Abstract
Renal cell carcinoma (RCC) is a common cancer of the urinary system. The potential therapeutic effects of certain natural products against renal cell carcinoma have been reported both in vivo and in vitro, but no reviews have been published classifying and summarizing the mechanisms of action of various natural products. In this study, we used PubMed and Google Scholar to collect and screen the recent literature on natural products with anti-renal-cancer effects. The main mechanisms of action of these products include the induction of apoptosis, inhibition of angiogenesis, inhibition of metastasis and reduction of drug resistance. In total, we examined more than 30 natural products, which include kahweol acetate, honokiol, englerin A and epigallocatechin-3-gallate, among others, have demonstrated a variety of anti-renal-cancer effects. In conclusion, natural products may have a wider application in kidney cancer than previously believed and are potential candidates for treatment in RCC.
1. Introduction
Renal cell carcinoma (RCC) is the most common malignancy in kidney, accounting for more than 80% of cases. RCC causes around 140,000 deaths per year worldwide, with an average incidence of 3–4% in Europe and the United States, regardless of gender [1,2]. The incidence in China is slightly lower than that in Europe and the United States, at ~1.5% in 2015, ranking 14th among all cancers [3]. More than 70% of RCC cases are diagnosed incidentally at check-ups due to a lack of heralding symptoms. The remaining 30% of cases present primarily with advanced disease or metastasis, which may show manifestations of back pain, hematuria or abdominal bulking—a triad that concurrently occurs in less than 10% of cases [4].
RCC is generally histologically classified into clear-cell type (70~90%), papillary type (10~15%) and chromophobe cell type (3~5%) [5]. The different histological subtypes are indicative of disparity in prognosis, metastatic tendency and recurrent probability [6]. Surgical resection, radical or partial, remains the mainstay of treatment for localized disease, and is curative in certain scenarios [7,8,9]. For disease at the advanced or metastatic stage, combination targeted and immunotherapy represent the frontline strategy. The identification of driver genetic events is important. Loss of 3p is the hallmark of clear-cell RCC (ccRCC). To date, four gene deletions on 3p are commonly accepted as driver events, that is, PBRM1, BAP1, SETD2 and VHL. The VHL deletion is the most important among these, as it leads to the accumulation of downstream HIF proteins, which enter the nucleus and bind to the hypoxia response element as a stimulator, regulating the transcription and expression of the downstream apoptosis-related protein family, as well as activate VEGF signaling and eventually angiogenesis. Furthermore, promiscuous HIF signaling (HIF1α and HIF2α) has been demonstrated to lead to extensive crosstalk with canonical pro-tumorigenic mTOR and PIK3/Akt pathways [10,11,12,13]. Tyrosine kinase inhibitors (TKIs) and mTOR inhibitors such as sunitinib, sorafenib, cabozantinib and everolimus have been developed on the basis of these driver molecular features in ccRCC. Immune checkpoint inhibitors (ICIs) featuring PD-1/PD-L1 and CTLA-4 antibodies such as nivolumab, pembrolizumab and avelumab have also been game-changing in the treatment of metastatic RCC [14,15,16]. In ccRCC, combinations of TKIs and ICIs stand at the front line of systemic therapy [17].
Notwithstanding, ~30% of metastatic cases do not respond to cutting-edge treatment, and most are heavily treated before being identified as non-responders, entailing various adverse events (AEs). Novel treatments with minimal AEs are thus urgently needed, and natural products have great potential to fill this gap. To date, numerous natural products derived from plants and animals have been reported to possess antitumor activity. Several have even been approved in clinical practice, and achieved better effects by being administered in combination with or even partially replacing traditional cytotoxic chemotherapeutic and targeted agents [18]. Natural products have shown promising effects in RCC in both basic and translational studies with regard to apoptosis induction, autophagy initiation, anti-angiogenesis, tumor metabolism inhibition and motility inhibition through various pathways [19,20,21]. For instance, kahweol acetate extracted from coffee bean was demonstrated to inhibit the phosphorylation of PIK3/Akt and Ras/MEK/ERK to directly exert anti-tumor, as well as a synergistic effect with VEGF receptor inhibitor in inducing apoptosis through downregulating the VEGF recepotor-2 in ccRCC [22]. The compound 6-gingerol extracted from ginger has been shown to inhibit the phosphorylation of cell-cycle-dependent kinases, and to induce G1 phase blockage through GSK3/cyclin D1 signaling [23].
In addition to the above mechanisms, natural products mediate a variety of cellular processes, including DNA methylation and the modification of non-coding RNAs and histones in RCC [24,25,26]. Here, we present a comprehensive review of reports regarding the use of natural products in RCC.
2. Methods
We searched the relevant literature published in recent years. The search was conducted on PubMed, Google Scholar and Web of Science, following the syntax “natural products and renal cell carcinoma”. We reserved articles published in journals with average impact factors >3.0 over the last five years and which used well-defined compounds or extracts for in vivo or in vitro assays. We then eliminated duplicate and non-English papers published between January 2015 and March 2022. The remaining articles were downloaded, and original texts were collated.
3. Results and Discussion
In line with the anti-cancer pharmacological effects and the chemical properties of natural products, natural products with theoretical potential for treating RCC can be broadly categorized as follows.
3.1. Apoptosis Induction
The elimination of cancer cells by inducing apoptosis has been a cornerstone of cancer therapy for more than three decades, and this process of promoting programmed cell death is usually mediated by several signaling pathways triggered by multiple factors (cellular stress, DNA damage, immune surveillance, etc.) [27]. Dysregulation of apoptotic machinery is also a “prelude” to malignant transformation, tumor metastasis and resistance to anti-cancer drugs [28]. Therefore, natural products that target the apoptosis process in common RCC cell lines such as ACHN, 786-O, A-498 and Caki-1/2 have a potential anticancer therapeutic effect.
We reviewed the apoptosis-inducing effect of 19 compounds derived from natural products or their extracts, as listed in Table 1 and Table 2, respectively. Tomoyuki et al. reported that kahweol and cafestol acetate, two extracts from coffee bean, could induce apoptosis and inhibit proliferation and migration in Caki and ACHN cells. Of note, combined treatment with both extracts demonstrated a stronger synergistic effect at low concentration (30 μM). In addition to downregulating apoptosis-related proteins of the Bcl family and inhibiting EMT, kahweol and cafestol acetate also downregulated the expression of chemokine receptors (CCRs) 2, 5 and 6, and inhibited PIK3/Akt signaling, which plays a crucial role in cell proliferation and migration [22].

Table 1.
Single compounds from natural products showing cancer-intrinsic inhibition (major in apoptosis induction and/or proliferation inhibition) in renal cell carcinoma.

Table 2.
Extracts from natural products showing cancer-intrinsic inhibition (major in apoptosis induction and/or proliferation inhibition) in renal cell carcinoma.
