; Aihara, K.; Aoki, Y.; Takehara, I.; Takano, K.; Fujiwara, S. Effect of Continuous Ingestion of a Beverage Prepared with Lactobacillus gasseri CP2305 Inactivated by Heat Treatment on the Regulation of Intestinal Function. Food Res. Int. 2016, 79, 33–39. [Google Scholar] [CrossRef]
- Yoshikawa, K.; Aota, K.; Takata, Y.; Nakamura, T.; Hoshino, T.; Yamashita, S.I.; Takara, T. Efficacy of the Lactobacillus brevis SBC8803 (SBL88TM) Intake on the Quality of Sleep-a Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study. Jpn. Pharmacol. Ther. 2018, 46, 1723–1738. [Google Scholar]
- Shimamura, S.; Abe, F.; Ishibashi, N.; Miyakawa, H.; Yaeshima, T.; Araya, T.; Tomita, M. Relationship between Oxygen Sensitivity and Oxygen Metabolism of Bifidobacterium Species. J. Dairy Sci. 1992, 75, 3296–3306. [Google Scholar] [CrossRef]



| Items | Unit | Placebo | SBT2786 | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Number of Subjects | 65 | 61 | ||||||
| Sex | Male/Female | 30/35 | 32/29 | 0.593 | ||||
| Age | Years | 46.7 | ± | 7.3 | 46.1 | ± | 7.0 | 0.642 |
| Height | cm | 164.1 | ± | 7.1 | 166.2 | ± | 8.4 | 0.139 |
| Weight | kg | 61.1 | ± | 10.2 | 62.4 | ± | 11.6 | 0.516 |
| BMI | kg/cm2 | 22.6 | ± | 2.9 | 22.4 | ± | 2.8 | 0.730 |
| Systolic blood pressure | mmHg | 119.4 | ± | 13.8 | 118.7 | ± | 13.2 | 0.784 |
| Diastolic blood pressure | mmHg | 74.6 | ± | 9.9 | 74.6 | ± | 11.9 | 0.985 |
| Pulse rate | beat/min | 68.9 | ± | 9.5 | 71.7 | ± | 10.0 | 0.117 |
| PSQI-J global score | 7.6 | ± | 1.5 | 7.6 | ± | 1.6 | 0.936 | |
| Test sample consumption | % | 100.0 | ± | 0.0 | 100.0 | ± | 0.0 | - |
| Items | Unit | Placebo | SBT2786 | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Number of Subjects | 29 | 26 | ||||||
| Sex | Male/Female | 12/17 | 12/14 | 0.789 | ||||
| Age | Years | 48.4 | ± | 6.6 | 47.7 | ± | 6.9 | 0.708 |
| Height | cm | 164.3 | ± | 6.5 | 165.8 | ± | 8.2 | 0.465 |
| Weight | kg | 59.8 | ± | 10.1 | 62.7 | ± | 10.7 | 0.295 |
| BMI | kg/cm2 | 22.1 | ± | 3.0 | 22.7 | ± | 2.6 | 0.400 |
| Systolic blood pressure | mmHg | 119.1 | ± | 13.7 | 116.7 | ± | 11.3 | 0.482 |
| Diastolic blood pressure | mmHg | 76.4 | ± | 7.8 | 74.5 | ± | 11.1 | 0.459 |
| Pulse rate | beat/min | 71.3 | ± | 10.7 | 70.9 | ± | 10.3 | 0.872 |
| PSQI-J global score | 7.7 | ± | 1.4 | 7.6 | ± | 1.9 | 0.807 | |
| Test sample consumption | % | 100.0 | ± | 0.0 | 100.0 | ± | 0.0 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murakami, H.; Ko, T.; Ouchi, H.; Namba, T.; Ebihara, S.; Kobayashi, S. Bifidobacterium adolescentis SBT2786 Improves Sleep Quality in Japanese Adults with Relatively High Levels of Stress: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients 2024, 16, 1702. https://doi.org/10.3390/nu16111702
Murakami H, Ko T, Ouchi H, Namba T, Ebihara S, Kobayashi S. Bifidobacterium adolescentis SBT2786 Improves Sleep Quality in Japanese Adults with Relatively High Levels of Stress: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients. 2024; 16(11):1702. https://doi.org/10.3390/nu16111702
Chicago/Turabian StyleMurakami, Hiroki, Taro Ko, Haruka Ouchi, Toshiharu Namba, Shukuko Ebihara, and Shunjiro Kobayashi. 2024. "Bifidobacterium adolescentis SBT2786 Improves Sleep Quality in Japanese Adults with Relatively High Levels of Stress: A Randomized, Double-Blind, Placebo-Controlled Study" Nutrients 16, no. 11: 1702. https://doi.org/10.3390/nu16111702
APA StyleMurakami, H., Ko, T., Ouchi, H., Namba, T., Ebihara, S., & Kobayashi, S. (2024). Bifidobacterium adolescentis SBT2786 Improves Sleep Quality in Japanese Adults with Relatively High Levels of Stress: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients, 16(11), 1702. https://doi.org/10.3390/nu16111702