Ma et al. conducted in vitro experiments using sinularin extracted from soft coral in 786-O and ACHN cells. Gradient doses at 5, 10, 20, 40, 60 and 80 μM sinularin were applied in tumor cells, and cell viability was measured at 24, 48, 72 and 96 h. An overall decrease in cell activity was observed. Western blotting revealed the downregulation of anti-apoptotic proteins Bcl-2 and Bcl-xl, and the upregulation of pro-apoptotic protein Bax in a dose-dependent manner. Ma et al. also noted decreased PIK3/Akt/mTOR signaling, further supporting an apoptosis-inducing effect of sinularin [29]. Meng et al. reported the significant cell arrest in G2/M phase and apoptosis in the presence of quercetin in ccRCC Caki-2 cells. The pro-apoptotic effect was enhanced in combination with Snail knockdown. They also noted a decreased activity in the Akt/mTOR pathway following quercetin treatment [31]. In a study by Alexander et al., D-fraction, a bioactive proteoglucan extracted from Grifola frondosa exhibited antioxidant and anticancer activities by regulating the expression of apoptosis-related proteins and inducing the oxidative stress accompanied by a G1 cell cycle arrest, which were enhanced by combined treatment with vitamin C. A gradient of 0–1000 μg/mL of D-fraction and 0–700 μM of vitamin C was tested in the treatment of ACHN cells, and cell viability was decreased by ~40% and ~65% at 700 and 1000 μg/mL D-fraction, respectively. In contrast, 300 μg/mL of D-fraction combined with 200 μM of vitamin C induced >90% cell death with alterations in a series of apoptosis regulators [30].
Liu et al. reported that cyclovirobuxine, a triterpenoid extracted from small-leaf boxwood, showed biological activity in inducing apoptosis and inhibiting proliferation and migration in 786-O and ACHN cells. WB assay demonstrated a dose-dependent effect in downregulating the Bcl-2, while it upregulated the expression of Bax. Furthermore, exposure to cyclovirobuxine significantly decreased levels of p-AKT, p-STAT3, p-JNK, p-P38 and p-ERK. Mechanistic analyses suggested that cyclovirobuxine inhibits RCC cells by blocking the insulin-like growth factor binding protein 3(IGFBP3)-Akt/STAT3/MAPK-Snail pathway [32]. Ratnayake et al. extracted two unique bioactive sesquiterpenes from Tanzanian Phyllanthus engleri, namely englerin A and B [48]. Williams et al. found that the apoptosis of A-498 cells treated with englerin A at 100 nM for 46 h was much higher than that of the control group, similarly to vincristine. Meanwhile, Williams et al. presumed that englerin A plays a role through caspase-independent proteins such as cathepsins and calpains, as no alterations in caspase were noted. Of note, englerin A also induced G2/M phase arrest and led to downregulation of the PIK3/Akt pathway through increased inhibitory phosphorylation of insulin receptor substrate 1 (IRS1) [35]. In a study by Chen et al. [36], epigallocatechin-3-gallate (EGCG) significantly decreased the activity of matrix metalloproteinases (MMPs) 2 and 9. Additionally, the pluripotent EGCG can also inhibit the migration of cancer cells through c-Jun N-terminal kinase (JNK) signaling and focal adhesion kinase/extracellular regulated kinase/nuclear factor-κB. Meanwhile, EGCG exerted time- and dose-dependent anti-proliferative and pro-apoptotic effects in both 786-O and ACHN cells, the specific mechanism remains yet to be illustrated [49,50]. Kim et al. performed a similar study using resveratrol extracted from grape in Caki-1 and 786-O cells, demonstrating multiple anti-cancer effects, such as downregulating the expression of various oncogenic genes, causing the inhibition of proliferation, increasing accumulation of cells in S phase, suppressing invasive and colony formation activity, and significantly potentiating the apoptotic effects of sorafenib in RCC cells by inhibiting the activation of JAK1/2, c-Src, further suppressing the STAT3 and STAT5, as well as inducing the expression of protein tyrosine phosphatases PTPε and SHP-2 [39]. Curcumin is a well-studied product in a variety of cancers. Gong et al. reported apoptosis induction and autophagy activation mediated by Akt/mTOR signaling in ACHN cells in vitro [40].
Apoptosis induction has been a main effect shown in most studies of natural products in RCC. Of note, alterations in the PIK3/Akt/mTOR pathway have also been noted in most studies. Those findings correspond to the canonical strategy of targeting tumors by endogenous, exogenous and anti-apoptotic pathways. The endogenous apoptotic pathway is mainly controlled by Bcl-2 family proteins, which release cytochrome c into the cytoplasm and lead to the formation of apoptotic bodies and the activation of caspase-3. The exogenous pathway is mainly activated by apoptosis receptor proteins in the cell membrane, such as Fas, TNFR1/2 and its downstream caspase-8/10. The major anti-apoptotic pathway has been attributed to several signaling molecules, such as AKT, ERK, RAS, RAF, MEK and mTOR kinases [27]. However, most current studies on compounds derived from natural products focused more on validating or re-revealing known pathways in vitro, and less on new mechanisms of apoptosis in vivo or dose exploration.
In addition to single compounds, extracts with multiple organic solvents from natural products have also been reported to mediate apoptosis in RCC. Extracts from the genus Physalis were found to exert selective cytotoxicity on RCC cells, and those components contained 2,3-enone and 5b,6b-epoxide fractions on their A and B rings [42]. Predes et al. reported the hydroethanolic extract from Arctium lappa root showed strong anti-oxidation effect and inhibited the proliferation of RCC 786-O cells [43]. Likewise, extracts from the Brazilian shrub Pothomorphe umbellate were also toxic to 786-O cells [44]. Liu et al. reported an apoptotic effect of green-synthesized gold nanoparticles from Curcuma wenyujin extracts against human renal cell carcinoma A-498 cells, which were more sensitive than SW-156 cells, with increased caspase-3 and -9 and decreased Bcl-2 [46]. Verma et al. reported that the aqueous extract of the anticancer drug CRUEL herbomineral formulation capsules exerted anti-proliferative effects in RCC cell lines [47].
Unlike single compounds, extracts present hurdles such as the separation and purification of bioactive components, which requires the development of common chemical screening assays with chromatographic or non-chromatographic techniques [51]. Nevertheless, most studies on extracts correspond to compounds promoting apoptosis via Bcl-associated apoptotic signaling.
3.2. Anti-Angiogenesis
Angiogenesis is a hallmark of ccRCC. Genetic and genomic alterations hijack hypoxia signaling for neovascularization that fuels cancer with a rapidly available energy supply and facilitates the route to metastasis [52,53]. Aside from upstream factors that are difficult to target, major druggable pro-angiogenic factors include vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), basic fibroblast growth factor (bFGF) and their ligands, or the whole pathways therein, among others [54,55]. Therefore, natural products that inhibit these factors are theoretically beneficial for ccRCC patients.
Most studies of natural products focus on cancer-intrinsic activity, and only a few discuss angiogenesis, which is a hallmark of ccRCC. Sasamura et al. [56] reported that genistein, an isoflavone derived from soybean, could inhibit angiogenesis in RCC by downregulating the expression of VEGF and bFGF. Given the shared signaling in angiogenesis, studies in other cancer types may very well be extrapolated to ccRCC. Here, we review studies of anti-angiogenic natural products. In their study of breast cancer and lymphoma, Wang et al. [57] reported that tumors treated with deguelin, a drug derived from Derris trifoliata Lour. or Mundulea sericea Legu., showed a 42% decrease of micro-vessel density. Deguelin also demonstrated inhibitory activity in sprouting and chorioallantoic membrane (CAM) assays. Functional analyses revealed that deguelin inhibited the synthesis of HIF1α, leading to a decrease of downstream VEGF and BFGF signaling.
El-Khashab et al. [58] showed that the oral administration of Ganoderma lucidum extracts in a mouse model of Ehrlich’s solid tumor induced decreased VEGF levels. Cho et al. found that Kochia scoparia seed extracts (KSEs) could inhibit tumor growth and angiogenesis by modulating VEGFR2 and the PI3K/AKT/mTOR pathway. They treated human vascular endothelial cells (HUVECs) with 10–20μg/mL KSEs and 20–50 ng/mL VEGF, and showed that treatment with KSEs significantly inhibited VEGF-induced migration, invasion and capillary formation in rat aortic rings. In addition, KSEs downregulated the phosphorylation of PI3K/AKT/mTOR and VEGFR2 in HUVECs [59]. Methanol extracts of Syzygium campanulatum (SC) were shown to significantly inhibit the growth of microvessels in rat aortic rings with minimal cytotoxicity to normal cells. SC extracts inhibited endothelial cell migration and suppressed VEGF expression, while in vivo anti-angiogenic studies demonstrated that SC extracts inhibited neovascularization in a CAM assay [60]. Zhu et al. showed that 5-formylhonokiol, which is derived from honokiol, could inhibit the proliferation of HUVECs in a time-dependent manner. Moreover, 5-formylhonokiol exerted a dose-dependent inhibition in a zebrafish angiogenesis model. Functional analyses indicated that 5-formylhonokiol downregulated the expression of ERK and its phosphorylation without affecting Akt signaling [61]. Lu et al. reported that polyphenols extracted from Cinnamomum zeylanicum could block signal transmission from VEGF to its receptor VEGFR2, both in an in vitro Matrigel plug assay and in mouse aortic ring in vivo [62]. Likewise, penduliflaworosin extracted from Croton crassifolius was shown to exert an anti-angiogenic effect by forming hydrogen bonds within the ATP-binding region of the VEGFR2 kinase unit to interfere with the VEGF/VEGFR2 pathway, while the cytotoxicity assay showed that penduliflaworosin possessed little toxicity toward both cancer and normal cells [63]. We can conclude from these studies that certain natural products could exert an anti-angiogenic effect through targeting HIF-1 and its induced proteins downstream in ccRCC. Proof-of-concept studies are still needed.
3.3. Inhibition of Motility
Migratory ability is another hallmark of cancer metastasis that is independent of growth and apoptosis [53,64]. Amongst all cellular processes that mediate migration, epithelial–mesenchymal transition (EMT) is a hotspot of both basic and translational studies. The myriad kinases participating in EMT render this process druggable [65], and natural products are theoretically effective through their interaction with one or more of these kinases.
We identified 15 active natural products that can inhibit the migration of RCC (Table 3). Li et al. reported that honokiol extracted from Magnolia spp. bark inhibited the migration and invasion of A-498 ccRCC cell line via miR-141/ZEB2-mediated EMT signaling and cancer stem cell properties [66]. Amygdalin extracted from Semen armeniacae Amarum inhibited cell adhesion, chemotactic activity and the invasion of ccRCC cells via the downregulation of integrin α5 and integrin α6, as well as suppression of integrin β1 to traffic to the plasma membrane, which has been shown to increase the metastatic potential of RCC cells [67]. Esculetin, extracted from Cortex fraxini, was shown to inhibit cell proliferation and block cell cycle progression, and to inhibit the migration of ccRCC cells by suppressing IGF-1/EGFR/PI3K/Akt pathway, downregulating the N-cadherin and vimentin, as well as upregulating the E-cadherin due to reversal of EMT activation [68]. Hsieh et al. showed that fisetin, a natural flavonoid, inhibited invasion and migration in four different ccRCC cell lines in a dose-dependent manner through the downregulation of cyclin D1/E, cathepsin B, cathepsin S and cathepsin V accompanied with the increased phosphorylation of ERK [69]. Antcin-H, a bioactive component extracted from Antrodia Cinnamon, was shown to inhibit the expression of MMP-2, -3, -7 and -13, and inhibited migration in 786-O cells [70]. Thymoquinone was also shown to inhibit the metastasis of 786-O renal cell carcinoma cells through the downregulation of MMP-2 and the suppression of PI3K/Src signaling [71].

Table 3.
Natural products showing cancer-intrinsic inhibition (major in motility inhibition) in renal cell carcinoma.
These studies support the assertion that certain natural products are capable of inhibiting the motility of RCC cells. The implications of these findings could alter the current paradigm of medicinal treatment of metastatic RCC by adding natural products to the current TKIs and/or immunotherapy. Studies in this field are quite appealing, and investigations have been carried out evaluating the use of natural products as sensitizers.
3.4. Drug Sensitizer
TKIs remain the mainstay of treatment for metastatic ccRCC, especially in the modern era of combined therapy with checkpoint inhibitors. However, TKIs themselves inevitably induce resistance via multiple signaling shunts [76]. The addition of any drug in these heavily treated patients is challenging, as adverse events may overtake any potential advantages or synergistic effects. Natural products theoretically fit this niche. We reviewed six natural products that have demonstrated therapeutic effects in combination with TKIs for RCC (Table 4).

Table 4.
Natural products showing drug sensitizing effect in renal cell carcinoma.
Korean red ginseng extracts have been shown to improve chemosensitivity to sorafenib in RCC by inducing p53 phosphorylation [80]. Xu et al. reported that Physachenolide C as sensitizers of renal carcinoma cells to tumor necrosis factor-alpha-related apoptosis-inducing ligand (TRAIL)-mediated apoptosis [78]. Chen et al. injected Lycium barbarum polysaccharides into a Renca mouse model of RCC and found synergy with interferon-α2b. The combination also reduced myeloid-derived suppressor cells (MDSCs), blocked the G0/G1 phase transition, alleviated immunosuppression and restored innate immunity and acquired immunity [79]. In addition, kahweol acetate has also been reported to increase the sensitivity of RCC cells to sorafenib by reducing the expression of Mcl-1 and c-FLIP, which mediates resistance to TRAIL-dependent apoptosis [22]. Some other natural products may have an effect via the microenvironment, and only show synergy in vivo. Min et al. reported that osthole, extracted from Cnidium monnieri, showed no effect on apoptosis in Caki cells when used alone in vitro, whereas it synergistically enhanced apoptosis in combination with TRAIL. Mechanistic analyses showed that osthol significantly induces the downregulation of c-FLIP [77].
There is still a dearth of studies on synergy, and we speculate that this could be a research hotspot for RCC treatment given the wide prevalence of traditional and complementary medicine practiced worldwide, especially in East Asia.
Several natural products listed in the current review have already been or are in the progress of being applied as food supplements (Figure 1). For example, amygdalin was detected in a variety of food such as apples, apricots and almonds and its amounts are higher in seeds from Rosaceae species [81]. Antcin B, H and K (antcins) are bioactive compounds isolated from Antrodia cinnamomea, a medical mushroom widely used in Asian countries [82]. Of note, Curcuma longa extract and curcumin supplements have shown comparable relieving effects on osteoarthritis to non-steroidal anti-inflammatory drugs (NSAIDs) with less adverse effects [83]. Likewise, EGCG, another widely accepted food supplement has shown various effects in combating metabolic syndrome and cancer [84]. Furthermore, dietary sulforaphane from broccoli was studied in a plethora of conditions ranging from cancer to psychiatric disorder [85,86]. Honokiol, a major component of magnolia bark which is widely used in food supplements worldwide can now be quantified and purified with modified technology [87]. Advances in technique may also contribute to purification of isothiocyanates from Moringa oleifera Lam., a tropical plant widely used in traditional medicines and as a food supplement [88]. Though not reported in RCC, flavonols (kaempferol, fisetin and myricetin) play a role in reducing risks for advanced prostate cancer but show no effect on bladder cancer susceptibility [89]. Interestingly, fisetin, as well as chelerythrine are also reported to be important supplements for poultry to avoid heat stress-associated morbidities and spotty liver disease, respectively [90,91]. Lastly, animal studies on Lycium barbarum polysaccharides, osthole and thymoquinone have also shown satisfactory tolerability in vivo and those products hold promise to the manufacture of relevant supplements [92,93,94].
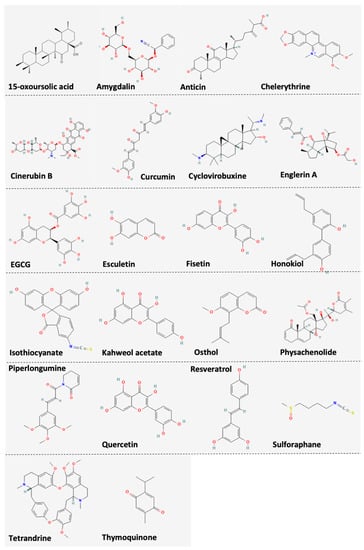
Figure 1.
Chemical structures of compounds listed in the current review.
4. Limitations and Conclusions
Our review has limitations. We did not include reports on compound decoctions or ongoing clinical trials. On evaluating the relevant literature, we believe that the studies are still immature or lack specificity, which informed our decision to exclude those categories. In all, we reviewed the antitumor effects of the extracts or derivatives of more than 30 natural products in RCC, including mechanisms such as apoptosis induction, motility inhibition, anti-angiogenesis and drug sensitization. All studies support the notion that natural products exert anti-cancer activity with minimal adverse events, and these series of studies reveal that natural products bear very wide application prospects in future. Large-scale and solid clinical studies are thus eagerly awaited.
Author Contributions
C.F. and L.G. carried out the literature search. J.W. and C.F. participated in the study design. C.F. reviewed evidence. C.F. and Y.L. drafted the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was sponsored in part by Beijing Advanced Innovation Center for Food Nutrition and Human Health, Beijing Technology and Business University (BTBU) and the National Natural Science Foundation of China (Grant No. 81874123).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Escudier, B.; Porta, C.; Schmidinger, M.; Rioux-Leclercq, N.; Bex, A.; Khoo, V.; Grunwald, V.; Gillessen, S.; Horwich, A.; ESMO Guidelines Committee. Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-updagger. Ann. Oncol. 2019, 30, 706–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barata, P.C.; Rini, B.I. Treatment of renal cell carcinoma: Current status and future directions. CA Cancer J. Clin. 2017, 67, 507–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.; Zheng, R.; Baade, P.D.; Zhang, S.; Zeng, H.; Bray, F.; Jemal, A.; Yu, X.Q.; He, J. Cancer statistics in China, 2015. CA Cancer J. Clin. 2016, 66, 115–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capitanio, U.; Montorsi, F. Renal cancer. Lancet 2016, 387, 894–906. [Google Scholar] [CrossRef]
- Warren, A.Y.; Harrison, D. WHO/ISUP classification, grading and pathological staging of renal cell carcinoma: Standards and controversies. World J. Urol. 2018, 36, 1913–1926. [Google Scholar] [CrossRef] [Green Version]
- Dudani, S.; de Velasco, G.; Wells, J.C.; Gan, C.L.; Donskov, F.; Porta, C.; Fraccon, A.; Pasini, F.; Lee, J.L.; Hansen, A.; et al. Evaluation of Clear Cell, Papillary, and Chromophobe Renal Cell Carcinoma Metastasis Sites and Association With Survival. JAMA Netw. Open 2021, 4, e2021869. [Google Scholar] [CrossRef]
- Frank, I.; Blute, M.L.; Cheville, J.C.; Lohse, C.M.; Weaver, A.L.; Zincke, H. An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: The SSIGN score. J. Urol. 2002, 168, 2395–2400. [Google Scholar] [CrossRef]
- Leibovich, B.C.; Blute, M.L.; Cheville, J.C.; Lohse, C.M.; Frank, I.; Kwon, E.D.; Weaver, A.L.; Parker, A.S.; Zincke, H. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: A stratification tool for prospective clinical trials. Cancer 2003, 97, 1663–1671. [Google Scholar] [CrossRef]
- Patard, J.J.; Kim, H.L.; Lam, J.S.; Dorey, F.J.; Pantuck, A.J.; Zisman, A.; Ficarra, V.; Han, K.R.; Cindolo, L.; De La Taille, A.; et al. Use of the University of California Los Angeles integrated staging system to predict survival in renal cell carcinoma: An international multicenter study. J. Clin. Oncol. 2004, 22, 3316–3322. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Kaelin, W.G., Jr. Targeting the HIF2-VEGF axis in renal cell carcinoma. Nat. Med. 2020, 26, 1519–1530. [Google Scholar] [CrossRef]
- Brugarolas, J. Molecular genetics of clear-cell renal cell carcinoma. J. Clin. Oncol. 2014, 32, 1968–1976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iliopoulos, O. Molecular biology of renal cell cancer and the identification of therapeutic targets. J. Clin. Oncol. 2006, 24, 5593–5600. [Google Scholar] [CrossRef] [PubMed]
- D’Avella, C.; Abbosh, P.; Pal, S.K.; Geynisman, D.M. Mutations in renal cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 763–773. [Google Scholar] [CrossRef]
- Keenan, T.E.; Burke, K.P.; Van Allen, E.M. Genomic correlates of response to immune checkpoint blockade. Nat. Med. 2019, 25, 389–402. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Escudier, B.; McDermott, D.F.; George, S.; Hammers, H.J.; Srinivas, S.; Tykodi, S.S.; Sosman, J.A.; Procopio, G.; Plimack, E.R.; et al. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2015, 373, 1803–1813. [Google Scholar] [CrossRef] [PubMed]
- Tannir, N.; Hammers, H.; Amin, A. First-line vascular endothelial growth factor targeted therapy in renal cell carcinoma: Priming the tumor microenvironment for immunotherapy. Curr. Med. Res. Opin. 2018, 34, 825–831. [Google Scholar] [CrossRef]
- Bedke, J.; Albiges, L.; Capitanio, U.; Giles, R.H.; Hora, M.; Lam, T.B.; Ljungberg, B.; Marconi, L.; Klatte, T.; Volpe, A.; et al. The 2021 Updated European Association of Urology Guidelines on Renal Cell Carcinoma: Immune Checkpoint Inhibitor-based Combination Therapies for Treatment-naive Metastatic Clear-cell Renal Cell Carcinoma Are Standard of Care. Eur. Urol. 2021, 80, 393–397. [Google Scholar] [CrossRef]
- Atanasov, A.G.; Zotchev, S.B.; Dirsch, V.M.; International Natural Product Sciences, T.; Supuran, C.T. Natural products in drug discovery: Advances and opportunities. Nat. Rev. Drug Discov. 2021, 20, 200–216. [Google Scholar] [CrossRef]
- Olgen, S. Overview on Anticancer Drug Design and Development. Curr. Med. Chem. 2018, 25, 1704–1719. [Google Scholar] [CrossRef]
- Gao, L.; Wu, Z.X.; Assaraf, Y.G.; Chen, Z.S.; Wang, L. Overcoming anti-cancer drug resistance via restoration of tumor suppressor gene function. Drug Resist. Updat. 2021, 57, 100770. [Google Scholar] [CrossRef]
- Buyel, J.F. Plants as sources of natural and recombinant anti-cancer agents. Biotechnol. Adv. 2018, 36, 506–520. [Google Scholar] [CrossRef] [PubMed]
- Makino, T.; Izumi, K.; Hiratsuka, K.; Kano, H.; Shimada, T.; Nakano, T.; Kadomoto, S.; Naito, R.; Iwamoto, H.; Yaegashi, H.; et al. Anti-proliferative and anti-migratory properties of coffee diterpenes kahweol acetate and cafestol in human renal cancer cells. Sci. Rep. 2021, 11, 675. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Zhang, H.; Liu, T.; Yang, W.; Lv, W.; He, D.; Guo, P.; Li, L. 6-Gingerol induces cell-cycle G1-phase arrest through AKT-GSK 3beta-cyclin D1 pathway in renal-cell carcinoma. Cancer Chemother. Pharmacol. 2020, 85, 379–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, M.; Wang, Y.; Song, Y.; Bu, R.; Yin, B.; Fei, X.; Guo, Q.; Wu, B. Expression profiling and clinicopathological significance of DNA methyltransferase 1, 3A and 3B in sporadic human renal cell carcinoma. Int. J. Clin. Exp. Pathol. 2014, 7, 7597–7609. [Google Scholar]
- Jonasch, E.; Gao, J.; Rathmell, W.K. Renal cell carcinoma. BMJ 2014, 349, g4797. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y.; Wang, P.; Fu, X.; Lin, W. Circular RNAs in renal cell carcinoma: Implications for tumorigenesis, diagnosis, and therapy. Mol. Cancer 2020, 19, 149. [Google Scholar] [CrossRef]
- Carneiro, B.A.; El-Deiry, W.S. Targeting apoptosis in cancer therapy. Nat. Rev. Clin. Oncol. 2020, 17, 395–417. [Google Scholar] [CrossRef]
- Wong, R.S. Apoptosis in cancer: From pathogenesis to treatment. J. Exp. Clin. Cancer Res. 2011, 30, 87. [Google Scholar] [CrossRef] [Green Version]
- Ma, Q.; Meng, X.Y.; Wu, K.R.; Cao, J.Z.; Yu, R.; Yan, Z.J. Sinularin exerts anti-tumor effects against human renal cancer cells relies on the generation of ROS. J. Cancer 2019, 10, 5114–5123. [Google Scholar] [CrossRef]
- Alexander, B.; Fishman, A.I.; Eshghi, M.; Choudhury, M.; Konno, S. Induction of cell death in renal cell carcinoma with combination of D-fraction and vitamin C. Integr. Cancer Ther. 2013, 12, 442–448. [Google Scholar] [CrossRef]
- Meng, F.D.; Li, Y.; Tian, X.; Ma, P.; Sui, C.G.; Fu, L.Y.; Jiang, Y.H. Synergistic effects of snail and quercetin on renal cell carcinoma Caki-2 by altering AKT/mTOR/ERK1/2 signaling pathways. Int. J. Clin. Exp. Pathol. 2015, 8, 6157–6168. [Google Scholar] [PubMed]
- Liu, Y.; Lv, H.; Li, X.; Liu, J.; Chen, S.; Chen, Y.; Jin, Y.; An, R.; Yu, S.; Wang, Z. Cyclovirobuxine inhibits the progression of clear cell renal cell carcinoma by suppressing the IGFBP3-AKT/STAT3/MAPK-Snail signalling pathway. Int. J. Biol. Sci. 2021, 17, 3522–3537. [Google Scholar] [CrossRef] [PubMed]
- Son, J.Y.; Yoon, S.; Tae, I.H.; Park, Y.J.; De, U.; Jeon, Y.; Park, Y.J.; Rhyu, I.J.; Lee, B.M.; Chung, K.H.; et al. Novel therapeutic roles of MC-4 in combination with everolimus against advanced renal cell carcinoma by dual targeting of Akt/pyruvate kinase muscle isozyme M2 and mechanistic target of rapamycin complex 1 pathways. Cancer Med. 2018, 7, 5083–5095. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.J.; Crevelin, E.J.; Souza, D.T.; Lacerda-Junior, G.V.; de Oliveira, V.M.; Ruiz, A.; Rosa, L.H.; Moraes, L.A.B.; Melo, I.S. Actinobacteria from Antarctica as a source for anticancer discovery. Sci. Rep. 2020, 10, 13870. [Google Scholar] [CrossRef]
- Williams, R.T.; Yu, A.L.; Diccianni, M.B.; Theodorakis, E.A.; Batova, A. Renal cancer-selective Englerin A induces multiple mechanisms of cell death and autophagy. J. Exp. Clin. Cancer Res. 2013, 32, 57. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.J.; Yao, X.D.; Peng, B.O.; Xu, Y.F.; Wang, G.C.; Huang, J.; Liu, M.; Zheng, J.H. Epigallocatechin-3-gallate inhibits migration and invasion of human renal carcinoma cells by downregulating matrix metalloproteinase-2 and matrix metalloproteinase-9. Exp. Ther. Med. 2016, 11, 1243–1248. [Google Scholar] [CrossRef] [Green Version]
- Negrette-Guzman, M.; Huerta-Yepez, S.; Vega, M.I.; Leon-Contreras, J.C.; Hernandez-Pando, R.; Medina-Campos, O.N.; Rodriguez, E.; Tapia, E.; Pedraza-Chaverri, J. Sulforaphane induces differential modulation of mitochondrial biogenesis and dynamics in normal cells and tumor cells. Food Chem. Toxicol. 2017, 100, 90–102. [Google Scholar] [CrossRef]
- Ali, S.; Nisar, M.; Qaisar, M.; Khan, A.; Khan, A.A. Evaluation of the cytotoxic potential of a new pentacyclic triterpene from Rhododendron arboreum stem bark. Pharm. Biol. 2017, 55, 1927–1930. [Google Scholar] [CrossRef] [Green Version]
- Kim, C.; Baek, S.H.; Um, J.Y.; Shim, B.S.; Ahn, K.S. Resveratrol attenuates constitutive STAT3 and STAT5 activation through induction of PTPepsilon and SHP-2 tyrosine phosphatases and potentiates sorafenib-induced apoptosis in renal cell carcinoma. BMC Nephrol. 2016, 17, 19. [Google Scholar] [CrossRef] [Green Version]
- Gong, X.; Jiang, L.; Li, W.; Liang, Q.; Li, Z. Curcumin induces apoptosis and autophagy inhuman renal cell carcinoma cells via Akt/mTOR suppression. Bioengineered 2021, 12, 5017–5027. [Google Scholar] [CrossRef]
- He, H.; Zhuo, R.; Dai, J.; Wang, X.; Huang, X.; Wang, H.; Xu, D. Chelerythrine induces apoptosis via ROS-mediated endoplasmic reticulum stress and STAT3 pathways in human renal cell carcinoma. J. Cell. Mol. Med. 2020, 24, 50–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, Y.-M.; Wijeratne, E.M.K.; Brooks, A.D.; Tewary, P.; Xuan, L.-J.; Wang, W.-Q.; Sayers, T.J.; Gunatilaka, A.A.L. Cytotoxic and other withanolides from aeroponically grown Physalis philadelphica. Phytochemistry 2018, 152, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Predes, F.S.; Ruiz, A.L.; Carvalho, J.E.; Foglio, M.A.; Dolder, H. Antioxidative and in vitro antiproliferative activity of Arctium lappa root extracts. BMC Complement. Altern. Med. 2011, 11, 25. [Google Scholar] [CrossRef] [Green Version]
- Sacoman, J.L.; Monteiro, K.M.; Possenti, A.; Figueira, G.M.; Foglio, M.A.; Carvalho, J.E. Cytotoxicity and antitumoral activity of dichloromethane extract and its fractions from Pothomorphe umbellata. Braz. J. Med. Biol. Res. 2008, 41, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Cortelo, P.C.; Demarque, D.P.; Dusi, R.G.; Albernaz, L.C.; Braz-Filho, R.; Goncharova, E.I.; Bokesch, H.R.; Gustafson, K.R.; Beutler, J.A.; Espindola, L.S. A Molecular Networking Strategy: High-Throughput Screening and Chemical Analysis of Brazilian Cerrado Plant Extracts against Cancer Cells. Cells 2021, 10, 691. [Google Scholar] [CrossRef]
- Liu, R.; Pei, Q.; Shou, T.; Zhang, W.; Hu, J.; Li, W. Apoptotic effect of green synthesized gold nanoparticles from Curcuma wenyujin extract against human renal cell carcinoma A498 cells. Int. J. Nanomed. 2019, 14, 4091–4103. [Google Scholar] [CrossRef] [Green Version]
- Verma, S.P.; Sisoudiya, S.; Das, P. Aqueous Extract of Anticancer Drug CRUEL Herbomineral Formulation Capsules Exerts Anti-proliferative Effects in Renal Cell Carcinoma Cell Lines. Asian Pac. J. Cancer Prev. 2015, 16, 8419–8423. [Google Scholar] [CrossRef] [Green Version]
- Ratnayake, R.; Covell, D.; Ransom, T.T.; Gustafson, K.R.; Beutler, J.A. Englerin A, a selective inhibitor of renal cancer cell growth, from Phyllanthus engleri. Org. Lett. 2009, 11, 57–60. [Google Scholar] [CrossRef] [Green Version]
- Deng, Y.T.; Lin, J.K. EGCG inhibits the invasion of highly invasive CL1-5 lung cancer cells through suppressing MMP-2 expression via JNK signaling and induces G2/M arrest. J. Agric. Food Chem. 2011, 59, 13318–13327. [Google Scholar] [CrossRef]
- Sen, T.; Dutta, A.; Chatterjee, A. Epigallocatechin-3-gallate (EGCG) downregulates gelatinase-B (MMP-9) by involvement of FAK/ERK/NFkappaB and AP-1 in the human breast cancer cell line MDA-MB-231. Anticancer Drugs 2010, 21, 632–644. [Google Scholar] [CrossRef]
- Sasidharan, S.; Chen, Y.; Saravanan, D.; Sundram, K.M.; Yoga Latha, L. Extraction, isolation and characterization of bioactive compounds from plants’ extracts. Afr. J. Tradit Complement. Altern. Med. 2011, 8, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yehya, A.H.S.; Asif, M.; Petersen, S.H.; Subramaniam, A.V.; Kono, K.; Majid, A.; Oon, C.E. Angiogenesis: Managing the Culprits behind Tumorigenesis and Metastasis. Medicina 2018, 54, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qin, S.; Li, A.; Yi, M.; Yu, S.; Zhang, M.; Wu, K. Recent advances on anti-angiogenesis receptor tyrosine kinase inhibitors in cancer therapy. J. Hematol. Oncol. 2019, 12, 27. [Google Scholar] [CrossRef] [Green Version]
- Argentiero, A.; Solimando, A.G.; Krebs, M.; Leone, P.; Susca, N.; Brunetti, O.; Racanelli, V.; Vacca, A.; Silvestris, N. Anti-angiogenesis and Immunotherapy: Novel Paradigms to Envision Tailored Approaches in Renal Cell-Carcinoma. J. Clin. Med. 2020, 9, 1594. [Google Scholar] [CrossRef]
- Sasamura, H.; Takahashi, A.; Miyao, N.; Yanase, M.; Masumori, N.; Kitamura, H.; Itoh, N.; Tsukamoto, T. Inhibitory effect on expression of angiogenic factors by antiangiogenic agents in renal cell carcinoma. Br. J. Cancer 2002, 86, 768–773. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Ma, W.; Zheng, W. Deguelin, a novel anti-tumorigenic agent targeting apoptosis, cell cycle arrest and anti-angiogenesis for cancer chemoprevention. Mol. Clin. Oncol. 2013, 1, 215–219. [Google Scholar] [CrossRef] [Green Version]
- El-Khashab, I.H. Antiangiogenic and Proapoptotic Activities of Atorvastatin and Ganoderma lucidum in Tumor Mouse Model via VEGF and Caspase-3 Pathways. Asian Pac. J. Cancer Prev. 2021, 22, 1095–1104. [Google Scholar] [CrossRef]
- Cho, H.D.; Kim, J.H.; Park, J.K.; Hong, S.M.; Kim, D.H.; Seo, K.I. Kochia scoparia seed extract suppresses VEGF-induced angiogenesis via modulating VEGF receptor 2 and PI3K/AKT/mTOR pathways. Pharm Biol 2019, 57, 684–693. [Google Scholar] [CrossRef] [Green Version]
- Aisha, A.F.; Ismail, Z.; Abu-Salah, K.M.; Siddiqui, J.M.; Ghafar, G.; Abdul Majid, A.M. Syzygium campanulatum korth methanolic extract inhibits angiogenesis and tumor growth in nude mice. BMC Complement. Altern. Med. 2013, 13, 168. [Google Scholar] [CrossRef] [Green Version]
- Zhu, W.; Fu, A.; Hu, J.; Wang, T.; Luo, Y.; Peng, M.; Ma, Y.; Wei, Y.; Chen, L. 5-Formylhonokiol exerts anti-angiogenesis activity via inactivating the ERK signaling pathway. Exp. Mol. Med. 2011, 43, 146–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, J.; Zhang, K.; Nam, S.; Anderson, R.A.; Jove, R.; Wen, W. Novel angiogenesis inhibitory activity in cinnamon extract blocks VEGFR2 kinase and downstream signaling. Carcinogenesis 2010, 31, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Zhang, Y.; Wang, G.; Li, Y.; Huang, W. Penduliflaworosin, a Diterpenoid from Croton crassifolius, Exerts Anti-Angiogenic Effect via VEGF Receptor-2 Signaling Pathway. Molecules 2017, 22, 126. [Google Scholar] [CrossRef] [Green Version]
- Moserle, L.; Casanovas, O. Anti-angiogenesis and metastasis: A tumour and stromal cell alliance. J. Intern. Med. 2013, 273, 128–137. [Google Scholar] [CrossRef]
- Winer, A.; Adams, S.; Mignatti, P. Matrix Metalloproteinase Inhibitors in Cancer Therapy: Turning Past Failures Into Future Successes. Mol. Cancer Ther. 2018, 17, 1147–1155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, W.; Wang, Q.; Su, Q.; Ma, D.; An, C.; Ma, L.; Liang, H. Honokiol suppresses renal cancer cells’ metastasis via dual-blocking epithelial-mesenchymal transition and cancer stem cell properties through modulating miR-141/ZEB2 signaling. Mol. Cells 2014, 37, 383–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Juengel, E.; Afschar, M.; Makarevic, J.; Rutz, J.; Tsaur, I.; Mani, J.; Nelson, K.; Haferkamp, A.; Blaheta, R.A. Amygdalin blocks the in vitro adhesion and invasion of renal cell carcinoma cells by an integrin-dependent mechanism. Int. J. Mol. Med. 2016, 37, 843–850. [Google Scholar] [CrossRef]
- Duan, J.; Shi, J.; Ma, X.; Xuan, Y.; Li, P.; Wang, H.; Fan, Y.; Gong, H.; Wang, L.; Pang, Y.; et al. Esculetin inhibits proliferation, migration, and invasion of clear cell renal cell carcinoma cells. Biomed. Pharmacother. 2020, 125, 110031. [Google Scholar] [CrossRef]
- Hsieh, M.H.; Tsai, J.P.; Yang, S.F.; Chiou, H.L.; Lin, C.L.; Hsieh, Y.H.; Chang, H.R. Fisetin Suppresses the Proliferation and Metastasis of Renal Cell Carcinoma through Upregulation of MEK/ERK-Targeting CTSS and ADAM9. Cells 2019, 8, 948. [Google Scholar] [CrossRef] [Green Version]
- Hung, T.W.; Chen, P.N.; Wu, H.C.; Wu, S.W.; Tsai, P.Y.; Hsieh, Y.S.; Chang, H.R. Kaempferol Inhibits the Invasion and Migration of Renal Cancer Cells through the Downregulation of AKT and FAK Pathways. Int. J. Med. Sci. 2017, 14, 984–993. [Google Scholar] [CrossRef] [Green Version]
- Liou, Y.F.; Hsieh, Y.S.; Hung, T.W.; Chen, P.N.; Chang, Y.Z.; Kao, S.H.; Lin, S.W.; Chang, H.R. Thymoquinone inhibits metastasis of renal cell carcinoma cell 786-O-SI3 associating with downregulation of MMP-2 and u-PA and suppression of PI3K/Src signaling. Int. J. Med. Sci. 2019, 16, 686–695. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Golovine, K.; Makhov, P.; Naito, S.; Raiyani, H.; Tomaszewski, J.; Mehrazin, R.; Tulin, A.; Kutikov, A.; Uzzo, R.G.; Kolenko, V.M. Piperlongumine and its analogs down-regulate expression of c-Met in renal cell carcinoma. Cancer Biol. Ther. 2015, 16, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Chiu, K.Y.; Chen, T.H.; Wen, C.L.; Lai, J.M.; Cheng, C.C.; Liu, H.C.; Hsu, S.L.; Tzeng, Y.M. Antcin-H Isolated from Antrodia cinnamomea Inhibits Renal Cancer Cell Invasion Partly through Inactivation of FAK-ERK-C/EBP-beta/c-Fos-MMP-7 Pathways. Evid.-Based Complement. Alternat. Med. 2017, 2017, 5052870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Liu, W.; Wang, K.; Fan, Y.; Chen, J.; Ma, J.; Wang, X.; He, D.; Zeng, J.; Li, L. Tetrandrine inhibits migration and invasion of human renal cell carcinoma by regulating Akt/NF-kappaB/MMP-9 signaling. PLoS ONE 2017, 12, e0173725. [Google Scholar] [CrossRef]
- Xie, J.; Qian, Y.Y.; Yang, Y.; Peng, L.J.; Mao, J.Y.; Yang, M.R.; Tian, Y.; Sheng, J. Isothiocyanate From Moringa oleifera Seeds Inhibits the Growth and Migration of Renal Cancer Cells by Regulating the PTP1B-dependent Src/Ras/Raf/ERK Signaling Pathway. Front. Cell Dev. Biol. 2021, 9, 790618. [Google Scholar] [CrossRef]
- Vasan, N.; Baselga, J.; Hyman, D.M. A view on drug resistance in cancer. Nature 2019, 575, 299–309. [Google Scholar] [CrossRef] [Green Version]
- Min, K.J.; Han, M.A.; Kim, S.; Park, J.W.; Kwon, T.K. Osthole enhances TRAIL-mediated apoptosis through downregulation of c-FLIP expression in renal carcinoma Caki cells. Oncol. Rep. 2017, 37, 2348–2354. [Google Scholar] [CrossRef]
- Xu, Y.M.; Brooks, A.D.; Wijeratne, E.M.; Henrich, C.J.; Tewary, P.; Sayers, T.J.; Gunatilaka, A.A. 17beta-Hydroxywithanolides as Sensitizers of Renal Carcinoma Cells to Tumor Necrosis Factor-alpha Related Apoptosis Inducing Ligand (TRAIL) Mediated Apoptosis: Structure-Activity Relationships. J. Med. Chem. 2017, 60, 3039–3051. [Google Scholar] [CrossRef]
- Chen, S.; Liang, L.; Wang, Y.; Diao, J.; Zhao, C.; Chen, G.; He, Y.; Luo, C.; Wu, X.; Zhang, Y. Synergistic immunotherapeutic effects of Lycium barbarum polysaccharide and interferon-alpha2b on the murine Renca renal cell carcinoma cell line in vitro and in vivo. Mol. Med. Rep. 2015, 12, 6727–6737. [Google Scholar] [CrossRef] [Green Version]
- Kim, C.; Lee, J.H.; Baek, S.H.; Ko, J.H.; Nam, D.; Ahn, K.S. Korean Red Ginseng Extract Enhances the Anticancer Effects of Sorafenib through Abrogation of CREB and c-Jun Activation in Renal Cell Carcinoma. Phytother. Res. 2017, 31, 1078–1089. [Google Scholar] [CrossRef]
- Bolarinwa, I.F.; Orfila, C.; Morgan, M.R.A. Amygdalin content of seeds, kernels and food products commercially-available in the UK. Food Chem. 2014, 152, 133–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.-J.; Lee, S.-C.; Hsu, C.-H.; Kuo, Y.-H.; Yang, C.-C.; Lin, F.-J. Antcins, triterpenoids from Antrodia cinnamomea, as new agonists for peroxisome proliferator-activated receptor α. J. Food Drug Anal. 2019, 27, 295–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, L.; Yu, G.; Hao, W.; Yang, K.; Chen, H. The efficacy and safety of Curcuma longa extract and curcumin supplements on osteoarthritis: A systematic review and meta-analysis. Biosci. Rep. 2021, 41, BSR20210817. [Google Scholar] [CrossRef]
- Samavat, H.; Newman, A.R.; Wang, R.; Yuan, J.-M.; Wu, A.H.; Kurzer, M.S. Effects of green tea catechin extract on serum lipids in postmenopausal women: A randomized, placebo-controlled clinical trial. Am. J. Clin. Nutr. 2016, 104, 1671–1682. [Google Scholar] [CrossRef]
- Dickerson, F.; Origoni, A.; Katsafanas, E.; Squire, A.; Newman, T.; Fahey, J.; Xiao, J.-C.; Stallings, C.; Goga, J.; Khushalani, S.; et al. Randomized controlled trial of an adjunctive sulforaphane nutraceutical in schizophrenia. Schizophr. Res. 2021, 231, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Grammatikopoulou, M.G.; Gkiouras, K.; Papageorgiou, S.Τ.; Myrogiannis, I.; Mykoniatis, I.; Papamitsou, T.; Bogdanos, D.P.; Goulis, D.G. Dietary Factors and Supplements Influencing Prostate-Specific Antigen (PSA) Concentrations in Men with Prostate Cancer and Increased Cancer Risk: An Evidence Analysis Review Based on Randomized Controlled Trials. Nutrients 2020, 12, 2985. [Google Scholar] [CrossRef]
- Łata, E.; Fulczyk, A.; Ott, P.G.; Kowalska, T.; Sajewicz, M.; Móricz, Á.M. Thin-layer chromatographic quantification of magnolol and honokiol in dietary supplements and selected biological properties of these preparations. J. Chromatogr. A 2020, 1625, 461230. [Google Scholar] [CrossRef]
- Borgonovo, G.; De Petrocellis, L.; Schiano Moriello, A.; Bertoli, S.; Leone, A.; Battezzati, A.; Mazzini, S.; Bassoli, A. Moringin, A Stable Isothiocyanate from Moringa oleifera, Activates the Somatosensory and Pain Receptor TRPA1 Channel In Vitro. Molecules 2020, 25, 976. [Google Scholar] [CrossRef] [Green Version]
- Crocetto, F.; di Zazzo, E.; Buonerba, C.; Aveta, A.; Pandolfo, S.D.; Barone, B.; Trama, F.; Caputo, V.F.; Scafuri, L.; Ferro, M.; et al. Kaempferol, Myricetin and Fisetin in Prostate and Bladder Cancer: A Systematic Review of the Literature. Nutrients 2021, 13, 3750. [Google Scholar] [CrossRef]
- Ogbuagu, N.E.; Aluwong, T.; Ayo, J.O.; Sumanu, V.O. Effect of fisetin and probiotic supplementation on erythrocyte osmotic fragility, malondialdehyde concentration and superoxide dismutase activity in broiler chickens exposed to heat stress. J. Vet. Med. Sci. 2018, 80, 1895–1900. [Google Scholar] [CrossRef] [Green Version]
- Quinteros, J.A.; Scott, P.C.; Wilson, T.B.; Anwar, A.M.; Scott, T.; Muralidharan, C.; Van, T.T.H.; Moore, R.J. Isoquinoline alkaloids induce partial protection of laying hens from the impact of Campylobacter hepaticus (spotty liver disease) challenge. Poult. Sci. 2021, 100, 101423. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Chen, D.; Yan, Y.; Chen, G.; Ran, L.; Mi, J.; Lu, L.; Zeng, X.; Cao, Y. Effects of long-term consumption of polysaccharides from the fruit of Lycium barbarum on host’s health. Food Res. Int. 2021, 139, 109913. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Ouyang, S.; Yang, R.; Li, S.; Gong, Y.; Zou, L.; Jia, T.; Zhao, S.; Wu, B.; Yi, Z.; et al. Osthole alleviated diabetic neuropathic pain mediated by the P2X4 receptor in dorsal root ganglia. Brain Res. Bull. 2018, 142, 289–296. [Google Scholar] [CrossRef]
- Alrafiah, A. Thymoquinone Protects Neurons in the Cerebellum of Rats through Mitigating Oxidative Stress and Inflammation Following High-Fat Diet Supplementation. Biomolecules 2021, 11, 165. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).